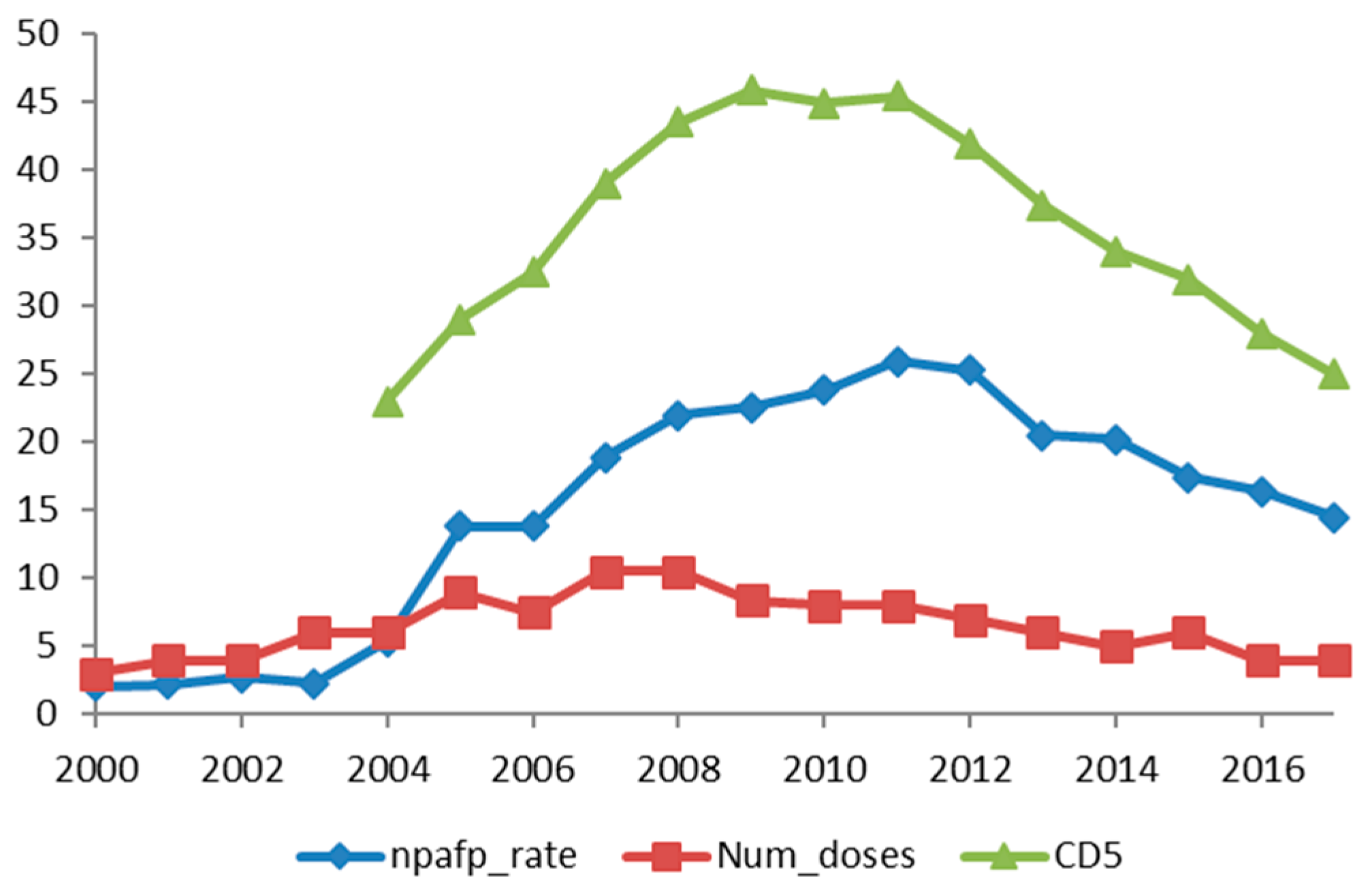
Correlation between Non-Polio Acute Flaccid Paralysis Rates with Pulse Polio Frequency in India
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Horsemann, D.M.; Paul, J.R. The incubation period in human poliomyelitis and its implications. J. Am. Med. Assoc. 1947, 135, 11–14. [Google Scholar] [CrossRef]
- Banerjee, K.; Hlady, W.G.; Andrus, J.K.; Sarkar, S.; Fitzsimmons, J.; Abeykoon, P. Poliomyelitis surveillance: The model used in India for polio eradication. Bull. World Health Organ. 2000, 78, 321–329. [Google Scholar] [PubMed]
- Tangermann, R.H.; Lamoureux, C.; Tallis, G.; Goel, A. The critical role of acute flaccid paralysis surveillance in the Global Polio Eradication Initiative. Int. Health 2017, 9, 156–163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahmad, A.; Rehman, A. One year surveillance data of acute flaccid paralysis at Bahwal Victoria Hospital Bahawalpur Pakistan. J. Med. Sci. 2007, 23, 308–312. [Google Scholar]
- Canadian Pediatric Society. Surveillance Canadian Pediatric Surveillance Programme Acute Flaccid Paralysis. Available online: http://www.cps.ca/english/Surveillance/CPSP/Studies/acute.htm (accessed on 25 May 2018).
