Hunger, Food Cravings, and Diet Satisfaction are Related to Changes in Body Weight During a 6-Month Behavioral Weight Loss Intervention: The Beef WISE Study
Abstract
:1. Introduction
2. Materials and Methods
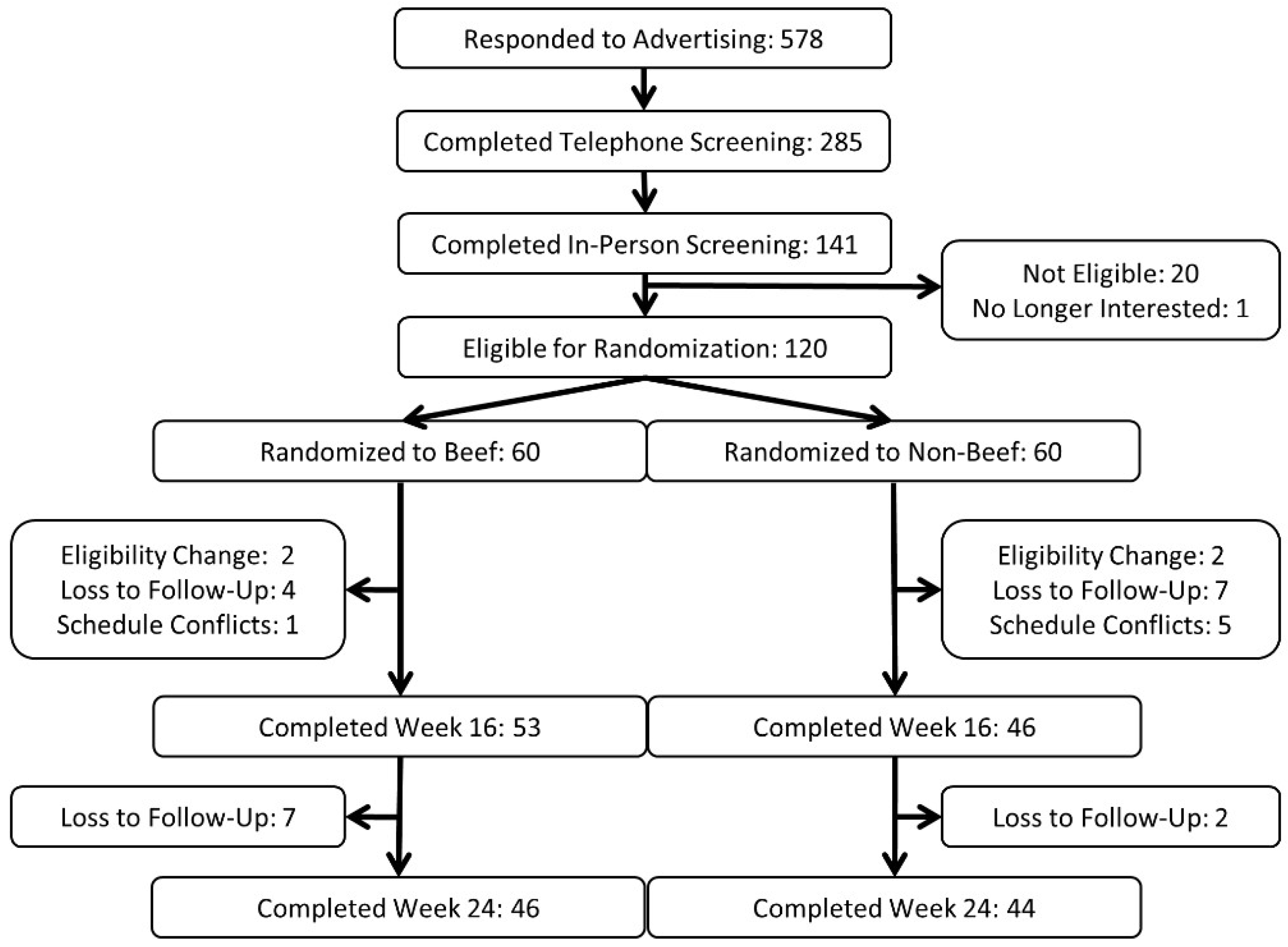
2.1. Participants
2.2. Experimental Design
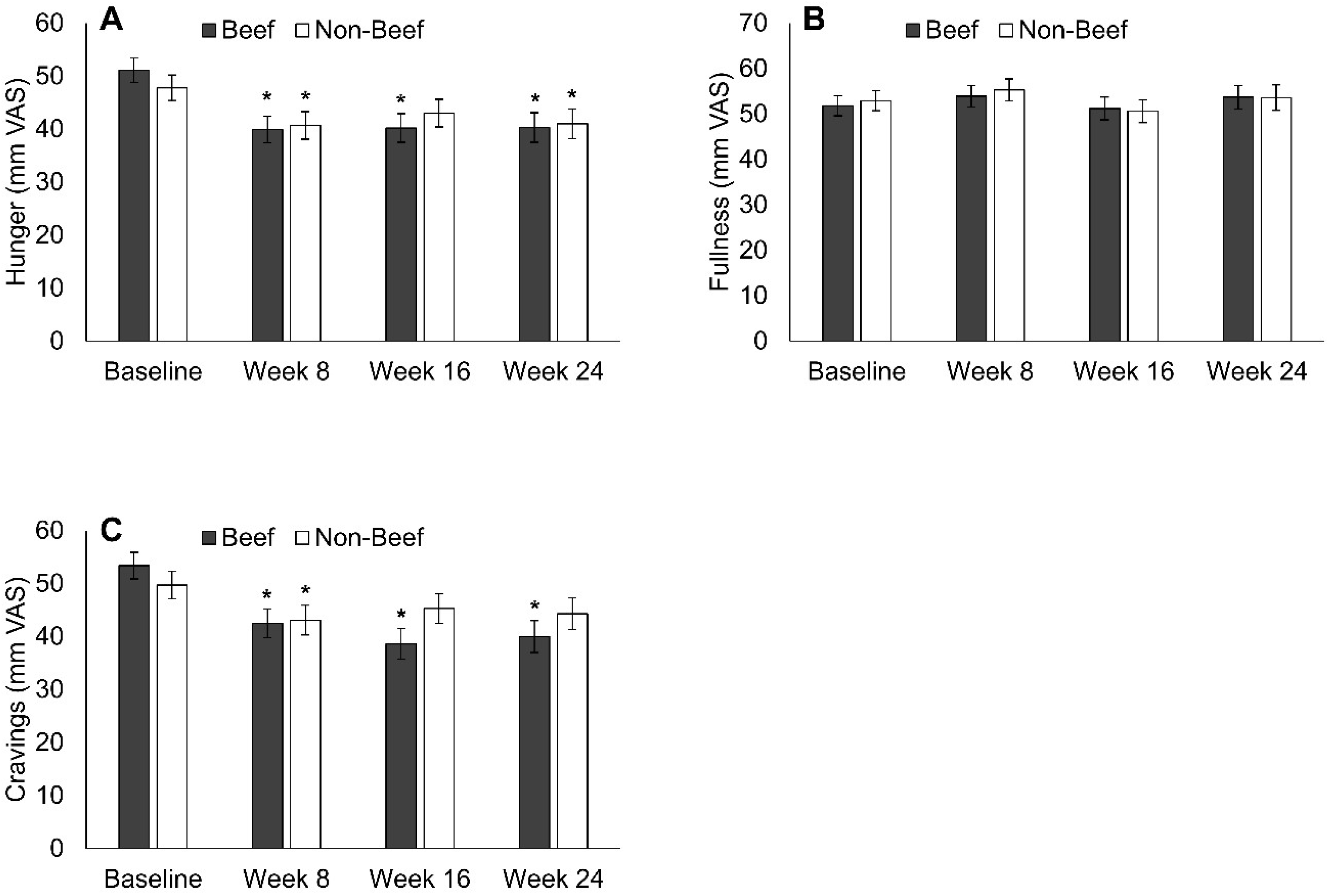
2.3. Appetite and Craving Ratings
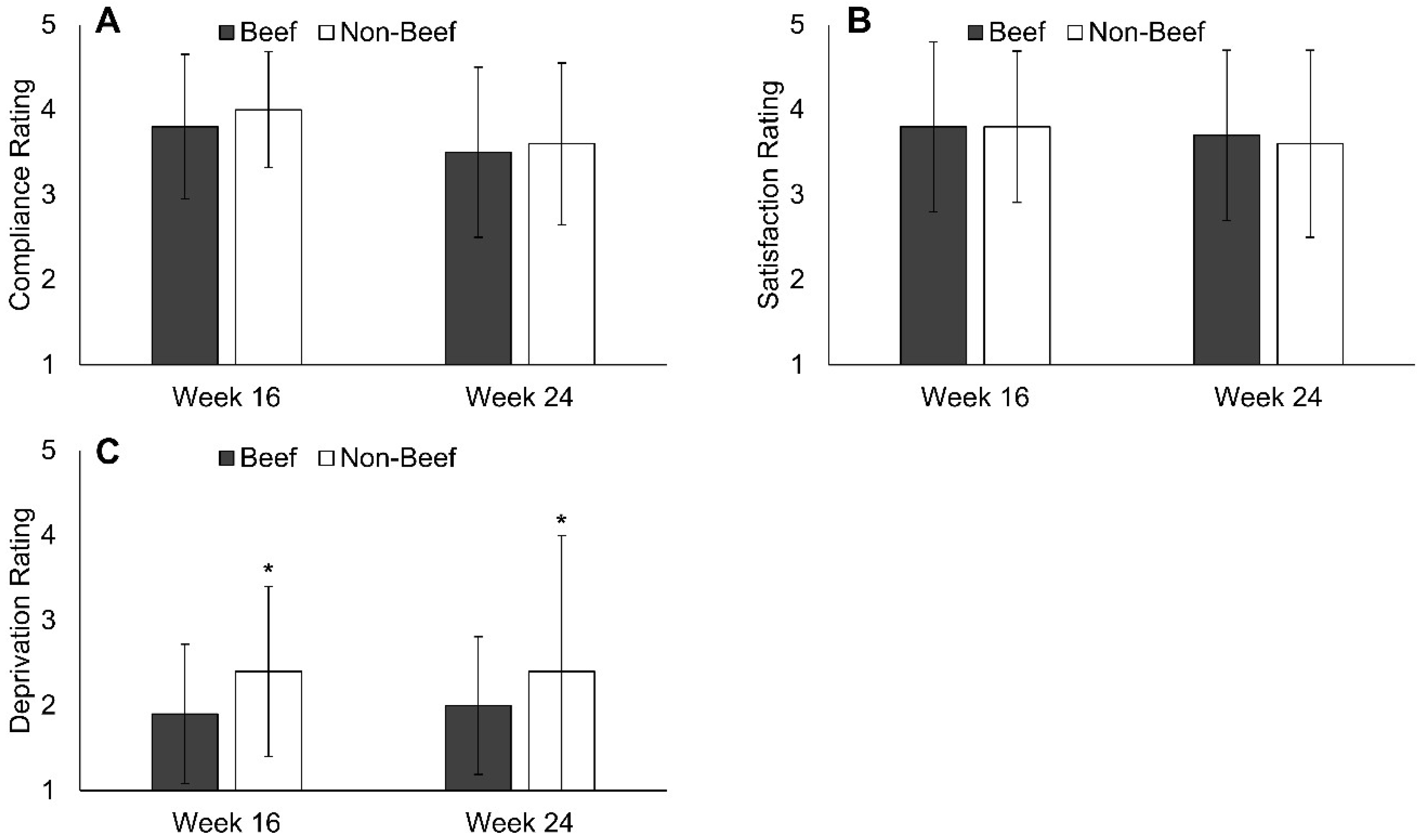
2.4. Diet Satisfaction
2.5. Anthropometric Measurements
2.6. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. Appetite and Cravings
3.3. Diet Satisfaction and Compliance
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Jensen, M.D.; Ryan, D.H.; Apovian, C.M.; Ard, J.D.; Comuzzie, A.G.; Donato, K.A.; Hu, F.B.; Hubbard, V.S.; Jakicic, J.M.; Kushner, R.F.; et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation 2014, 129, S102–S138. [Google Scholar] [CrossRef] [PubMed]
- Hooper, L.; Abdelhamid, A.; Moore, H.J.; Douthwaite, W.; Skeaff, C.M.; Summerbell, C.D. Effect of reducing total fat intake on body weight: Systematic review and meta-analysis of randomised controlled trials and cohort studies. BMJ 2012, 345, e7666. [Google Scholar] [CrossRef] [PubMed]
- Johnston, B.C.; Kanters, S.; Bandayrel, K.; Wu, P.; Naji, F.; Siemieniuk, R.A.; Ball, G.D.; Busse, J.W.; Thorlund, K.; Guyatt, G.; et al. Comparison of weight loss among named diet programs in overweight and obese adults: A meta-analysis. JAMA 2014, 312, 923–933. [Google Scholar] [CrossRef]
- Kim, J.E.; O’Connor, L.E.; Sands, L.P.; Slebodnik, M.B.; Campbell, W.W. Effects of dietary protein intake on body composition changes after weight loss in older adults: A systematic review and meta-analysis. Nutr. Rev. 2016, 74, 210–224. [Google Scholar] [CrossRef] [PubMed]
