Prevalence of Low Back Pain among Primary School Students from the City of Valencia (Spain)
Abstract
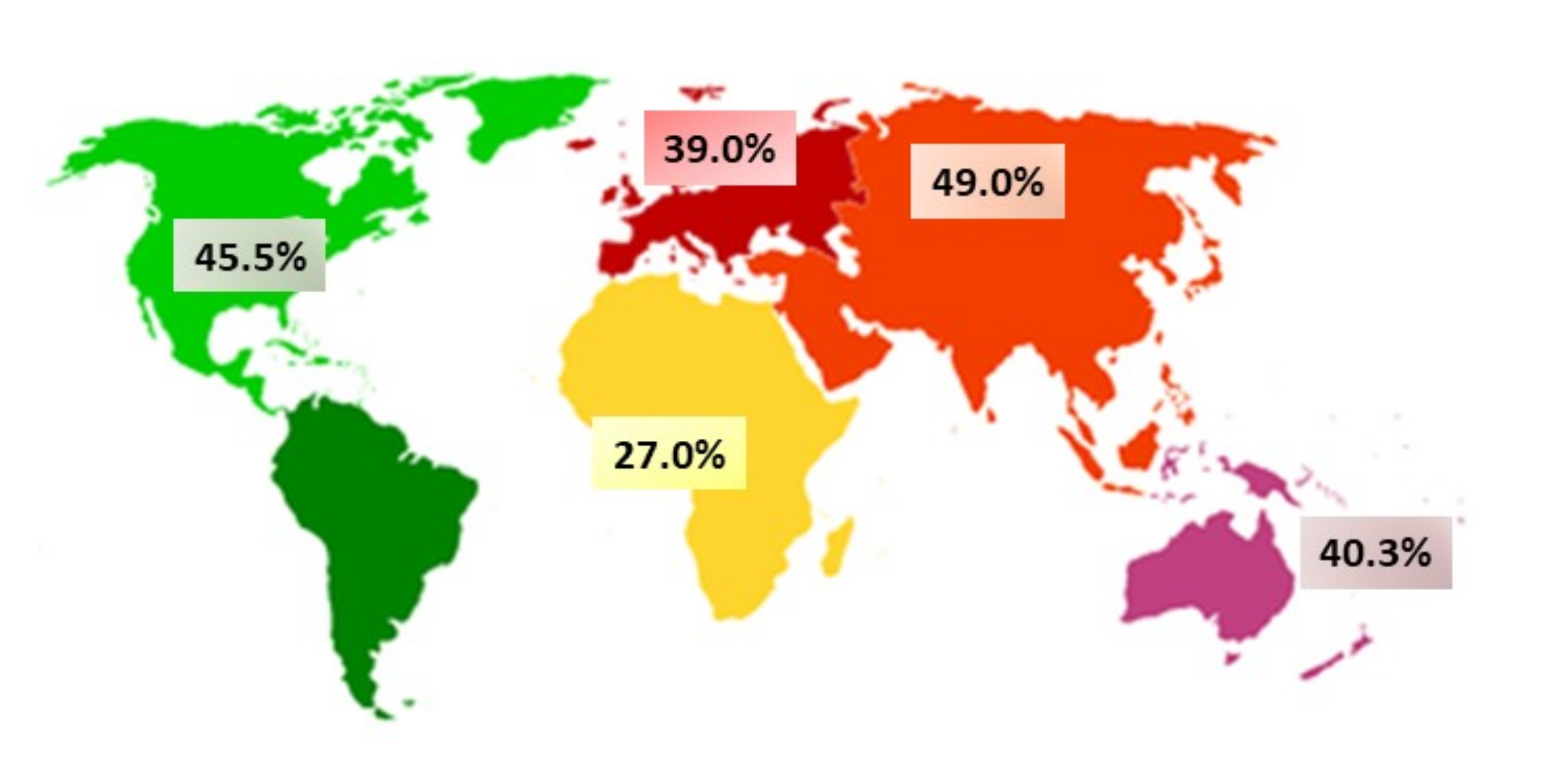
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Selection Criteria
2.3. Evaluation Instruments
2.4. Procedure
2.5. Statistical Analysis
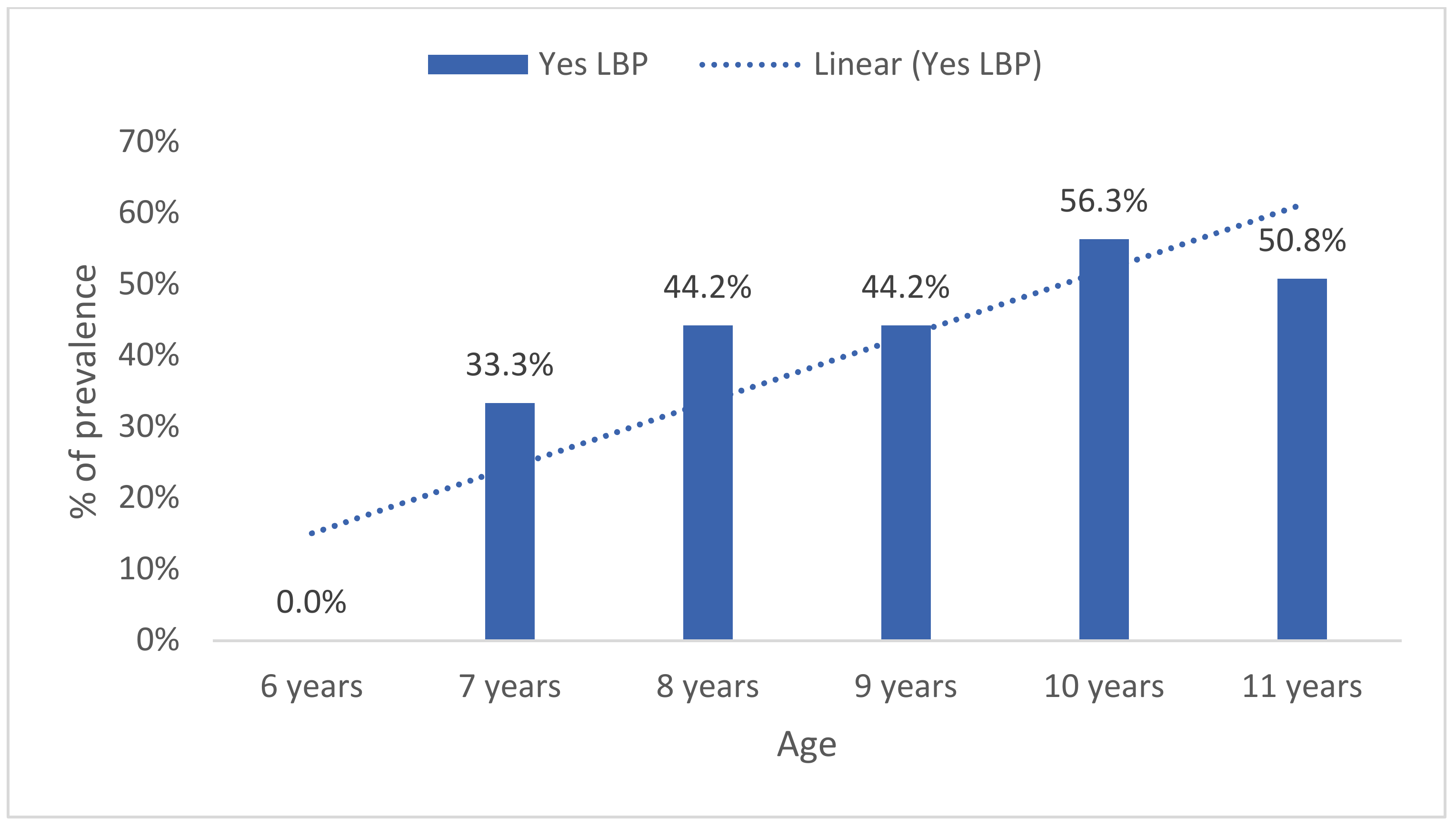
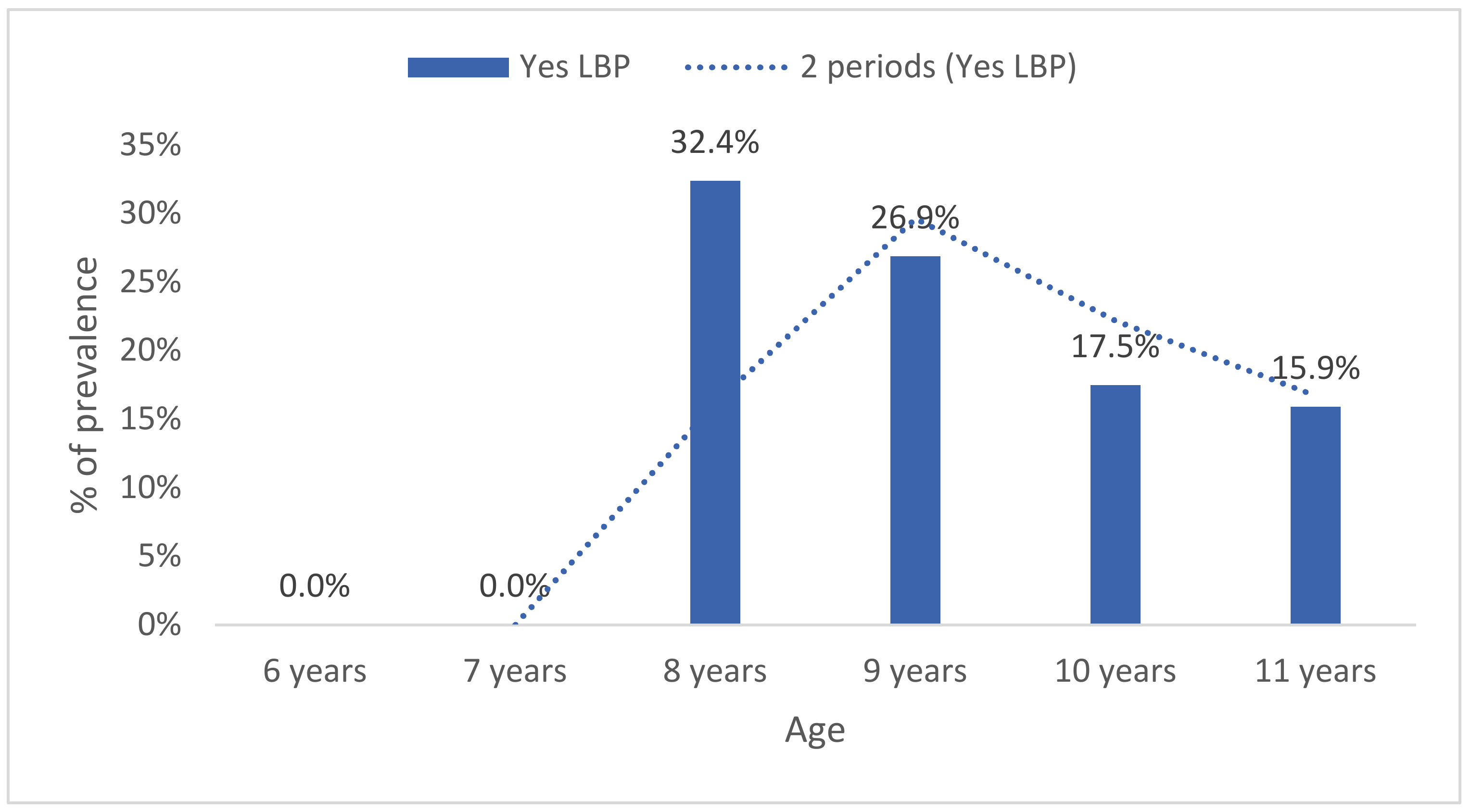
3. Results
Level of Back Pain Prevalence
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Salminen, J.J. The adolescent back. A field survey of 370 Finnish schoolchildren. Acta Paediatr. Scand. Suppl. 1984, 315, 1–122. [Google Scholar] [CrossRef]
- Calvo-Muñoz, I.; Gómez-Conesa, A.; Sánchez-Meca, J. Prevalence of low back pain in children and adolescents: A meta-analysis. BMC Pediatr. 2013, 13, 14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Balague, F.; Mannion, A.F.; Pellise, F.; Cedraschi, C. Non-specific low back pain. Lancet 2012, 379, 482–491. [Google Scholar] [CrossRef] [Green Version]
- Hoy, D.; March, L.; Brooks, P.; Blyth, F.; Woolf, A.; Bain, C.; Williams, G.; Smith, E.; Vos, T.; Barendregt, J.; et al. The global burden of low back pain: Estimates from the Global Burden of Disease 2010 study. Ann. Rheum. Dis. 2014, 73, 968–974. [Google Scholar] [CrossRef] [Green Version]
- Louw, Q.A.; Morris, L.D.; Grimmer-Somers, K. The prevalence of low back pain in Africa: A systematic review. BMC Musculoskelet. Disorder. 2007, 8, 105. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miñana-Signes, V.; Monfort-Pañego, M. Back Health in Adolescents between 12–18 Years of the Valencian Community, Spain: Prevalence and Consequences. J. Spine 2015, 4, 2. [Google Scholar]
