Abstract
The challenges in the diagnosis, prognosis, and monitoring of Gaucher disease (GD), an autosomal recessive inborn error of glycosphingolipid metabolism, can negatively impact clinical outcomes. This systematic literature review evaluated the value of glucosylsphingosine (lyso-Gb1), as the most reliable biomarker currently available for the diagnosis, prognosis, and disease/treatment monitoring of patients with GD. Literature searches were conducted using MEDLINE, Embase, PubMed, ScienceOpen, Science.gov, Biological Abstracts, and Sci-Hub to identify original research articles relevant to lyso-Gb1 and GD published before March 2019. Seventy-four articles met the inclusion criteria, encompassing 56 related to pathology and 21 related to clinical biomarkers. Evidence for lyso-Gb1 as a pathogenic mediator of GD was unequivocal, although its precise role requires further elucidation. Lyso-Gb1 was deemed a statistically reliable diagnostic and pharmacodynamic biomarker in GD. Evidence supports lyso-Gb1 as a disease-monitoring biomarker for GD, and some evidence supports lyso-Gb1 as a prognostic biomarker, but further study is required. Lyso-Gb1 meets the criteria for a biomarker as it is easily accessible and reliably quantifiable in plasma and dried blood spots, enables the elucidation of GD molecular pathogenesis, is diagnostically valuable, and reflects therapeutic responses. Evidentiary standards appropriate for verifying inter-laboratory lyso-Gb1 concentrations in plasma and in other anatomical sites are needed.
1. Introduction
Gaucher disease (GD) is an autosomal recessive disease of glycosphingolipid metabolism caused by a functional deficiency of the lysosomal enzyme β-glucocerebrosidase (glucosylceramidase (GBA); EC 3.2.1.45), resulting from variants in the GBA1 gene [1,2]. GD is one of the more common lysosomal storage disorders, occurring with an incidence of approximately 1 in 50,000 to 100,000 live births [3,4], although genetic studies indicate a homozygote frequency of ∼1:850 in the Ashkenazi Jewish population [5].
GBA deficiency results in the progressive accumulation of the substrate glucosylceramide (Gb1), along with a build-up of related glycosphingolipids almost exclusively in cells of the mononuclear phagocyte (reticulo-endothelial) system [6,7]. These transform into Gaucher cells, which have a distinct macrophage phenotype with a characteristic morphology and are metabolically active and alternatively activated [8]. Although GD presents as a continuum of phenotypes, the disease is typically categorized into three main types. Type 1 GD (OMIM #230800), the non-neuronopathic and most prevalent variant among Caucasians, is a multisystem inflammatory disorder most often characterized by major liver, spleen, bone, and hematological pathology [1,9]. Lung involvement, pulmonary hypertension, and renal involvement are rarer presentations [1]. Type 2 GD (OMIM #230900) is the acute neuronopathic variant, occurring in very young children, and type 3 GD (OMIM #231000) is a subacute neuronopathic variant that tends to manifest neurologically in childhood or adolescence [1].
One of the challenges in the care of patients with GD is the development of biomarkers as validated tools that aid diagnosis, prognosis, follow-up, treatment decisions, and pathophysiologic understanding [6,10,11]. A biomarker is defined by the National Institutes of Health (NIH) Biomarkers Definitions Working Group as “a characteristic that is objectively measured and evaluated as an indicator of normal biological processes, pathogenic processes, or pharmacologic responses to a therapeutic intervention” [12]. In the era of newborn screening for GD, the use of a reliable biomarker in combination with testing for GBA activity has the potential to reduce the false positive rate and inform decisions about when to start therapy. Patients with GD require continual monitoring and follow-up. Ideally, a real-time pharmacodynamic biomarker with the capacity to identify non-responses could effect changes in management (e.g., dose adaptation) promptly, such that disease progression and organ damage could be avoided.
Selecting appropriate candidate biomarkers has been hampered by the complexity of this monogenetic disorder, in which modifier genes, epigenetics, and external factors give rise to vast clinical and biochemical heterogeneity [6,13,14,15,16,17]. This phenomenon partly explains why there are such poor correlations between the GBA genotype and residual GBA activity as a diagnostic and prognostic tool [6]. Historical plasma biomarkers for disease monitoring and evaluation of treatment (i.e., tartrate-resistant acid phosphatase, angiotensin-converting enzyme, ferritin, and alkaline phosphatase) are not specific to GD, are only elevated moderately in patients with GD relative to controls and are influenced by other factors [18,19,20,21,22,23].
The utility of more widely used plasma biomarkers is also limited. The hydrolase chitotriosidase and the chemokine (C-C motif) ligand 18 (CCL18) are secreted by activated macrophages, including Gaucher cells [23,24], and are thus indicative of overall Gaucher cell burden. Although chitotriosidase and CCL18 are elevated in patients with GD relative to healthy controls and decrease during disease-specific treatment [22,23,24,25,26,27,28], neither biomarker is central to disease pathophysiology [24]. Furthermore, chitotriosidase and CCL18 are not specific for GD [24,29] and one in 20 individuals are entirely deficient in chitotriosidase activity owing to homozygosity for the 24-base-pair duplication in the CHIT1 gene [30].
Over the last half-century, there has been ongoing focus on the occurrence of the sphingoid base in the primary lysosomal storage lipids as mediators of disease [6,11,31]. Gaucher cells are laden with lipids and are known to secrete an array of macromolecules into the local environment they infiltrate [32]. The presence of Gaucher cells along with exposure of tissue to their secretome is thought to partly explain the multifaceted characteristics of the disease [32]. In GD, there is evidence that elevated levels of the lysosomal storage product and sphingolipid, glucosylsphingosine (lyso-Gb1), a direct metabolite of Gb1, are pathogenic to cells [6,7,33].
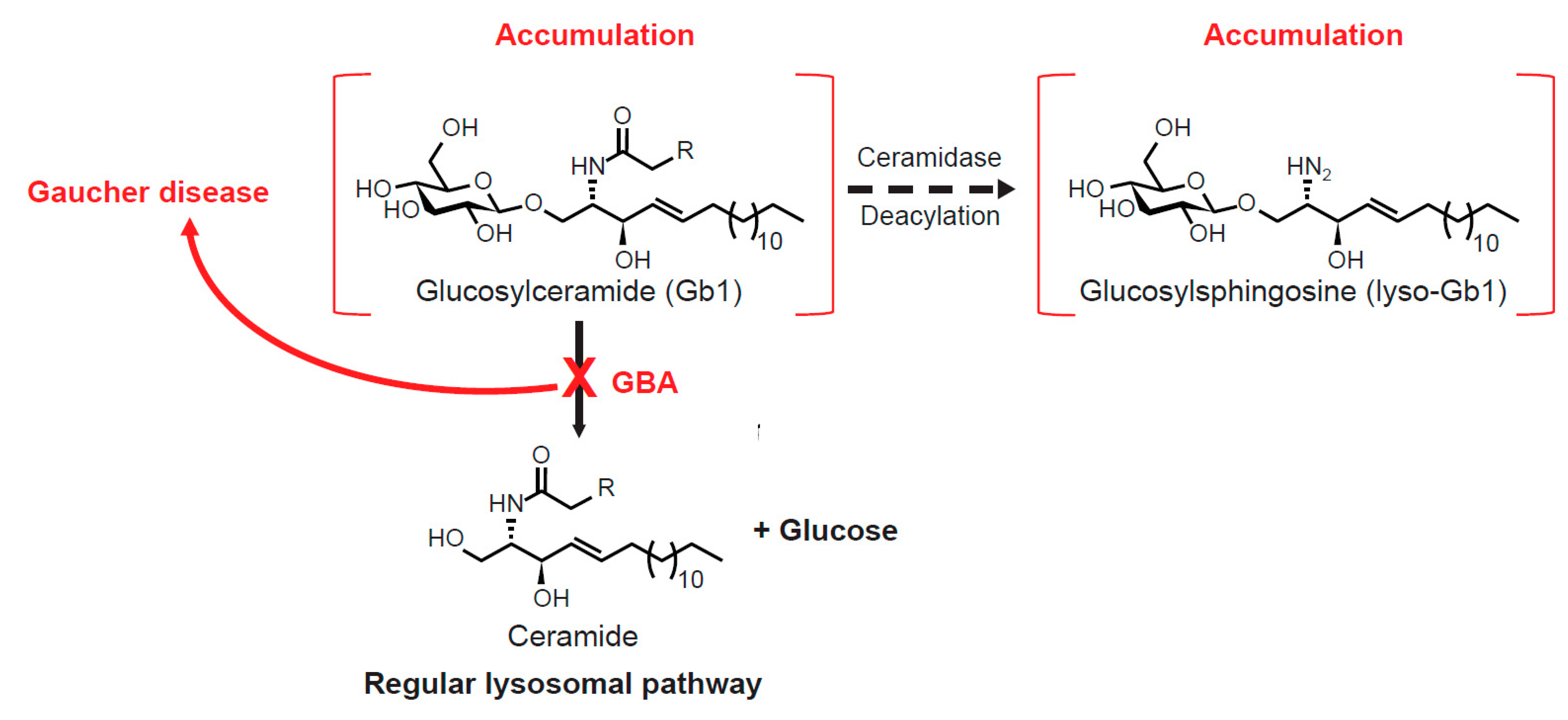
1.1. Gb1 Metabolism and Lyso-Gb1
There are at least three adaptations in Gb1 metabolism that occur during GBA deficiency—namely, the increased anabolism of Gb1 to gangliosides, excessive transglycosylation by cytosol-faced retaining β-glucosidase GBA2, and the active deacylation of Gb1 by acid ceramidase to lyso-Gb1 (the latter pathway is illustrated in Figure 1) [7]. The differential activation of these pathways may account, at least in part, for the inconsistencies observed in the translation of the GBA genotype, lipid storage deposition, and GD phenotype [6]. Variable alterations in lipid metabolism secondary to Gb1 (and lyso-Gb1) accumulation may also induce multiple pathologies reflected in phenotypic heterogeneity [34].
Figure 1.
Catabolic route of glycosphingolipid generation in Gaucher disease [7].
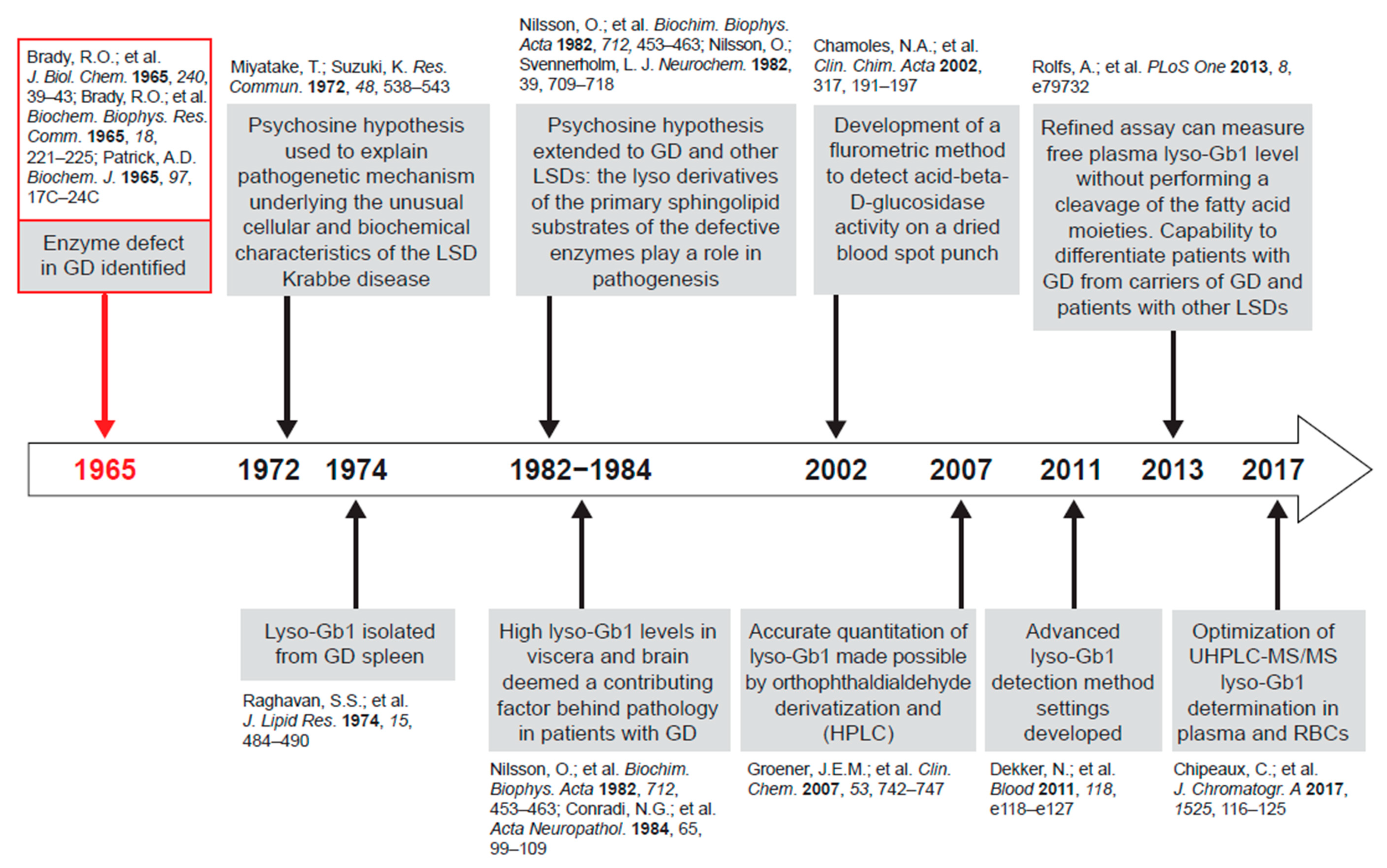
Lyso-Gb1, being more hydrophilic than Gb1, has physicochemical characteristics likely permitting egress from the lysosomal system into the cytoplasm and extracellular space [6]. Results of studies across different research settings over the last 50 years implicate the acid ceramidase pathway in GD because supraphysiological lyso-Gb1 concentrations are present at specific anatomical sites in affected patients and in animal models of GD (Figure 2) [6,7,11]. Furthermore, elevated lyso-Gb1 is associated with the development of GD pathology [6].