- Marx, A.; Glass, J.D.; Sutter, R.W. Differential diagnosis of acute flaccid paralysis and its role in poliomyelitis surveillance. Epidemiol. Rev. 2000, 2, 298–316. [Google Scholar] [CrossRef]
- WHO-Recommended Surveillance Standard of Poliomyelitis. Available online: http://www.who.int/immunization/monitoring_surveillance/burden/vpd/surveillance_type/active/poliomyelitis_standards/en/ (accessed on 25 May 2018).
- Pan American Health Organisation and World Health Organisations. Polio Weekly Bulletin. Available online: https://www.paho.org/hq/index.php?option=com_content&view=article&view=article&id=295&Itemid=3626&lang=en (accessed on 25 May 2018).
- Kennedy, R.H.; Danielson, M.A.; Mulder, D.W.; Kurland, L.T. Guillain-Barre syndrome: A 42-year epidemiologic and clinical study. Mayo. Clin. Proc. 1978, 53, 93–99. [Google Scholar] [PubMed]
- Alcala, H. The differential diagnosis of poliomyelitis and other flaccid paralysis. Biol. Med. Infant Mex. 1993, 50, 136–144. [Google Scholar]
- Vikram, R. World Bank. A Polio-Free India Is One of the Biggest Achievements in Global Health May 29, 2014. Available online: http://www.worldbank.org/en/news/feature/2014/05/29/polio-free-india-biggest-achievements-global-health (accessed on 30 May 2018).
- Vashisht, N.; Puliyel, J. Polio programme: Let us declare victory and move on Indian. J. Med. Ethics 2012, 9, 114–117. [Google Scholar] [CrossRef] [PubMed]
- Puliyel, J.; Sathyamala, C.; Banerji, D. Protective efficacy of a monovalent oral type 1 poliovirus vaccine. Lancet 2007, 370, 129–130. [Google Scholar] [CrossRef]
- Grassly, N.C.; Wenger, J.; Bahl, S.; Sutter, R.W.; Aylward, R.B. Protective efficacy of a monovalent oral type 1 poliovirus vaccine Authors reply. Lancet 2007, 370, 129–130. [Google Scholar] [CrossRef]
- Puliyel, J.M.; Gupta, M.A.; Mathew, J.L. Polio eradication and the future for other programmes: Situation analysis for strategic planning in India. Indian J. Med. Res. 2007, 125, 1–4. [Google Scholar] [PubMed]
- Sathyamala, C. Polio eradication programme in India. Indian J. Med. Res. 2007, 125, 695–696. [Google Scholar] [PubMed]
- Naranjo, C.A.; Busto, U.; Sellers, E.M.; Sandor, P.; Ruiz, I.; Roberts, E.A.; Janecek, E.; Domecq, C.; Greenblatt, D.J. A method for estimating the probability of adverse drug reactions. Clin Pharmacol. Ther. 1981, 30, 239–245. [Google Scholar] [CrossRef] [PubMed]
- Kinnunen, E.; Farkkila, M.; Hovi, T.; Juntunen, J.; Weckstrom, P. Incidence of Guillain-Barré syndrome during a nationwide oral poliovirus vaccine campaign. Neurology 1989, 39, 1034–1036. [Google Scholar] [CrossRef] [PubMed]
- Uhari, M.; Rantala, H.; Niemela, M. Cluster of childhood Guillain-Barré cases after an oral poliovaccine campaign (letter). Lancet 1989, 2, 440–441. [Google Scholar] [CrossRef]
- Anlar, O.; Tombul, T.; Arslan, S.; Akdeniz, H.; Caksen, H.; Gundem, A.; Akbayram, S. Report of five children with Guillain-Barré syndrome following a nationwide oral polio vaccine campaign in Turkey. Neurol. India 2003, 51, 544–555. [Google Scholar] [PubMed]
