Urinary Protein and Peptide Markers in Chronic Kidney Disease
Abstract
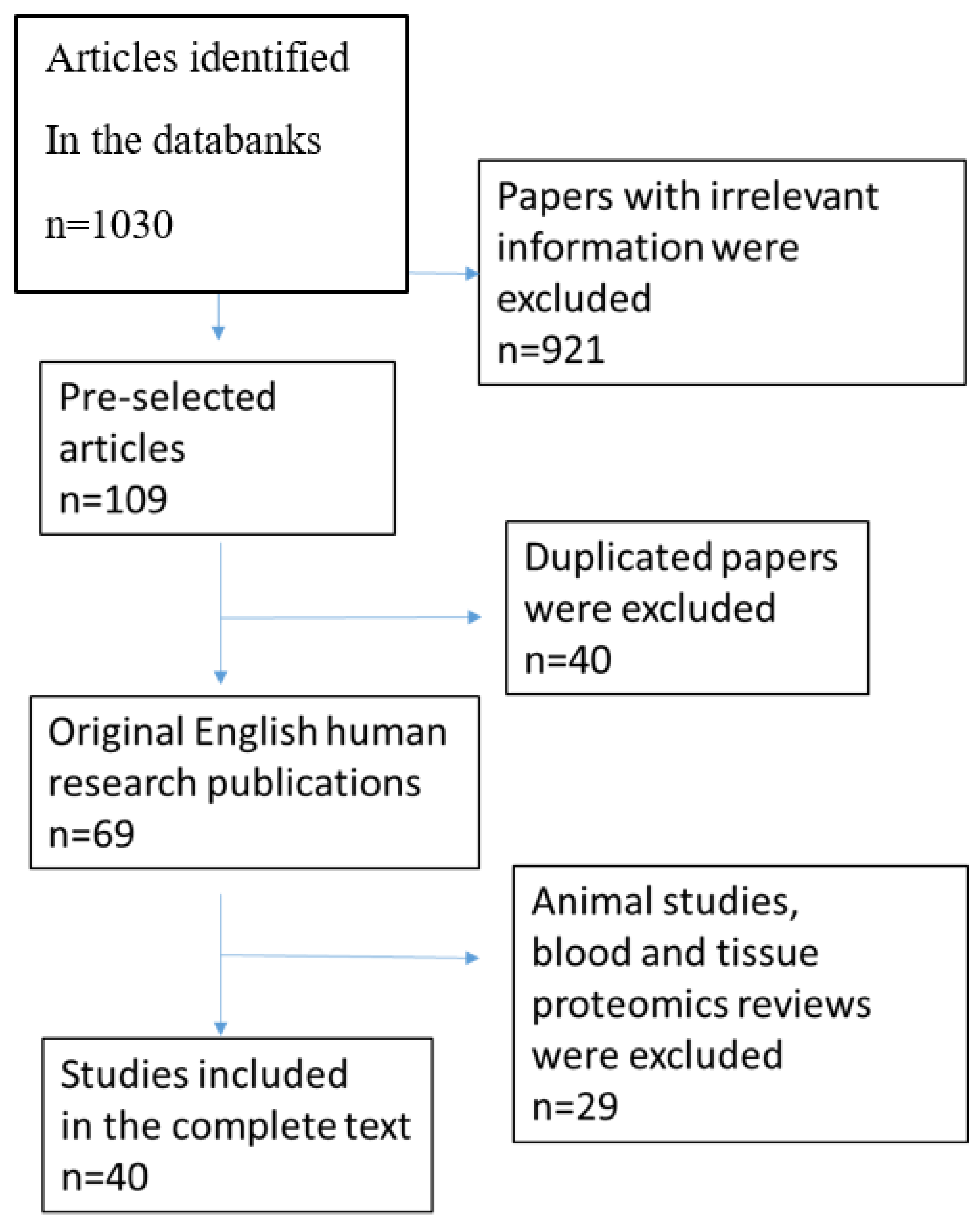
:1. Introduction
| Nephropathy Types | Method | Number of Patients | The Main Biomarkers | Functions of Proteins/Main Processes | References |
|---|---|---|---|---|---|
| Chronic kidney disease | CE-MS | 4766 | CKD 273 classifier ↓ fragments of different collagens, ↑ A1AT, serum albumin, hemoglobin α chain, fibrinogen α chain, uromodulin, Na+/K+-ATPase γ chain, and membrane-associated progesterone receptor component 1 | CKD progression and fibrosis accumulation | Good et al., 2010 [45] |
| CE-ESI-TOF MS | 1028 | CKD 273 classifier validation | Puntillo et al., 2017 [46] | ||
| CE-ESI-TOF MS | 1990 | CKD 273 classifier validation | Schanstra et al., 2015 [18] | ||
| CE-MS | 435 | FPP_29BH classifier ↑ cathepsin D, MMP-2, collagenase 3, MMP-14, α-2-HS-glycoprotein, fetuin-A, and 19 different collagen peptide fragments | Fibrosis accumulation | Catanese et al., 2021 [47] | |
| FSGS/MCD | 2D-DIGE-MS | 49 | A1AT, transferrin histatin-3 39S ribosomal protein L17 ↓ (FSGS vs. MCD) calretinin ↑ (FSGS vs. MCD) | Modulating immunity, inflammation and apoptosis; abnormal permeability of GBM, cell proliferation and differentiation | Perez et al., 2017 [48] |
| 2D-LC-MS/MS | 30 FSGS 30- MCD | ↑ Ubiquitin-60S ribosomal protein L40 (UBA52) (FSGS vs. MCD) | Protein degradation, stress response, and overexpression of UBA52 ameliorated the cell-cycle arrest | Wang et al., 2017 [49] | |
| LC-MS/MS | 4 MCD 4 FSGS | CD14, C9, and A1AT ↑ cadherin-like 26, RNase A Family 1, DIS3-like exonuclease 1 | Complement activation, inflammation, apoptosis, cells adhesion, and cell death | Choi et al., 2017 [50] | |
| nano-LC-MS/MS | 10 FSGS | ↑ Apolipoprotein 1 matrix-remodeling protein 8 (MXRA8) | Lipid oxidation and matrix accumulation | Kalantari et al., 2014 [51] | |
| nanoLC-MS/MS | 11 FSGS | ↑ DPEP1, CD59, CD44, insulin-like growth factor-binding protein 7, and roundabout homolog 4 | DPEP1 activates TRPC6 in podocytes complement activation, PETs activation, cell–cell interactions, cell adhesion, and maintenance of endothelial barrier organization and function | Nafar et al., 2014 [52] | |
| MALDI-MS imaging | 6 FSGS | A1AT | Marker of podocyte stress, excessive loss, and hypertrophy of podocytes and glomerulosclerosis | Smith et al. 2016 [53] | |
| CE-MS | 110 FSGS 35 MCD | ↑ Collagens, A1AT ↓ clusterin, uromodulin polymeric immunoglobulin receptor, Golgi-associated olfactory signaling regulator ↑ collagens, uromodulin, keratin apolipoprotein C-IV ↓ β-2-microglobulin, clusterin, complement C3 | Siwy et al., 2017 [54] | ||
| CE-MS | MCD 14 DN 11 | retinol-binding protein 4 and SH3 domain-binding glutamic acid-rich-like protein 3 | Proteins could distinguish between MCNS and DN | Araumi et al., 2021 [55] | |
| Membranous nephropathy | LC-MS/MS | 4 | SERPINA7 and CD44 | Cell–cell interactions, cell adhesion, and migration | Choi et al., 2017 [50] |
| iTRAQ and LC-MS/MS | 5 | Lysosome membrane protein-2 | Immune inflammation | Rood et al., 2015 [56] | |
| TMT1 and TMT2+nanoLC- MS/MS | 63 | A1ATafamin | Contribute to accumulation of mesangial matrix lipid metabolism | Pang et al., 2018 [57] | |
| MALDI-TOF MS | 13 | ↑UMOD ↑A1AT | Tubular dysfunction inflammation and apoptosis; matrix accumulation | Navarro-Muñoz et al., 2012 [58] | |
| CE-MS | 77 | ↑ A1AT, uromodulin, α-1B-glycoprotein, plasminogen, keratin, apolipoprotein C-IV ↓Fibrinogen α-chain, zinc finger protein ZFPM2, E1A-binding protein Microtubule-associated protein tauAP-3 complex subunit delta-1 | Siwy et al., 2017 [54] | ||
| CE-MS | 23 | The combination of urinary afamin and complement C3 urine/plasma ratio | Could distinguish between MN and DN | Araumi et al., 2021 [55] | |
| IgA nephropathy | iTRAQ-MS | 4 | Complement C9, Ig kappa chain C region, cytoskeletal keratins type I (10), and type 2 (1, 5) | Complement activation; glomerular filtration barrier damage | Ning et al., 2017 [59] |
| 2D-LC-MS/MS and iTRAQ | 12 | ICAM 1, metalloproteinase inhibitor 1, antitrombin III, and adiponectin | Inflammation; urine proteins originated from serum leakage | Guo et al., 2018 [60] | |
| MALDI-TOF/TOF MS | 20 | ↓ UMOD ↑ A1AT | Accumulation of mesangial matrix | Prikryl et al., 2017 [61] | |
| CE-MS | 209 | ↓ Collagen I ↑ A1AT | Matrix accumulation and glomerulosclerosis | Rudnicki et al., 2020 [62] | |
| IEF/LC-MS/MS | 30 | ↑ α-2-macroglobulin, ceruloplasmin, complement C3, complement C4a, haptoglobin, prothrombin, and antithrombin-III | Coagulation, complement activation, and cell interaction in inflammation | Mucha et al., 2014 [63] | |
| 2D-DIGE-MALDI-TOF/TOF | 43 | Albumin fragments, A1AT, and α-1- β-glycoprotein ↓ laminin G-like 3 (LG3) fragment of endorepellin | Matrix accumulation apoptosis of endothelial cells; extensive fibrosis | Surin et al., 2013 [64] | |
| nanoLC-MS/MS | 13 | CD44, glycoprotein 2, vasorin, epidermal growth factor, CMRF35-like molecule 9, protocadherin, utreoglobin, dipeptidyl peptidase IV, NHL repeat-containing protein 3, SLAM family member 5 (CD84) | Activation of apoptosis, immune inflammation, coagulation, and complement | Samavat et al., 2015 [36] | |
| LC-MS/MS | 24 | ↓ Aminopeptidase N and vasorin precursor levels were higher on average in the urinary exosome samples ↑ A1AT and ceruloplasmin | IgAN markers vs. thin basement membrane nephropathy | Moon et al., 2011 [65] | |
| CE-MS | 179 | ↑ Small proline-rich protein, leucine-rich repeat-containing protein, A1AT, sodium/potassium-transporting ATPase subunit gamma | Siwy et al., 2017 [54] | ||
