Development of a Murine Model for Aerosolized Ebolavirus Infection Using a Panel of Recombinant Inbred Mice
Abstract
:1. Introduction
2. Results and Discussion
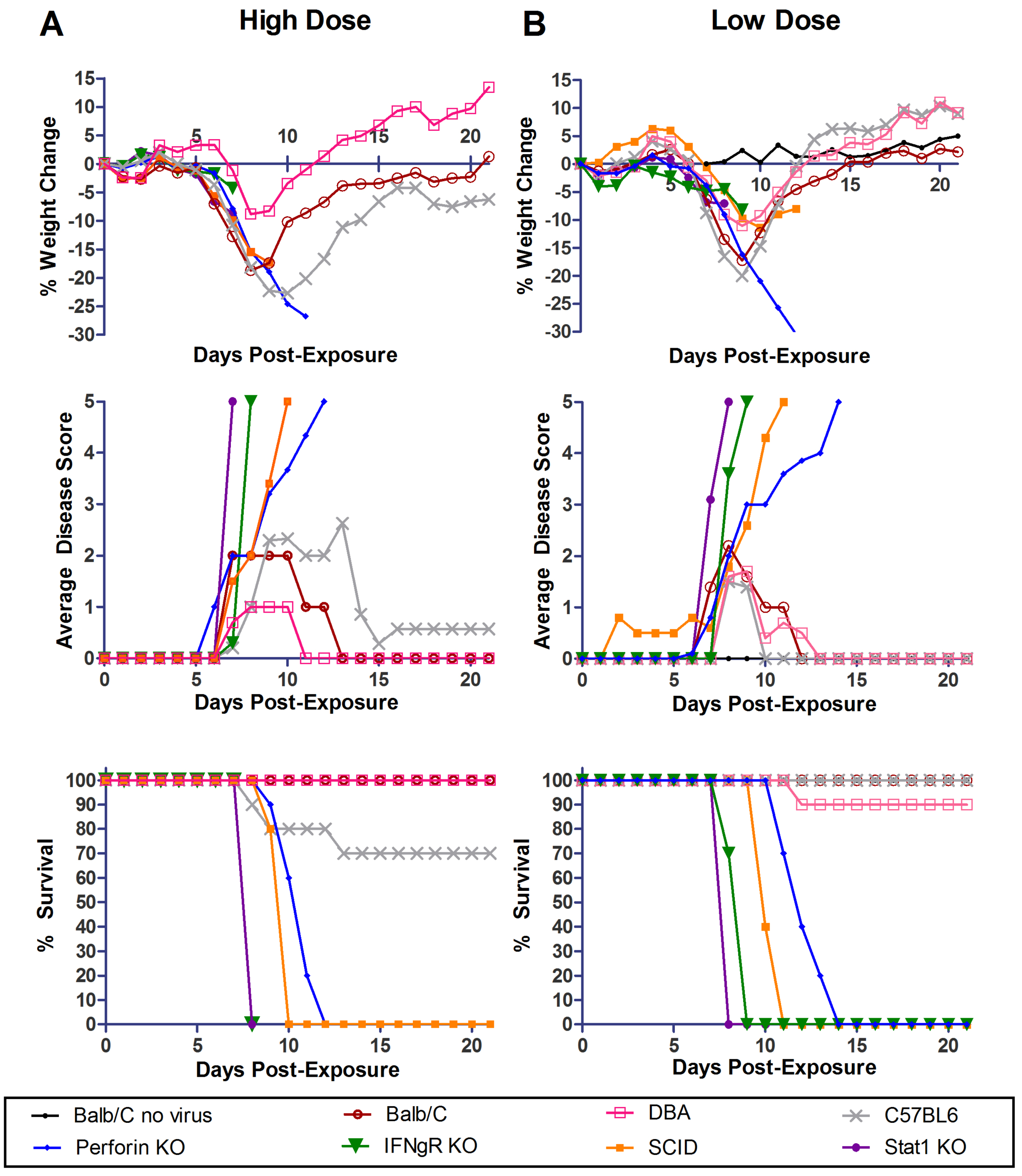
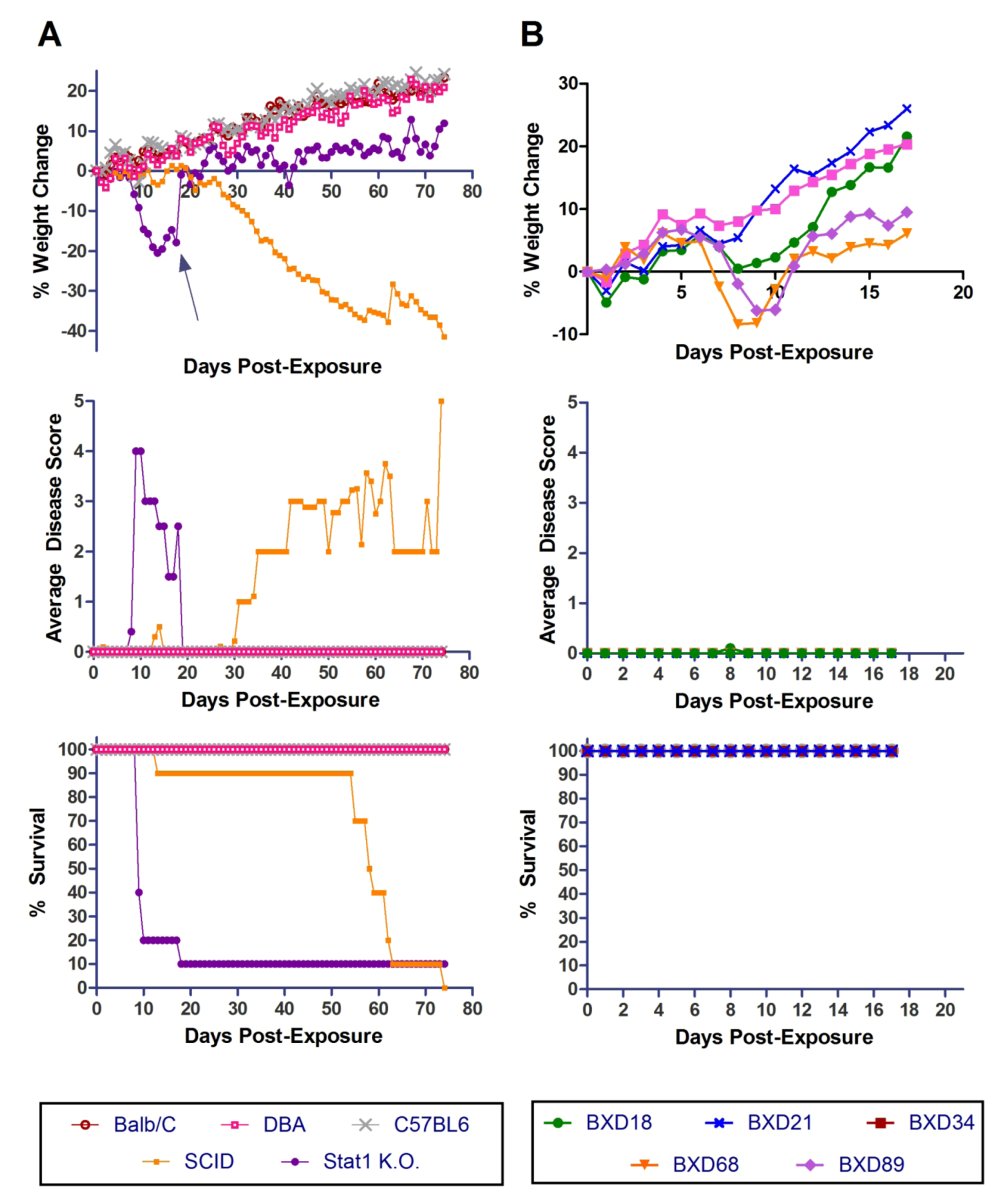
2.1. Exposure of Wild-Type and Immunocompromised Mice to a High Dose of Aerosolized MA-EBOV
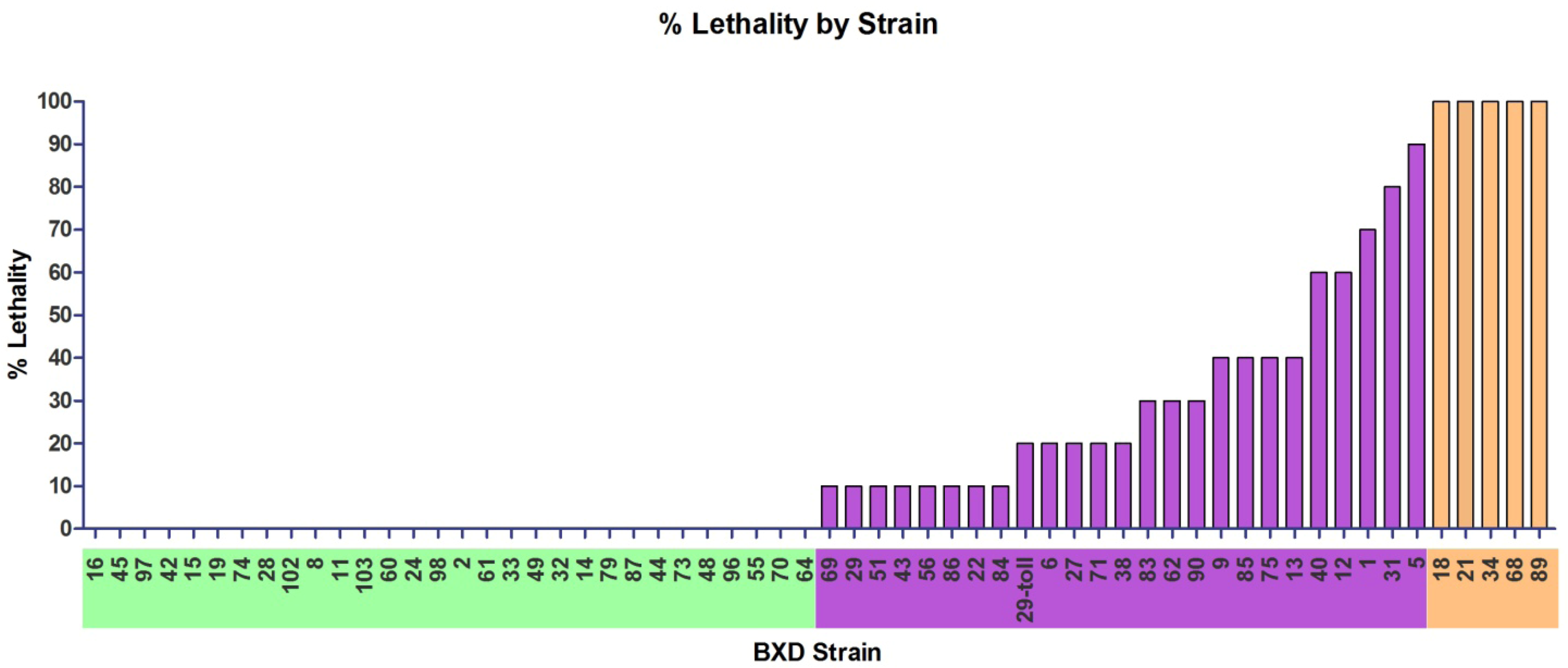
2.2. Differential Susceptibility of BXD RI and ARI Mice Strains Exposed to a High Dose of Aerosolized MA-EBOV
| BXD Strain | Ave. Age (days) | Dose | Ave. Starting Weight (g) | Max Weight Loss (%) | Onset clinical signs | % with clinical signs | Cumulative disease score | % Survival | 1st day Mori-bund | Last Day Mori-bund |
|---|---|---|---|---|---|---|---|---|---|---|
| C57Bl6 | 44 | 2573 | 19.7 | -18.1 | 7 | 100 | 169 | 70 | 9 | 13 |
| DBA | 44 | 2132 | 15.2 | -8.8 | 7 | 100 | 37 | 100 | na | na |
| 16 | 55 | 1291 | 21.2 | -9.2 | na | 0 | 0 | 100 | na | na |
| 45 | 63 | 301 | 17.8 | -11.3 | na | 0 | 0 | 100 | na | na |