- Nordmann, A.J.; Nordmann, A.; Briel, M.; Keller, U.; Yancy, W.S.; Brehm, B.J.; Bucher, H.C. Effects of low-carbohydrate vs low-fat diets on weight loss and cardiovascular risk factors: A meta-analysis of randomized controlled trials. Arch. Intern. Med. 2006, 166, 285–293. [Google Scholar] [CrossRef]
- Schwingshackl, L.; Hoffmann, G. Comparison of effects of long-term low-fat vs high-fat diets on blood lipid levels in overweight or obese patients: A systematic review and meta-analysis. J. Acad. Nutr. Diet. 2013, 113, 1640–1661. [Google Scholar] [CrossRef] [PubMed]
- Wycherley, T.P.; Moran, L.J.; Clifton, P.M.; Noakes, M.; Brinkworth, G.D. Effects of energy-restricted high-protein, low-fat compared with standard-protein, low-fat diets: A meta-analysis of randomized controlled trials. Am. J. Clin. Nutr. 2012, 96, 1281–1298. [Google Scholar] [CrossRef] [PubMed]
- Sacks, F.M.; Bray, G.A.; Carey, V.J.; Smith, S.R.; Ryan, D.H.; Anton, S.D.; McManus, K.; Champagne, C.M.; Bishop, L.M.; Laranjo, N.; et al. Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates. N. Engl. J. Med. 2009, 360, 859–873. [Google Scholar] [CrossRef] [PubMed]
- MacLean, P.S.; Wing, R.R.; Davidson, T.; Epstein, L.; Goodpaster, B.; Hall, K.D.; Levin, B.E.; Perri, M.G.; Rolls, B.J.; Rosenbaum, M.; et al. NIH working group report: Innovative research to improve maintenance of weight loss. Obes. Silver Spring 2015, 23, 7–15. [Google Scholar] [CrossRef] [PubMed]
- Drapeau, V.; King, N.; Hetherington, M.; Doucet, E.; Blundell, J.; Tremblay, A. Appetite sensations and satiety quotient: Predictors of energy intake and weight loss. Appetite 2007, 48, 159–166. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hill, A.J. The psychology of food craving. Proc. Nutr. Soc. 2007, 66, 277–285. [Google Scholar] [CrossRef]