- Woolf, A.D.; Pfleger, B. Burden of major musculoskeletal conditions. Bull. World Health Organ. 2003, 81, 646–656. [Google Scholar]
- Leboeuf-Yde, C.; Kyvik, K.O. At what age does low back pain become a common problem? A study of 29,424 individuals aged 12–41 years. Spine 1998, 23, 228–234. [Google Scholar] [CrossRef]
- Jeffries, L.J.; Milanese, S.F.; Grimmer-Somers, K.A. Epidemiology of adolescent spinal pain: A systematic overview of the research literature. Spine 2007, 32, 2630–2637. [Google Scholar] [CrossRef]
- Maher, C.; Underwood, M.; Buchbinder, R. Non-specific low back pain. Lancet 2017, 389, 736–747. [Google Scholar] [CrossRef] [Green Version]
- Cieply, R.; Milbrandt, T. Back pain in children and adolescents. Curr. Orthop. Pract. 2009, 20, 627–633. [Google Scholar] [CrossRef]
- Roth-Isigkeit, A.; Thyen, U.; Stoven, H.; Schwarzenberger, J.; Schmucker, P. Pain among children and adolescents: Restrictions in daily living and triggering factors. Pediatrics 2005, 115, e152–e162. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vidal, J.; Borras, P.A.; Ponseti, F.J.; Cantallops, J.; Ortega, F.B.; Palou, P. Effects of a postural education program on school backpack habits related to low back pain in children. Eur. Spine J. 2013, 22, 782–787. [Google Scholar] [CrossRef] [Green Version]
- Vidal, J.; Borras, P.A.; Ortega, F.B.; Cantallops, J.; Ponseti, X.; Palou, P. Effects of postural education on daily habits in children. Int. J. Sports Med. 2011, 32, 303–308. [Google Scholar] [CrossRef]
- Hill, J.J.; Keating, J.L. Daily exercises and education for preventing low back pain in children: Cluster randomized controlled trial. Phys. Ther. 2015, 95, 507–516. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dullien, S.; Grifka, J.; Jansen, P. Cluster-randomized, controlled evaluation of a teacher led multi factorial school based back education program for 10 to 12-year old children. BMC Pediatr. 2018, 18, 312. [Google Scholar] [CrossRef] [Green Version]
