Factors Influencing Anti-Malarial Prophylaxis and Iron Supplementation Non-Compliance among Pregnant Women in Simiyu Region, Tanzania
Abstract
:1. Introduction
2. Methods
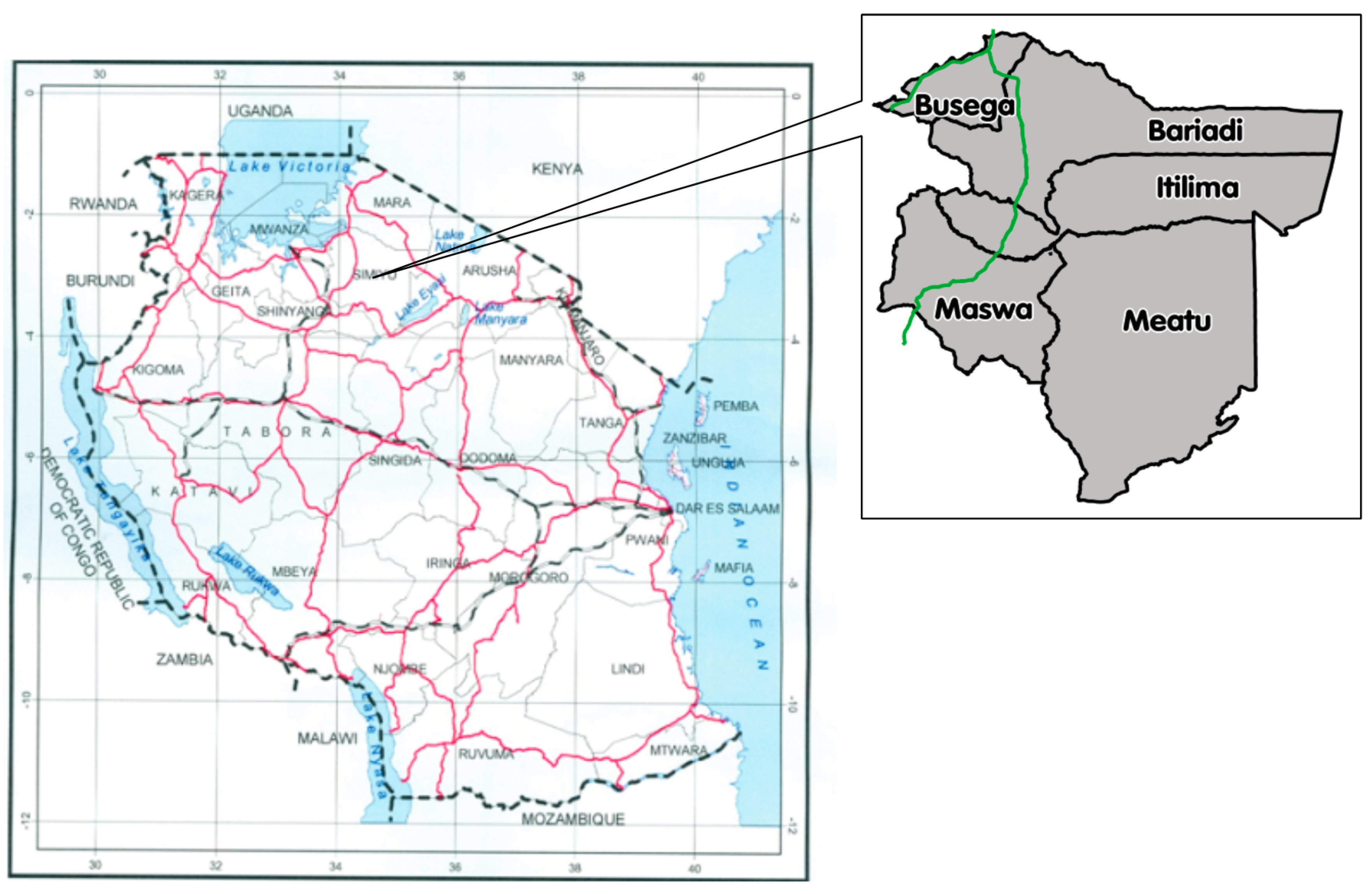
2.1. Study Design and Settings
2.2. Study Population and Sampling
2.3. Data Collection
2.4. Ethical Considerations
2.5. Data Processing and Analysis
3. Results
3.1. Socio-Demographic Characteristics of Study Participants
3.2. Pregnancy Status and Delivery
3.3. ANC Attendance during the Previous Pregnancy
3.4. Anti-Malarial Prophylaxis and Iron Tablets Medication Non-Compliance
3.5. Iron Supplement and Health Education
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- World Health Organization. Assessing the Iron Status of Populations—Including Literature Reviews: Report of a Joint World Health Organization/Centers for Disease Control and Prevention Technical Consultation on the Assessment of Iron Status at the Population Level; World Health Organization: Geneva, Switzerland, 2004. [Google Scholar]
- World Health Organization. The Global Prevalence of Anaemia in 2011; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- McLean, E.; Cogswell, M.; Egli, I.; Wojdla, D.; de Benoist, B. Worldwide prevalence of anaemia, WHO vitamin and mineral nutrition information system, 1993–2005. Public Health Nutr. 2009, 12, 444–454. [Google Scholar] [CrossRef] [PubMed]
- Galloway, R.; McGuire, J. Determinants of compliance with iron supplementation: Supplies, side effects, or psychology? Soc. Sci. Med. 1994, 39, 381–390. [Google Scholar] [CrossRef]
- Tanzania National Bureau of Statistics (NBS); ICF Macro. Tanzania Demographic and Health Survey 2010; INBS and ICF Macro: Dar es Salaam, Tanzania, 2011.