- Forman, E.M.; Schumacher, L.M.; Crosby, R.; Manasse, S.M.; Goldstein, S.P.; Butryn, M.L.; Wyckoff, E.P.; Graham Thomas, J. Ecological Momentary Assessment of Dietary Lapses Across Behavioral Weight Loss Treatment: Characteristics, Predictors, and Relationships with Weight Change. Ann. Behav. Med. Publ. Soc. Behav. Med. 2017. [Google Scholar] [CrossRef] [PubMed]
- Thomas, E.A.; Mcnair, B.; Bechtell, J.L.; Ferland, A.; Cornier, M.-A.; Eckel, R.H. Greater hunger and less restraint predict weight loss success with phentermine treatment. Obes. Silver Spring Md 2016, 24, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Reed, J.L.; Chaput, J.-P.; Tremblay, A.; Doucet, É. The maintenance of energy balance is compromised after weight loss. Can. J. Diabetes 2013, 37, 121–127. [Google Scholar] [CrossRef] [PubMed]
- Batra, P.; Das, S.K.; Salinardi, T.; Robinson, L.; Saltzman, E.; Scott, T.; Pittas, A.G.; Roberts, S.B. Relationship of cravings with weight loss and hunger. Results from a 6 month worksite weight loss intervention. Appetite 2013, 69, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Martin, C.K.; O’Neil, P.M.; Pawlow, L. Changes in food cravings during low-calorie and very-low-calorie diets. Obes. Silver Spring 2006, 14, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Massey, A.; Hill, A.J. Dieting and food craving. A descriptive, quasi-prospective study. Appetite 2012, 58, 781–785. [Google Scholar] [CrossRef] [PubMed]
- Anton, S.D.; Gallagher, J.; Carey, V.J.; Laranjo, N.; Cheng, J.; Champagne, C.M.; Ryan, D.H.; McManus, K.; Loria, C.M.; Bray, G.A.; et al. Diet type and changes in food cravings following weight loss: Findings from the POUNDS LOST Trial. Eat. Weight Disord. 2012, 17, e101–e108. [Google Scholar] [CrossRef] [PubMed]
- Martin, C.K.; Rosenbaum, D.; Han, H.; Geiselman, P.J.; Wyatt, H.R.; Hill, J.O.; Brill, C.; Bailer, B.; Miller, B.V.; Stein, R.; et al. Change in food cravings, food preferences, and appetite during a low-carbohydrate and low-fat diet. Obes. Silver Spring 2011, 19, 1963–1970. [Google Scholar] [CrossRef] [PubMed]