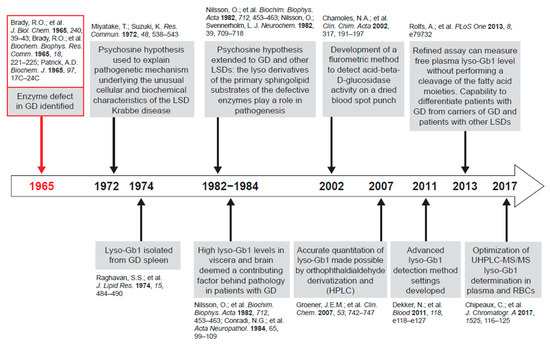
Figure 2.
Research milestones culminating in glucosylsphingosine (lyso-Gb1) as a focus of biomarker research.
A close examination of lyso-Gb1 as a pathogenic metabolite in GD was made possible in 2007 when the quantitation of lyso-Gb1 in biological samples was significantly improved by orthophthaldialdehyde derivatization and high-performance liquid chromatography [35]. Further improvement to the technique was achieved by the development of a liquid chromatography tandem mass spectrometry (LC/MS/MS) method using an identical radiolabeled Gb1 standard [7]. The validation and clinical utility of this method was demonstrated in a prospective observational study of a cohort of patients with type 1 GD and controls [33].
1.2. Systematic Literature Review Objectives
In light of recent research efforts in this area, we undertook what we believe is the first systematic review of the published literature to report on lyso-Gb1 as a potential biomarker for diagnosis, prognosis, and disease/treatment monitoring. The review scrutinizes the role of lyso-Gb1 in GD pathophysiology and as a bona fide biomarker that has a central role in this process.
2. Results
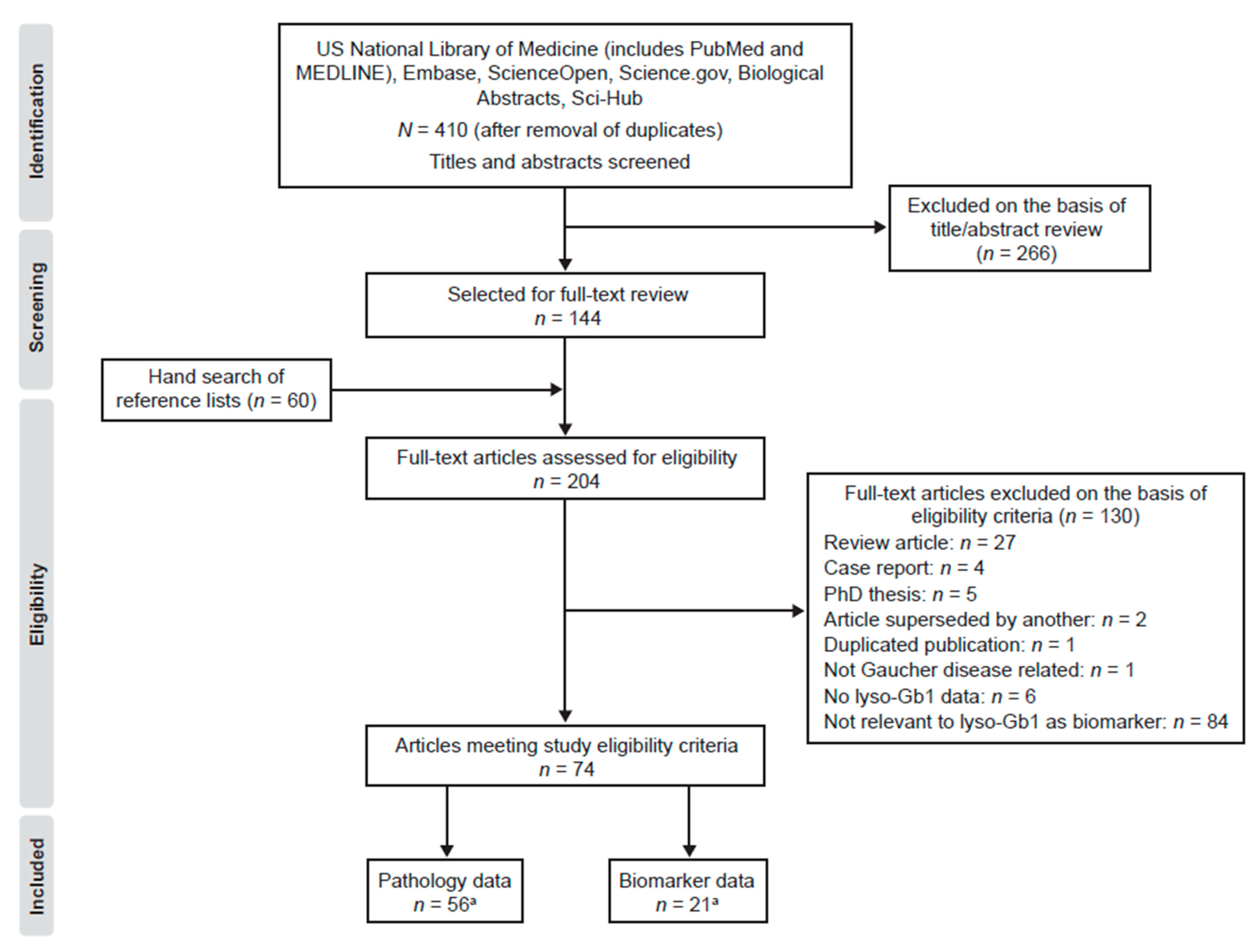
2.1. Search Results
The literature searches on lyso-Gb1 and GD identified 410 articles (Figure 3). During title and abstract screening, 266 articles were excluded according to study exclusion criteria. One hundred and forty-four articles were retrieved in full text, and an additional 60 articles meeting inclusion criteria were identified from hand searches of reference lists from full text articles. Of the 204 articles that were reviewed in full text, 130 were excluded, primarily owing to article type or for their lack of relevance to lyso-Gb1 as a biomarker for GD. Thus, 74 articles met the study eligibility criteria and were included in the review. Of these, one was a randomized clinical trial, one was a pooled analysis of phase III trials, 29 were non-randomized clinical trials or observational studies, and 48 were preclinical studies (five publications reported both preclinical and clinical data).
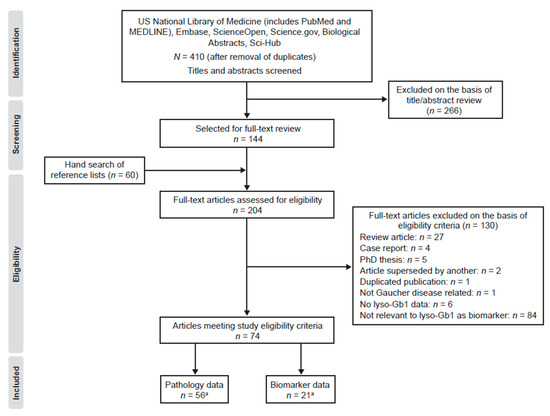
Figure 3.
Literature identification and study selection process for publications reporting on glucosylsphingosine (lyso-Gb1) in Gaucher disease (PRISMA flowchart). a: Three articles reported on roles for lyso-Gb1 in pathophysiology and as a biomarker [26,45,53].
2.2. Quality Assessment
Using the NICE STA method, risk of bias in the sole randomized controlled trial was deemed low, although bias regarding the allocation concealment process and between-group baseline similarities was unclear (Table S1) [36]. Thirty non-randomized clinical trials and observational studies with full-study reporting were assessed using the Newcastle–Ottawa scoring tool [3,26,33,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63], of which 19 were deemed to have a high risk of bias (score 0–3; Table S2). Thirty-two animal studies were assessed using the SYRCLE risk of bias tool [45,53,58,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92]; 20 were considered low-risk, nine high-risk, and the level of bias was unclear in the remaining three studies (Table S3). Other preclinical studies could not be quality assessed owing to a lack of suitable validated tools.
2.3. Pathology
Of the 74 articles included, 56 articles pertained to lyso-Gb1 and GD pathology. They encompassed (in a non-mutually exclusive manner) ten clinical (autopsy) studies [54,55,56,57,58,59,61,62,63,93] and 48 studies reporting preclinical data (19 studies reporting in vitro data and 32 studies reporting in vivo data) [26,45,53,58,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,94,95,96,97,98,99,100,101,102,103,104,105,106,107].
2.3.1. Accumulation of Lyso-Gb1 in Gaucher Disease
Evidence for lyso-Gb1 accumulation consistent with the pathology of GD was found in all ten autopsy studies (Table 1) [54,55,56,57,58,59,61,62,63,93]. Large quantities of lyso-Gb1 were found in the spleen and liver of deceased patients with GD [54,55,93] and lyso-Gb1 had accumulated in the cerebrum and cerebellar cortices of patients with types 2 and 3 GD with severe neurodegeneration [56,57,58,59,61,62,63]. Elevated lyso-Gb1 was not present in one patient with non-neuronopathic GD [57,61]; however, brain lyso-Gb1 was found in large amounts in the cerebellar cortex of severely affected patients with type 1 GD [54]. Lyso-Gb1 was detected in the brain, liver, and spleen tissue of human fetuses with type 2 GD [58].

Table 1.
Autopsy and biopsy studies reporting on lyso-Gb1 levels in Gaucher disease (GD).
Seven of eight in vitro studies provided evidence for a role of lyso-Gb1 accumulation in GD (Table S4). In cultured human cells collected from patients with types 1 and 2 GD, intracellular lyso-Gb1 was substantially higher than in cells from healthy control subjects [26,94,103,108]. These observations were recapitulated when control cells were exposed to conduritol B epoxide (CBE) [26,99,103], a specific GBA inhibitor, and reversed when Gaucher cells were exposed to non-inhibitory chaperones of GBA or acid ceramidase inhibition and CBE removal [26,94,108]. Taken together, these findings confirm the intralysosomal conversion of accumulating Gb1 to lyso-Gb1 [26]. A human in vitro study that reported normal lyso-Gb1 concentrations and lyso-Gb1 hydrolysis in human fibroblasts isolated from patients with types 1, 2, and 3 GD was rationalized by a relatively high residual activity of GBA versus that found in other cells [99]. Intracellular lyso-Gb1 also accumulated in GBA knockout mice models and in newborn neural cells from a type 3 GD mouse model in the presence of CBE [84,101,102].
Table S5 shows that all 31 in vivo studies of experimental GD provided evidence of lyso-Gb1 accumulation, with eight studies citing a reduction in lyso-Gb1 after exposure to GBA or promoters of GBA expression [66,89], or a removal of factors promoting the inhibition of GBA expression [76,79,81,82,90,92].
In all five pharmacologically induced GD murine models, lyso-Gb1 was significantly elevated in the brain after exposure to the GBA inhibitor CBE [64,72,76,81,85], and in the liver and spleen of one model with cyclophellitol [64]. However, these agents may have effects on additional targets: both cyclophellitol and CBE have been shown to inhibit GBA2 as well as GBA, although CBE only at significantly higher concentrations than those used for GBA [109,110].
In type 1 GD murine models, lyso-Gb1 was elevated in the spleen and liver [45,66,71,77,80,92], blood [79,80], and bone [66], but not brain. Lyso-Gb1 declined after mice were exposed to eliglustat, a potent and selective inhibitor of glucosylceramide synthase [79]. Lyso-Gb1 was also significantly decreased in the bone marrow, spleen, and liver of mice with an induced deletion in the Gba genes (Mx1-Cre+ Gbaflox/flox) treated with therapeutic vectors containing the Gba gene, relative to control mice [66].
Lyso-Gb1 accumulation was observed in the brain [53,65,67,68,69,70,72,73,76,82,83,84,85,86,88,89,90,91,111], viscera [65,73,86,91], and blood [111], but not bone, and in a wide range of neuronopathic GD murine models and one ovine model. Although murine models are highly economical, lamb brain is considered more translationally relevant to the human brain as both are gyrencephalic and have similar anatomy and physiological vital signs. In a newborn lamb model of type 2 GD harboring a pathogenic C381Y mutation that corresponds to the same mutation in humans with a similar clinical outcome, lyso-Gb1 concentrations were several orders of magnitude higher in the brain, cervical spinal cord, spleen, and liver than in corresponding samples from wild-type and heterozygous lambs [73].
2.3.2. Relationship between Lyso-Gb1 and GD Pathology
GD pathology is marked by the presence of Gaucher cells, neuropathology, and chronic low-grade inflammation [112]. Evidence for lyso-Gb1 as a pathogenic mediator in GD based on an association with these features was found in all 16 in vitro studies (Table 2) and 14 of 17 in vivo studies (Table 3). With the exception of one in vivo study [45], the effects of lyso-Gb1 on cells and tissues were always damaging, ranging from moderate to high cytotoxicity depending on lyso-Gb1 concentration and the type of cell or tissue under study. It is important to bear in mind that in preclinical studies examining the effects of exogenous lyso-Gb1, concentrations of lyso-Gb1 used were lower than the elevated intracellular lyso-Gb1 seen in some animal models and patients with GD.

Table 2.
In vitro studies reporting association between lyso-Gb1 and GD pathology.

Table 3.
In vivo studies reporting association between lyso-Gb1 and GD pathology.