- Habybabady, R.H.; Ansari-Moghaddam, A.; Mirzaei, R.; Mohammadi, M.; Rakhshani, M.; Khammar, A. Efficacy and impact of back care education on knowledge and behaviour of elementary schoolchildren. J. Pak. Med. Assoc. 2012, 62, 580–584. [Google Scholar]
- Kovacs, F.; Oliver-Frontera, M.; Plana, M.N.; Royuela, A.; Muriel, A.; Gestoso, M. Spanish Back Pain Research Network. Improving schoolchildren’s knowledge of methods for the prevention and management of low back pain: A cluster randomized controlled trial. Spine 2011, 36, E505–E512. [Google Scholar] [CrossRef]
- Miñana-Signes, V.; Monfort-Pañego, M. Design and Validation of a Health Questionnaire about Knowledge for Health and Back Care Related to the Practice of Physical Activity and Exercise for Adolescents: COSACUES-AEF. J. Spine 2015, 4, 1–4. [Google Scholar]
- Monfort-Pañego, M.; Molina-García, J.; Miñana-Signes, V.; Bosch-Biviá, A.H.; Gómez-López, A.; Munguía-Izquierdo, D. Development and psychometric evaluation of a health questionnaire on back care knowledge in daily life physical activities for adolescent students. Eur. Spine J. 2016, 25, 2803–2808. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Monfort-Pañego, M.; Miñana-Signes, V. Psychometric Study and Content Validity of a Questionnaire to Assess Back-Health-Related Postural Habits in Daily Activities. Meas. Phys. Educ. Exerc. Sci. 2020, 24, 218–227. [Google Scholar] [CrossRef]