- Allen, L.H. Anemia and iron deficiency: Effects on pregnancy outcome. Am. J. Clin. Nutr. 2000, 71, 1280–1284. [Google Scholar]
- Oppenheimer, S.J. Iron and its relation to immunity and infectious disease. J. Nutr. 2001, 131, 616–635. [Google Scholar]
- Gillespie, S.; Kevany, J.; Mason, J. Controlling Iron Deficiency—Nutrition Policy Discussion Paper No. 9; The Lavenham Press Ltd.: Geneva, Switzerland, 1991. [Google Scholar]
- Galloway, R.; Dusch, E.; Elder, L.; Acha, E.; Grajeda, R.; Hurtado, E.; Favin, M.; Kanani, S.; Marsaban, J.; Meda, N.; Moore, K.N.; et al. Women’s perceptions of iron deficiency and anemia prevention and control in eight developing countries. Soc. Sci. Med. 2002, 55, 529–544. [Google Scholar] [CrossRef]
- World Health Organization. Standards for Maternal and Neonatal Care—Group 1: General Standards of Care for Healthy Pregnancy and Childbirth; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- Tanzania Ministry of Health and Social Welfare. The National Road Map Strategic Plan: 2008–2015; MOHSW: Dar es Salaam, Tanzania, 2008.
- Holtz, T.H.; Kachur, S.P.; Roberts, J.M.; Marum, L.H.; Mkandala, C.; Chizani, N.; Macheso, A.; Parise, M.E. Use of antenatal care services and intermittent preventive treatment for malaria among pregnant women in Blantyre district, Malawi. Trop. Med. Int. Health 2004, 9, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Helitzer-Allen, D.L.; McFarland, D.A.; Wilima, J.J.; Macheso, A.P. Malaria chemoprophylaxis compliance in pregnant women: A cost-effectiveness analysis of alternative interventions. Soc. Sci. Med. 1993, 36, 403–407. [Google Scholar] [CrossRef]
- Steketee, R.W.; Nahlen, B.L.; Parise, M.E.; Menendez, C. The burden of malaria in pregnancy in malaria-endemic areas. Am. J. Trop. Med. Hyg. 2001, 64, 28–35. [Google Scholar] [PubMed]
- Olsen, B.E.; Hinderaker, S.G.; Bergsjo, P.; Lie, R.T.; Olsen, O.H.; Gasheka, P.; Kvale, G. Causes and characteristics of maternal deaths in rural northern Tanzania. Acta. Obstet. Gynecol. Scand. 2002, 81, 1101–1109. [Google Scholar] [CrossRef] [PubMed]
- Launiala, A.; Honkasalo, M.L. Ethnographic study of factors influencing compliance to intermittent preventive treatment of malaria during pregnancy among Yao women in rural Malawi. Trans. R. Soc. Trop. Med. Hyg. 2007, 101, 980–989. [Google Scholar] [CrossRef] [PubMed]
- Heymann, D.L.; McFarland, D.A.; Wilima, J.J.; Macheso, A.P. Antenatal chloroquine chemoprophylaxis in Malawi: Chloroquine resistance, compliance, protective efficacy and cost. Trans. Res. Soc. Trop. Med. Hyg. 1990, 84, 496–498. [Google Scholar] [CrossRef]
- National Bereau of Statistics and Office of Government’s Chief Statistician. 2012 Population and Housing Census: Population Distribution by Administrative Areas; NBS: Dar es Salaam, Tanzania, 2013.