From a mechanistic viewpoint at the cellular level, lyso-Gb1 evoked HEK293 and RH7777 cells to form globoid cells (multinucleated macrophages) [106], a common manifestation of GD, via the activation of the G protein–coupled receptor T cell-associated gene 8 (TDAG8). Binding of TDAG8 by lyso-Gb1 promoted inflammation via the activation of phospholipase A2 [104]. Immortalized GBA−/− neurons had marked accumulation of Gb1 and lyso-Gb1, enlarged lysosomes, and an impaired ATP-dependent calcium-influx response [101]. A wide range of in vitro experiments has also demonstrated that lyso-Gb1 is cytotoxic to some cell types and pro-inflammatory in others, is damaging to specific neurons, impairs cell fission during cytokinesis, and interferes with osteoblasts, immune regulation, and signal transduction (Table 2). Exogenous lyso-Gb1 induced hemolysis and was cytotoxic towards cultured human cholinergic neurons, human umbilical vein endothelial cells, and 3T3 and PC12 cell lines [64,83,100,107]. Lyso-Gb1 toxicity towards fibroblasts and neural crest-derived neoplastic cells in vitro occurred at a similar concentration to that which it accumulates in vivo [64].
Over the past two decades, it has become apparent that there is an association between GD and Parkinson disease, with both diseases sharing neuropathological features [10]. Lyso-Gb1 promoted not only the elevation of α-synuclein levels in neurons from patients with type 2 GD or Parkinsonism but also the formation of toxic oligomeric α-synuclein aggregates [84,102,108], a hallmark of Parkinson disease [10].
Results from 14 of 17 experimental animal models of GD have shown that lyso-Gb1 is associated with: pro-inflammatory effects [75]; hepatosplenomegaly [67,74,75,77]; poor hematologic [75,77], skeletal [77], and neurologic outcomes [68,76,82,83]; B-cell malignancy [79]; death [89,90] (Table 3). Two in vivo studies did not evaluate the effect of lyso-Gb1 in specific aspects of GD pathology [45,78].
In the CBE-induced murine GD model, high levels of lyso-Gb1 alone or in combination with Gb1 were accompanied by brain α-synuclein aggregation, neurodegeneration, microglia and complement C1q activation, and premature death [81,85], with gliosis and neurobehavioral deficits reversed by the specific glucosylceramide synthase inhibitor venglustat (ibiglustat) [76].
In a lyso-Gb1-induced GD model reflecting lyso-Gb1 levels observed in moderate to severely affected patients with untreated GD, decreased hemoglobin (Hb) and hematocrit was observed along with hepatosplenomegaly [75]. In addition, there was a strong increase in CD68 immunoreactivity in the spleen sections of lyso-Gb1-treated mice when compared with vehicle controls [75].
Most pathologic associations of lyso-Gb1 in the conditional type 1 GD model were incidental, although two studies using the GBA1 knockout mouse model (Mx1-Cre+) detected a correlation between splenic lyso-Gb1 levels and splenomegaly [74,77]. Interestingly, this clinical phenotype, including the bone pathology, was rescued by GBA2 knockout despite elevated Gb1 and lyso-Gb1 levels [45]. These data implicate lyso-Gb1 as a source of sphingosine generation in aspects of GD pathology.
Similar to the type 1 GD models, most associations of lyso-Gb1 with pathology in the neuronopathic variants were incidental (Table 3). In the two correlational analyses, there was no association detected between brain concentrations of lyso-Gb1 and neuronal loss in the neuronopathic GD murine GBAflox/flox; nestin-Cre model [70], whereas an intracerebroventricular administration of recombinant human GBA resulted in dose-dependent reductions in lyso-Gb1 in the brain samples of neonatal K-14Cre+ GBAlnl/lnl mice and improved survival [89].
Preclinical data and evidence from 20 patients with GD showed that the frequency of lyso-Gb1-specific T cells correlates with disease activity and therapeutic response [113].
Excessive lyso-Gb1 has a role in dysregulating humoral immunity by promoting chronic B-cell activation and gammopathy, which can evolve into multiple myeloma, a relatively common blood cancer in patients with GD [113].
2.4. Lyso-Gb1 as a Clinical Biomarker
Of the 74 articles included in the analysis, 21 reported data that pertained to plasma lyso-Gb1 as a biomarker in GD.
2.4.1. Diagnosis
Eleven studies provided information relevant to the diagnosis of GD [3,26,33,38,40,41,44,46,47,49,50]. Normally, lyso-Gb1 is undetectable or found at trace levels in plasma (i.e., <4.9 ng/mL (10.61 nmol/L)) and tissue [39,114]. Data from five prospective observational studies indicated consistently that lyso-Gb1 in plasma and red blood cell (RBC) membranes were higher in untreated patients with GD than in control subjects (Table 4) [3,26,40,44,46]. In addition, findings from an open-label pilot clinical trial showed that lyso-Gb1 in cerebrospinal fluid were below the lower limit of quantification (10.0 pg/mL (21.66 pmol/mL)) in all control subjects but were elevated in patients with neuronopathic GD [49]. An additional five observational studies were specifically designed to assess the value of lyso-Gb1 as a diagnostic biomarker (Table 4) [33,38,41,47,50]. All utilized sensitive LC/MS/MS techniques for the detection and quantification of lyso-Gb1 in plasma.

Table 4.
Cross-sectional, observational studies reporting on lyso-Gb1, as measured by liquid chromatography techniques, in subjects with and without GD.
Two groups, Dekker et al. [33] and Rolfs et al. [50] reported on the use of lyso-Gb1 as a biomarker for patients with GD. Dekker et al. prospectively recruited 64 patients with GD, 34 obligate carriers of GD, and 28 healthy controls from centers in the Netherlands, United States, and Poland. Most of the patients with GD were compound heterozygotes for N370S (c.1226A > G) and one other GBA mutation, with the exception of five patients homozygous for N370S. Fourteen homozygotes for the N370S mutation were also studied, two patients with saposin C deficiency, and three patients with type 3 GD [33]. Prominent increases in lyso-Gb1 (300-fold) were detected in the plasma of symptomatic patients with type 1 GD versus healthy controls. The extent of this abnormality was emphasized by the plasma Gb1 level, which was only three-fold higher in these patients with type 1 GD [33].
Rolfs et al. retrospectively analyzed non-Jewish Caucasian patients from a single center in Germany [50]. The marker was specific for GD, as carriers and patients with other lysosomal storage disorders did not show signs of elevated lyso-Gb1. A plasma lyso-Gb1 threshold of 12 ng/mL (25.99 nmol/mL) differentiated between patients with genetically defined GD from healthy probands, patients with other lysosomal storage diseases, and GD carriers, with 100% sensitivity and 100% specificity [50]. The observation was also independent of sex, as male and female patients with GD had similar lyso-Gb1 levels [50].
In a US study, Murugesan et al. prospectively compared plasma lyso-Gb1 in patients with type 1 GD and healthy controls. In this cohort, the investigators found that a lyso-Gb1 cut-off of 4 ng/mL had 100% sensitivity and specificity as a diagnostic tool [47]. The different diagnostic cut-off values for plasma lyso-Gb1 thus reflect the different populations under study and different means of lyso-Gb1 measurement.
Fuller et al. described an accurate, reproducible, robust, and easy-to-perform assay for the determination of plasma lyso-Gb1 concentrations in a routine laboratory setting using N-palmitoyl-d3-lactosyl ceramide as an internal standard [41]. This assay reported a performance of 100% sensitivity and specificity using a lyso-Gb1 cut-off of 4 pmol/mL (1.85 ng/mL).
Chipeaux et al. prospectively recruited 64 patients with GD, 34 obligate carriers of GD, and 28 healthy controls from three centers in France [38]. Plasma lyso-Gb1 (limit of quantification, 0.7 nM) was the only relevant biomarker in both plasma and RBCs for GD diagnosis when compared with Gb1, sphingosine, and sphingosine-1-phosphate [38].
The findings of one additional study showed that it is possible for patients other than those with GD to have high lyso-Gb1 [42]. In patients with action myoclonus-renal failure (AMRF), deficiency of the lysosomal integral membrane protein-2 prevents the cell type-specific trafficking of GBA to lysosomes. GBA is almost absent in the lysosomes of AMRF fibroblasts, but is present in white blood cells. As a result, AMRF macrophages can still produce lyso-Gb1, but patients with AMRF do not present with Gaucher cells, and do not have elevated macrophage markers such as chitotriosidase [42], important factors for consideration in diagnostic assay specificity.
2.4.2. Prognosis
Four studies provided information on lyso-Gb1 as a prognostic biomarker of GD (Table 5) [26,33,39,50].

Table 5.
Overview of studies assessing lyso-Gb1, as measured by liquid chromatography tandem mass spectrometry (LC/MS/MS), as a prognostic biomarker in GD.
In a prospective, case-control study, modest increases in plasma lyso-Gb1 were evident in mildly affected patients [33]. Plasma lyso-Gb1 concentration was correlated with the genotype (N370S GBA homozygous patients only), liver volume, and bone marrow fat fraction but not correlated with macrophage inflammatory protein 1-β, the presence of a spleen, skeletal complications, osteocalcin, and procollagen type 1 N propeptide in this study [33].
In a retrospective, case-control study, plasma lyso-Gb1 appeared to reflect the severity of the individual genetic variant [50]. Patients with N370S displayed lower concentrations of lyso-Gb1 than those with L444P (c.1448T > C), which is known to be more frequent in patients with a more fatal course of disease [50,115]. An exploratory pooled analysis of phase III clinical trials revealed that mean plasma lyso-Gb1 was twice as high for 17 patients with ≥1 allele with the N370S variant (N370S/N370S or N370S/other) than for five patients with non-N370S mutations [39].
Lyso-Gb1 concentrations were also excessive in the cultured fibroblasts of a collodion patient with GD (homozygous for the recombination RecNci allele) with virtually no residual GBA activity versus more modest elevations among patients with type 1 GD and neuronopathic variants [26].
2.4.3. Disease Monitoring/Responsivity to Treatment
In 17 studies, cross-sectional and longitudinal data on lyso-Gb1 in treated and untreated patients with GD were compared [33,36,37,38,39,40,41,43,44,45,47,48,49,50,51,52,53]. Results from 16 of the 17 studies showed that treatment with enzyme replacement therapy (ERT) and substrate reduction therapy (SRT) either alone or in combination produced marked reductions in lyso-Gb1 concentrations in plasma, cerebrospinal fluid (CSF), and urine relative to baseline or control (Table S6). For most patients, a significant reduction in plasma lyso-Gb1 occurred after ERT initiation before levelling off at a lower concentration and increasing when ERT was stopped [39,50]. Similar findings were observed after the initiation of SRT [43]. A retrospective analysis of 25 non-splenectomized patients with GD homozygous for the non-neuronopathic N370S GBA mutation in the GBA1 gene who received low-dose ERT (15 units/kg/month) revealed an exponential decay (Pearson product moment determination coefficient (r2), 0.84) in lyso-Gb1 plasma over 72 months [37]. ERT also lowered lyso-Gb1 content in RBC membranes in a prospective, multicenter, cross-sectional, case-control study of 15 patients with type 1 and neuronopathic GD receiving ERT versus 16 untreated counterparts [40]. A combination of ERT plus ambroxol reduced lyso-Gb1 concentration in CSF by 26% versus baseline in a multicenter open-label pilot study of five patients with neuronopathic GD; concentrations were below the lower limit of quantification (10.0 pg/mL) in all 37 control subjects [49]. However, in all studies, the lyso-Gb1 concentration remained higher than that observed in healthy controls regardless of sample type, and higher than the 4 or 12 ng/mL diagnostic cut-off level for lyso-Gb1 in plasma (Table S6).
Ten of the 17 studies provided different evidence levels of information on lyso-Gb1 as a response biomarker in GD (Table 6) [36,37,38,39,40,43,44,47,49,51]. The results of a prospective, multicenter, cross-sectional, case-control study in treatment-naïve and splenectomized patients with type 1 GD showed that lyso-Gb1 concentrations in plasma (Pearson product moment correlation coefficient (r), –0.83) and RBC membranes (−0.65) correlated inversely with hematocrit [38]. Nine studies were of patients with GD undergoing treatment with ERT, SRT, or ambroxol [36,37,39,40,43,44,47,49,51]. Five of the associations between lyso-Gb1 and clinical outcomes were incidental, albeit with strong temporal and kinetic links, whereas the other five studies demonstrated correlations between lyso-Gb1 and clinical outcomes.

Table 6.
Clinical studies reporting an association between reduced lyso-Gb1 concentration and outcomes.
Regarding incidental findings in the periphery, as plasma lyso-Gb1 decreased upon treatment with either ERT or SRT, platelet counts, Hb, and the bone marrow fat fraction increased, whereas spleen and liver volumes decreased [36,37,43,51]. The lumbar spine T-score also increased to the normal range from baseline as plasma lyso-Gb1 decreased owing to SRT in a phase II multicenter clinical trial [43]. Centrally, as CSF lyso-Gb1 concentrations decreased among five patients with neuronopathic GD receiving ERT plus ambroxol, myoclonus, seizures, and pupillary light reflex dysfunction markedly improved [49].
With respect to correlations, an exploratory pooled analysis of phase III clinical trials of treatment-naïve patients with type 1 GD receiving ERT revealed that there was moderate pairing between decreasing plasma lyso-Gb1 concentrations and increasing platelet counts at weeks 13 (r, −0.530), 25 (r, −0.654), and 53 (r, −0.503), and between decreasing plasma lyso-Gb1 concentrations and decreasing spleen volumes at weeks 25 (r, 0.621) and 101 (r, 0.459) [39]. In the participating treatment-naïve patients, median platelet counts rose during ERT from 63.0 × 109/L at baseline (n = 22) to 146.5 × 109/L at week 209 (n = 10), whereas the median spleen volume decreased from 16.6 MN at baseline (n = 22) to 4.2 multiples of normal at week 209 (n = 12) [39]. The ERT-induced reduction in the plasma lyso-Gb1 concentration anteceded the increase in platelets but not the reduction in spleen volume [39].