| Lupus nephritis | SELDI-TOF MS | 49 inactive 26 active | Protein ions with m/z of 3340 and 3980 | Distinguished active from inactive LN | Mosley et al., 2006 [66] |
| SELDI-TOF MS | 19 active | Hepcidin, fragments of A1AT, and albumin | Infiltration interstitial leukocytes, cytokines production, and matrix accumulation | Zhang et al., 2008 [67] | |
| CE-MS | 92 | Collagens, uromodulin, protein S100-A9, clusterin, β-2-microglobulin, and α-2-HS-glycoprotein | Matrix accumulation | Siwy et al., 2017 [54] | |
| 2D- DIGE-MALDI-TOF MS/MS | 88 | Haptoglobin, α-1 anti-chymotrypsin, and retinol-binding protein | Effect on inflammation loss of proximal renal tubule function | Aggarwal et al., 2017 [68] | |
| iTRAQ-MS | 61 | α1-antichymotrypsin (SERPINA3) | Marker of LN activity | Turnier et al., 2019 [69] | |
| CE-MS | 93 | CKD273 validation | It could not identify urinary biomarkers and predict active LN | Tailliar et al., 2021 [70] | |
| Diabetic nephropathy | 2D-DIGE-LC-MS/MS | 33 | ↑ α1B-Glycoprotein zinc-α2-glycoprotein, α2-HS-glycoprotein vitamin D–binding protein (VDBP), calgranulin B, A1AT, hemopexin ↓ Transthyretin, apolipoprotein A1, AMBP, and plasma retinol-binding protein | Hyperglycosylated state and matrix accumulation | Rao et al., 2007 [71] |
| CE-MS | 305 | ↓ Collagen type I and uromodulin fragments ↑albumin | Increased synthesis of protease inhibitors diminishes excretion of collagen fragments | Rossing et al., 2008 [72] | |
| CE-MS | 126 | CKD 273 classifier | Good et al., 2010 [45] | ||
| CE-MS | 576 | ↑ Clusterin, apolipiprotein ↓ hemoglobin, uromodulin, small proline-rich protein 3, leucine-rich repeat-containing protein 25 | Accumulation of proteins in the extracellular matrix chronic renal damage | Siwy et al., 2017 [54] | |
| iTRAQ | 50 | 408 N-linked glycoproteins, A1AT, and ceruloplasmin | Different stage of DN | Jin et al., 2020 [73] | |
| 2D-DIGE-MALDI Q-TOF | 268 | Transthyretin/prealbumin and Ig kappa C chain region + cystatin C, and ubiquitin + α-1-acid glycoprotein 1, apolipoprotein A1, α-1 microglobulin/bikunin precursor, pigment epithelium-derived factor, zinc α-2 glycoprotein | 0–5 years of T2DM duration 5–10 years more than 10 years | Patel and Kalia, 2019 [74] | |
| iTRAQ | 65 | ↑Haptoglobin and α-1-microglobulin/bikunin precursor | Liao et al., 2018 [75] | ||
| C18 plate–MALDI-TOF | 174 | ↑ β2-microglobulin and clara-cell protein | Proximal tubular dysfunction | Chen et al., 2018 [76] |
2. Chronic Kidney Disease (CKD)
3. Minimal Change Disease and Focal Segmental Glomerulosclerosis
4. Membranous Nephropathy
5. IgA Nephropathy
6. Diabetic Nephropathy
7. Lupus Nephritis
8. Non-Specific Urinary Protein Markers
9. Conclusions
| Potential Urine Protein Marker | Nephropaty | ||||||
|---|---|---|---|---|---|---|---|
| CKD | FSGS | MCD | MN | IgAN | LN | DN | |
| α-1-antitrypsin (A1AT) | ↑ [45] | ↑ [48,53,54] | ↑ [48,50] | ↑ [54,57,58,82] | ↑ [54,61,62,64,65] | ↑ [67] | ↑ [71,73] |
| Serum albumin | ↑ [45] | ↑ [64] | ↑ [67] | ↑ [72,74] | |||
| Hemoglobin | ↑ [45] | ↓ [54] | |||||
| Fibrinogen α chain | ↑ [45] | ↓ [54] | |||||
| Uromodulin | ↑ [45] | ↓ [54] | ↑ [54] | ↑ [54,58] | ↓ [61] | ↑ [54] | ↓ [54,72] |
| Na+/K+-ATPase γ chain | ↑ [45] | ↑ [54] | |||||
| Membrane-associated progesterone receptor component 1 | ↑ [45] | ||||||
| Collagens | ↓ [45] ↑ [47] | ↑ [54] | ↑ [54] | ↓ [45,62,72] | ↑ [54] | ↓ [72] | |
| Cathepsin D | ↑ [47] | ||||||
| MMP-2 | ↑ [47] | ||||||
| MMP-14 | ↑ [47] | ||||||
| Collagenase 3 | ↑ [47] | ||||||
| α-2-HS-glycoprotein | ↑ [47] | ↑ [54] | ↑ [71] | ||||
| Fetuin-A | ↑ [47] | ||||||
| Cathepsin B | ↑ [94] | ||||||
| Cathepsin C | ↑ [94] | ||||||
| Annexin A3 | ↑ [94] | ||||||
| Transferrin | ↑ [48] | ↑ [48] | |||||
| Histatin-3 | ↑ [48] | ↑ [48] | |||||
| 39S ribosomal protein L17 (FSGS/MCD) | ↓ [48] | ↑ [48] | |||||
| Calretinin (FSGS/MCD) | ↑ [48] | ↓ [48] | |||||
| UBA52 (FSGS/MCD) | ↑ [49] | ↓ [49] | |||||
| Cadherin-like 26 | ↑ [50] | ||||||
| RNase A Family 1 | ↑ [50] | ||||||
| DIS3-like exonuclease 1 | ↑ [50] | ||||||
| CD14 | ↑ [50] | ||||||
| Complement C9 | ↑ [50] | ↑ [59] | |||||
| Apolipoprotein A1 | ↑ [51] | ↓ [71], ↑ [54,74] | |||||
| Matrix-remodeling protein 8 | ↑ [51] | ||||||
| Dipeptidase 1 (DPEP1) | ↓ [52] | ||||||
| CD59 | ↑ [52] | ||||||
| CD44 | ↑ [52] | ↑ [50] | ↑ [36] | ||||
| Insulin-like growth factor-binding protein 7 | ↑ [52] | ||||||
| Roundabout homolog 4 | ↑ [52] | ||||||
| Clusterin | ↓ [54] | ↓ [54] | ↑ [54] | ↑ [54] | |||
| Polymeric immunoglobulin receptor | ↓ [54] | ||||||
| Golgi-associated olfactory signaling regulator | ↓ [54] | ||||||
| Apolipoprotein C-IV | ↑ [54] | ↑ [54] | |||||
| β-2-microglobulin | ↓ [54] | ↑ [54] | ↑ [76] | ||||
| Complement C3 | ↓ [54] | [55] | ↑ [63] | ||||
| Retinol-binding protein 4 | [55] | [117] | [55] | ||||
| SH3 domain-binding glutamic acid-rich-like protein 3 | [55] | [55] | |||||
| Thyroxine-binding globulin (SERPINA7) | ↑ [50] | ||||||
| Lysosome membrane protein-2 | ↑ [105] | ||||||
| Afamin | ↑ [55,57,101] | ||||||
| α-1B-glycoprotein | ↑ [54] | ↑ [64] | ↑ [71] | ||||
| Plasminogen | ↑ [54] | ||||||
| Zinc finger protein ZFPM2 | ↓ [54] | ||||||
| E1A-binding protein | ↓ [54] | ||||||
| Microtubule-associated protein tauAP-3 complex subunit delta-1 | ↓ [54] | ||||||
| LDB3 | ↑ [100] | ||||||
| PDLI5 | ↑ [100] | ||||||
| Ig kappa chain C region | ↑ [59] | ↑ [74] | |||||
| Cytoskeletal keratins type I (10) and type 2 (1, 5) | ↑ [59] | ||||||
| ICAM1 | ↑ [60] | ||||||
| Metalloproteinase inhibitor 1 | ↑ [60] | ||||||
| Antitrombin III | ↑ [60,63] | ||||||
| Adiponectin | ↑ [60] | ||||||
| α-2-macroglobulin | ↑ [63] | ||||||
| Ceruloplasmin | ↑ [63,65] | ↑ [73] | |||||
| Complement C4a | ↑ [63] | ||||||