- Noll, M.; Candotti, C.T.; Vieira, A.; Loss, J.F. Back pain and body posture evaluation instrument (BackPEI): Development, content validation and reproducibility. Int. J. Public Health 2013, 58, 565–572. [Google Scholar] [CrossRef]
- Kuorinka, I.; Jonsson, B.; Kilbom, A.; Vinterberg, H.; Biering-Sørensen, F.; Andersson, G.; Jørgensen, K. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl. Ergon. 1987, 18, 233–237. [Google Scholar] [CrossRef]
- Weigold, A.; Weigold, I.K.; Natera, S.N. Response Rates for Surveys Completed with Paper-and-Pencil and Computers: Using Meta-Analysis to Assess Equivalence. Soc. Sci. Comput. Rev. 2019, 37, 649–668. [Google Scholar] [CrossRef]
- Salminen, J.J.; Erkintalo, M.; Laine, M.; Pentti, J. Low back pain in the young. A prospective three-year follow-up study of subjects with and without low back pain. Spine 1995, 20, 2101–2107. [Google Scholar] [CrossRef] [PubMed]
- Rezapur-Shahkolai, F.; Gheysvandi, E.; Tapak, L.; Dianat, I.; Karimi-Shahanjarini, A.; Heidarimoghadam, R. Risk factors for low back pain among elementary school students in western Iran using penalized logistic regression. Epidemiol. Health 2020, 42, e2020039. [Google Scholar] [CrossRef]
- Calvo-Muñoz, I.; Kovacs, F.M.; Roqué, M.; Gago Fernandez, I.; Seco Calvo, J. Risk Factors for Low Back Pain in Childhood and Adolescence. Clin. J. Pain 2018, 34, 468–484. [Google Scholar] [CrossRef] [PubMed]
- Mierau, D.; Cassidy, J.D.; Yong-Hing, K. Low-back pain and straight leg raising in children and adolescents. Spine 1989, 14, 526–528. [Google Scholar] [CrossRef]
- Dos Santos, M.A.; Lunkes, L.C.; de Oliveira Ribeiro, A.; de Castro Souza, A. Low back pain and risk factors during the third infancy. Fisioter. Mov. 2019, 32, e003210. [Google Scholar] [CrossRef]