In a prospective, single-center, longitudinal, case-control study of 169 patients with type 1 GD receiving ERT or SRT, plasma lyso-Gb1 concentration correlated significantly with indicators of severity of visceral disease: splenic volume (r, 0.27), liver (r, 0.28), and age (r, −0.22) [47].
In a prospective, multicenter, cross-sectional, case-control study, lyso-Gb1 content in RBCs was higher in untreated patients with type 1 and neuronopathic GD (0.69 p/mol per kg protein) than in healthy controls (0.15 p/mol per kg protein) and in patients who had been receiving ERT for at least 1 year (0.34 p/mol per kg protein) [40]. Higher concentrations of lyso-Gb1 in RBC membranes correlated with low Hb and abnormal deformability and morphology [40]. Urine lyso-Gb1 concentration correlated with liver volume in a prospective, single-center, cross-sectional study of patients with type 1 GD receiving ERT and healthy controls [44].
Correlations between lyso-Gb1 concentrations and other established biomarkers of GD were evaluated in six studies [33,40,41,44,47,52] (Table S6). Significant correlations between lyso-Gb1 and chitotriosidase concentrations in plasma and RBCs were observed in four studies [33,41,47,52], with Pearson coefficient values from 0.59 to >0.9, and a similar trend reported in one additional study [40]. Correlations between lyso-Gb1 and CCL18 concentrations were reported in three studies [33,40,48]. No correlation between urinary lyso-Gb1 and either chitotriosidase or CCL18 was observed in one study [44].
3. Discussion
By systematically evaluating preclinical and clinical publications relevant to lyso-Gb1 in GD up to March 2019, we have identified strong evidence for the use of lyso-Gb1 as a pathogenic mediator of disease and a diagnostic and pharmacodynamic biomarker, and some evidence for the use of lyso-Gb1 as a prognostic and disease-monitoring biomarker in GD. Although lyso-Gb1, chitotriosidase, and CCL18 correlate well with each other in patients with GD, lyso-Gb1 is more sensitive and specific than the other two biomarkers, irrespective of the chitotriosidase genotype [41,50]. Lyso-Gb1 fulfils many of the criteria required for a biomarker in that it is accessible in a clinical sample, easily and reliably quantifiable [33], diagnostically highly valuable, and reflects responses to therapeutic interventions [11]. Further research is warranted with respect to the relationship of lyso-Gb1 with clinical manifestations, including the prediction of comorbidities, burden of disease, and clinical outcomes, to fulfil conditions of an ideal biomarker of disease. Overall, the lyso-Gb1 data in GD adds to the body of evidence that the accumulation of corresponding sphingoid bases in other lysosomal storage disorders are pathogenic and diagnostic [7].
Since the literature search for this systematic review was conducted, additional data on the value of lyso-Gb1 as a biomarker in GD have been published. Lyso-Gb1 measured in dried blood spots was found to be highly sensitive and specific for GD in a case-control study conducted in the Russian Federation [118]. Further, the diagnostic laboratory work-up by Fuller et al. [41] showing the capacity of elevated plasma lyso-Gb1 to identify patients with GD with 100% sensitivity and specificity was extended successfully to testing using dried blood spots and, additionally, samples in a prenatal setting [119]. On the basis of a normal lyso-Gb1 reference interval of <0.16 pmol per dried blood spot, all patients with GD were differentiated from control samples and patients with other inherited metabolic disorders [119]. Indeed, Saville et al. report that in utero lyso-Gb1 quantitation (limit of detection, 1 pmol/mg protein) facilitates GD diagnosis in the prenatal setting [119]. Further, Polo et al. reported a significant elevation of lyso-Gb1 in neonatal dried blood spots using a newly developed and validated assay [120]. These findings support the value of measuring lyso-Gb1 in dried blood spots as a means to conduct high-throughput newborn screening, first conducted by Kang et al. in China [3]. Although few countries have newborn screening programs that include GD, high rates of false positives have been reported on the measurement of enzyme activity on dried blood spots [121,122], and second-tier analyses are being introduced. In North Eastern Italy, lyso-Gb1 testing on dried blood spots was found to have a positive predictive value of 100%, with all neonates returning elevated lyso-Gb1 confirmed as true positives for GD [121].
Data from these studies additionally suggest that lyso-Gb1 concentrations measured in dried blood spots have prognostic power [118,119]. Plasma lyso-Gb1 concentrations were found to be significantly higher in patients with neuronopathic GD than in those with non-neuronopathic disease, even in the neonatal period [119]. A neonate diagnosed at 1 day of age (homozygous for N370S), owing to an affected older sibling, had a plasma lyso-Gb1 level of 70 nmol/L compared with 1070–2620 nmol/L for four neuronopathic patients diagnosed at <20 days of age [119]. Lyso-Gb1 measured in dried blood spots also correlated with hepatomegaly and splenomegaly in the Russian study [118]. Another three studies providing information on plasma lyso-Gb1 as a prognostic biomarker were identified. Firstly, in a family in which all members over two generations presented with splenomegaly owing to four distinct GBA genotypes, a plasma lyso-Gb1 level spanning more than one order of magnitude correlated well with the presumed pathogenicity of the genotypes and with hepatosplenomegaly, thrombocytopenia, and bone pain [123]. Secondly, moderate-to-strong correlations between plasma lyso-Gb1 and spleen volume, liver volume, and Hb but not platelet count at baseline were detected in eliglustat clinical trials of treatment-naïve adults with type 1 GD [124]. Thirdly, in untreated pediatric and adult patients with GD, plasma lyso-Gb1 correlated with disease load and severity, with the highest concentrations (up to 200-fold elevations) observed in those with the type 2 and type 3 forms [125].
Four recent studies found that lyso-Gb1 measurement in dried blood spots is useful for monitoring patients with GD [126,127,128]. Among 103 untreated adult patients with type 1 GD who were followed up over a median of 20 years, the median lyso-Gb1 in dried blood spots at the last visit was 108.5 ng/mL (normal, <8 ng/mL) [126]. Patients with the R496H/other genotype had the lowest lyso-Gb1 concentrations and patients refusing therapy had the highest concentrations [126]. Lyso-Gb1 concentrations negatively correlated with platelet count in non-splenectomized patients but not with any other GD-related parameter [126]. In a separate study, up to 10 years of lyso-Gb1 data (measured in plasma and dried blood spots) from 292 patients enrolled in a single center participating in the Gaucher Outcome Survey registry were analyzed with respect to treatment outcomes [127]. Most patients had the homozygous N370S genotype and received relatively low doses of ERT [127]. At the time of first lyso-Gb1 assessment, patients on treatment had lower concentrations of plasma lyso-Gb1 than patients who were untreated at that time [127]. Treatment with ERT resulted in further reductions in plasma lyso-Gb1 in most treatment-naïve and previously treated patients [127]. This study demonstrated that routine lyso-Gb1 monitoring using the dried blood spot assay is feasible. A separate retrospective chart review conducted by the same research group found that lyso-Gb1 concentrations were significantly lower in children with mild type 1 GD than in those with severe type 1 GD and, in untreated children, lyso-Gb1 concentrations were inversely correlated with platelet counts [127]. During follow-up, lyso-Gb1 concentration increased in almost 50% of untreated children, more commonly in younger children [127]. A fourth study determined that lyso-Gb1 monitoring has utility in the assessment of loss of therapeutic effect, as indicated by increased lyso-Gb1 concentrations during periods of treatment interruption during a 3-year evaluation period [128]. Dried blood spot-based quantification of lyso-Gb1 concentrations was validated and applied to 19 patients with GD from a single center in Albania. During the ~25-month period of continuous ERT, there was a tendency for lyso-Gb1 values to decrease over time; however, lyso-Gb1 concentrations were found to increase 1.3–3.8-fold (median, 2.16) after treatment interruption. Findings from this study enabled the separation of patients undergoing treatment from patients not currently receiving treatment, with high sensitivity and specificity [128].
The value of plasma lyso-Gb1 as a pharmacodynamic and response biomarker was reported in three recent studies [124,125,127]. Reductions in plasma lyso-Gb1 concentrations after eliglustat treatment of 92% and 84% in phase II and phase III trials, respectively, correlated well with reductions in hepatosplenomegaly and increases in Hb and platelet counts [124]. Lyso-Gb1, as quantified in dried blood spots, was inversely correlated with Hb in children with type 1 GD receiving ERT in a retrospective chart review [127]. The counterintuitive increase in lyso-Gb1 observed in eight of the treated children was interpreted as suboptimal ERT dosing owing to weight gain [127]. Finally, modest plasma lyso-Gb1 elevations from baseline were observed among treated patients with GD, which may have correlated with residual disease activity due to continued bone marrow involvement, and with decreased hematologic and bone density values; however, in those with advanced disease including complications such as history of osteonecrosis or gammopathy, no significant correlation was observed [125].
It is interesting to speculate as to why not all measures of disease severity correlated with plasma lyso-Gb1 [33]. The generation of lyso-Gb1 in plasma is dependent on GBA activity, Gb1 substrate concentration, acid ceramidase activity, GBA2 activity [45], and transport capacity from the lysosome to cytoplasm to the extracellular space. The role of lyso-Gb1 in specific GD pathologies such as bone and central nervous system disease can be restricted to those anatomical structures and therefore may not manifest as an abnormal level in plasma. In treated patients, it is also possible that SRT and ERT have different effects on lyso-Gb1 dynamics in plasma.
Lyso-Gb1 measurement techniques continued to advance during the conduct of our review. Elevated concentrations of lyso-Gb1 could be detected in only 20 µL of plasma collected from patients with GD using reverse-phase LC-Differential Mobility Spectrometry-MS/MS, which enables the resolution of the corresponding stereoisomer [129]. Compared with plasma analysis, the measurement of lyso-Gb1 in dried blood spots offers a more convenient means of high-throughput testing without the need for an intravenous blood draw, with applications as a companion diagnostic and monitoring tool [119,120,127,130]. Dried-blood spot analysis has the advantage of requiring a smaller volume of blood, and being easily transportable to laboratory facilities, although the concentration of target analyte can potentially be low, necessitating a sensitive and specific assay for detection and quantification [131]. However, results can be influenced by sample integrity, and hematocrit level, which can vary widely, especially in neonates [132]. One assay that requires two 3.2-mm dried blood spot punches and facilitates the measurement of lyso-Gb1 at concentrations as low as 5 ng/mL could differentiate clearly between presumed normal patients and confirmed patients with GD [130]. Another assay demonstrated a high correlation between measurements of lyso-Gb1 concentrations in dried blood spots and plasma in GD; however, the diagnostic performance of lyso-Gb1 in dried blood spots was slightly lower than that in plasma [120].
One important limitation of lyso-Gb1 analyses is the variable methodology employed by different laboratories or within the same laboratory over time, preventing the ability to directly compare findings. In addition, the storage conditions of the pathology samples from which lyso-Gb1 concentrations were measured cannot be assured in some early studies. High variability of longitudinal lyso-Gb1 measurements has been reported in multiple studies, with potential explanations including the impact of the circadian rhythm, effects of nutrition and/or physical activity, or effects of coexisting pathological conditions [128]. Thus, the interpretation of lyso-Gb1 concentrations across studies should focus on trends rather than absolute quantitation. Further, the risk of bias for the different studies and study designs was variable. A risk of bias was particularly high in nRCTs and observational studies (63%) and these should be interpreted with care. Collaboration between laboratories is now required to allow future comparison of inter-laboratory lyso-Gb1 data. Firstly, standardization of the unit of lyso-Gb1 measurement is required across laboratories, as, currently, levels may be expressed in ng/mL, or using SI and ERNDIM units in nmol/L. Cross-validation between laboratories is required to confirm the validity of lyso-Gb1 biomarker data, while quality assurance programs to ascertain that laboratories maintain high levels of statistical reliability when measuring lyso-Gb1 will aid the cross-validation process.
4. Methods
The systematic literature review was conducted and reported in line with criteria stipulated by the Preferred Items for Systematic Review and Meta-Analyses Protocols (PRISMA-P) recommendations [133].
4.1. Search Strategy
Search terms were developed on the basis of Medical Subject Headings (MeSH), and free-text words and abbreviations related to lyso-Gb1. The specific search terms and Boolean strategy were as follows: (glucosylsphingosine OR GlcSph OR lyso-GL1 OR Lyso-Gb1 OR psychosine) AND Gaucher. The databases searched were the US National Library of Medicine (includes PubMed and MEDLINE), Embase, ScienceOpen, Science.gov, Biological Abstracts, and Sci-Hub. The searches were conducted between February and March 2019, with no restrictions with respect to the search period. Additional references identified from the reference lists of published articles were identified.
4.2. Eligibility Criteria
Eligible articles included original research articles (preclinical and clinical) reporting information on lyso-Gb1 in GD published at any time in the medical literature. Meta-analyses were included but systematic (without meta-analysis) or narrative reviews and single-patient case studies were excluded.
4.3. Screening and Data Collection
Citations and abstracts retrieved from the searches were compiled to create a single list of references. Abstracts were reviewed by three researchers to determine the articles to be included. If information in the abstract was not sufficient to make a decision, the full text publication was obtained and reviewed. Data were extracted from each eligible publication using a standardized Microsoft Excel® form developed for the systematic review. Extracted data included those related to study design, sample (size, type, and source), lyso-Gb1 assay method, interventions, and type of information on lyso-Gb1 as a pathogenic mediator and biomarker in GD.