| Haptoglobin | ↑ [63] | ↑ [68] | ↑ [75] | ||||
| Prothrombin | ↑ [63] | ||||||
| LG3 fragment of endorepellin | ↓ [64] | ||||||
| Glycoprotein 2 | ↑ [36] | ||||||
| Vasorin | ↑ [36] ↓ [65] | ||||||
| Epidermal growth factor | ↑ [36] | ||||||
| CMRF35-like molecule 9 | ↑ [36] | ||||||
| Protocadherin | ↑ [36] | ||||||
| Utreoglobin | ↑ [36] | ||||||
| Dipeptidyl peptidase IV | ↑ [36] | ||||||
| NHL repeat-containing protein 3 | ↑ [36] | ||||||
| SLAM family member 5 (CD84) | ↑ [36] | ||||||
| Aminopeptidase N | ↓ [65] | ||||||
| Fibulin-5 | ↓ [108] | ||||||
| YIP1 family member 3 | ↓ [108] | ||||||
| Prasoposin | ↓ [108] | ||||||
| Osteopontin | ↓ [108] | ↑ [110] | |||||
| Small proline-rich protein 3 | ↑ [108] | ↓ [54] | |||||
| Leucine-rich repeat-containing protein 25 | ↑ [54] | ↓ [54] | |||||
| 3340 and 39110 (m/z) | ↑ [66] | ||||||
| Hepcidin | ↑ [67] | ||||||
| Protein S89-A9 | ↑ [54] | ||||||
| α-1 anti-chymotrypsin (SERPINA3) | ↑ [68,69] | ||||||
| Retinol binding protein | ↑ [68] | ↓ [71] | |||||
| Zinc-α2-glycoprotein | ↑ [71,74] | ||||||
| Vitamin D-binding protein | ↑ [71] | ||||||
| Calgranulin B | ↑ [71] | ||||||
| Hemopexin | ↑ [71] | ||||||
| Transthyretin | ↓ [71,74] | ||||||
| α-1 microglobulin/bikunin precursor (AMBP) | ↓ [71] ↑ [74,75] | ||||||
| 408 N-linked glycoproteins | ↑ [73] | ||||||
| Cystatin C | ↑ [74] | ||||||
| Ubiquitin | ↑ [74] | ||||||
| α-1-acid glycoprotein 1 | ↑ [74] | ||||||
| Pigment epithelium-derived factor | ↑ [74] | ||||||
| Clara cell protein CC16 | ↑ [76] | ||||||
| Fibronectin | ↑ [110] | ||||||
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kidney Disease Improving Global Outcomes (KDIGO). KDIGO Clinical Practice Guideline for Glomerulonephritis; Kidney International Supplements; Nature Publishing Group: New York, NY, USA, 2012. [Google Scholar]
- National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: Evaluation, classification, and stratification. Am. J. Kidney Dis. 2002, 39, 1–266. [Google Scholar]
- Sarnak, M.J.; Levey, A.S.; Schoolwerth, A.C.; Coresh, J.; Culleton, B.; Hamm, L.L.; McCullough, P.A.; Kasiske, B.L.; Kelepouris, E.; Klag, M.J.; et al. Kidney Disease as a Risk Factor for Development of Cardiovascular Disease. Circulation 2003, 108, 2154–2169. [Google Scholar] [CrossRef] [PubMed]
- Alani, H.; Tamimi, A.; Tamimi, N. Cardiovascular co-morbidity in chronic kidney disease: Current knowledge and future research needs. World J. Nephrol. 2014, 3, 156–168. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.; Ordoñez, J.; Chertow, G.; Fan, D.; McCulloch, C.; Go, A. The risk of acute renal failure in patients with chronic kidney disease. Kidney Int. 2008, 74, 101–107. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tonelli, M.; Wiebe, N.; Culleton, B.; House, A.; Rabbat, C.; Fok, M.; McAlister, F.; Garg, A.X. Chronic Kidney Disease and Mortality Risk: A Systematic Review. J. Am. Soc. Nephrol. 2006, 17, 2034–2047. [Google Scholar] [CrossRef] [Green Version]
- Hsu, C.-Y.; Iribarren, C.; McCulloch, C.E.; Darbinian, J.; Go, A.S. Risk Factors for End-Stage Renal Disease: 25-year follow-up. Arch. Intern. Med. 2009, 169, 342–350. [Google Scholar] [CrossRef] [Green Version]
- Hill, N.R.; Fatoba, S.T.; Oke, J.L.; Hirst, J.; O’Callaghan, C.A.; Lasserson, D.; Hobbs, R. Global Prevalence of Chronic Kidney Disease—A Systematic Review and Meta-Analysis. PLoS ONE 2016, 11, e0158765. [Google Scholar] [CrossRef]
- Schieppati, A.; Remuzzi, G. Chronic renal diseases as a public health problem: Epidemiology, social, and economic implications. Kidney Int. 2005, 68, S7–S10. [Google Scholar] [CrossRef] [Green Version]
- Bommer, J. Prevalence and socio-economic aspects of chronic kidney disease. Nephrol. Dial. Transplant. 2002, 17, 8–12. [Google Scholar] [CrossRef] [Green Version]
- Vos, T.; Allen, C.; Arora, M.; Barber, R.M.; Bhutta, Z.A.; Brown, A.; Carter, A.; Casey, D.C.; Charlson, F.J.; Chen, A.Z.; et al. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2015, 388, 1545–1602. [Google Scholar] [CrossRef] [Green Version]
- Dhaun, N.; Bellamy, C.O.; Cattran, D.C.; Kluth, D.C. Utility of renal biopsy in the clinical management of renal disease. Kidney Int. 2014, 85, 1039–1048. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Filip, S.; Pontillo, C.; Schanstra, J.P.; Vlahou, A.; Mischak, H.; Klein, J. Urinary proteomics and molecular determinants of chronic kidney disease: Possible link to proteases. Expert Rev. Proteom. 2014, 11, 535–548. [Google Scholar] [CrossRef] [PubMed]
- Mischak, H.; Delles, C.; Vlahou, A.; Vanholder, R. Proteomic biomarkers in kidney disease: Issues in development and im-plementation. Nat. Rev. Nephrol. 2015, 11, 221–232. [Google Scholar] [CrossRef]
- Decramer, S.; Gonzalez de Peredo, A.; Breuil, B.; Mischak, H.; Monsarrat, B.; Bascands, J.-L.; Schanstra, J.P. Urine in Clinical Proteomics. Mol. Cell. Proteom. 2008, 7, 850–1862. [Google Scholar] [CrossRef] [Green Version]
- Thomas, S.; Hao, L.; Ricke, W.; Li, L. Biomarker discovery in mass spectrometry-based urinary proteomics. Proteom. Clin. Appl. 2016, 10, 358–370. [Google Scholar] [CrossRef] [PubMed]
- Argiles, A.; Siwy, J.; Duranton, F.; Gayrard, N.; Dakna, M.; Lundin, U.; Osaba, L.; Delles, C.; Mourad, G.; Weinberger, K.M.; et al. CKD273, a New Proteomics Classifier Assessing CKD and Its Prognosis. PLoS ONE 2013, 8, e62837. [Google Scholar] [CrossRef] [Green Version]
- Schanstra, J.P.; Zürbig, P.; Alkhalaf, A.; Argiles, A.; Bakker, S.J.L.; Beige, J.; Bilo, H.J.G.; Chatzikyroku, C.; Dakna, M.; Dawson, J.; et al. Diagnosis and prediction of CKD progression by assessment of urinary peptides. JASN 2015, 26, 1999–2010. [Google Scholar] [CrossRef] [PubMed]