- National Bureau of Statistics and Office of the Chief Government Statistician—Zanzibar. Tanzania Demographic and Health Survey 2004–2005; NBS: Dar es Salaam, Tanzania, 2005.
- Tanzanian Ministry of Lands, Housing and Human Settlements Development. The Government Offial Blog. Available online: http://tanzaniangovernment.blogspot.com/2016/05/ramani-rasmi-ya-tanzania.html (accessed on 21 June 2016).
- Malaria Consortium. Tanzania Roll Back Malaria Consultative Mission Report; Malaria Consortium: London, UK, 2004; p. 17. [Google Scholar]
- Onoka, C.A.; Hanson, K.; Onwujekwe, O.E. Low coverage of intermittent preventive treatment for malaria in pregnancy in Nigeria: Demand-side influences. Malar. J. 2012, 11, 82. [Google Scholar] [CrossRef] [PubMed]
- Mubyazi, G.; Bloch, P.; Kamugisha, M.; Kitua, A.; Ijumba, J. Intermittent preventive treatment of malaria during pregnancy: A qualitative study of knowledge, attitudes and practices of district health managers, antenatal care staff and pregnant women in Korogwe district, north-eastern Tanzania. Malar. J. 2005, 4, 31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- RamaRao, S.; Caleb, L.; Khan, M.; Townsend, J.W. Safer maternal health in rural Uttar Pradesh: Do primary health services contribute? Health Policy Plan. 2001, 16, 256–263. [Google Scholar] [CrossRef] [PubMed]
- De Savigny, D.; Mayombana, C.; Mwageni, E.; Masanja, H.; Minhaj, A.; Mkilindi, Y.; Mbuya, C.; Kasale, H.; Reid, G. Care-seeking patterns for fatal malaria in Tanzania. Malar. J. 2004, 3, 27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hill, J.; Hoyt, J.; van Ejik, M.A.; D’Mello-Guett, L.; ter Kuile, O.F.; Steketee, R.; Smith, H.; Webster, J. Factors affecting the delivery, access, and use of interventions to prevent malaria in pregnancy in sub-Saharan Africa: A systematic review and meta-analysis. PLoS Med. 2013, 10, e1001488. [Google Scholar]
- Iliyasu, Z.; Gajida, A.U.; Galadanci, H.S.; Abubakari, A.S.; Baba, A.S.; Jibo, A.M.; Aliyu, M.H. Adherence to intermittent preventive treatment for malaria in pregnancy in urban Kano, Northern Nigeria. Pathog. Glob. Health 2012, 106, 323–329. [Google Scholar] [CrossRef] [PubMed]
- Grietens, K.P.; Gies, S.; Coulibaly, O.S.; Ky, C.; Somda, J.; Toomer, E.; Ribera, J.M.; D’Alessandro, U. Bottlenecks for high coverage of intermittent preventive treatment in pregnancy: The case of adolescent pregnancies in rural Burkina Faso. PLoS ONE 2010, 5, e12013. [Google Scholar] [CrossRef] [PubMed]
- Amoran, O.E.; Ariba, A.A.; Iyaniwura, C.A. Determinants of intermittent preventive treatment of malaria during pregnancy (IPTp) utilization in a rural town in western Nigeria. Reprod. Health 2012, 9, 12. [Google Scholar] [CrossRef] [PubMed]
- Nagata, J.M.; Gatti, L.R.; Barg, F.K. Social determinants of iron supplementation among women of reproductive age: A systematic review of qualitative data. Matern. Child. Nutr. 2012, 8, 1–18. [Google Scholar] [CrossRef] [PubMed]


| Background Variables | n = 430 | % |
|---|---|---|
| Age (in years) | ||
| 15–24 | 142 | 33.1 |
| 25–34 | 146 | 34.0 |
| ≥35 | 142 | 32.9 |
| Education | ||
| No education | 167 | 38.8 |
| Some primary school | 69 | 16.0 |
| Completed primary school | 150 | 34.9 |
| Secondary and above | 44 | 10.2 |
| District of residence | ||
| Bariadi | 88 | 20.5 |
| Busega | 83 | 19.3 |
| Itilima | 87 | 20.2 |
| Maswa | 93 | 21.6 |
| Meatu | 79 | 18.4 |
| Ever given birth | ||
| No | 59 | 13.8 |
| Yes | 369 | 86.2 |