| 97 | 55 | 1244 | 17.4 | -11.7 | na | 0 | 0 | 100 | na | na |
| 42 | 70 | 1093 | 19.5 | -12.8 | na | 0 | 0 | 100 | na | na |
| 15 | 55 | 1335 | 22 | -13 | na | 0 | 0 | 100 | na | na |
| 19 | 51 | 2295 | 17.5 | -14.6 | na | 0 | 0 | 100 | na | na |
| 74 | 41 | 1335 | 15 | -14.7 | na | 0 | 0 | 100 | na | na |
| 28 | 78 | 1808 | 22.8 | -23.7 | na | 0 | 0 | 100 | na | na |
| 102 | 71 | 2782 | 19.4 | -13.5 | 8 | 10 | 1 | 100 | na | na |
| 8 | 78 | 1466 | 20 | -19.6 | 6 | 10 | 2 | 100 | na | na |
| 11 | 55 | 1145 | 17.9 | -11.3 | 9 | 50 | 8 | 100 | na | na |
| 103 | 63 | 2650 | 18.2 | -18.6 | 8 | 50 | 9 | 100 | na | na |
| 60 | 70 | 1562 | 20.6 | -19.7 | 9 | 80 | 16 | 100 | na | na |
| 24 | 49 | 1721 | 17.2 | -9 | 7 | 100 | 64 | 100 | na | na |
| 98 | 57 | 1126 | 16 | -11.2 | 7 | 100 | 13 | 100 | na | na |
| 2 | 55 | 1356 | 22.4 | -11.8 | 7 | 100 | 12 | 100 | na | na |
| 61 | 63 | 1279 | 19.9 | -14.8 | 7 | 100 | 41 | 100 | na | na |
| 33 | 63 | 1667 | 15.5 | -16 | 8 | 100 | 20 | 100 | na | na |