- Bruckert, E.; Pouchain, D.; Auboiron, S.; Mulet, C. Cross-analysis of dietary prescriptions and adherence in 356 hypercholesterolaemic patients. Arch. Cardiovasc. Dis. 2012, 105, 557–565. [Google Scholar] [CrossRef]
- Cheng, L.; Leung, D.Y.-P.; Sit, J.W.-H.; Li, X.-M.; Wu, Y.-N.; Yang, M.-Y.; Gao, C.-X.; Hui, R. Factors associated with diet barriers in patients with poorly controlled type 2 diabetes. Patient Prefer. Adherence 2016, 10, 37–44. [Google Scholar] [CrossRef] [PubMed]
- Leidy, H.J.; Clifton, P.M.; Astrup, A.; Wycherley, T.P.; Westerterp-Plantenga, M.S.; Luscombe-Marsh, N.D.; Woods, S.C.; Mattes, R.D. The role of protein in weight loss and maintenance. Am. J. Clin. Nutr. 2015. [Google Scholar] [CrossRef] [PubMed]
- Halton, T.L.; Hu, F.B. The effects of high protein diets on thermogenesis, satiety and weight loss: A critical review. J. Am. Coll. Nutr. 2004, 23, 373–385. [Google Scholar] [CrossRef] [PubMed]
- Hoertel, H.A.; Will, M.J.; Leidy, H.J. A randomized crossover, pilot study examining the effects of a normal protein vs. high protein breakfast on food cravings and reward signals in overweight/obese “breakfast skipping”, late-adolescent girls. Nutr. J. 2014, 13, 80. [Google Scholar] [CrossRef] [PubMed]
- McConnon, A.; Horgan, G.W.; Lawton, C.; Stubbs, J.; Shepherd, R.; Astrup, A.; Handjieva-Darlenska, T.; Kunešová, M.; Larsen, T.M.; Lindroos, A.K.; et al. Experience and acceptability of diets of varying protein content and glycemic index in an obese cohort: Results from the Diogenes trial. Eur. J. Clin. Nutr. 2013, 67, 990–995. [Google Scholar] [CrossRef] [PubMed]
- Johnston, C.S.; Tjonn, S.L.; Swan, P.D. High-protein, low-fat diets are effective for weight loss and favorably alter biomarkers in healthy adults. J. Nutr. 2004, 134, 586–591. [Google Scholar] [CrossRef] [PubMed]