- Zürbig, P.; Jerums, G.; Hovind, P.; MacIsaac, R.J.; Mischak, H.; Nielsen, S.E.; Panagiotopoulos, S.; Persson, F.; Rossing, P. Urinary Proteomics for Early Diagnosis in Diabetic Nephropathy. Diabetes 2012, 61, 3304–3313. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Celis, J.E.; Gromova, I.; Moreira, J.M.; Cabezon, T.; Gromov, P. Impact of proteomics on bladder cancer research. Pharmacogenomics 2004, 5, 381–394. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.-T.; Chen, H.-W.; Domanski, D.; Smith, D.S.; Liang, K.-H.; Wu, C.-C.; Chen, C.-L.; Chung, T.; Chen, M.-C.; Chang, Y.-S.; et al. Multiplexed quantification of 63 proteins in human urine by multiple reaction monitoring-based mass spectrometry for discovery of potential bladder cancer biomarkers. J. Proteom. 2012, 75, 3529–3545. [Google Scholar] [CrossRef] [PubMed]
- Shi, T.; Gao, Y.; Quek, S.I.; Fillmore, T.L.; Nicora, C.D.; Su, D.; Zhao, R.; Kagan, J.L.; Srivastava, S.; Rodland, K.D.; et al. A Highly Sensitive Targeted Mass Spectrometric As-say for Quantification of AGR2 Protein in Human Urine and Serum. J. Proteom. Res. 2014, 2, 875–882. [Google Scholar] [CrossRef] [PubMed]
- Ye, B.; Skates, S.; Mok, S.C.; Horick, N.K.; Rosenberg, H.F.; Vitonis, A.; Edwards, D.; Sluss, P.; Han, W.K.; Berkowitz, R.S.; et al. Proteomic-Based Discovery and Characterization of Glycosylated Eosinophil-Derived Neurotoxin and COOH-Terminal Osteopontin Fragments for Ovarian Cancer in Urine. Clin. Cancer Res. 2006, 12, 432–441. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mischak, H.; Kaiser, T.; Walden, M.; Hillmann, M.; Wittke, S.; Herrmann, A.; Knueppel, S.; Haller, H.; Fliser, D. Proteomic analysis for the assessment of diabetic renal damage in humans. Clin. Sci. 2004, 107, 485–495. [Google Scholar] [CrossRef] [PubMed]
- Buhimschi, I.A.; Zhao, G.; Funai, E.F.; Harris, N.; Sasson, I.E.; Bernstein, I.M.; Saade, G.R.; Buhimschi, C.S. Proteomic profiling of urine identifies specific fragments of SERPINA1 and albumin as biomarkers of preeclampsia. Am. J. Obstet. Gynecol. 2008, 199, 551.e1–551.e16. [Google Scholar] [CrossRef] [PubMed]
- Carty, D.M.; Siwy, J.; Brennand, J.E.; Zürbig, P.; Mullen, W.; Franke, J.; McCulloch, J.W.; North, R.A.; Chappell, L.C.; Mischak, H.; et al. Urinary Proteomics for Prediction of Preeclampsia. Hypertension 2011, 57, 561–569. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kononikhin, A.S.; Zakharova, N.V.; Sergeeva, V.A.; Indeykina, M.I.; Starodubtseva, N.L.; Bugrova, A.E.; Muminova, K.T.; Khodzhaeva, Z.S.; Popov, I.A.; Shao, W.; et al. Differential Diagnosis of Preeclampsia Based on Urine Peptidome Features Revealed by High Resolution Mass Spectrometry. Diagnostics 2020, 10, 1039. [Google Scholar] [CrossRef] [PubMed]
- Ward, D.G.; Nyangoma, S.; Joy, H.; Hamilton, E.; Wei, W.; Tselepis, C.; Steven, N.; Wakelam, M.J.; Johnson, P.J.; Ismail, T.; et al. Proteomic profiling of urine for the detection of colon cancer. Proteom. Sci. 2008, 6, 19. [Google Scholar] [CrossRef] [Green Version]
- Tantipaiboonwong, P.; Sinchaikul, S.; Sriyam, S.; Phutrakul, S.; Chen, S.-T. Different techniques for urinary protein analysis of normal and lung cancer patients. Proteomics 2005, 5, 1140–1149. [Google Scholar] [CrossRef] [PubMed]
- Metzger, J.; Negm, A.A.; Plentz, R.R.; Weismüller, T.J.; Wedemeyer, J.; Karlsen, T.H.; Dakna, M.; Mullen, W.; Mischak, H.; Manns, M.P.; et al. Urine proteomic analysis differentiates cholangiocarcinoma from primary sclerosing cholangitis and other benign biliary disorders. Gut 2012, 62, 122–130. [Google Scholar] [CrossRef]
- Zimmerli, L.U.; Schiffer, E.; Zürbig, P.; Good, D.M.; Kellmann, M.; Mouls, L.; Pitt, A.R.; Coon, J.J.; Schmeider, R.D.; Peter, K.H.; et al. Urinary Proteomic Biomarkers in Coronary Artery Disease. Mol. Cell. Proteom. 2008, 7, 290–298. [Google Scholar] [CrossRef] [Green Version]
- Kaiser, T.; Kamal, H.; Rank, A.; Kolb, H.-J.; Holler, E.; Ganser, A.; Hertenstein, B.; Mischak, B.; Weisseinger, M.E. Proteomics applied to the clinical follow-up of pa-tients after allogeneic hematopoietic stem cell transplantation. Blood 2004, 104, 340–349. [Google Scholar] [CrossRef] [Green Version]
- Taneja, S.; Sen, S.; Gupta, V.K.; Aggarwal, R.; Jameel, S. Plasma and urine biomarkers in acute viral hepatitis E. Proteome Sci. 2009, 7, 39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kalantari, S.; Jafari, A.; Moradpoor, R.; Ghasemi, E.; Khalkhal, E. Human urine proteomics: Analytical techniques and clini-cal applications in renal diseases. Int. J. Proteom. 2015, 2015, 1–17. [Google Scholar] [CrossRef]
- Fang, X.; Wu, H.; Lu, M.; Cao, Y.; Wang, R.; Wang, M.; Gao, C.; Xia, Z. Urinary proteomics of Henoch-Schönlein purpura nephri-tis in children using liquid chromatography-tandem mass spectrometry. Clin. Proteom. 2020, 17, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Samavat, S.; Kalantari, S.; Nafar, M.; Rutishauser, D.; Rezaei-Tavirani, M.; Parvin, M.; Zubarev, R.A. Diagnostic Urinary Pro-teome Profile for Immunoglobulin A Nephropathy. Iran. J. Kid. Dis. 2015, 9, 239–248. [Google Scholar]
- Cunningham, R.; Ma, D.; Li, L. Mass spectrometry-based proteomics and peptidomics for systems biology and biomarker discovery. Front. Biol. 2012, 7, 313–335. [Google Scholar] [CrossRef] [PubMed]
- Di Meo, A.; Pasic, M.D.; Yousef, G.M. Proteomics and peptidomics: Moving toward precision medicine in urological malignancies. Oncotarget 2016, 7, 52460–52474. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feist, P.; Hummon, A.B. Proteomic Challenges: Sample Preparation Techniques for Microgram-Quantity Protein Analysis from Biological Samples. Int. J. Mol. Sci. 2015, 16, 3537. [Google Scholar] [CrossRef] [Green Version]