| 49 | 67 | 1632 | 21.8 | -16.1 | 8 | 100 | 15 | 100 | na | na |
| 32 | 71 | 1910 | 21.1 | -17.2 | 8 | 100 | 26 | 100 | na | na |
| 14 | 61 | 1577 | 21.7 | -17.4 | 8 | 100 | 15 | 100 | na | na |
| 79 | 66 | 2169 | 18.7 | -18.2 | 8 | 100 | 14 | 100 | na | na |
| 87 | 56 | 279 | 16.1 | -18.7 | 9 | 100 | 21 | 100 | na | na |
| 44 | 55 | 949 | 16.2 | -18.9 | 7 | 100 | 40 | 100 | na | na |
| 73 | 51 | 2369 | 17.8 | -20.1 | 7 | 100 | 35 | 100 | na | na |
| 48 | 77 | 1655 | 22.2 | -20.5 | 8 | 100 | 24 | 100 | na | na |
| 96 | 70 | 1592 | 24.2 | -20.5 | 7 | 100 | 30 | 100 | na | na |
| 55 | 70 | 1280 | 19.9 | -20.6 | 7 | 100 | 26 | 100 | na | na |
| 70 | 70 | 2409 | 21.5 | -21 | 6 | 100 | 38 | 100 | na | na |
| 64 | 46 | 1505 | 17.6 | -24.7 | 6 | 100 | 40 | 100 | na | na |
| 69 | 63 | 1557 | 18.4 | -13.4 | 7 | 100 | 56 | 90 | 11 | 11 |
| 29 | 64 | 1600 | 19.3 | -13.5 | 9 | 50 | 10 | 90 | 10 | 10 |
| 51 | 62 | 1584 | 21 | -16.7 | 6 | 100 | 28 | 90 | 17 | 17 |
| 43 | 75 | 1777 | 19.1 | -17.7 | 9 | 100 | 20 | 90 | 17 | 17 |