- Leidy, H.J.; Carnell, N.S.; Mattes, R.D.; Campbell, W.W. Higher Protein Intake Preserves Lean Mass and Satiety with Weight Loss in Pre-obese and Obese Women. Obesity 2007, 15, 421–429. [Google Scholar] [CrossRef] [PubMed]
- Santesso, N.; Akl, E.A.; Bianchi, M.; Mente, A.; Mustafa, R.; Heels-Ansdell, D.; Schunemann, H.J. Effects of higher- versus lower-protein diets on health outcomes: A systematic review and meta-analysis. Eur. J. Clin. Nutr 2012, 66, 780–788. [Google Scholar] [CrossRef] [PubMed]
- Sayer, R.D.; Speaker, K.J.; Pan, Z.; Peters, J.C.; Wyatt, H.R.; Hill, J.O. Equivalent reductions in body weight during the Beef WISE Study: Beef’s role in weight improvement, satisfaction and energy: The Beef WISE Study. Obes. Sci. Pract. 2017. [Google Scholar] [CrossRef] [PubMed]
- Daniel, C.R.; Cross, A.J.; Koebnick, C.; Sinha, R. Trends in meat consumption in the USA. Public Health Nutr. 2011, 14, 575–583. [Google Scholar] [CrossRef] [PubMed]
- Hill, J.O.; Wyatt, H.; Aschwanden, C. State of Slim: Fix Your Metabolism and Drop 20 Pounds in 8 Weeks on the Colorado Diet; Rodale: Emmaus, PA, USA, 2013; ISBN 978-1-60961-491-1. [Google Scholar]
- Dhurandhar, N.V.; Schoeller, D.; Brown, A.W.; Heymsfield, S.B.; Thomas, D.; Sørensen, T.I.A.; Speakman, J.R.; Jeansonne, M.; Allison, D.B. Energy Balance Measurement Working Group Energy balance measurement: When something is not better than nothing. Int. J. Obes. 2005 2015, 39, 1109–1113. [Google Scholar] [CrossRef]