- Khan, A.; Packer, N. Simple Urinary Sample Preparation for Proteomic Analysis. J. Proteom. Res. 2006, 5, 2824–2838. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, T.; Biancotto, A.; Moaddel, R.; Moore, A.Z.; Gonzalez-Freire, M.; Aon, M.A.; Candia, J.; Zhang, P.; Cheung, F.; Fantoni, G.; et al. Plasma proteomic signature of age in healthy humans. Aging Cell 2018, 17, e12799. [Google Scholar] [CrossRef] [Green Version]
- Shao, C.; Zhao, M.; Chen, X.; Sun, H.; Yang, Y.; Xiao, X.; Guo, Z.; Liu, X.; Lv, Y.; Chen, X.; et al. Comprehensive Analysis of Individual Variation in the Urinary Proteome Revealed Significant Gender Differences. Mol. Cell. Proteom. 2019, 18, 1110–1122. [Google Scholar] [CrossRef] [PubMed]
- Nkuipou-Kenfack, E.; Bhat, A.; Klein, J.; Jankowski, V.; Mullen, W.; Vlahou, A.; Dakna, M.; Koeck, T.; Schanstra, J.P.; Zürbig, P.; et al. Identification of ageing-associated naturally occurring peptides in human urine. Oncotarget 2015, 6, 34106–34117. [Google Scholar] [CrossRef] [PubMed]
- Mischak, H.; Ioannidis, J.P.; Argiles, A.; Attwood, T.; Bongcam-Rudloff, E.; Brönstrup, M.; Charonis, A.; Chrousos, G.P.; Delles, C.; Dominiczak, A.; et al. Implementation of proteomic biomarkers: Making it work. Eur. J. Clin. Investig. 2012, 42, 1027–1036. [Google Scholar] [CrossRef] [PubMed]
- Good, D.M.; Zürbig, P.; Argilés, A.; Bauer, H.W.; Behrens, G.; Coon, J.J.; Dakna, M.; Decramer, S.; Delles, C.; Dominiczak, A.F.; et al. Naturally occurring human urinary peptides for use in diagnosis of chronic kidney disease. Mol. Cell. Proteom. 2010, 9, 2424–2437. [Google Scholar] [CrossRef] [Green Version]
- Pontillo, C.; Zhang, Z.-Y.; Schanstra, J.P.; Jacobs, L.; Zürbig, P.; Thijs, L.; Ramírez-Torres, A.; Heerspink, H.J.; Lindhardt, M.; Klein, R.; et al. Prediction of Chronic Kidney Disease Stage 3 by CKD273, a Urinary Proteomic Biomarker. Kidney Int. Rep. 2017, 2, 1066–1075. [Google Scholar] [CrossRef]
- Catanese, L.; Siwy, J.; Mavrogeorgis, E.; Amann, K.; Mischak, H.; Beige, J.; Rupprecht, H. A Novel Urinary Proteomics Classifier for Non-Invasive Evaluation of Interstitial Fibrosis and Tubular Atrophy in Chronic Kidney Disease. Proteomes 2021, 9, 32. [Google Scholar] [CrossRef] [PubMed]
- Pérez, V.; López, D.; Boixadera, E.; Ibernón, M.; Espinal, A.; Bonet, J.; Romero, R. Comparative differential proteomic analysis of minimal change disease and focal segmental glomerulosclerosis. BMC Nephrol. 2017, 18, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; Zheng, C.; Wang, X.; Zuo, K.; Liu, Z. Proteomic profile-based screening of potential protein biomarkers in the urine of patients with nephrotic syndrome. Mol. Med. Rep. 2017, 16, 6276–6284. [Google Scholar] [CrossRef]
- Choi, Y.W.; Kim, Y.G.; Song, M.-Y.; Moon, J.-Y.; Jeong, K.-H.; Lee, T.-W.; Ihm, C.-G.; Park, K.-S.; Lee, S.-H. Potential urine proteomics biomarkers for primary nephrotic syndrome. Clin. Proteom. 2017, 14, 18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kalantari, S.; Nafar, M.; Samavat, S.; Rezaei-Tavirani, M.; Rutishauser, D.; Zubarev, R. Urinary Prognostic Biomarkers in Patients With Focal Segmental Glomerulosclerosis. Nephro-Urol. Mon. 2014, 6, e16806. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nafar, M.; Kalantari, S.; Samavat, S.; Rezaei-Tavirani, M.; Rutishuser, D.; Zubarev, R.A. The novel diagnostic bi-omarkers for focal segmental Glomerulosclerosis. Int. J. Nephrol. 2014, 2014, 574261. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, A.; L’Imperio, V.; De Sio, G.; Ferrario, F.; Scalia, S.; Dell’Antonio, G.; Pierrutzzi, F.; Pontillo, C.; Filip, S.; Markoska, A.; et al. α-1-Antitrypsin detected by MALDI imaging in the study of glomerulonephritis: Its relevance in chronic kidney disease progression. Proteomics 2016, 16, 1759–1766. [Google Scholar] [CrossRef] [PubMed]
- Siwy, J.; Zürbig, P.; Argiles, A.; Beige, J.; Haubitz, M.; Jankowski, J.; Julian, B.A.; Linde, P.B.; Marx, D.; Mishkac, H.; et al. Noninvasive diagnosis of chronic kidney diseases using urinary proteome analysis. Nephrol. Dial. Transplant. 2017, 32, 2079–2089. [Google Scholar] [CrossRef] [PubMed]
- Araumi, A.; Osaki, T.; Ichikawa, K.; Kudo, K.; Suzuki, N.; Watanabe, S.; Watanabe, M.; Konta, T. Urinary and plasma proteomics to discover biomarkers for diagnosing between diabetic nephropathy and minimal change nephrotic syndrome or mem-branous nephropathy. Biochem. Biophys. Rep. 2021, 27, 101102. [Google Scholar] [CrossRef]
- Rood, I.M.; Merchant, M.L.; Wilkey, D.W.; Zhang, T.; Zabrouskov, V.; van der Vlag, J.; Dijikman, H.B.; Wilemens, B.K.; Wetzles, J.F.; Klein, J.B.; et al. Increased expression of lysosome membrane protein 2 in glomeruli of patients with idiopathic membranous nephropathy. Proteomics 2015, 15, 3722–3730. [Google Scholar] [CrossRef] [PubMed]
- Pang, L.; Li, Q.; Li, Y.; Liu, Y.; Duan, N.; Li, H. Urine proteomics of primary membranous nephropathy using nanoscale liquid chromatography tandem mass spectrometry analysis. Clin. Proteom. 2018, 15, 5. [Google Scholar] [CrossRef] [Green Version]
- Navarro-Muñoz, M.; Ibernon, M.; Bonet, J.; Pérez, V.; Pastor, M.C.; Bayés, B.; Casado-Vela, J.; Navarro, M.; Ara, J.; Espinal, A.; et al. Uromodulin and α1-Antitrypsin Urinary Peptide Analysis to Differentiate Glomerular Kidney Diseases. Kidney Blood Press. Res. 2012, 35, 314–325. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ning, X.; Yin, Z.; Li, Z.; Xu, J.; Wang, L.; Shen, W.; Lu, Y.; Cai, G.; Zhang, X.; Chen, X. Comparative proteomic analysis of urine and laser microdissected glomeruli in IgA nephropathy. Clin. Exp. Pharmacol. Physiol. 2017, 44, 576–585. [Google Scholar] [CrossRef]