4.4. Data Analysis
A two-tiered approach to data analyses was applied on the basis of the US Food and Drug Administration/National Institutes of Health Biomarker Working Group definition of a biomarker as follows: “a defined characteristic that is measured as an indicator of normal biological processes, pathogenic processes, or responses to an exposure or intervention, including therapeutic interventions” [12]. The two main categories were as follows: (1) lyso-Gb1 involvement in the pathophysiology of GD, and (2) evidence on lyso-Gb1 as a biomarker in GD. Pathology studies included human autopsy data and preclinical studies reporting on the accumulation and effects of lyso-Gb1. The experimental effects of lyso-Gb1 were graded by the criteria of causation, with controlled studies demonstrating induction (e.g., dose response) and reversibility given more credence than studies showing incidental observations. Biomarker studies were clinical studies reporting on lyso-Gb1 concentrations in subjects with and without GD, and in treated and untreated patients with GD. These data provided evidence for lyso-Gb1 as a potential diagnostic, prognostic, and disease/treatment monitoring biomarker in GD. More credence was given to studies specifically designed to examine lyso-Gb1 as a biomarker in GD than studies reporting observations incidental to lyso-Gb1 levels.
4.5. Quality (Risk of Bias) Assessment
A validated tool matched to the study type was used to assess the strength and validity of the empirical data for each individual study. The assessment of the quality of randomized controlled trials was carried out using recommendations from the National Institute for Health and Care Excellence (NICE) single technology appraisal (STA) manufacturer’s template [134]. The Newcastle–Ottawa instrument [135] was used to assess the quality of all non-randomized and observational studies. Animal studies were assessed using the Systematic Review Centre for Laboratory animal Experimentation (SYRCLE) risk of bias tool [136]. Some preclinical studies were not evaluated beyond the recognition of standard scientific methods, as suitable tools were not available at the time of analysis.
5. Conclusions
After systematically searching for and evaluating an extensive list of manuscripts published since 1974 according to PRISMA-P guidelines, we conclude that circulating lyso-Gb1 is a selective and sensitive biomarker of GD throughout the course of the disease, as a companion diagnostic and pharmacodynamic biomarker. There is a high degree of confidence that lyso-Gb1 mediates GD pathophysiology but further study is required on its specific roles in this process. Although there is some evidence supporting a role of lyso-Gb1 as a prognostic and disease-monitoring biomarker in GD, the associations of lyso-Gb1 level with prognosis, secondary clinical events, and bone disease requires further research.
Supplementary Materials
The following are available online at https://www.mdpi.com/1422-0067/21/19/7159/s1. Table S1: Quality assessment of RCTs using National Institute for Health and Care Excellence (NICE) single technology appraisal (STA). Table S2: Quality assessment of nRCTs using the Newcastle-Ottawa scoring (NOS) tool. Table S3: Quality assessment of animal studies using Syrcle. Table S4: In vitro studies reporting on intracellular lyso-Gb1 levels in GD models or cell lines. Table S5: In vivo studies reporting on lyso-Gb1 accumulation in GD models. Table S6: Clinical studies reporting on lyso-Gb1 levels, as measured by liquid chromatography techniques, in GD during treatment with ERT and/or SRT.
Author Contributions
Conceptualization and design, S.R.-V. and M.F.; Evaluation of data, S.R.-V., M.F., and A.Z.; Writing—review and editing, S.R.-V., M.F., and A.Z. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Takeda.
Acknowledgments
Under the direction of the authors, Malcolm Darkes, employee of Envision Pharma Group, provided writing assistance for this manuscript. Takeda Pharmaceutical Company Limited provided funding to Excel Medical Affairs for support in writing and editing this manuscript. Support with the design and conduct of the systematic literature review was provided by Robert Rhoades, employee of INNOTIO GmbH, and Catherine Rolland, employee of Envision Pharma Group, and was funded by Takeda.
Conflicts of Interest
The SZMC Gaucher Unit receives support from Sanofi/Genzyme for participation in the ICGG Registry, from Takeda for the GOS Registry, and Pfizer for TALIAS. S.R.-V. has received research/speaker fees and travel support from Pfizer, Sanofi Genzyme, and Takeda (Shire) and advisory fee from Takeda (Shire) and Prevail therapeutics. M.F. has received travel and research support from Sanofi-Genzyme and Takeda (Shire) A.Z. has received honoraria from Pfizer, Takeda (Shire) and BioEvents, and consultancy fees from Prevail Therapeutics, Avrobio, Insightec and Takeda. Takeda was involved in the concept and design of the study, and had no role in the collection or interpretation of data.
Abbreviations
| AMRF | Action myoclonus-renal failure |
| CBE | Conduritol B epoxide |
| CCL18 | (C-C motif) ligand 18 |
| CNS | Central nervous system |
| CSF | Cerebrospinal fluid |
| ERT | Enzyme replacement therapy |
| GBA | Glucosylceramidase |
| GD | Gaucher disease |
| Hb | Hemoglobin |
| HPLC | High-performance liquid chromatography |
| HPTLC | High-performance thin-layer chromatography |
| LC/MS/MS | Liquid chromatography tandem mass spectrometry |
| Lyso-Gb1 | Glucosylsphingosine |
| NICE | National Institute for Health and Care Excellence |
| PRISMA-P | Preferred Items for Systematic Review and Meta-Analyses Protocols |
| RBC | Red blood cell |
| SRT | Substrate reduction therapy |
| STA | Single technology appraisal |
| SYRCLE | Systematic Review Centre for Laboratory animal Experimentation |
| TDAG8 | T cell death-associated gene 8 |
| TLC | Thin-layer chromatography. |
References
- Zimran, A.; Elstein, D. Gaucher Disease and Related Lysosomal Storage Diseases. In Williams Hematology, 9th ed.; Kaushansky, K., Lichtman, M., Prchal, J., Levi, M.M., Press, O., Burns, L., Caligiuri, M., Eds.; McGraw-Hill: New York, NY, USA, 2016. [Google Scholar]
- Hruska, K.S.; LaMarca, M.E.; Scott, C.R.; Sidransky, E. Gaucher disease: Mutation and polymorphism spectrum in the glucocerebrosidase gene (GBA). Hum. Mutat. 2008, 29, 567–583. [Google Scholar] [CrossRef] [PubMed]
- Kang, L.; Zhan, X.; Gu, X.; Zhang, H. Successful newborn screening for Gaucher disease using fluorometric assay in China. J. Hum. Genet. 2017, 62, 763–768. [Google Scholar] [CrossRef] [PubMed]
- Matern, D.; Gavrilov, D.; Oglesbee, D.; Raymond, K.; Rinaldo, P.; Tortorelli, S. Newborn screening for lysosomal storage disorders. Semin. Perinatol. 2015, 39, 206–216. [Google Scholar] [CrossRef] [PubMed]
- Horowitz, M.; Pasmanik-Chor, M.; Borochowitz, Z.; Falik-Zaccai, T.; Heldmann, K.; Carmi, R.; Parvari, R.; Beit-Or, H.; Goldman, B.; Peleg, L.; et al. Prevalence of glucocerebrosidase mutations in the Israeli Ashkenazi Jewish population. Hum. Mutat. 1998, 12, 240–244. [Google Scholar] [CrossRef]
- Ferraz, M.J.; Kallemeijn, W.W.; Mirzaian, M.; Herrera Moro, D.; Marques, A.; Wisse, P.; Boot, R.G.; Willems, L.I.; Overkleeft, H.S.; Aerts, J.M. Gaucher disease and Fabry disease: New markers and insights in pathophysiology for two distinct glycosphingolipidoses. Biochim. Biophys. Acta 2014, 1841, 811–825. [Google Scholar] [CrossRef]
- Aerts, J.; Kuo, C.L.; Lelieveld, L.T.; Boer, D.E.C.; van der Lienden, M.J.C.; Overkleeft, H.S.; Artola, M. Glycosphingolipids and lysosomal storage disorders as illustrated by Gaucher disease. Curr. Opin. Chem. Biol. 2019, 53, 204–215. [Google Scholar] [CrossRef]
- Boven, L.A.; van Meurs, M.; Boot, R.G.; Mehta, A.; Boon, L.; Aerts, J.M.; Laman, J.D. Gaucher cells demonstrate a distinct macrophage phenotype and resemble alternatively activated macrophages. Am. J. Clin. Pathol. 2004, 122, 359–369. [Google Scholar] [CrossRef]
- Brady, R.O.; Kanfer, J.N.; Bradley, R.M.; Shapiro, D. Demonstration of a deficiency of glucocerebroside-cleaving enzyme in Gaucher’s disease. J. Clin. Investig. 1966, 45, 1112–1115. [Google Scholar] [CrossRef]
- Mistry, P.K.; Lopez, G.; Schiffmann, R.; Barton, N.W.; Weinreb, N.J.; Sidransky, E. Gaucher disease: Progress and ongoing challenges. Mol. Genet. Metab. 2017, 120, 8–21. [Google Scholar] [CrossRef]
- Lobato, B.J.; Hidalgo, M.J.; Jimenez, L.M.J. Biomarkers in lysosomal storage diseases. Diseases 2016, 4, 40. [Google Scholar] [CrossRef]
- Biomarkers Definitions Working Group. Biomarkers and surrogate endpoints: Preferred definitions and conceptual framework. Clin. Pharm. 2001, 69, 89–95. [Google Scholar]
- Hassan, S.; Sidransky, E.; Tayebi, N. The role of epigenetics in lysosomal storage disorders: Uncharted territory. Mol. Genet. Metab. 2017, 122, 10–18. [Google Scholar] [CrossRef] [PubMed]
- Biegstraaten, M.; van Schaik, I.N.; Aerts, J.M.; Langeveld, M.; Mannens, M.M.; Bour, L.J.; Sidransky, E.; Tayebi, N.; Fitzgibbon, E.; Hollak, C.E. A monozygotic twin pair with highly discordant Gaucher phenotypes. Blood Cells Mol. Dis. 2011, 46, 39–41. [Google Scholar] [CrossRef] [PubMed]
- Goker-Alpan, O.; Hruska, K.S.; Orvisky, E.; Kishnani, P.S.; Stubblefield, B.K.; Schiffmann, R.; Sidransky, E. Divergent phenotypes in Gaucher disease implicate the role of modifiers. J. Med. Genet. 2005, 42, e37. [Google Scholar] [CrossRef]
- Lachmann, R.H.; Grant, I.R.; Halsall, D.; Cox, T.M. Twin pairs showing discordance of phenotype in adult Gaucher’s disease. QJM 2004, 97, 199–204. [Google Scholar] [CrossRef]
- Lo, S.M.; Choi, M.; Liu, J.; Jain, D.; Boot, R.G.; Kallemeijn, W.W.; Aerts, J.M.; Pashankar, F.; Kupfer, G.M.; Mane, S.; et al. Phenotype diversity in type 1 Gaucher disease: Discovering the genetic basis of Gaucher disease/hematologic malignancy phenotype by individual genome analysis. Blood 2012, 119, 4731–4740. [Google Scholar] [CrossRef]
- Sims, K.B.; Pastores, G.M.; Weinreb, N.J.; Barranger, J.; Rosenbloom, B.E.; Packman, S.; Kaplan, P.; Mankin, H.; Xavier, R.; Angell, J.; et al. Improvement of bone disease by imiglucerase (Cerezyme) therapy in patients with skeletal manifestations of type 1 Gaucher disease: Results of a 48-month longitudinal cohort study. Clin. Genet. 2008, 73, 430–440. [Google Scholar] [CrossRef]
- Stein, P.; Yu, H.; Jain, D.; Mistry, P.K. Hyperferritinemia and iron overload in type 1 Gaucher disease. Am. J. Hematol. 2010, 85, 472–476. [Google Scholar] [CrossRef]
- Koppe, T.; Doneda, D.; Siebert, M.; Paskulin, L.; Camargo, M.; Tirelli, K.M.; Vairo, F.; Daudt, L.; Schwartz, I.V. The prognostic value of the serum ferritin in a southern Brazilian cohort of patients with Gaucher disease. Genet. Mol. Biol. 2016, 39, 30–34. [Google Scholar] [CrossRef]