- Stubbs, R.J.; Hughes, D.A.; Johnstone, A.M.; Rowley, E.; Reid, C.; Elia, M.; Stratton, R.; Delargy, H.; King, N.; Blundell, J.E. The use of visual analogue scales to assess motivation to eat in human subjects: A review of their reliability and validity with an evaluation of new hand-held computerized systems for temporal tracking of appetite ratings. Br. J. Nutr. 2000, 84, 405–415. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Maclean, P.S.; Bergouignan, A.; Cornier, M.A.; Jackman, M.R. Biology’s response to dieting: The impetus for weight regain. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2011, 301, R581–R600. [Google Scholar] [CrossRef] [PubMed]
- MacLean, P.S.; Rothman, A.J.; Nicastro, H.L.; Czajkowski, S.M.; Agurs-Collins, T.; Rice, E.L.; Courcoulas, A.P.; Ryan, D.H.; Bessesen, D.H.; Loria, C.M. The Accumulating Data to Optimally Predict Obesity Treatment (ADOPT) Core Measures Project: Rationale and Approach. Obes. Silver Spring 2018, 26 (Suppl. 2), S6–S15. [Google Scholar] [CrossRef] [PubMed]
- Sutin, A.R.; Boutelle, K.; Czajkowski, S.M.; Epel, E.S.; Green, P.A.; Hunter, C.M.; Rice, E.L.; Williams, D.M.; Young-Hyman, D.; Rothman, A.J. Accumulating Data to Optimally Predict Obesity Treatment (ADOPT) Core Measures: Psychosocial Domain. Obes. Silver Spring 2018, 26 (Suppl. 2), S45–S54. [Google Scholar] [CrossRef] [PubMed]
- Hill, J.O.; Thompson, H.; Wyatt, H. Weight maintenance: What’s missing? J. Am. Diet. Assoc. 2005, 105, S63–S66. [Google Scholar] [CrossRef] [PubMed]
- Interagency Committee on Human Nutrition Research. National Nutrition Research Roadmap 2016‒2021: Advancing Nutrition Research to Improve and Sustain Health; Interagency Committee on Human Nutrition Research: Washington, DC, USA, 2016. [Google Scholar]
| Parameter | All | Beef | Non-Beef |
|---|---|---|---|
| Sample Size (# Female) | 120 (99) | 60 (49) | 60 (50) |
| Age (year) | 37.6 ± 8.1 | 36.0 ± 8.3 | 39.3 ± 7.8 * |
| Body Weight (kg) | 101.1 ± 22.8 | 100.8 ± 21.9 | 101.5 ± 24.0 |
| BMI (kg/m2) | 35.7 ± 7.0 | 35.9 ± 6.8 | 35.4 ± 7.1 |