| 56 | 65 | 1285 | 20 | -18 | 20 | 10 | 5 | 90 | 20 | 20 |
| 86 | 80 | 343 | 21.2 | -18.7 | 9 | 100 | 24 | 90 | 10 | 10 |
| 22 | 70 | 964 | 16.5 | -18.9 | 8 | 100 | 53 | 90 | 10 | 10 |
| 84 | 68 | 2212 | 19.2 | -20.3 | 6 | 100 | 42 | 90 | 13 | 13 |
| 29-Toll | 74 | 1564 | 18.8 | -11.6 | 8 | 100 | 30 | 80 | 10 | 11 |
| 6 | 58 | 1141 | 17.8 | -15 | 8 | 100 | 26 | 80 | 9 | 10 |
| 27 | 51 | 2503 | 19.6 | -16.3 | 7 | 100 | 51 | 80 | 10 | 11 |
| 71 | 68 | 1303 | 20.4 | -20.3 | 6 | 100 | 68 | 80 | 12 | 14 |
| 38 | 65 | 2355 | 17.6 | -21 | 7 | 100 | 98 | 80 | 12 | 12 |
| 83 | 60 | 2728 | 18.9 | -12.3 | 7 | 100 | 49 | 70 | 9 | 10 |
| 62 | 77 | 2233 | 19.4 | -16.6 | 9 | 100 | 45 | 70 | 9 | 11 |
| 90 | 53 | 1170 | 16.8 | -17 | 7 | 100 | 70 | 70 | 10 | 10 |
| 9 | 70 | 1492 | 30 | -17.8 | 7 | 100 | 90 | 60 | 11 | 123 |
| 85 | 58 | 1347 | 19.4 | -18.2 | 5 | 100 | 107 | 60 | 10 | 14 |
| 75 | 49 | 1575 | 18.7 | -19.4 | 8 | 100 | 54 | 60 | 10 | 12 |
| 13 | 54 | 1249 | 20.3 | -19.8 | 9 | 100 | 37 | 60 | 10 | 13 |