- Institute of Medicine (US) Vaccine Safety Committee. Adverse Events Associated with Childhood Vaccines Evidence Bearing on Causality; Stratton, K.R., Howe, C.J., Johnston, R.B., Jr., Eds.; National Academies Press (US): Washington, DC, USA, 1994; ISBN-10 0-309-04895-8. [Google Scholar]
- Vashisht, N.; Puliyel, J.; Sreenivas, V. Trends in non-polio acute flaccid paralysis incidence in India 2000–2013. F1000 Res. (Poster) 2018, 7, 202, doi:10.7490/f1000research.1115276.1. Pediatrics 2015, 135 (Suppl. S1), S16–S17. [Google Scholar] [CrossRef]

| Serial No. | Number of Years of Cumulative Doses | NPAFP Rate Regression Coefficient R | p Value |
|---|---|---|---|
| 1 | 1 Year | 0.52 | p < 0.001 |
| 2 | 2 Years | 0.60 | p < 0.001 |
| 3 | 3 Years | 0.67 | p < 0.001 |
| 4 | 4 Years | 0.72 | p < 0.001 |
| 5 | 5 Years | 0.76 | p < 0.001 |
| 6 | 6 Years | 0.75 | p < 0.001 |
| Year | AFP Rate | NPAFP Rate | AFP | NPAFP | Expected NPAFP | Excess NPAFP |
|---|---|---|---|---|---|---|
| 2000 | 2.16 | 1.94 | 7260 | 7485 | −225 | |
| 2001 | 1.91 | 1.75 | 7510 | 6858 | 7838 | −980 |
| 2002 | 2.45 | 1.87 | 9713 | 7404 | 7919 | −515 |
| October 2003 | 2.11 | 1.67 | 6850 | 5417 | 6487 | −1070 |
| 2004 | 3.24 | 3.11 | 13,274 | 12,765 | 8209 | 4556 |
| 2005 | 6.54 | 6.43 | 27,049 | 26,586 | 8269 | 18,317 |
| 2006 | 7.63 | 7.35 | 32,194 | 31,024 | 8442 | 22,582 |
| 2007 | 9.71 | 9.32 | 41,534 | 39,831 | 8547 | 31,284 |
| 2008 | 10.5 | 9.93 | 45,586 | 43,103 | 8681 | 34,422 |
| 2008 | 11.64 | 11.33 | 50,412 | 49,082 | 8664 | 40,418 |
| 2010 | 12.7 | 12.65 | 55,785 | 55,548 | 8782 | 46,766 |
| 2011 | 13.55 | 13.35 | 60,750 | 59,849 | 8966 | 50,883 |
| 2012 | 13.97 | 13.61 | 61,038 | 59,462 | 8738 | 50,724 |
| 2013 | 12.51 | 12.48 | 54,645 | 54,511 | 8736 | 45,775 |
| 2014 | 12.48 | 12.48 | 53,933 | 53,910 | 8639 | 45,271 |
| 2015 | 10.78 | 10.77 | 46,970 | 46,957 | 8720 | 38,237 |
| 2016 | 10.61 | 10.16 | 46,524 | 44,571 | 8774 | 35,797 |
| 2017 | 8.97 | 8.72 | 39,339 | 38,232 | 8769 | 29,463 |
| Totals | 653,106 | 642,370 | 150,666 | 49,1704 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dhiman, R.; Prakash, S.C.; Sreenivas, V.; Puliyel, J. Correlation between Non-Polio Acute Flaccid Paralysis Rates with Pulse Polio Frequency in India. Int. J. Environ. Res. Public Health 2018, 15, 1755. https://doi.org/10.3390/ijerph15081755
Dhiman R, Prakash SC, Sreenivas V, Puliyel J. Correlation between Non-Polio Acute Flaccid Paralysis Rates with Pulse Polio Frequency in India. International Journal of Environmental Research and Public Health. 2018; 15(8):1755. https://doi.org/10.3390/ijerph15081755
Chicago/Turabian StyleDhiman, Rachana, Sandeep C. Prakash, V. Sreenivas, and Jacob Puliyel. 2018. "Correlation between Non-Polio Acute Flaccid Paralysis Rates with Pulse Polio Frequency in India" International Journal of Environmental Research and Public Health 15, no. 8: 1755. https://doi.org/10.3390/ijerph15081755