- Stirnemann, J.; Boutten, A.; Vincent, C.; Mekinian, A.; Heraoui, D.; Fantin, B.; Fain, O.; Mentre, F.; Belmatoug, N. Impact of imiglucerase on the serum glycosylated-ferritin level in Gaucher disease. Blood Cells Mol. Dis. 2011, 46, 34–38. [Google Scholar] [CrossRef]
- Cabrera-Salazar, M.A.; O’Rourke, E.; Henderson, N.; Wessel, H.; Barranger, J.A. Correlation of surrogate markers of Gaucher disease. Implications for long-term follow up of enzyme replacement therapy. Clin. Chim. Acta 2004, 344, 101–107. [Google Scholar] [CrossRef] [PubMed]
- Boot, R.G.; Verhoek, M.; de Fost, M.; Hollak, C.E.; Maas, M.; Bleijlevens, B.; van Breemen, M.J.; van Meurs, M.; Boven, L.A.; Laman, J.D.; et al. Marked elevation of the chemokine CCL18/PARC in Gaucher disease: A novel surrogate marker for assessing therapeutic intervention. Blood 2004, 103, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Hollak, C.E.; van Weely, S.; van Oers, M.H.; Aerts, J.M. Marked elevation of plasma chitotriosidase activity. A novel hallmark of Gaucher disease. J. Clin. Investig. 1994, 93, 1288–1292. [Google Scholar] [CrossRef] [PubMed]
- Deegan, P.B.; Moran, M.T.; McFarlane, I.; Schofield, J.P.; Boot, R.G.; Aerts, J.M.; Cox, T.M. Clinical evaluation of chemokine and enzymatic biomarkers of Gaucher disease. Blood Cells Mol. Dis. 2005, 35, 259–267. [Google Scholar] [CrossRef] [PubMed]
- Ferraz, M.J.; Marques, A.R.; Appelman, M.D.; Verhoek, M.; Strijland, A.; Mirzaian, M.; Scheij, S.; Ouairy, C.M.; Lahav, D.; Wisse, P.; et al. Lysosomal glycosphingolipid catabolism by acid ceramidase: Formation of glycosphingoid bases during deficiency of glycosidases. FEBS Lett. 2016, 590, 716–725. [Google Scholar] [CrossRef]
- Gonzalez, D.E.; Turkia, H.B.; Lukina, E.A.; Kisinovsky, I.; Dridi, M.F.; Elstein, D.; Zahrieh, D.; Crombez, E.; Bhirangi, K.; Barton, N.W.; et al. Enzyme replacement therapy with velaglucerase alfa in Gaucher disease: Results from a randomized, double-blind, multinational, Phase 3 study. Am. J. Hematol. 2013, 88, 166–171. [Google Scholar] [CrossRef] [PubMed]
- Pastores, G.M.; Shankar, S.P.; Petakov, M.; Giraldo, P.; Rosenbaum, H.; Amato, D.J.; Szer, J.; Chertkoff, R.; Brill-Almon, E.; Zimran, A. Enzyme replacement therapy with taliglucerase alfa: 36-month safety and efficacy results in adult patients with Gaucher disease previously treated with imiglucerase. Am. J. Hematol. 2016, 91, 661–665. [Google Scholar] [CrossRef]
- Schutyser, E.; Richmond, A.; Van Damme, J. Involvement of CC chemokine ligand 18 (CCL18) in normal and pathological processes. J. Leukoc. Biol. 2005, 78, 14–26. [Google Scholar] [CrossRef]
- van Dussen, L.; Hendriks, E.J.; Groener, J.E.; Boot, R.G.; Hollak, C.E.; Aerts, J.M. Value of plasma chitotriosidase to assess non-neuronopathic Gaucher disease severity and progression in the era of enzyme replacement therapy. J. Inherit. Metab. Dis. 2014, 37, 991–1001. [Google Scholar] [CrossRef]
- Suzuki, K. Twenty five years of the “psychosine hypothesis”: A personal perspective of its history and present status. Neurochem. Res. 1998, 23, 251–259. [Google Scholar] [CrossRef]
- Linari, S.; Castaman, G. Clinical manifestations and management of Gaucher disease. Clin. Cases Min. Bone Metab. 2015, 12, 157–164. [Google Scholar] [CrossRef] [PubMed]
- Dekker, N.; van Dussen, L.; Hollak, C.E.; Overkleeft, H.; Scheij, S.; Ghauharali, K.; van Breemen, M.J.; Ferraz, M.J.; Groener, J.E.; Maas, M.; et al. Elevated plasma glucosylsphingosine in Gaucher disease: Relation to phenotype, storage cell markers, and therapeutic response. Blood 2011, 118, e118–e127. [Google Scholar] [CrossRef] [PubMed]
- Meikle, P.J.; Whitfield, P.D.; Rozaklis, T.; Blacklock, D.; Duplock, S.; Elstein, D.; Zimran, A.; Mengel, E.; Cannell, P.; Hopwood, J.J.; et al. Plasma lipids are altered in Gaucher disease: Biochemical markers to evaluate therapeutic intervention. Blood Cells Mol. Dis. 2008, 40, 420–427. [Google Scholar] [CrossRef] [PubMed]
- Groener, J.E.; Poorthuis, B.J.; Kuiper, S.; Helmond, M.T.; Hollak, C.E.; Aerts, J.M. HPLC for simultaneous quantification of total ceramide, glucosylceramide, and ceramide trihexoside concentrations in plasma. Clin. Chem. 2007, 53, 742–747. [Google Scholar] [CrossRef] [PubMed]
- Mistry, P.K.; Lukina, E.; Ben Turkia, H.; Shankar, S.P.; Baris, H.; Ghosn, M.; Mehta, A.; Packman, S.; Pastores, G.; Petakov, M.; et al. Outcomes after 18 months of eliglustat therapy in treatment-naive adults with Gaucher disease type 1: The phase 3 ENGAGE trial. Am. J. Hematol. 2017, 92, 1170–1176. [Google Scholar] [CrossRef]
- Arkadir, D.; Dinur, T.; Revel-Vilk, S.; Becker Cohen, M.; Cozma, C.; Hovakimyan, M.; Eichler, S.; Rolfs, A.; Zimran, A. Glucosylsphingosine is a reliable response biomarker in Gaucher disease. Am. J. Hematol. 2018, 93, E140–E142. [Google Scholar] [CrossRef]
- Chipeaux, C.; de Person, M.; Burguet, N.; Billette de Villemeur, T.; Rose, C.; Belmatoug, N.; Heron, S.; Le Van Kim, C.; Franco, M.; Moussa, F. Optimization of ultra-high pressure liquid chromatography-tandem mass spectrometry determination in plasma and red blood cells of four sphingolipids and their evaluation as biomarker candidates of Gaucher’s disease. J. Chromatogr. A 2017, 1525, 116–125. [Google Scholar] [CrossRef]
- Elstein, D.; Mellgard, B.; Dinh, Q.; Lan, L.; Qiu, Y.; Cozma, C.; Eichler, S.; Bottcher, T.; Zimran, A. Reductions in glucosylsphingosine (lyso-Gb1) in treatment-naive and previously treated patients receiving velaglucerase alfa for type 1 Gaucher disease: Data from phase 3 clinical trials. Mol. Genet. Metab. 2017, 122, 113–120. [Google Scholar] [CrossRef]
- Franco, M.; Reihani, N.; Marin, M.; De Person, M.; Billette de Villemeur, T.; Rose, C.; Colin, Y.; Moussa, F.; Belmatoug, N.; Le Van Kim, C. Effect of velaglucerase alfa enzyme replacement therapy on red blood cell properties in Gaucher disease. Am. J. Hematol. 2017, 92, E561–E563. [Google Scholar] [CrossRef]
- Fuller, M.; Szer, J.; Stark, S.; Fletcher, J.M. Rapid, single-phase extraction of glucosylsphingosine from plasma: A universal screening and monitoring tool. Clin. Chim. Acta 2015, 450, 6–10. [Google Scholar] [CrossRef]
- Gaspar, P.; Kallemeijn, W.W.; Strijland, A.; Scheij, S.; Van Eijk, M.; Aten, J.; Overkleeft, H.S.; Balreira, A.; Zunke, F.; Schwake, M.; et al. Action myoclonus-renal failure syndrome: Diagnostic applications of activity-based probes and lipid analysis. J. Lipid Res. 2014, 55, 138–145. [Google Scholar] [CrossRef] [PubMed]
- Lukina, E.; Watman, N.; Dragosky, M.; Lau, H.; Avila Arreguin, E.; Rosenbaum, H.; Zimran, A.; Foster, M.C.; Gaemers, S.J.M.; Peterschmitt, M.J. Outcomes after 8 years of eliglustat therapy for Gaucher disease type 1: Final results from the Phase 2 trial. Am. J. Hematol. 2019, 94, 29–38. [Google Scholar] [CrossRef] [PubMed]
- Mirzaian, M.; Wisse, P.; Ferraz, M.J.; Gold, H.; Donker-Koopman, W.E.; Verhoek, M.; Overkleeft, H.S.; Boot, R.G.; Kramer, G.; Dekker, N.; et al. Mass spectrometric quantification of glucosylsphingosine in plasma and urine of type 1 Gaucher patients using an isotope standard. Blood Cells Mol. Dis. 2015, 54, 307–314. [Google Scholar] [CrossRef] [PubMed]
- Mistry, P.K.; Liu, J.; Sun, L.; Chuang, W.L.; Yuen, T.; Yang, R.; Lu, P.; Zhang, K.; Li, J.; Keutzer, J.; et al. Glucocerebrosidase 2 gene deletion rescues type 1 Gaucher disease. Proc. Natl. Acad. Sci. USA 2014, 111, 4934–4939. [Google Scholar] [CrossRef] [PubMed]
- Moraitou, M.; Dimitriou, E.; Dekker, N.; Monopolis, I.; Aerts, J.; Michelakakis, H. Gaucher disease: Plasmalogen levels in relation to primary lipid abnormalities and oxidative stress. Blood Cells Mol. Dis. 2014, 53, 30–33. [Google Scholar] [CrossRef]
- Murugesan, V.; Chuang, W.L.; Liu, J.; Lischuk, A.; Kacena, K.; Lin, H.; Pastores, G.M.; Yang, R.; Keutzer, J.; Zhang, K.; et al. Glucosylsphingosine is a key biomarker of Gaucher disease. Am. J. Hematol. 2016, 91, 1082–1089. [Google Scholar] [CrossRef] [PubMed]
- Murugesan, V.; Liu, J.; Yang, R.; Lin, H.; Lischuk, A.; Pastores, G.; Zhang, X.; Chuang, W.L.; Mistry, P.K. Validating glycoprotein non-metastatic melanoma B (gpNMB, osteoactivin), a new biomarker of Gaucher disease. Blood Cells Mol. Dis. 2018, 68, 47–53. [Google Scholar] [CrossRef]
- Narita, A.; Shirai, K.; Itamura, S.; Matsuda, A.; Ishihara, A.; Matsushita, K.; Fukuda, C.; Kubota, N.; Takayama, R.; Shigematsu, H.; et al. Ambroxol chaperone therapy for neuronopathic Gaucher disease: A pilot study. Ann. Clin. Transl. Neurol. 2016, 3, 200–215. [Google Scholar] [CrossRef]
- Rolfs, A.; Giese, A.K.; Grittner, U.; Mascher, D.; Elstein, D.; Zimran, A.; Bottcher, T.; Lukas, J.; Hubner, R.; Golnitz, U.; et al. Glucosylsphingosine is a highly sensitive and specific biomarker for primary diagnostic and follow-up monitoring in Gaucher disease in a non-Jewish, Caucasian cohort of Gaucher disease patients. PLoS ONE 2013, 8, e79732. [Google Scholar] [CrossRef]
- Smid, B.E.; Ferraz, M.J.; Verhoek, M.; Mirzaian, M.; Wisse, P.; Overkleeft, H.S.; Hollak, C.E.; Aerts, J.M. Biochemical response to substrate reduction therapy versus enzyme replacement therapy in Gaucher disease type 1 patients. Orphanet J. Rare Dis. 2016, 11, 28. [Google Scholar] [CrossRef]
- Tylki-Szymanska, A.; Szymanska-Rozek, P.; Hasinski, P.; Lugowska, A. Plasma chitotriosidase activity versus plasma glucosylsphingosine in wide spectrum of Gaucher disease phenotypes-A statistical insight. Mol. Genet. Metab. 2018, 123, 495–500. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Oehrle, M.; Prada, C.E.; Schwartz, I.V.D.; Chutipongtanate, S.; Wattanasirichaigoon, D.; Inskeep, V.; Dai, M.; Pan, D.; Sun, Y.; et al. A convenient approach to facilitate monitoring Gaucher disease progression and therapeutic response. Analyst 2017, 142, 3380–3387. [Google Scholar] [CrossRef] [PubMed]
- Nilsson, O.; Grabowski, G.A.; Ludman, M.D.; Desnick, R.J.; Svennerholm, L. Glycosphingolipid studies of visceral tissues and brain from type 1 Gaucher disease variants. Clin. Genet. 1985, 27, 443–450. [Google Scholar] [CrossRef] [PubMed]
- Nilsson, O.; Mansson, J.E.; Hakansson, G.; Svennerholm, L. The occurrence of psychosine and other glycolipids in spleen and liver from the three major types of Gaucher’s disease. Biochim. Biophys. Acta 1982, 712, 453–463. [Google Scholar] [CrossRef]
- Nilsson, O.; Svennerholm, L. Accumulation of glucosylceramide and glucosylsphingosine (psychosine) in cerebrum and cerebellum in infantile and juvenile Gaucher disease. J. Neurochem. 1982, 39, 709–718. [Google Scholar] [CrossRef] [PubMed]
- Orvisky, E.; Park, J.K.; LaMarca, M.E.; Ginns, E.I.; Martin, B.M.; Tayebi, N.; Sidransky, E. Glucosylsphingosine accumulation in tissues from patients with Gaucher disease: Correlation with phenotype and genotype. Mol. Genet. Metab. 2002, 76, 262–270. [Google Scholar] [CrossRef]