| Number of biological children | ||
| 1–2 | 128 | 34.7 |
| 3–5 | 140 | 37.9 |
| ≥6 | 101 | 27.4 |
| Living with their children | ||
| No | 32 | 8.8 |
| Yes | 331 | 91.2 |
| Women whose children died within a month of delivery | ||
| No | 383 | 89.1 |
| Yes | 47 | 10.9 |
| Women whose children died after delivery | ||
| No | 406 | 94.4 |
| Yes | 24 | 5.6 |
| Pregnancy Variables | n = 430 | % |
|---|---|---|
| Are you pregnant now? | ||
| No | 391 | 90.9 |
| Yes | 39 | 9.1 |
| Gestation age | ||
| 1st trimester | 15 | 38.5 |
| 2nd trimester | 7 | 18.0 |
| 3rd trimester | 17 | 43.6 |
| Place of birth of the last child | ||
| Home | 85 | 23.0 |
| Traditional birth attendant | 71 | 19.2 |
| Health facility | 212 | 57.5 |
| others | 1 | 0.3 |
| Reasons for home delivery | ||
| Heath facility is far from home | 32 | 37.7 |
| I did not have money for transport | 9 | 10.6 |
| Services at health facility are poor | 2 | 2.4 |
| Others | 42 | 49.4 |
| Anti-Malarial Variables | n = 228 | % |
|---|---|---|
| Were anti-malaria prophylaxis received during ANC visits? | ||
| Yes | 150 | 65.8 |
| No | 78 | 34.2 |
| Self-reported type of anti-malaria prophylaxis received | ||
| SP | 127 | 84.7 |
| Other prophylaxis | 23 | 15.3 |
| If received, was it swallowed? | ||
| Yes | 100 | 66.7 |
| No | 50 | 33.3 |
| How many doses did you swallow? | ||
| One | 62 | 62.0 |
| Two | 27 | 27.0 |
| Three | 11 | 11.0 |
| Why you did not swallow? | ||
| I did not like them | 13 | 26.0 |
| Fear of miscarriage | 6 | 12.0 |
| My husband did not allow me | 10 | 20.0 |
| Other reasons | 21 | 41.0 |
| Type of Service Provided | n = 228 | % |
|---|---|---|
| Was iron supplements provided during ANC visits? | ||
| Yes | 103 | 45.2 |
| No | 125 | 54.8 |
| Duration iron supplements were used | ||
| <3 months | 95 | 92.8 |
| ≥3 months | 8 | 7.2 |
| Were iron supplements taken as advised? | ||
| Yes | 73 | 70.9 |
| No | 30 | 29.1 |
| Why you did not take iron supplements as advised? | ||
| I did not like them | 7 | 23.6 |
| They made me sick | 14 | 46.7 |
| They caused other health problems | 5 | 16.7 |
| Other reasons | 4 | 13.3 |
| Were the health education provided during ANC visits? | ||
| Yes | 77 | 33.8 |
| No | 151 | 66.2 |
| Was nutrition education provided during ANC visits? | ||
| Yes | 98 | 43 |
| No | 130 | 57 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sambili, B.; Kimambo, R.; Peng, Y.; Ishunga, E.; Matasha, E.; Matumu, G.; Noronha, R.; Ngilangwa, D.P. Factors Influencing Anti-Malarial Prophylaxis and Iron Supplementation Non-Compliance among Pregnant Women in Simiyu Region, Tanzania. Int. J. Environ. Res. Public Health 2016, 13, 626. https://doi.org/10.3390/ijerph13070626
Sambili B, Kimambo R, Peng Y, Ishunga E, Matasha E, Matumu G, Noronha R, Ngilangwa DP. Factors Influencing Anti-Malarial Prophylaxis and Iron Supplementation Non-Compliance among Pregnant Women in Simiyu Region, Tanzania. International Journal of Environmental Research and Public Health. 2016; 13(7):626. https://doi.org/10.3390/ijerph13070626
Chicago/Turabian StyleSambili, Benatus, Ronald Kimambo, Yun Peng, Elison Ishunga, Edna Matasha, Godfrey Matumu, Rita Noronha, and David P. Ngilangwa. 2016. "Factors Influencing Anti-Malarial Prophylaxis and Iron Supplementation Non-Compliance among Pregnant Women in Simiyu Region, Tanzania" International Journal of Environmental Research and Public Health 13, no. 7: 626. https://doi.org/10.3390/ijerph13070626