- Guo, Z.; Wang, Z.; Lu, C.; Yang, S.; Sun, H.; Reziw; Guo, Y.; Sun, W.; Yue, H. Analysis of the differential urinary protein profile in IgA nephropathy patients of Uygur ethnicity. BMC Nephrol. 2018, 19, 358. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Prikryl, P.; Vojtova, I.; Maixnerova, D.; Vokurka, M.; Neprasova, M.; Zima, T.; Tesar, V. Proteomic Approach for Identification of IgA Nephropathy-Related Biomarkers in Urine. Physiol. Res. 2017, 66, 621–632. [Google Scholar] [CrossRef] [PubMed]
- Rudnicki, M.; Siwy, J.; Wendt, R.; Lipphardt, M.; Koziolek, M.J.; Maixnerova, D.; Peters, B.; Kerschbaum, J.; Leierer, J.; Neprasova, M.; et al. Urine proteomics for prediction of disease progression in patients with IgA nephropathy. Nephrol. Dial. Transplant. 2020, 3, 32. [Google Scholar] [CrossRef]
- Mucha, K.; Bakun, M.; Jaźwiec, R.; Dadlez, M.; Florczak, M.; Bajor, M.; Gala, K.; Pączek, L. Complement components, proteolysis-related, and cell communication?related proteins detected in urine proteomics are associated with IgA nephropathy. Pol. Arch. Intern. Med. 2014, 124, 380–386. [Google Scholar] [CrossRef] [PubMed]
- Surin, B.; Sachon, E.; Rougier, J.-P.; Steverlynck, C.; Garreau, C.; Lelongt, B. LG3 fragment of endorepellin is a possible bi-omarker of severity in IgA nephropathy. Proteomics 2013, 13, 142–152. [Google Scholar] [CrossRef]
- Moon, P.G.; Lee, J.E.; You, S.; Kim, T.K.; Cho, J.H.; Kim, I.S.; Kwon, T.-H.; Kim, C.-D.; Park, S.-H.; Hwang, D.; et al. Proteomic analysis of urinary exosomes from patients of early IgA nephropathy and thin basement membrane nephropathy. Proteomics 2011, 11, 2459–2475. [Google Scholar] [CrossRef] [PubMed]
- Mosley, K.; Tam, F.W.K.; Edwards, R.J.; Crozier, J.; Pusey, C.D.; Lightstone, L. Urinary proteomic profiles distinguish between active and inactive lupus nephritis. Rheumatology 2006, 45, 1497–1504. [Google Scholar] [CrossRef] [Green Version]
- Zhang, X.; Jin, M.; Wu, H.; Nadasdy, T.; Nadasdy, G.; Harris, N.; Green-Church, K.; Nagaraja, H.; Birmingham, D.J.; Yu, C.-Y.; et al. Biomarkers of lupus nephritis determined by serial urine proteomics. Kidney Int. 2008, 74, 799–807. [Google Scholar] [CrossRef] [Green Version]
- Aggarwal, A.; Gupta, R.; Negi, V.S.; Rajasekhar, L.; Misra, R.; Singh, P.; Chaturvedi, V.; Sinha, S. Urinary haptoglobin, alpha-1 anti-chymotrypsin and retinol binding protein identified by proteomics as potential biomarkers for lupus nephritis. Clin. Exp. Immunol. 2017, 188, 254–262. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Turnier, J.L.; Brunner, H.I.; Bennett, M.; Aleed, A.; Gulati, G.; Haffey, W.D.; Thornton, S.; Wagner, M.; Devarajan, P.; Witte, D.; et al. Discovery of SERPINA3 as a candidate urinary biomarker of lupus nephritis activity. Rheumatology 2018, 58, 321–330. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tailliar, M.; Schanstra, J.; Dierckx, T.; Breuil, B.; Hanouna, G.; Charles, N.; Bascands, J.-L.; Dussol, B.; Vazi, A.; Chiche, L.; et al. Urinary Peptides as Potential Non-Invasive Biomarkers for Lupus Nephritis: Results of the Peptidu-LUP Study. J. Clin. Med. 2021, 10, 1690. [Google Scholar] [CrossRef]
- Rao, P.V.; Lu, X.; Standley, M.; Pattee, P.; Neelima, G.; Girisesh, G.; Dakshinamurthy, K.V.; Roberts, C.T., Jr.; Nagalla, S.S. Proteomic identification of urinary biomarkers of diabetic nephropathy. Diabetes Care 2007, 30, 629–637. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rossing, K.; Mischak, H.; Dakna, M.; Zürbig, P.; Novak, J.; Julian, B.A.; Good, D.M.; Coon, J.J.; Tarnow, L.; Rossing, P.; et al. Urinary Proteomics in Diabetes and CKD. J. Am. Soc. Nephrol. 2008, 19, 1283–1290. [Google Scholar] [CrossRef]
- Jin, J.; Gong, J.; Zhao, L.; Li, Y.; Wang, Y.; He, Q. iTRAQ-based comparative proteomics analysis reveals specific urinary biomarkers for various kidney diseases. Biomark. Med. 2020, 14, 839–854. [Google Scholar] [CrossRef]
- Patel, D.N.; Kalia, K. Characterization of low molecular weight urinary proteins at varying time intervals in type 2 diabetes mellitus and diabetic nephropathy patients. Diabetol. Metab. Syndr. 2019, 11, 39. [Google Scholar] [CrossRef] [PubMed]
- Liao, W.-L.; Chang, C.-T.; Chen, C.-C.; Lee, W.-J.; Lin, S.-Y.; Liao, H.-Y.; Wu, C.-M.; Chang, Y.-W.; Chen, C.-J.; Tsai, F.-J. Urinary Proteomics for the Early Diagnosis of Diabetic Nephropathy in Taiwanese Patients. J. Clin. Med. 2018, 7, 483. [Google Scholar] [CrossRef] [Green Version]
- Chen, C.J.; Liao, W.L.; Chang, C.T.; Liao, H.Y.; Tsai, F.J. Urine proteome analysis by C18 plate-matrix-assisted laser desorption/ionization time-of-flight mass spectrometry allows non-invasive differential diagnosis and prediction of diabetic nephropathy. PLoS ONE 2018, 13, e0200945. [Google Scholar] [CrossRef] [Green Version]
- He, T.; Pejchinovski, M.; Mullen, W.; Beige, J.; Mischak, H.; Jankowski, V. Peptides in Plasma, Urine, and Dialysate: Toward Unravelling Renal Peptide Handling. Proteom. Clin. Appl. 2020, 15, e2000029. [Google Scholar] [CrossRef]
- He, T.; Siwy, J.; Metzger, J.; Mullen, W.; Mischak, H.; Schanstra, J.P.; Zurbin, P.; Jankowski, V. Associations of urinary polymeric immunoglobulin receptor peptides in the context of cardiorenal syndrome. Sci. Rep. 2020, 10, 1–7. [Google Scholar]
- Alkhalaf, A.; Zürbig, P.; Bakker, S.J.L.; Bilo, H.J.G.; Cerna, M.; Fischer, C.; Fuchs, S.; Jannsen, N.; Medek, C.; Miskhac, H.; et al. Multicentric validation of proteomic biomarkers in urine specific for diabetic nephropathy. PLoS ONE 2010, 5, e13421. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Currie, G.E.; von Scholten, B.J.; Mary, S.; Guerrero, J.-L.F.; Lindhardt, M.; Reinhard, H.; Jacobsen, P.K.; Mullen, W.; Parving, H.-H.; Mischak, H.; et al. Urinary proteomics for prediction of mortality in patients with type 2 diabetes and microalbuminuria. Cardiovasc. Diabetol. 2018, 17, 1–8. [Google Scholar] [CrossRef]