| 40 | 75 | 1783 | 19.2 | -17.3 | 8 | 100 | 92 | 40 | 11 | 11 |
| 12 | 65 | 1101 | 17.2 | -20.4 | 7 | 100 | 99 | 40 | 9 | 10 |
| 1 | 60 | 1221 | 19.5 | -21 | 7 | 100 | 117 | 30 | 8 | 12 |
| 31 | 71 | 1735 | 21.5 | -14.5 | 8 | 100 | 84 | 20 | 8 | 11 |
| 5 | 68 | 1429 | 19 | -16.9 | 8 | 100 | 136 | 10 | 10 | 17 |
| 18 | 78 | 1552 | 21.3 | -17 | 8 | 100 | 95 | 0 | 9 | 12 |
| 21 | 51 | 2036 | 14.9 | -17.7 | 7 | 100 | 103 | 0 | 10 | 11 |
| 34 | 78 | 2110 | 24.1 | -11.97 | 6 | 100 | 81 | 0 | 7 | 7 |
| 68 | 51 | 2408 | 18.3 | -20.2 | 7 | 100 | 90 | 0 | 10 | 10 |
| 89 | 47 | 1345 | 20.3 | -13 | 7 | 100 | 93 | 0 | 9 | 10 |
2.3. Uniform Lethality in Five BXD Mouse Strains Exposed to a High Dose of Aerosolized MA-EBOV
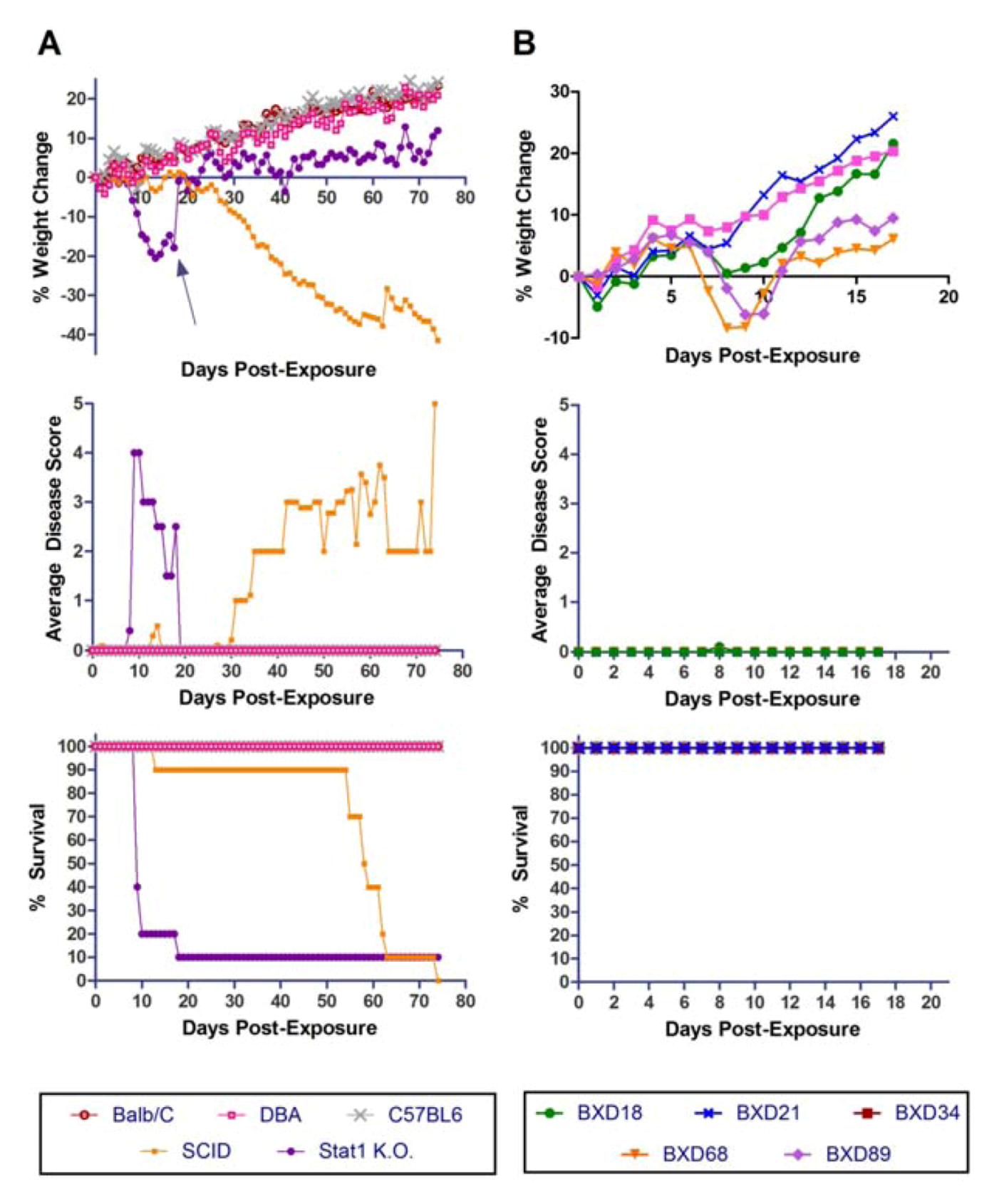
2.4. Exposure of Susceptible BXD Mouse Strains to a Low Dose of Aerosolized MA-EBOV
2.5. Tissue Viral Load and Histopathology in BXD Mouse Strains Exposed to Aerosolized MA-EBOV
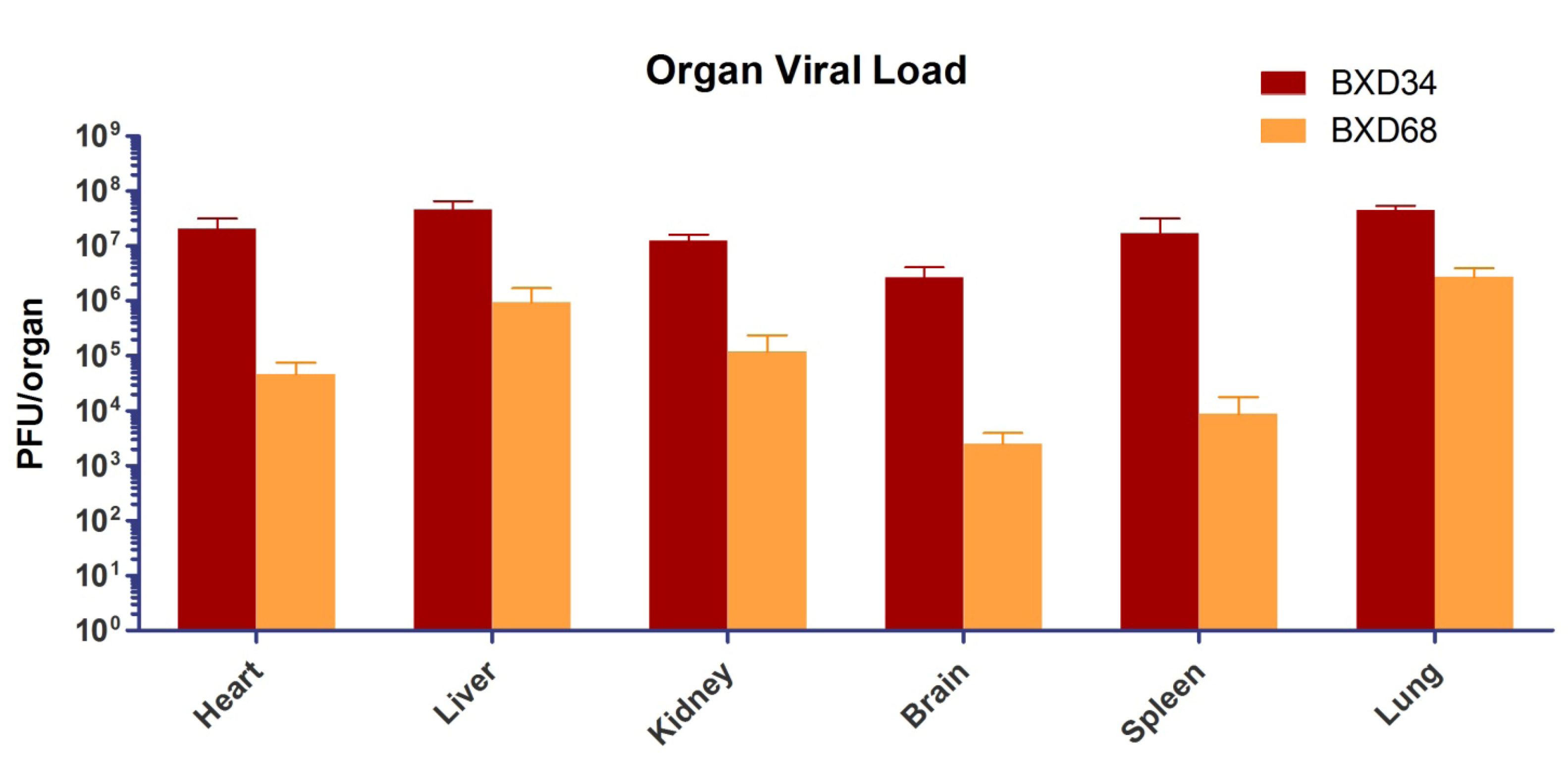
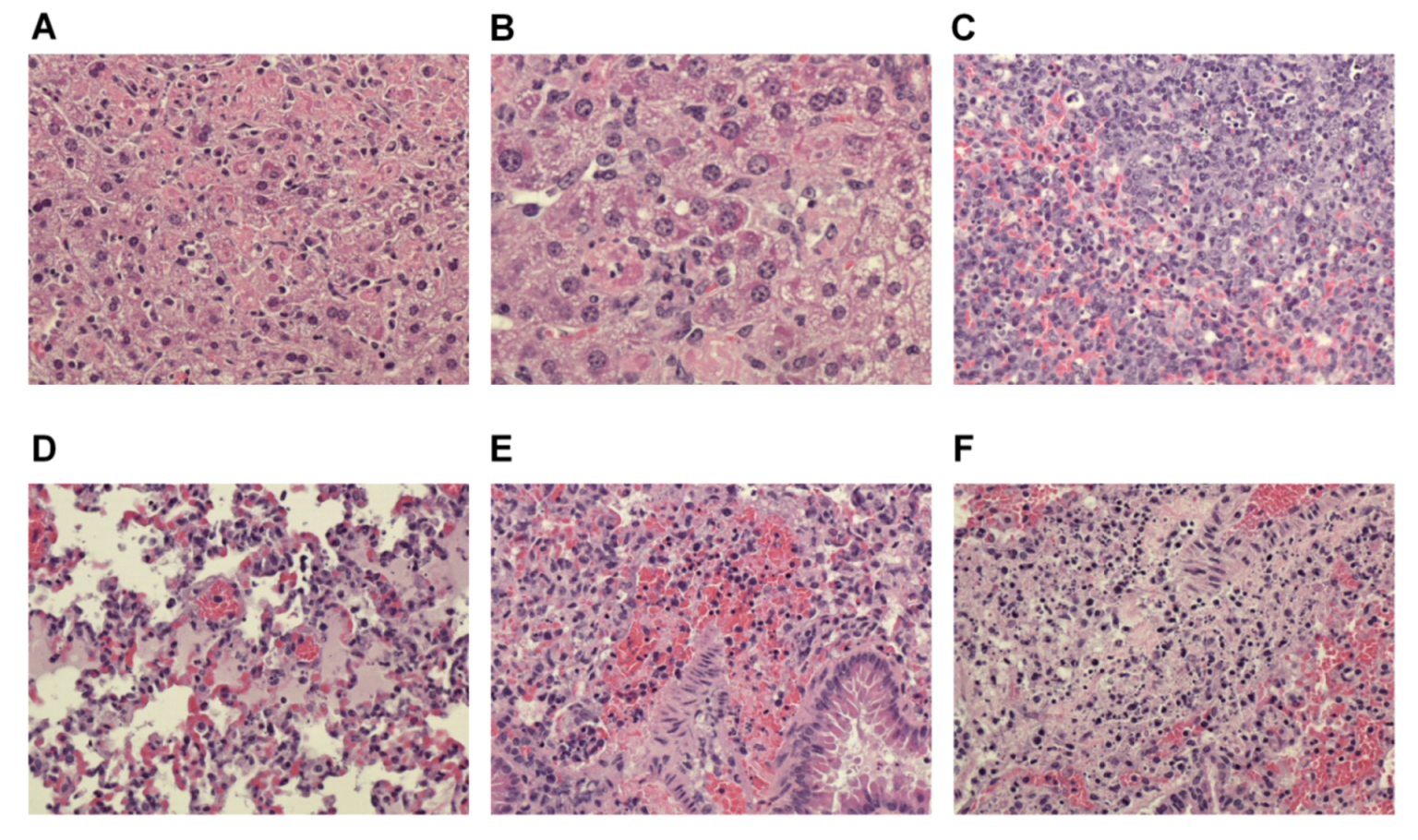