- Orvisky, E.; Sidransky, E.; McKinney, C.E.; Lamarca, M.E.; Samimi, R.; Krasnewich, D.; Martin, B.M.; Ginns, E.I. Glucosylsphingosine accumulation in mice and patients with type 2 Gaucher disease begins early in gestation. Pediatr. Res. 2000, 48, 233–237. [Google Scholar] [CrossRef]
- Park, J.K.; Orvisky, E.; Tayebi, N.; Kaneski, C.; Lamarca, M.E.; Stubblefield, B.K.; Martin, B.M.; Schiffmann, R.; Sidransky, E. Myoclonic epilepsy in Gaucher disease: Genotype-phenotype insights from a rare patient subgroup. Pediatr. Res. 2003, 53, 387–395. [Google Scholar] [CrossRef]
- Raghavan, S.S.; Mumford, R.A.; Kanfer, J.N. Deficiency of glucosylsphingosine: Beta-glucosidase in Gaucher disease. Biochem. Biophys. Res. Commun. 1973, 54, 256–263. [Google Scholar] [CrossRef]
- Tayebi, N.; Walker, J.; Stubblefield, B.; Orvisky, E.; LaMarca, M.E.; Wong, K.; Rosenbaum, H.; Schiffmann, R.; Bembi, B.; Sidransky, E. Gaucher disease with parkinsonian manifestations: Does glucocerebrosidase deficiency contribute to a vulnerability to parkinsonism? Mol. Genet. Metab. 2003, 79, 104–109. [Google Scholar] [CrossRef]
- Conradi, N.G.; Sourander, P.; Nilsson, O.; Svennerholm, L.; Erikson, A. Neuropathology of the Norrbottnian type of Gaucher disease. Morphological and biochemical studies. Acta Neuropathol. 1984, 65, 99–109. [Google Scholar] [CrossRef] [PubMed]
- Lloyd-Evans, E.; Pelled, D.; Riebeling, C.; Bodennec, J.; de-Morgan, A.; Waller, H.; Schiffmann, R.; Futerman, A.H. Glucosylceramide and glucosylsphingosine modulate calcium mobilization from brain microsomes via different mechanisms. J. Biol. Chem. 2003, 278, 23594–23599. [Google Scholar] [CrossRef] [PubMed]
- Atsumi, S.; Nosaka, C.; Iinuma, H.; Umezawa, K. Accumulation of tissue glucosylsphingosine in Gaucher-like mouse induced by the glucosylceramidase inhibitor cyclophellitol. Arch. Biochem. Biophys. 1993, 304, 302–304. [Google Scholar] [CrossRef]
- Barnes, S.; Xu, Y.H.; Zhang, W.; Liou, B.; Setchell, K.D.; Bao, L.; Grabowski, G.A.; Sun, Y. Ubiquitous transgene expression of the glucosylceramide-synthesizing enzyme accelerates glucosylceramide accumulation and storage cells in a Gaucher disease mouse model. PLoS ONE 2014, 9, e116023. [Google Scholar] [CrossRef] [PubMed]
- Dahl, M.; Doyle, A.; Olsson, K.; Mansson, J.E.; Marques, A.R.A.; Mirzaian, M.; Aerts, J.M.; Ehinger, M.; Rothe, M.; Modlich, U.; et al. Lentiviral gene therapy using cellular promoters cures type 1 Gaucher disease in mice. Mol. Ther. 2015, 23, 835–844. [Google Scholar] [CrossRef]
- Dai, M.; Liou, B.; Swope, B.; Wang, X.; Zhang, W.; Inskeep, V.; Grabowski, G.A.; Sun, Y.; Pan, D. Progression of behavioral and CNS deficits in a viable murine model of chronic neuronopathic Gaucher disease. PLoS ONE 2016, 11, e0162367. [Google Scholar] [CrossRef]
- Dasgupta, N.; Xu, Y.H.; Li, R.; Peng, Y.; Pandey, M.K.; Tinch, S.L.; Liou, B.; Inskeep, V.; Zhang, W.; Setchell, K.D.; et al. Neuronopathic Gaucher disease: Dysregulated mRNAs and miRNAs in brain pathogenesis and effects of pharmacologic chaperone treatment in a mouse model. Hum. Mol. Genet. 2015, 24, 7031–7048. [Google Scholar] [CrossRef]
- Enquist, I.B.; Lo Bianco, C.; Ooka, A.; Nilsson, E.; Mansson, J.E.; Ehinger, M.; Richter, J.; Brady, R.O.; Kirik, D.; Karlsson, S. Murine models of acute neuronopathic Gaucher disease. Proc. Natl. Acad. Sci. USA 2007, 104, 17483–17488. [Google Scholar] [CrossRef]
- Farfel-Becker, T.; Vitner, E.B.; Kelly, S.L.; Bame, J.R.; Duan, J.; Shinder, V.; Merrill, A.H., Jr.; Dobrenis, K.; Futerman, A.H. Neuronal accumulation of glucosylceramide in a mouse model of neuronopathic Gaucher disease leads to neurodegeneration. Hum. Mol. Genet. 2014, 23, 843–854. [Google Scholar] [CrossRef]
- Ferraz, M.J.; Marques, A.R.; Gaspar, P.; Mirzaian, M.; van Roomen, C.; Ottenhoff, R.; Alfonso, P.; Irun, P.; Giraldo, P.; Wisse, P.; et al. Lyso-glycosphingolipid abnormalities in different murine models of lysosomal storage disorders. Mol. Genet. Metab. 2016, 117, 186–193. [Google Scholar] [CrossRef]
- Hamler, R.; Brignol, N.; Clark, S.W.; Morrison, S.; Dungan, L.B.; Chang, H.H.; Khanna, R.; Frascella, M.; Valenzano, K.J.; Benjamin, E.R.; et al. Glucosylceramide and glucosylsphingosine quantitation by liquid chromatography-tandem mass spectrometry to enable in vivo preclinical studies of neuronopathic Gaucher disease. Anal. Chem. 2017, 89, 8288–8295. [Google Scholar] [CrossRef] [PubMed]
- Karageorgos, L.; Hein, L.; Rozaklis, T.; Adams, M.; Duplock, S.; Snel, M.; Hemsley, K.; Kuchel, T.; Smith, N.; Hopwood, J.J. Glycosphingolipid analysis in a naturally occurring ovine model of acute neuronopathic Gaucher disease. Neurobiol. Dis. 2016, 91, 143–154. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Halene, S.; Yang, M.; Iqbal, J.; Yang, R.; Mehal, W.Z.; Chuang, W.L.; Jain, D.; Yuen, T.; Sun, L.; et al. Gaucher disease gene GBA functions in immune regulation. Proc. Natl. Acad. Sci. USA 2012, 109, 10018–10023. [Google Scholar] [CrossRef] [PubMed]
- Lukas, J.; Cozma, C.; Yang, F.; Kramp, G.; Meyer, A.; Nesslauer, A.M.; Eichler, S.; Bottcher, T.; Witt, M.; Brauer, A.U.; et al. Glucosylsphingosine causes hematological and visceral changes in mice-evidence for a pathophysiological role in Gaucher disease. Int. J. Mol. Sci. 2017, 18, 2192. [Google Scholar] [CrossRef]
- Marshall, J.; Sun, Y.; Bangari, D.S.; Budman, E.; Park, H.; Nietupski, J.B.; Allaire, A.; Cromwell, M.A.; Wang, B.; Grabowski, G.A.; et al. CNS-accessible inhibitor of glucosylceramide synthase for substrate reduction therapy of neuronopathic Gaucher disease. Mol Ther. 2016, 24, 1019–1029. [Google Scholar] [CrossRef]
- Mistry, P.K.; Liu, J.; Yang, M.; Nottoli, T.; McGrath, J.; Jain, D.; Zhang, K.; Keutzer, J.; Chuang, W.L.; Mehal, W.Z.; et al. Glucocerebrosidase gene-deficient mouse recapitulates Gaucher disease displaying cellular and molecular dysregulation beyond the macrophage. Proc. Natl. Acad. Sci. USA 2010, 107, 19473–19478. [Google Scholar] [CrossRef]
- Pandey, M.K.; Burrow, T.A.; Rani, R.; Martin, L.J.; Witte, D.; Setchell, K.D.; McKay, M.A.; Magnusen, A.F.; Zhang, W.; Liou, B.; et al. Complement drives glucosylceramide accumulation and tissue inflammation in Gaucher disease. Nature 2017, 543, 108–112. [Google Scholar] [CrossRef]
- Pavlova, E.V.; Archer, J.; Wang, S.; Dekker, N.; Aerts, J.M.; Karlsson, S.; Cox, T.M. Inhibition of UDP-glucosylceramide synthase in mice prevents Gaucher disease-associated B-cell malignancy. J. Pathol. 2015, 235, 113–124. [Google Scholar] [CrossRef]
- Pavlova, E.V.; Wang, S.Z.; Archer, J.; Dekker, N.; Aerts, J.M.; Karlsson, S.; Cox, T.M. B cell lymphoma and myeloma in murine Gaucher’s disease. J. Pathol. 2013, 231, 88–97. [Google Scholar] [CrossRef]
- Rocha, E.M.; Smith, G.A.; Park, E.; Cao, H.; Graham, A.R.; Brown, E.; McLean, J.R.; Hayes, M.A.; Beagan, J.; Izen, S.C.; et al. Sustained systemic glucocerebrosidase inhibition induces brain alpha-synuclein aggregation, microglia and complement C1q activation in mice. Antioxid. Redox Signal. 2015, 23, 550–564. [Google Scholar] [CrossRef]
- Sardi, S.P.; Viel, C.; Clarke, J.; Treleaven, C.M.; Richards, A.M.; Park, H.; Olszewski, M.A.; Dodge, J.C.; Marshall, J.; Makino, E.; et al. Glucosylceramide synthase inhibition alleviates aberrations in synucleinopathy models. Proc. Natl. Acad. Sci. USA 2017, 114, 2699–2704. [Google Scholar] [CrossRef] [PubMed]
- Smith, N.J.; Fuller, M.; Saville, J.T.; Cox, T.M. Reduced cerebral vascularization in experimental neuronopathic Gaucher disease. J. Pathol. 2018, 244, 120–128. [Google Scholar] [CrossRef] [PubMed]
- Taguchi, Y.V.; Liu, J.; Ruan, J.; Pacheco, J.; Zhang, X.; Abbasi, J.; Keutzer, J.; Mistry, P.K.; Chandra, S.S. Glucosylsphingosine promotes alpha-synuclein pathology in mutant GBA-associated Parkinson’s disease. J. Neurosci. 2017, 37, 9617–9631. [Google Scholar] [CrossRef] [PubMed]
- Vardi, A.; Zigdon, H.; Meshcheriakova, A.; Klein, A.D.; Yaacobi, C.; Eilam, R.; Kenwood, B.M.; Rahim, A.A.; Massaro, G.; Merrill, A.H., Jr.; et al. Delineating pathological pathways in a chemically induced mouse model of Gaucher disease. J. Pathol. 2016, 239, 496–509. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Liou, B.; Ran, H.; Skelton, M.R.; Williams, M.T.; Vorhees, C.V.; Kitatani, K.; Hannun, Y.A.; Witte, D.P.; Xu, Y.H.; et al. Neuronopathic Gaucher disease in the mouse: Viable combined selective saposin C deficiency and mutant glucocerebrosidase (V394L) mice with glucosylsphingosine and glucosylceramide accumulation and progressive neurological deficits. Hum. Mol. Genet. 2010, 19, 1088–1097. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Zhang, W.; Xu, Y.H.; Quinn, B.; Dasgupta, N.; Liou, B.; Setchell, K.D.; Grabowski, G.A. Substrate compositional variation with tissue/region and Gba1 mutations in mouse models-implications for Gaucher disease. PLoS ONE 2013, 8, e57560. [Google Scholar] [CrossRef]
- Bodennec, J.; Trajkovic-Bodennec, S.; Futerman, A.H. Simultaneous quantification of lyso-neutral glycosphingolipids and neutral glycosphingolipids by N-acetylation with [3H] acetic anhydride. J. Lipid Res. 2003, 44, 1413–1419. [Google Scholar] [CrossRef]
- Cabrera-Salazar, M.A.; Bercury, S.D.; Ziegler, R.J.; Marshall, J.; Hodges, B.L.; Chuang, W.L.; Pacheco, J.; Li, L.; Cheng, S.H.; Scheule, R.K. Intracerebroventricular delivery of glucocerebrosidase reduces substrates and increases lifespan in a mouse model of neuronopathic Gaucher disease. Exp. Neurol. 2010, 225, 436–444. [Google Scholar] [CrossRef]
- Cabrera-Salazar, M.A.; Deriso, M.; Bercury, S.D.; Li, L.; Lydon, J.T.; Weber, W.; Pande, N.; Cromwell, M.A.; Copeland, D.; Leonard, J.; et al. Systemic delivery of a glucosylceramide synthase inhibitor reduces CNS substrates and increases lifespan in a mouse model of type 2 Gaucher disease. PLoS ONE 2012, 7, e43310. [Google Scholar] [CrossRef]
- Sun, Y.; Ran, H.; Liou, B.; Quinn, B.; Zamzow, M.; Zhang, W.; Bielawski, J.; Kitatani, K.; Setchell, K.D.; Hannun, Y.A.; et al. Isofagomine in vivo effects in a neuronopathic Gaucher disease mouse. PLoS ONE 2011, 6, e19037. [Google Scholar] [CrossRef]
- Sun, Y.; Liou, B.; Xu, Y.H.; Quinn, B.; Zhang, W.; Hamler, R.; Setchell, K.D.; Grabowski, G.A. Ex vivo and in vivo effects of isofagomine on acid beta-glucosidase variants and substrate levels in Gaucher disease. J. Biol. Chem. 2012, 287, 4275–4287. [Google Scholar] [CrossRef] [PubMed]
- Raghavan, S.S.; Mumford, R.A.; Kanfer, J.N. Isolation and characterization of glucosylsphingosine from Gaucher’s spleen. J. Lipid Res. 1974, 15, 484–490. [Google Scholar] [PubMed]
- Aflaki, E.; Stubblefield, B.K.; Maniwang, E.; Lopez, G.; Moaven, N.; Goldin, E.; Marugan, J.; Patnaik, S.; Dutra, A.; Southall, N.; et al. Macrophage models of Gaucher disease for evaluating disease pathogenesis and candidate drugs. Sci. Transl. Med. 2014, 6, 240ra73. [Google Scholar] [CrossRef] [PubMed]
- Aflaki, E.; Westbroek, W.; Sidransky, E. The complicated relationship between Gaucher disease and Parkinsonism: Insights from a rare disease. Neuron 2017, 93, 737–746. [Google Scholar] [CrossRef] [PubMed]