- Brondani, L.D.A.; Soares, A.A.; Recamonde-Mendoza, M.; Dall’Agnol, A.; Camargo, J.L.; Monteiro, K.M.; Silveiro, S.P. Urinary peptidomics and bioinformatics for the detection of diabetic kidney disease. Sci. Rep. 2020, 10, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Praga, M.; Morales, E.; Herrero, J.C.; Campos, A.P.; Domínguez-Gil, B.; Alegre, R.; Vara, J.; Martínez, M.A. Absence of hypoalbuminemia despite massive proteinuria in focal segmental glomerulosclerosis secondary to hyperfiltration. Am. J. Kidney Dis. 1999, 33, 52–58. [Google Scholar] [CrossRef]
- Rydel, J.J.; Korbet, S.M.; Borok, R.Z.; Schwartz, M.M. Focal segmental glomerular sclerosis in adults: Presentation, course, and response to treatment. Am. J. Kidney Dis. 1995, 25, 534–542. [Google Scholar] [CrossRef]
- D’Agati, V.D.; Fogo, A.B.; Bruijn, J.A.; Jennette, J. Pathologic classification of focal segmental glomerulosclerosis: A working proposal. Am. J. Kidney Dis. 2004, 43, 368–382. [Google Scholar] [CrossRef]
- Rosenberg, A.Z.; Kopp, J.B. Focal Segmental Glomerulosclerosis. Clin. J. Am. Soc. Nephrol. 2017, 12, 502–517. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Savin, V.J.; Sharma, R.; Sharma, M.; McCarthy, E.T.; Swan, S.K.; Ellis, E.; Lovell, H.; Warady, B.; Gunwar, S.; Chonko, A.M.; et al. Circulating Factor Associated with Increased Glomerular Permeability to Albumin in Recurrent Focal Segmental Glomerulosclerosis. N. Engl. J. Med. 1996, 334, 878–883. [Google Scholar] [CrossRef]
- Wei, C.; El Hindi, S.; Li, J.; Fornoni, A.; Goes, N.; Sageshima, J.; Karumanchi, S.A.; Miguel, D.; Yap, H.-K.; Saalem, M.; et al. Circulating urokinase receptor as a cause of focal segmental glomerulosclerosis. Nat. Med. 2011, 17, 952–960. [Google Scholar] [CrossRef] [Green Version]
- Shankland, S.J.; Pollak, M.R. A suPAR circulating factor causes kidney disease. Nat. Med. 2011, 17, 926–927. [Google Scholar] [CrossRef]
- Sharma, M.; Zhou, J.; Gauchat, J.-F.; Sharma, R.; McCarthy, E.T.; Srivastava, T.; Savin, V.J. Janus kinase 2/signal transducer and activator of transcription 3 inhibitors attenuate the effect of cardiotrophin-like cytokine factor 1 and human focal segmental glomerulosclerosis serum on glomerular filtration barrier. Transl. Res. 2015, 166, 384–398. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Delville, M.; Sigdel, T.K.; Wei, C.; Li, J.; Hsieh, S.-C.; Fornoni, A.; Burke, G.W.; Bruneval, P.; Naesens, M.; Jackson, A.; et al. A circulating antibody panel for pretransplant prediction of FSGS recurrence after kidney transplantation. Sci. Transl. Med. 2014, 6, 256ra136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yu, C.-C.; Fornoni, A.; Weins, A.; Hakroush, S.; Maiguel, D.; Sageshima, J.; Chen, L.; Ciancio, G.; Faridi, M.H.; Behr, D.; et al. Abatacept in B7-1–Positive Proteinuric Kidney Disease. N. Engl. J. Med. 2013, 369, 2416–2423. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Korbet, S.M.; Schwartz, M.M.; Lewis, E.J. Primary Focal Segmental Glomerulosclerosis: Clinical Course and Response to Therapy. Am. J. Kidney Dis. 1994, 23, 773–783. [Google Scholar] [CrossRef]
- Wehrmann, M.; Bohle, A.; Held, H.; Schumm, G.; Kendziorra, H.; Pressler, H. Long-term prognosis of focal sclerosing glomerulonephritis. An analysis of 250 cases with particular regard to tubulointerstitial changes. Clin. Nephrol. 1990, 33, 115–122. [Google Scholar] [PubMed]
- Merchant, M.L.; Barati, M.T.; Caster, D.J.; Hata, J.L.; Hobeika, L.; Coventry, S.; Brier, M.E.; Wilkey, D.W.; Li, M.; Rood, I.M.; et al. Proteomic Analysis Identifies Distinct Glomerular Extracellular Matrix in Collapsing Focal Segmental Glomerulosclerosis. J. Am. Soc. Nephrol. 2020, 31, 1883–1904. [Google Scholar] [CrossRef]
- Schwaller, B. Calretinin: From a “simple” Ca2+ buffer to a multifunctional protein implicated in many biological processes. Front. Neuroanat. 2014, 8, 3. [Google Scholar] [CrossRef] [Green Version]
- Beeken, M.; Lindenmeyer, M.T.; Blattner, S.M.; Radón, V.; Oh, J.; Meyer, T.N.; Hildebrand, D.; Schlüter, H.; Reinicke, A.T.; Knop, J.-H.; et al. Alterations in the Ubiquitin Proteasome System in Persistent but Not Reversible Proteinuric Diseases. J. Am. Soc. Nephrol. 2014, 25, 2511–2525. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meyer-Schwesinger, C.; Meyer, T.; Münster, S.; Klug, P.; Saleem, M.; Helmchen, U.; Stahl, R. A new role for the neuronal ubiquitin C-terminal hydrolase-L1 (UCH-L1) in podocyte process formation and podocyte injury in human glomerulopathies. J. Pathol. 2009, 217, 452–464. [Google Scholar] [CrossRef]
- Meyer-Schwesinger, C.; Meyer, T.N.; Sievert, H.; Hoxha, E.; Sachs, M.; Klupp, E.M.; Munster, S.; Balabanov, S.; Carrier, L.; Helmchen, U.; et al. Ubiquitin C-terminal hydro-lase-l1 activity induces polyubiquitin accumulation in podocytes and increases proteinuria in rat membranous nephropathy. Am. J. Pathol. 2011, 178, 2044–2057. [Google Scholar] [CrossRef] [Green Version]
- Moroni, G.; Ponticelli, C. Secondary Membranous Nephropathy. A Narrative Review. Front. Med. 2020, 7. [Google Scholar] [CrossRef]
- Ligabue, G.; Magistroni, R.; Cantu’, M.; Genovese, F.; Lupo, V.; Cavazzini, F.; Furci, L.; Cappelli, F. Identification and Characterization of New Proteins in Podocyte Dysfunction of Membranous Nephropathy by Proteomic Analysis of Renal Biopsy. Curr. Pharmacogen. Person. Med. 2013, 11, 42–52. [Google Scholar]