2.6. Histological Findings
| Strain | Ave.Dose (pfu) | Day p.e. | Liver* | Spleen | Mesenteric LN | Lungs | Adrenals |
|---|---|---|---|---|---|---|---|
| BXD34 | 53 | 8 | lesions | necrosis | lymphocytolysis | WNL** | cortical necrosis |
| BXD68 | 51 | 9 | lesions | necrosis | lymphocytolysis | mf*** necrosis | cortical necrosis |
2.7. Susceptibility of WT and Immunocompromised Mouse Strains to Aerosolized WT-EBOV
2.8. Susceptibility of BXD Strains to Aerosolized WT-EBOV
2.9. Multiple Covariate Analysis Confirms the Role of BXD Mouse Strains Genetic Background in Modulating Differential Susceptibility to Aerosolized MA-EBOV
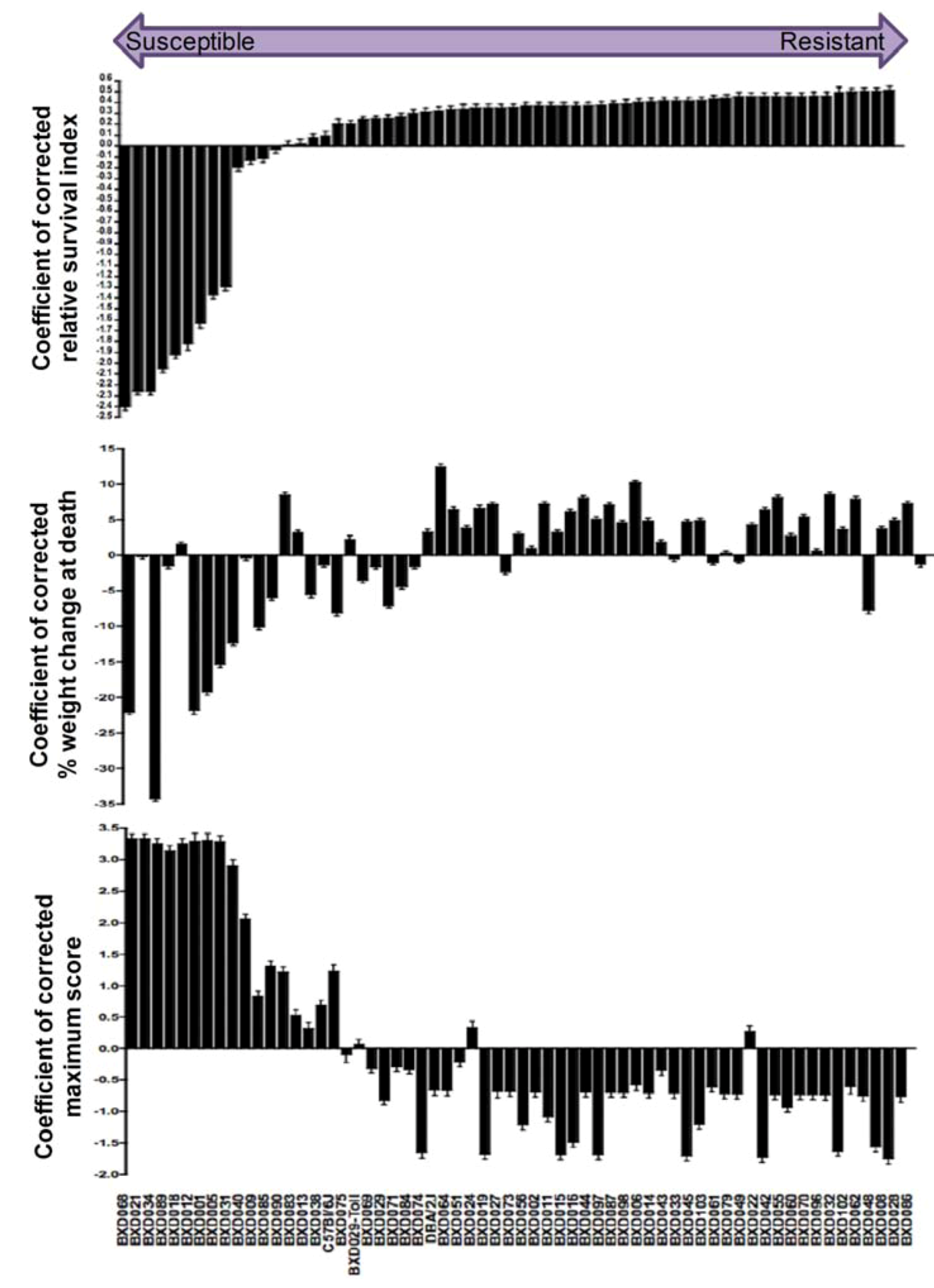
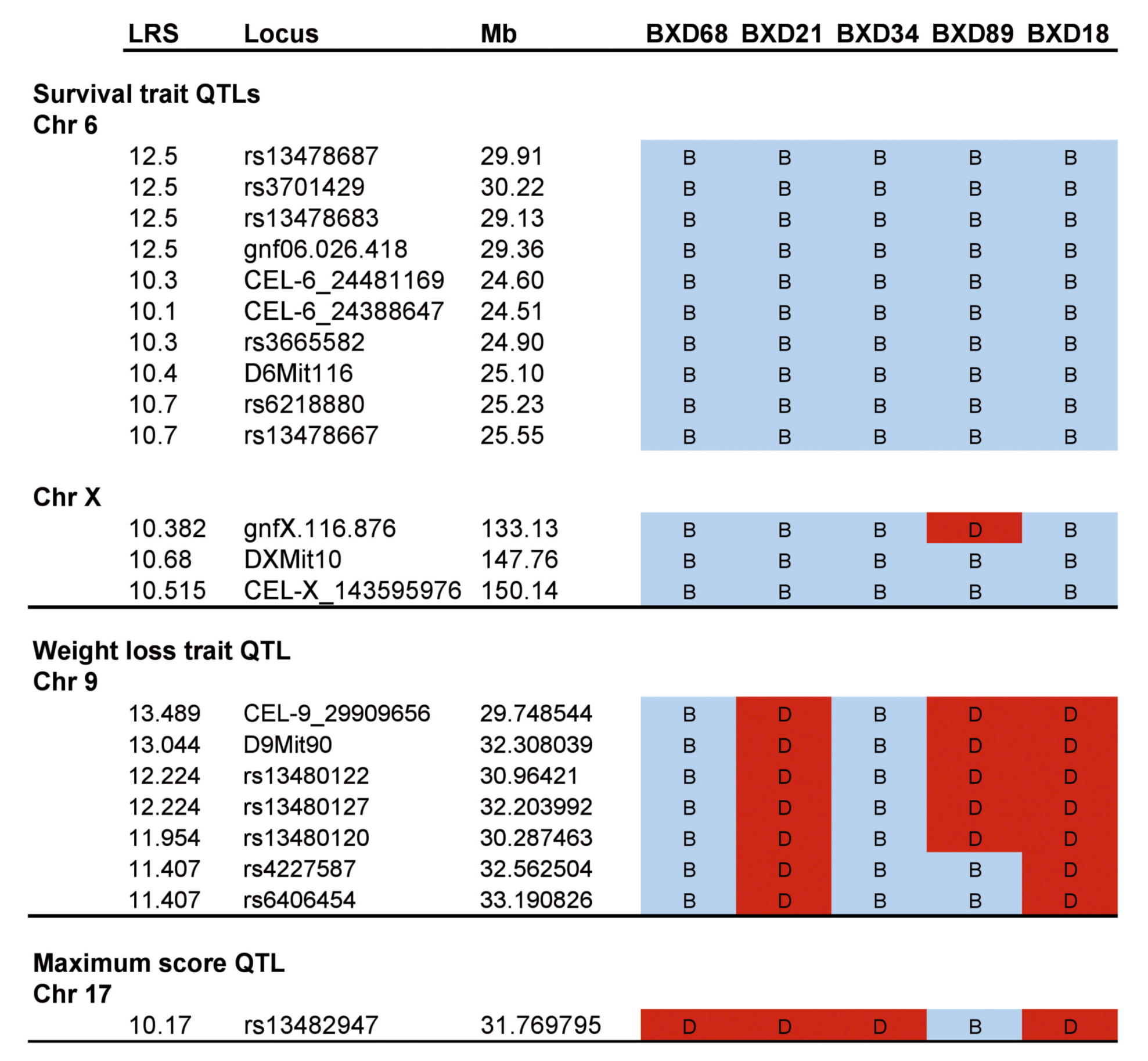
2.10. Preliminary Genome-Wide QTL Mapped Traits Associated with Differential Response of BXD Strains to Aerosolized MA-EBOV
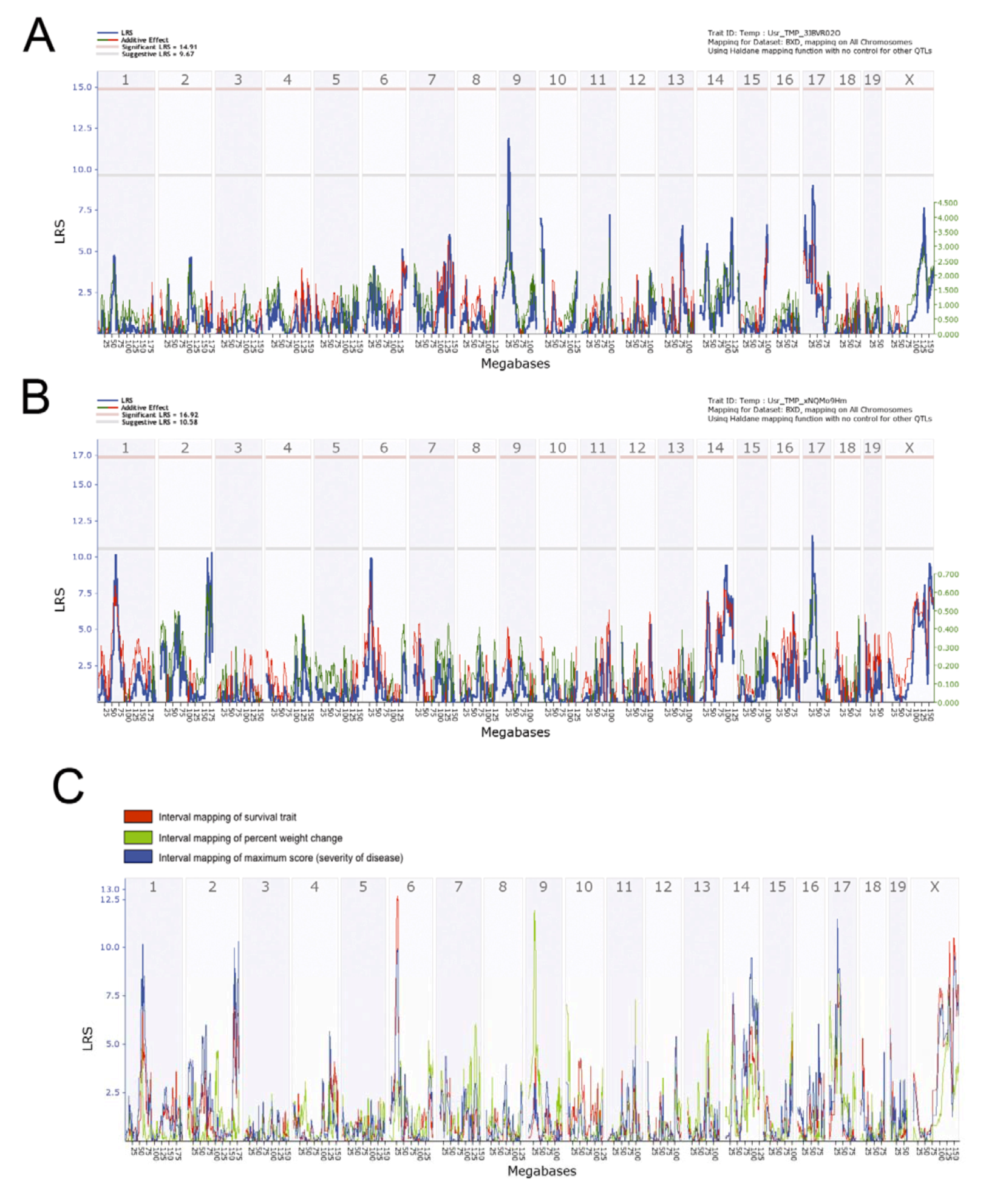
2.11. Linkage Analysis and Haplotype Mapping of Preliminary Survival QTLs Associated with Susceptibility to Airborne MA-EBOV.