- Igisu, H.; Hamasaki, N.; Ito, A.; Ou, W. Inhibition of cytochrome c oxidase and hemolysis caused by lysosphingolipids. Lipids 1988, 23, 345–348. [Google Scholar] [CrossRef] [PubMed]
- Nair, S.; Boddupalli, C.S.; Verma, R.; Liu, J.; Yang, R.; Pastores, G.M.; Mistry, P.K.; Dhodapkar, M.V. Type II NKT-TFH cells against Gaucher lipids regulate B-cell immunity and inflammation. Blood 2015, 125, 1256–1271. [Google Scholar] [CrossRef] [PubMed]
- Reed, M.C.; Schiffer, C.; Heales, S.; Mehta, A.B.; Hughes, D.A. Impact of sphingolipids on osteoblast and osteoclast activity in Gaucher disease. Mol. Genet. Metab. 2018, 124, 278–286. [Google Scholar] [CrossRef]
- Sasagasako, N.; Kobayashi, T.; Yamaguchi, Y.; Shinnoh, N.; Goto, I. Glucosylceramide and glucosylsphingosine metabolism in cultured fibroblasts deficient in acid beta-glucosidase activity. J. Biochem. 1994, 115, 113–119. [Google Scholar] [CrossRef]
- Schueler, U.H.; Kolter, T.; Kaneski, C.R.; Blusztajn, J.K.; Herkenham, M.; Sandhoff, K.; Brady, R.O. Toxicity of glucosylsphingosine (glucopsychosine) to cultured neuronal cells: A model system for assessing neuronal damage in Gaucher disease type 2 and 3. Neurobiol. Dis. 2003, 14, 595–601. [Google Scholar] [CrossRef]
- Westbroek, W.; Nguyen, M.; Siebert, M.; Lindstrom, T.; Burnett, R.A.; Aflaki, E.; Jung, O.; Tamargo, R.; Rodriguez-Gil, J.L.; Acosta, W.; et al. A new glucocerebrosidase-deficient neuronal cell model provides a tool to probe pathophysiology and therapeutics for Gaucher disease. Dis. Model. Mech. 2016, 9, 769–778. [Google Scholar] [CrossRef]
- Xu, Y.H.; Xu, K.; Sun, Y.; Liou, B.; Quinn, B.; Li, R.H.; Xue, L.; Zhang, W.; Setchell, K.D.; Witte, D.; et al. Multiple pathogenic proteins implicated in neuronopathic Gaucher disease mice. Hum. Mol. Genet. 2014, 23, 3943–3957. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Florer, J.; Mayhew, C.N.; Jia, Z.; Zhao, Z.; Xu, K.; Ran, H.; Liou, B.; Zhang, W.; Setchell, K.D.; et al. Properties of neurons derived from induced pluripotent stem cells of Gaucher disease type 2 patient fibroblasts: Potential role in neuropathology. PLoS ONE 2015, 10, e0118771. [Google Scholar] [CrossRef]
- Giri, S.; Khan, M.; Rattan, R.; Singh, I.; Singh, A.K. Krabbe disease: Psychosine-mediated activation of phospholipase A2 in oligodendrocyte cell death. J. Lipid Res. 2006, 47, 1478–1492. [Google Scholar] [CrossRef]
- Hannun, Y.A.; Bell, R.M. Lysosphingolipids inhibit protein kinase C: Implications for the sphingolipidoses. Science 1987, 235, 670–674. [Google Scholar] [CrossRef] [PubMed]
- Im, D.S.; Heise, C.E.; Nguyen, T.; O’Dowd, B.F.; Lynch, K.R. Identification of a molecular target of psychosine and its role in globoid cell formation. J. Cell Biol. 2001, 153, 429–434. [Google Scholar] [CrossRef] [PubMed]
- Taketomi, T.; Kawamura, N.; Hara, A.; Murakami, S. Comparative studies on chemical, hemolytic and diffusion-in-gel precipitation properties of various lysosphingolipids. Biochim. Biophys. Acta 1976, 424, 106–113. [Google Scholar] [PubMed]
- Aflaki, E.; Borger, D.K.; Moaven, N.; Stubblefield, B.K.; Rogers, S.A.; Patnaik, S.; Schoenen, F.J.; Westbroek, W.; Zheng, W.; Sullivan, P.; et al. A new glucocerebrosidase chaperone reduces alpha-synuclein and glycolipid levels in iPSC-derived dopaminergic neurons from patients with Gaucher disease and Parkinsonism. J. Neurosci. 2016, 36, 7441–7452. [Google Scholar] [CrossRef]
- Ridley, C.M.; Thur, K.E.; Shanahan, J.; Thillaiappan, N.B.; Shen, A.; Uhl, K.; Walden, C.M.; Rahim, A.A.; Waddington, S.N.; Platt, F.M.; et al. beta-Glucosidase 2 (GBA2) activity and imino sugar pharmacology. J. Biol. Chem. 2013, 288, 26052–26066. [Google Scholar] [CrossRef]
- Kuo, C.L.; Kallemeijn, W.W.; Lelieveld, L.T.; Mirzaian, M.; Zoutendijk, I.; Vardi, A.; Futerman, A.H.; Meijer, A.H.; Spaink, H.P.; Overkleeft, H.S.; et al. In vivo inactivation of glycosidases by conduritol B epoxide and cyclophellitol as revealed by activity-based protein profiling. Febs. J. 2019, 286, 584–600. [Google Scholar] [CrossRef]
- Sun, Y.; Zhang, W. Glycosphingolipid aspects of Gaucher disease lipidomics. Future Med. 2013. [Google Scholar] [CrossRef]
- Stirnemann, J.; Belmatoug, N.; Camou, F.; Serratrice, C.; Froissart, R.; Caillaud, C.; Levade, T.; Astudillo, L.; Serratrice, J.; Brassier, A.; et al. A Review of Gaucher Disease Pathophysiology, Clinical Presentation and Treatments. Int. J. Mol. Sci. 2017, 18, 441. [Google Scholar] [CrossRef] [PubMed]
- Nair, S.; Branagan, A.R.; Liu, J.; Boddupalli, C.S.; Mistry, P.K.; Dhodapkar, M.V. Clonal immunoglobulin against lysolipids in the origin of myeloma. N. Engl. J. Med. 2016, 374, 555–561. [Google Scholar] [CrossRef] [PubMed]
- Cozma, C.; Iurascu, M.; Mascher, H.; Rolfs, A. Quantification of glucosylsphingosine (luso-Gb1) for the diagnosis and monitoring of Gaucher disease. Mol. Genet. Metab. 2018, 123, S35. [Google Scholar]
- Mao, X.Y.; Burgunder, J.M.; Zhang, Z.J.; An, X.K.; Zhang, J.H.; Yang, Y.; Li, T.; Wang, Y.C.; Chang, X.L.; Peng, R. Association between GBA L444P mutation and sporadic Parkinson’s disease from Mainland China. Neurosci. Lett. 2010, 469, 256–259. [Google Scholar] [CrossRef] [PubMed]
- de Fost, M.; Hollak, C.E.; Groener, J.E.; Aerts, J.M.; Maas, M.; Poll, L.W.; Wiersma, M.G.; Haussinger, D.; Brett, S.; Brill, N.; et al. Superior effects of high-dose enzyme replacement therapy in type 1 Gaucher disease on bone marrow involvement and chitotriosidase levels: A 2-center retrospective analysis. Blood 2006, 108, 830–835. [Google Scholar] [CrossRef]
- Luan, Z.; Li, L.; Higaki, K.; Nanba, E.; Suzuki, Y.; Ohno, K. The chaperone activity and toxicity of ambroxol on Gaucher cells and normal mice. Brain Dev. 2013, 35, 317–322. [Google Scholar] [CrossRef]
- Savostyanova, K.; Pushkova, A.; Mura’vovaa, L.; Movsisyana, G.; Rykunovaa, A.; Ponomarevb, R.; Lukinab, K.; Lukinab, E.; Namazova-Baranovaa, L. Glucosylfingosine (lyso-GL1) may be the primary biomarker for screening Gaucher disease in Russian patients [Abstract number 318]. Mol. Genet. Metab. 2019, 126, S130. [Google Scholar]
- Saville, J.T.; McDermott, B.K.; Chin, S.J.; Fletcher, J.M.; Fuller, M. Expanding the clinical utility of glucosylsphingosine for Gaucher disease. J. Inherit. Metab. Dis. 2020, 43, 558–563. [Google Scholar] [CrossRef]
- Polo, G.; Burlina, A.P.; Ranieri, E.; Colucci, F.; Rubert, L.; Pascarella, A.; Duro, G.; Tummolo, A.; Padoan, A.; Plebani, M.; et al. Plasma and dried blood spot lysosphingolipids for the diagnosis of different sphingolipidoses: A comparative study. Clin. Chem. Lab. Med. 2019, 57, 1863–1874. [Google Scholar] [CrossRef]
- Burlina, A.; Polo, G.; Rubert, L.; Gueraldi, D.; Cazzorla, C.; Duro, G.; Salviati, L.; Burlina, A. Implementation of Second-Tier Tests in Newborn Screening for Lysosomal Disorders in North Eastern Italy. Int. J. Neonatal. Screen. 2019, 5, 24. [Google Scholar] [CrossRef]
- Bender, F.; Burin, M.G.; Tirelli, K.M.; Medeiros, F.; Bitencourt, F.H.; Civallero, G.; Kubaski, F.; Bravo, H.; Daher, A.; Carnier, V.; et al. Newborn screening for lysosomal disorders in Brazil: A pilot study using customized fluorimetric assays. Genet. Mol. Biol. 2020, 43, e20180334. [Google Scholar] [CrossRef] [PubMed]
- Cullufi, P.; Tabaku, M.; Beetz, C.; Tomori, S.; Velmishi, V.; Gjikopulli, A.; Bauer, P.; Wirth, S.; Rolfs, A. Comprehensive clinical, biochemical and genetic screening reveals four distinct GBA genotypes as underlying variable manifestation of Gaucher disease in a single family. Mol. Genet. Metab. Rep. 2019, 21, 100532. [Google Scholar] [CrossRef] [PubMed]
- Peterschmitt, M.J.; Foster, M.C.; Zhang, K.; Ji, A.; Cox, G. Correlations between glucosylsphingosine (lyso-GL-1) and baseline disease severity as well as response to treatment in two clinical trials of eliglustat in treatment-naïve adults with type 1 Gaucher disease (abstract number 281). Mol. Genet. Metab. 2019, 126, S117. [Google Scholar] [CrossRef]
- Dao, J.; Goker-Alpan, O.; Limgala, R. Evaluation of disease burden and therapy modifications using glucosylsphingosine (lyso-GL1) in Gaucher disease (abstract number 81). Mol. Genet. Metab. 2019, 126, S45. [Google Scholar] [CrossRef]
- Dinur, T.; Zimran, A.; Becker-Cohen, M.; Arkadir, D.; Cozma, C.; Hovakimyan, M.; Oppermann, S.; Demuth, L.; Rolfs, A.; Revel-Vilk, S. Long term follow-up of 103 untreated adult patients with type 1 Gaucher disease. J. Clin. Med. 2019, 8, 1662. [Google Scholar] [CrossRef]
- Hurvitz, N.; Dinur, T.; Becker-Cohen, M.; Cozma, C.; Hovakimyan, M.; Oppermann, S.; Demuth, L.; Rolfs, A.; Abramov, A.; Zimran, A.; et al. Glucosylsphingosine (lyso-Gb1) as a biomarker for monitoring treated and untreated children with Gaucher disease. Int. J. Mol. Sci. 2019, 20, 3033. [Google Scholar] [CrossRef]
- Cozma, C.; Cullufi, P.; Kramp, G.; Hovakimyan, M.; Velmishi, V.; Gjikopulli, A.; Tomori, S.; Fischer, S.; Oppermann, S.; Grittner, U.; et al. Treatment Efficiency in Gaucher Patients Can Reliably Be Monitored by Quantification of Lyso-Gb1 Concentrations in Dried Blood Spots. Int. J. Mol. Sci. 2020, 21, 4577. [Google Scholar] [CrossRef]
- Jones, M.G.; Blake, D.; Heidelberger, S.M.; Turner, C.; Dalton, R.N.; Cregeen, D.; Jackson, M. Plasma lysosphingolipid analysis by LC-DMS-MS/MS: Rapid sample preparation and resolution of stereoisomers (Abstract P-451). J. Inherit. Metab. Dis. 2019, 42. [Google Scholar]
- Smith, S.E.; Longua, M.; DiPerna, J. Quantitative measurement of glucosylsphingosine (lysoGb1) and galactosylsphingosine (psychosine) from dried blood spots. Presented at the 15th Annual WORLD Symposium, Orlando, FL, USA, 4–8 February 2019. [Google Scholar]
- Zakaria, R.; Allen, K.J.; Koplin, J.J.; Roche, P.; Greaves, R.F. Advantages and Challenges of Dried Blood Spot Analysis by Mass Spectrometry Across the Total Testing Process. EJIFCC 2016, 27, 288–317. [Google Scholar]
- de Vries, R.; Barfield, M.; van de Merbel, N.; Schmid, B.; Siethoff, C.; Ortiz, J.; Verheij, E.; van Baar, B.; Cobb, Z.; White, S.; et al. The effect of hematocrit on bioanalysis of DBS: Results from the EBF DBS-microsampling consortium. Bioanalysis 2013, 5, 2147–2160. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Care Excellence, NICE Technology Appraisal Guidance. 2018. Available online: https://www.nice.org.uk/about/what-we-do/our-programmes/nice-guidance/nice-technology-appraisal-guidance (accessed on 22 July 2019).
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality If Nonrandomized Studies in Meta-Analyses. 2012. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 20 November 2019).
- Hooijmans, C.R.; Rovers, M.M.; de Vries, R.B.; Leenaars, M.; Ritskes-Hoitinga, M.; Langendam, M.W. SYRCLE’s risk of bias tool for animal studies. BMC Med. Res. Methodol. 2014, 14, 43. [Google Scholar] [CrossRef] [PubMed]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).