- Dieplinger, H.; Dieplinger, B. Afamin—A pleiotropic glycoprotein involved in various disease states. Clin. Chim. Acta 2015, 446, 105–110. [Google Scholar] [CrossRef] [Green Version]
- McGrogan, A.; Franssen, C.F.; de Vries, C.S. The incidence of primary glomerulonephritis worldwide: A systematic review of the literature. Nephrol. Dial. Transplant. 2011, 26, 414–430. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zaza, G.; Bernich, P.; Lupo, A.; Triveneto’ Register of Renal Biopsies (TVRRB). Incidence of primary glomerulonephritis in a large North-Eastern Italian area: A 13-year renal biopsy study. Nephrol. Dial. Transplant. 2013, 28, 367–372. [Google Scholar] [CrossRef] [PubMed]
- Maixnerova, D.; Bauerova, L.; Skibova, J.; Rysava, R.; Reiterova, J.; Merta, M.; Honsova, E.; Tesar, V. The retrospective analysis of 343 Czech patients with IgA nephropathy—One centre experience. Nephrol. Dial. Transplant. 2012, 27, 1492–1498. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suzuki, H.; Kiryluk, K.; Novak, J.; Moldoveanu, Z.; Herr, A.; Renfrow, M.B.; Wyatt, R.; Scolari, F.; Mestecky, J.; Gharavi, A.G.; et al. The Pathophysiology of IgA Nephropathy. J. Am. Soc. Nephrol. 2011, 22, 1795–1803. [Google Scholar] [CrossRef] [Green Version]
- Zhang, W.; Lachmann, P.J. Glycosylation of IgA is required for optimal activation of the alternative complement pathway by immune complexes. Immunology 1994, 81, 137–141. [Google Scholar]
- Moura, I.C.; Arcos-Fajardo, M.; Gdoura, A.; Leroy, V.; Sadaka, C.; Mahlaoui, N.; Yves, L.; Vrtovnski, F.; Haddad, E.; Benhamou, M.; et al. Engagement of transferrin receptor by polymeric IgA1: Evidence for a positive feedback loop involving increased receptor expression and mesangial cell proliferation in IgA nephropathy. JASN 2005, 16, 2667–2676. [Google Scholar] [CrossRef]
- Majd, T.M.; Kalantari, S.; Shahraki, H.R.; Nafar, M.; Almasi, A.; Samavat, S.; Parvin, M.; Hashemian, A. Application of sparse linear discriminant analysis and elastic net for diagnosis of IgA nephropathy: Statistical and biological viewpoints. Iran. Biomed. J. 2018, 22, 374–384. [Google Scholar]
- Johnson, R.J.; Feehally, J.; Floege, J. Comprehensive Clinical Nephrology; Elsevier Health Sciences: Amsterdam, The Netherlands, 2019. [Google Scholar]
- Guillén-Gómez, E.; de Quixano, B.B.; Ferrer, S.; Brotons, C.; Knepper, M.A.; Carrascal, M.; Abian, J.; Mas, J.M.; Calero, F.; Ballarín, J.A.; et al. Urinary Proteome Analysis Identified Neprilysin and VCAM as Proteins Involved in Diabetic Nephropathy. J. Diabetes Res. 2018, 2018, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Ahn, H.-S.; Kim, J.H.; Jeong, H.; Yu, J.; Yeom, J.; Song, S.H.; Kim, S.S.; Kim, I.J.; Kim, K. Differential Urinary Proteome Analysis for Predicting Prognosis in Type 2 Diabetes Patients with and without Renal Dysfunction. Int. J. Mol. Sci. 2020, 21, 4236. [Google Scholar] [CrossRef]
- Musa, R.; Brent, L.H.; Qurie, A. Lupus Nephritis; Stat Pearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- 109Devuyst, O.; Bochud, M. Uromodulin, kidney function, cardiovascular disease, and mortality. Kidney Int. 2015, 88, 944–946. [Google Scholar] [CrossRef] [Green Version]
- Trudu, M.; Janas, S.; Lanzani, C.; Debaix, H.; Schaeffer, C.; Ikehata, M.; Citterio, L.; Demaretz, C.; Trevisani, F.; Ristango, G.; et al. Common noncoding UMOD gene variants induce salt-sensitive hypertension and kidney damage by increasing uromodulin expression. Nat. Med. 2013, 19, 1655–1660. [Google Scholar] [CrossRef] [PubMed]
- Jamin, A.; Berthelot, L.; Couderc, A.; Chemouny, J.M.; Boedec, E.; Dehoux, L.; Abbad, L.; Dossier, C.; Daugas, E.; Monteiro, R.; et al. Autoantibodies against podocytic UCHL1 are associated with idiopathic nephrotic syndrome relapses and induce proteinuria in mice. J. Autoimmun. 2018, 89, 149–161. [Google Scholar] [CrossRef]
- Bruschi, M.; Catarsi, P.; Candiano, G.; Pia, M.; Rastaldi, M.P.; Musante, L.; Scolari, F.; Artero, M.; Carraro, M.; Carrea, A.; et al. Apolipoprotein E in idiopathic nephrotic syndrome and focal segmental glomerulosclerosis. Kidney Int. 2003, 63, 686–695. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marek-Bukowiec, K.; Konieczny, A.; Ratajczyk, K.; Macur, K.; Czaplewska, P.; Czyżewska-Buczyńska, A.; Kowal, P.; Witkiewicz, W. The value of urinary RBP4 in the diagnosis of FSGS and other renal diseases. Trends Biomed. Res. 2020, 3. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chebotareva, N.; Vinogradov, A.; McDonnell, V.; Zakharova, N.V.; Indeykina, M.I.; Moiseev, S.; Nikolaev, E.N.; Kononikhin, A.S. Urinary Protein and Peptide Markers in Chronic Kidney Disease. Int. J. Mol. Sci. 2021, 22, 12123. https://doi.org/10.3390/ijms222212123
Chebotareva N, Vinogradov A, McDonnell V, Zakharova NV, Indeykina MI, Moiseev S, Nikolaev EN, Kononikhin AS. Urinary Protein and Peptide Markers in Chronic Kidney Disease. International Journal of Molecular Sciences. 2021; 22(22):12123. https://doi.org/10.3390/ijms222212123
Chicago/Turabian StyleChebotareva, Natalia, Anatoliy Vinogradov, Valerie McDonnell, Natalia V. Zakharova, Maria I. Indeykina, Sergey Moiseev, Evgeny N. Nikolaev, and Alexey S. Kononikhin. 2021. "Urinary Protein and Peptide Markers in Chronic Kidney Disease" International Journal of Molecular Sciences 22, no. 22: 12123. https://doi.org/10.3390/ijms222212123
APA StyleChebotareva, N., Vinogradov, A., McDonnell, V., Zakharova, N. V., Indeykina, M. I., Moiseev, S., Nikolaev, E. N., & Kononikhin, A. S. (2021). Urinary Protein and Peptide Markers in Chronic Kidney Disease. International Journal of Molecular Sciences, 22(22), 12123. https://doi.org/10.3390/ijms222212123