3. Experimental Section
3.1. Mice
3.2. Ethics and Animal Welfare
3.3. Virus
3.4. Aerosol Exposures
3.5. Post-Exposure Monitoring
3.6. Plaque Assay
3.7. Histopathology
3.8. Quantitative Trait Loci (QTL) Mapping
3.9. Data Handling and Statistical Analysis
4. Conclusions
Conflict of Interest
Acknowledgments
References
- Kuhn, J.H.; Becker, S.; Ebihara, H.; Geisbert, T.W.; Johnson, K.M.; Kawaoka, Y.; Lipkin, W.I.; Negredo, A.I.; Netesov, S.V.; Nichol, S.T.; et al. Proposal for a revised taxonomy of the family Filoviridae: Classification, names of taxa and viruses, and virus abbreviations. Arch. Virol. 2010, 155, 2083–2103. [Google Scholar] [CrossRef]
- Leffel, E.K.; Reed, D.S. Marburg and Ebola viruses as aerosol threats. Biosecur. Bioterror. 2004, 2, 186–191. [Google Scholar] [CrossRef]
- Reed, D.S.; Lackemeyer, M.G.; Garza, N.L.; Sullivan, L.J.; Nichols, D.K. Aerosol exposure to Zaire ebolavirus in three nonhuman primate species: Differences in disease course and clinical pathology. Microb. Infect. 2011, 13, 930–936. [Google Scholar] [CrossRef]
- Alves, D.A.; Glynn, A.R.; Steele, K.E.; Lackemeyer, M.G.; Garza, N.L.; Buck, J.G.; Mech, C.; Reed, D.S. Aerosol exposure to the angola strain of marburg virus causes lethal viral hemorrhagic Fever in cynomolgus macaques. Vet. Pathol. 2010, 47, 831–851. [Google Scholar] [CrossRef]
- Zumbrun, E.E.; Bloomfield, H.A.; Dye, J.M.; Hunter, T.C.; Dabisch, P.A.; Garza, N.L.; Bramel, N.R.; Baker, R.J.; Williams, R.D.; Nichols, D.K.; et al. A Characterization of aerosolized sudan Ebolavirus infection in African Green Monkeys, Cynomolgus Macaques, and rhesus macaques. Viruses 2012, 4, 2115–2136. [Google Scholar] [CrossRef]
- Kuhn, J.H. Filoviruses. A compendium of 40 years of epidemiological, clinical, and laboratory studies. Arch. Virol. Suppl. 2008, 20, 13–360. [Google Scholar] [CrossRef]
- Bray, M. The role of the type I interferon response in the resistance of mice to filovirus infection. J. Gen. Virol. 2001, 82, 1365–1373. [Google Scholar]
- Bradfute, S.B.; Braun, D.R.; Shamblin, J.D.; Geisbert, J.B.; Paragas, J.; Garrison, A.; Hensley, L.E.; Geisbert, T.W. Lymphocyte death in a mouse model of Ebola virus infection. J. Infect. Dis. 2007, 196, S296–S304. [Google Scholar] [CrossRef]
- Bray, M.; Davis, K.; Geisbert, T.; Schmaljohn, C.; Huggins, J. A mouse model for evaluation of prophylaxis and therapy of Ebola hemorrhagic fever. J. Infect. Dis. 1998, 178, 651–661. [Google Scholar]
- Lever, M.S.; Piercy, T.J.; Steward, J.A.; Eastaugh, L.; Smither, S.J.; Taylor, C.; Salguero, F.J.; Phillpotts, R.J. Lethality and pathogenesis of airborne infection with filoviruses in A129 α/β -/- interferon receptor-deficient mice. J. Med. Microbio. 2011, 6, 8–15. [Google Scholar]
- Gibb, T.R.; Bray, M.; Geisbert, T.W.; Steele, K.E.; Kell, W.M.; Davis, K.J.; Jaax, N.K. Pathogenesis of experimental Ebola Zaire virus infection in BALB/c mice. J. Comp. Pathol. 2001, 125, 233–242. [Google Scholar] [CrossRef]
- Bray, M.; Davis, K.; Geisbert, T.; Schmaljohn, C.; Huggins, J. A mouse model for evaluation of prophylaxis and therapy of Ebola hemorrhagic fever. J. Infect. Dis 1999, 179, S248–S258. [Google Scholar]
- Gupta, M.; Greer, P.; Mahanty, S.; Shieh, W.J.; Zaki, S.R.; Ahmed, R.; Rollin, P.E. CD8-mediated protection against Ebola virus infection is perforin dependent. J. Immunol. 2005, 174, 4198–4202. [Google Scholar]
- Caron, J.; Loredo-Osti, J.C.; Laroche, L.; Skamene, E.; Morgan, K.; Malo, D. Identification of genetic loci controlling bacterial clearance in experimental Salmonella enteritidis infection: An unexpected role of Nramp1 (Slc11a1) in the persistence of infection in mice. Genes Immun. 2002, 3, 196–204. [Google Scholar] [CrossRef]
- Churchill, G.A.; Airey, D.C.; Allayee, H.; Angel, J.M.; Attie, A.D.; Beatty, J.; Beavis, W.D.; Belknap, J.K.; Bennett, B.; Berrettini, W.; et al. The collaborative cross, a community resource for the genetic analysis of complex traits. Nat. Genet. 2004, 36, 1133–1137. [Google Scholar]
- Ouburg, S.; Bart, A.C.J.; Klinkenberg-Knol, E.C.; Mulder, C.J.; Salvador Pena, A.; Morre, S.A. A candidate gene approach of immune mediators effecting the susceptibility to and severity of upper gastrointestinal tract diseases in relation to Helicobacter pylori and Epstein-Barr virus infections. Eur. J. Gastroenterol. Hepatol. 2005, 17, 1213–1224. [Google Scholar] [CrossRef]
- Peirce, J.L.; Lu, L.; Gu, J.; Silver, L.M.; Williams, R.W. A new set of BXD recombinant inbred lines from advanced intercross populations in mice. BMC Genet. 2004, 5, 7. [Google Scholar]
- Aziz, R.K.; Kansal, R.; Abdeltawab, N.F.; Rowe, S.L.; Su, Y.; Carrigan, D.; Nooh, M.M.; Attia, R.R.; Brannen, C.; Gardner, L.A.; et al. Susceptibility to severe Streptococcal sepsis: Use of a large set of isogenic mouse lines to study genetic and environmental factors. Genes Immun. 2007, 8, 404–415. [Google Scholar] [CrossRef]
- Abdeltawab, N.F.; Aziz, R.K.; Kansal, R.; Rowe, S.L.; Su, Y.; Gardner, L.; Brannen, C.; Nooh, M.M.; Attia, R.R.; Abdelsamed, H.A.; et al. An unbiased systems genetics approach to mapping genetic loci modulating susceptibility to severe streptococcal sepsis. PLoS Pathog. 2008, 4, e1000042. [Google Scholar] [CrossRef]