| Parameter | Pearson r for Week 16 Weight Loss | p Value for Week 16 Weight Loss | Pearson r for Week 24 Weight Loss | p Value for Week 24 Weight Loss |
|---|---|---|---|---|
| Hunger | ||||
| Baseline | −0.22 * | 0.031 | −0.29 * | 0.007 |
| Week 16 | −0.13 | 0.233 | −0.17 | 0.123 |
| Week 24 | -- | -- | −0.25 * | 0.033 |
| Fullness | ||||
| Baseline | −0.11 | 0.280 | −0.13 | 0.250 |
| Week 16 | −0.17 | 0.132 | −0.06 | 0.627 |
| Week 24 | -- | -- | −0.06 | 0.586 |
| Food Cravings | ||||
| Baseline | −0.20 * | 0.048 | −0.23 * | 0.037 |
| Week 16 | −0.08 | 0.497 | −0.11 | 0.312 |
| Week 24 | -- | -- | −0.14 | 0.228 |
| Parameter | Pearson r for Week 16 Weight Loss | p Value for Week 16 Weight Loss | Pearson r for Week 24 Weight Loss | p Value for Week 24 Weight Loss |
|---|---|---|---|---|
| Compliance | 0.52 * | <0.001 | 0.52 * | <0.001 |
| Satisfaction | 0.33 * | 0.001 | 0.32 * | 0.002 |
| Deprivation | −0.21 * | 0.043 | −0.24 * | 0.028 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sayer, R.D.; Peters, J.C.; Pan, Z.; Wyatt, H.R.; Hill, J.O. Hunger, Food Cravings, and Diet Satisfaction are Related to Changes in Body Weight During a 6-Month Behavioral Weight Loss Intervention: The Beef WISE Study. Nutrients 2018, 10, 700. https://doi.org/10.3390/nu10060700
Sayer RD, Peters JC, Pan Z, Wyatt HR, Hill JO. Hunger, Food Cravings, and Diet Satisfaction are Related to Changes in Body Weight During a 6-Month Behavioral Weight Loss Intervention: The Beef WISE Study. Nutrients. 2018; 10(6):700. https://doi.org/10.3390/nu10060700
Chicago/Turabian StyleSayer, R. Drew, John C. Peters, Zhaoxing Pan, Holly R. Wyatt, and James O. Hill. 2018. "Hunger, Food Cravings, and Diet Satisfaction are Related to Changes in Body Weight During a 6-Month Behavioral Weight Loss Intervention: The Beef WISE Study" Nutrients 10, no. 6: 700. https://doi.org/10.3390/nu10060700