- Wirth, B.; Knecht, C.; Humphreys, K. Spine day 2012: Spinal pain in Swiss school children–epidemiology and risk factors. BMC Pediatr. 2013, 13, 159. [Google Scholar] [CrossRef]
- Tiendrebeogo, W.; Ouédraogo, S.; Yago, I.; Zabsonré, D.S.; Tiaho, Y. Low Back Pain among Primary School Children: Prevalence and Risk Factors. A Cross-Sectional Study in Ouagadougou (Burkina Faso). J. Rheumatol. Res. 2020, 2, 98–106. [Google Scholar]
- Taimela, S.; Kujala, U.M.; Salminen, J.J.; Viljanen, T. The prevalence of low back pain among children and adolescents. A nationwide, cohort-based questionnaire survey in Finland. Spine 1997, 22, 1132–1136. [Google Scholar]
- Wedderkopp, N.; Leboeuf-Yde, C.; Andersen, L.B.; Froberg, K.; Hansen, H.S. Back pain reporting pattern in a Danish population-based sample of children and adolescents. Spine 2001, 26, 1879–1883. [Google Scholar] [CrossRef] [PubMed]
- Gunzburg, R.; Balague, F.; Nordin, M.; Szpalski, M.; Duyck, D.; Bull, D.; Mélot, C. Low back pain in a population of school children. Eur. Spine J. 1999, 8, 439–443. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ratliffe, T.; Hannon, J.C. Prevalence and Consequences of low back pain in children. Presented at the 2010 AAHPERD National Convention and Exposition, Exhibit Hall RC Poster Area (Convention Center), Indianapolis, IN, USA, 18 March 2010. [Google Scholar]
- Cardon, G.; de Clercq, D.; Geldhof, E.; De Clercq, D.; de Bourdeaudhuij, I. Back education in elementary schoolchildren: The effects of adding a physical activity promotion program to a back care program. Eur. Spine J. 2007, 16, 125–133. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Geldhof, E.; Cardon, G.; De Bourdeaudhuij, I.; De Clercq, D. Back posture education in elementary schoolchildren: A 2-year follow-up study. Eur. Spine J. 2007, 16, 841–850. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- MacDonald, J.; Stuart, E.; Rodenberg, R. Musculoskeletal low back pain in school-aged children: A review. JAMA Pediatr. 2017, 171, 280–287. [Google Scholar] [CrossRef] [PubMed]
- Burton, A.K. Low back pain in children and adolescents: To treat or not? Bull. Hosp. Jt. Dis. 1996, 55, 127–129. [Google Scholar]


| Age (Years) | School 1 M ± SD | School 2 M ± SD | Total M ± SD |
|---|---|---|---|
| 9.3 ± 1.8 | 9.4 ± 1.2 | 9.4 ± 1.3 | |
| n (%) | n (%) | n (%) | |
| 6 | 9 (10.8%) | 8 (4.4%) | 17 (6.4%) |
| 7 | 10 (12.0%) | 5 (2.8%) | 15 (5.7%) |
| 8 | 3 (3.6%) | 34 (18.8%) | 37 (14.0%) |
| 9 | 13 (15.7%) | 39 (21.5%) | 52 (19.7%) |
| 10 | 34 (41.0%) | 46 (25.4%) | 80 (30.3%) |
| 11 | 14 (16.9%) | 49 (27.1%) | 63 (23.9%) |
| Total | 97 (100%) | 181 (100%) | 264 (100%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miñana-Signes, V.; Monfort-Pañego, M.; Bosh-Bivià, A.H.; Noll, M. Prevalence of Low Back Pain among Primary School Students from the City of Valencia (Spain). Healthcare 2021, 9, 270. https://doi.org/10.3390/healthcare9030270
Miñana-Signes V, Monfort-Pañego M, Bosh-Bivià AH, Noll M. Prevalence of Low Back Pain among Primary School Students from the City of Valencia (Spain). Healthcare. 2021; 9(3):270. https://doi.org/10.3390/healthcare9030270
Chicago/Turabian StyleMiñana-Signes, Vicente, Manuel Monfort-Pañego, Antonio Hans Bosh-Bivià, and Matias Noll. 2021. "Prevalence of Low Back Pain among Primary School Students from the City of Valencia (Spain)" Healthcare 9, no. 3: 270. https://doi.org/10.3390/healthcare9030270