- Chesler, E.J.; Lu, L.; Shou, S.; Qu, Y.; Gu, J.; Wang, J.; Hsu, H.C.; Mountz, J.D.; Baldwin, N.E.; Langston, M.A.; et al. Complex trait analysis of gene expression uncovers polygenic and pleiotropic networks that modulate nervous system function. Nat. Genet. 2005, 37, 233–422. [Google Scholar]
- Boon, A.C.; deBeauchamp, J.; Hollmann, A.; Luke, J.; Kotb, M.; Rowe, S.; Finkelstein, D.; Neale, G.; Lu, L.; Williams, R.W.; et al. Host genetic variation affects resistance to infection with a highly pathogenic H5N1 influenza A virus in mice. J. Virol. 2009, 83, 10417–10426. [Google Scholar]
- Srivastava, B.; Blazejewska, P.; Hessmann, M.; Bruder, D.; Geffers, R.; Mauel, S.; Gruber, A.D.; Schughart, K. Host genetic background strongly influences the response to influenza a virus infections. PLoS ONE 2009, 4, e4857. [Google Scholar]
- Williams, R.W.; Gu, J.; Qi, S.; Lu, L. The genetic structure of recombinant inbred mice: High-resolution consensus maps for complex trait analysis. Genome Biol 2001, 2, 11. [Google Scholar]
- Yang, S.; Banavali, N.K.; Roux, B. Mapping the conformational transition in Src activation by cumulating the information from multiple molecular dynamics trajectories. Proc. Natl. Acad. Sci. USA 2009, 106, 3776–3781. [Google Scholar]
- Shifman, S.; Bell, J.T.; Copley, R.R.; Taylor, M.S.; Williams, R.W.; Mott, R.; Flint, J. A high-resolution single nucleotide polymorphism genetic map of the mouse genome. PLoS Biol. 2006, 4, e395. [Google Scholar] [CrossRef]
- Taylor, B.A.; Wnek, C.; Kotlus, B.S.; Roemer, N.; MacTaggart, T.; Phillips, S.J. Genotyping new BXD recombinant inbred mouse strains and comparison of BXD and consensus maps. Mamm. Genome. 1999, 10, 335–348. [Google Scholar] [CrossRef]
- Mahanty, S.; Bray, M. Pathogenesis of filoviral haemorrhagic fevers. Lancet Infect. Dis. 2004, 4, 487–498. [Google Scholar]
- Gene Network, University of Tennessee, WebQTL. Available online: www.genenetwork.org/webqul/snpBrowser.py (accessed on 29 November 2012).
- WebQTL BXD Genotypes. Available online: ftp://atlas.uthsc.edu/Public/BXD_WebQTL_Genotypes (accessed on 29 November 2012).
- Churchill, G.A.; Doerge, R.W. Empirical threshold values for quantitative trait mapping. Genetics 1994, 138, 963–971. [Google Scholar]
- Brownstein, D.G.; Bhatt, P.N.; Gras, L.; Jacoby, R.O. Chromosomal locations and gonadal dependence of genes that mediate resistance to ectromelia (mousepox) virus-induced mortality. J. Virol. 1991, 65, 1946–1951. [Google Scholar]
- Anthony, L.S.; Ghadirian, E.; Nestel, F.P.; Kongshavn, P.A. The requirement for gamma interferon in resistance of mice to experimental tularemia. Microb. Pathog. 1989, 7, 421–428. [Google Scholar] [CrossRef]
- Goudreault, M.; D'Ambrosio, L.M.; Kean, M.J.; Mullin, M.J.; Larsen, B.G.; Sanchez, A.; Chaudhry, S.; Chen, G.I.; Sicheri, F.; Nesvizhskii, A.I.; et al. A PP2A phosphatase high density interaction network identifies a novel striatin-interacting phosphatase and kinase complex linked to the cerebral cavernous malformation 3 (CCM3) protein. Mol. Cell Proteomics 2009, 8, 157–171. [Google Scholar] [CrossRef]
- Huang, J.; Liu, T.; Xu, L.G.; Chen, D.; Zhai, Z.; Shu, H.B. SIKE is an IKK epsilon/TBK1-associated suppressor of TLR3- and virus-triggered IRF-3 activation pathways. EMBO J. 2005, 24, 4018–4028. [Google Scholar] [CrossRef]
- Eid, P.; Tovey, M.G. Characterization of a domain of a human type I interferon receptor protein involved in ligand binding. J. Interferon. Cytokine. Res. 1995, 15, 205–211. [Google Scholar] [CrossRef]
- Tsuchida, T.; Zou, J.; Saitoh, T.; Kumar, H.; Abe, T.; Matsuura, Y.; Kawai, T.; Akira, S. The ubiquitin ligase TRIM56 regulates innate immune responses to intracellular double-stranded DNA. Immunity 2010, 33, 765–776. [Google Scholar] [CrossRef]
- Luo, X.; Yang, W.; Ye, D.Q.; Cui, H.; Zhang, Y.; Hirankarn, N.; Qian, X.; Tang, Y.; Lau, Y.L.; de Vries, N.; et al. A functional variant in microRNA-146a promoter modulates its expression and confers disease risk for systemic lupus erythematosus. PLoS Genet. 2011, 7, e1002128. [Google Scholar]
© 2012 by the authors; licensee MDPI, Basel, Switzerland. This article is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Zumbrun, E.E.; Abdeltawab, N.F.; Bloomfield, H.A.; Chance, T.B.; Nichols, D.K.; Harrison, P.E.; Kotb, M.; Nalca, A. Development of a Murine Model for Aerosolized Ebolavirus Infection Using a Panel of Recombinant Inbred Mice. Viruses 2012, 4, 3468-3493. https://doi.org/10.3390/v4123468
Zumbrun EE, Abdeltawab NF, Bloomfield HA, Chance TB, Nichols DK, Harrison PE, Kotb M, Nalca A. Development of a Murine Model for Aerosolized Ebolavirus Infection Using a Panel of Recombinant Inbred Mice. Viruses. 2012; 4(12):3468-3493. https://doi.org/10.3390/v4123468
Chicago/Turabian StyleZumbrun, Elizabeth E., Nourtan F. Abdeltawab, Holly A. Bloomfield, Taylor B. Chance, Donald K. Nichols, Paige E. Harrison, Malak Kotb, and Aysegul Nalca. 2012. "Development of a Murine Model for Aerosolized Ebolavirus Infection Using a Panel of Recombinant Inbred Mice" Viruses 4, no. 12: 3468-3493. https://doi.org/10.3390/v4123468




