The Knowledge Base for Achieving the Sustainable Development Goal Targets on Water Supply, Sanitation and Hygiene
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Status of Drinking-Water, Sanitation, and Hygiene
3.1.1. Targets
3.1.2. Definitions
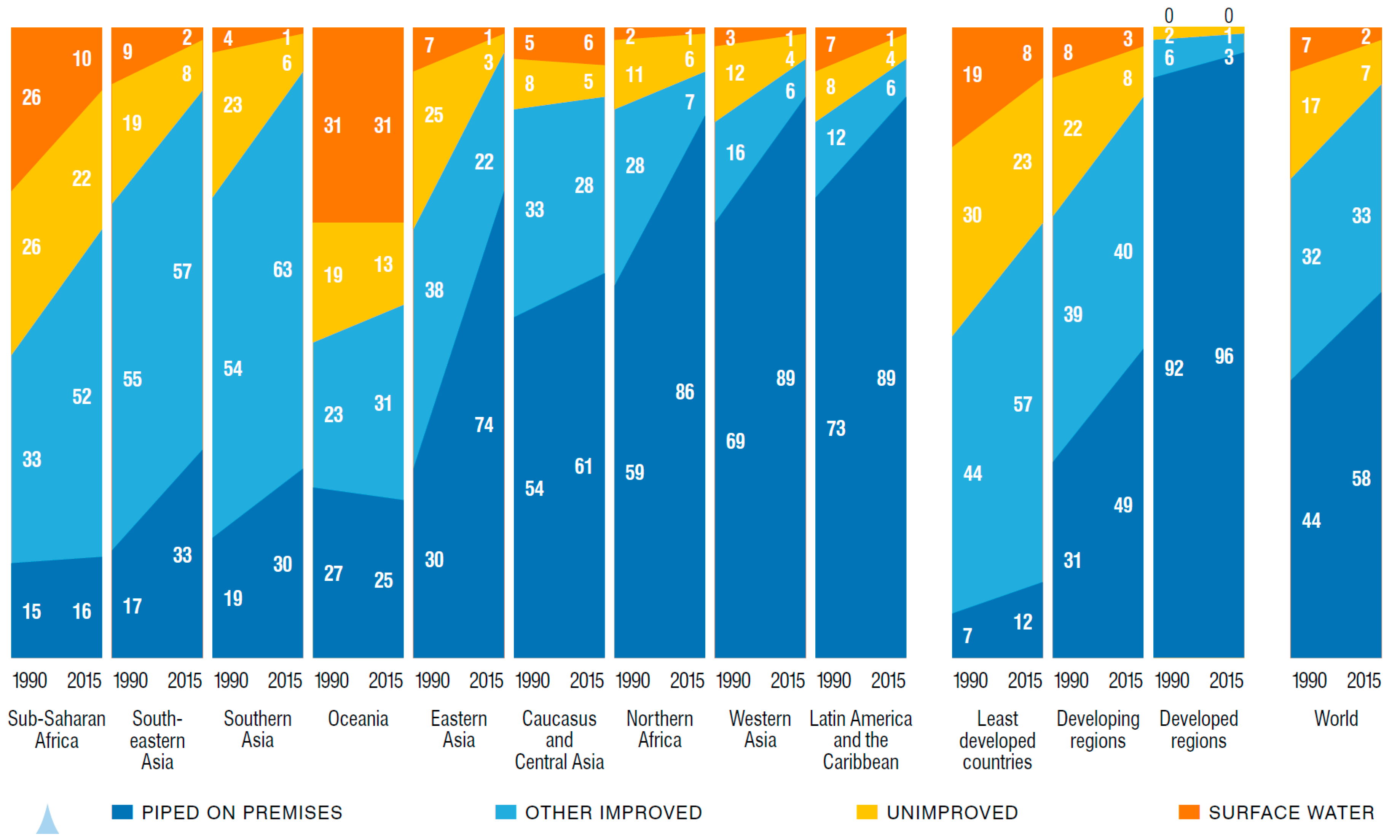
3.1.3. Coverage of Water Supply
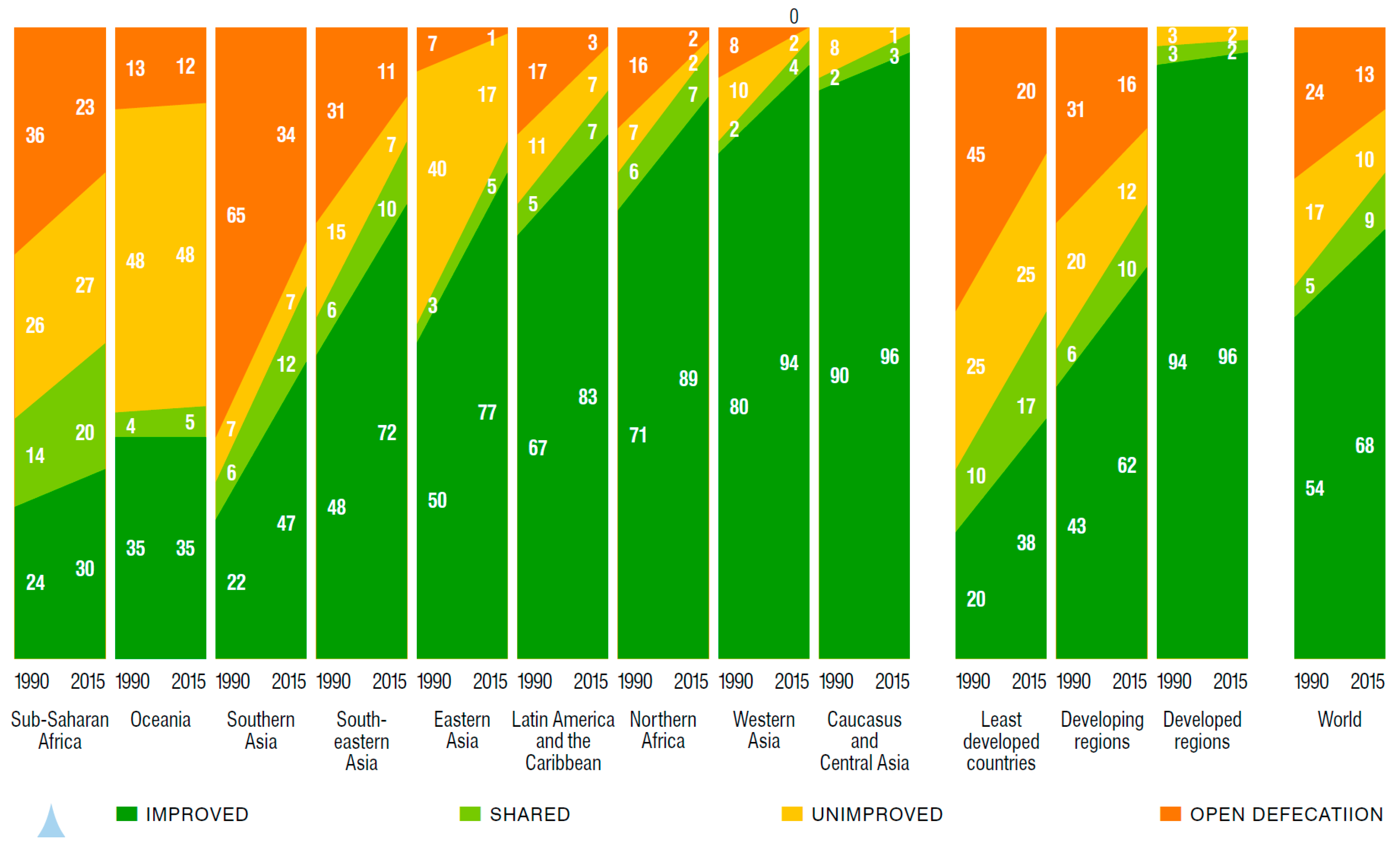
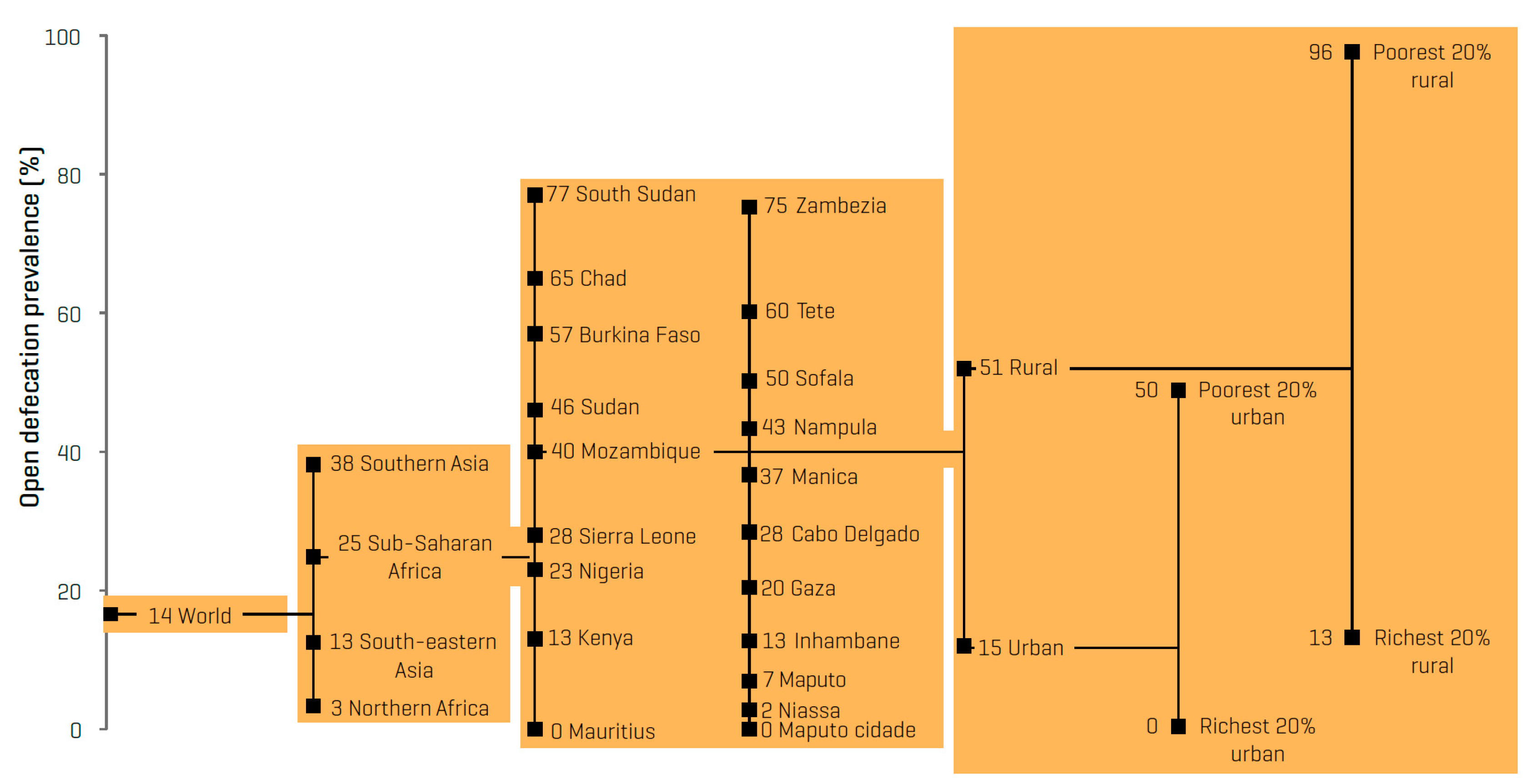
3.1.4. Coverage of Sanitation
3.1.5. Coverage of Hygiene
3.1.6. Distribution of Services
3.1.7. Institutional WASH
3.2. Impacts of Inadequate WASH
3.2.1. Health Consequences
Diarrheal Disease
Helminth Infections
Undernutrition and Environmental Enteric Dysfunction
3.2.2. Impacts on Well-Being
3.2.3. Environmental Consequences
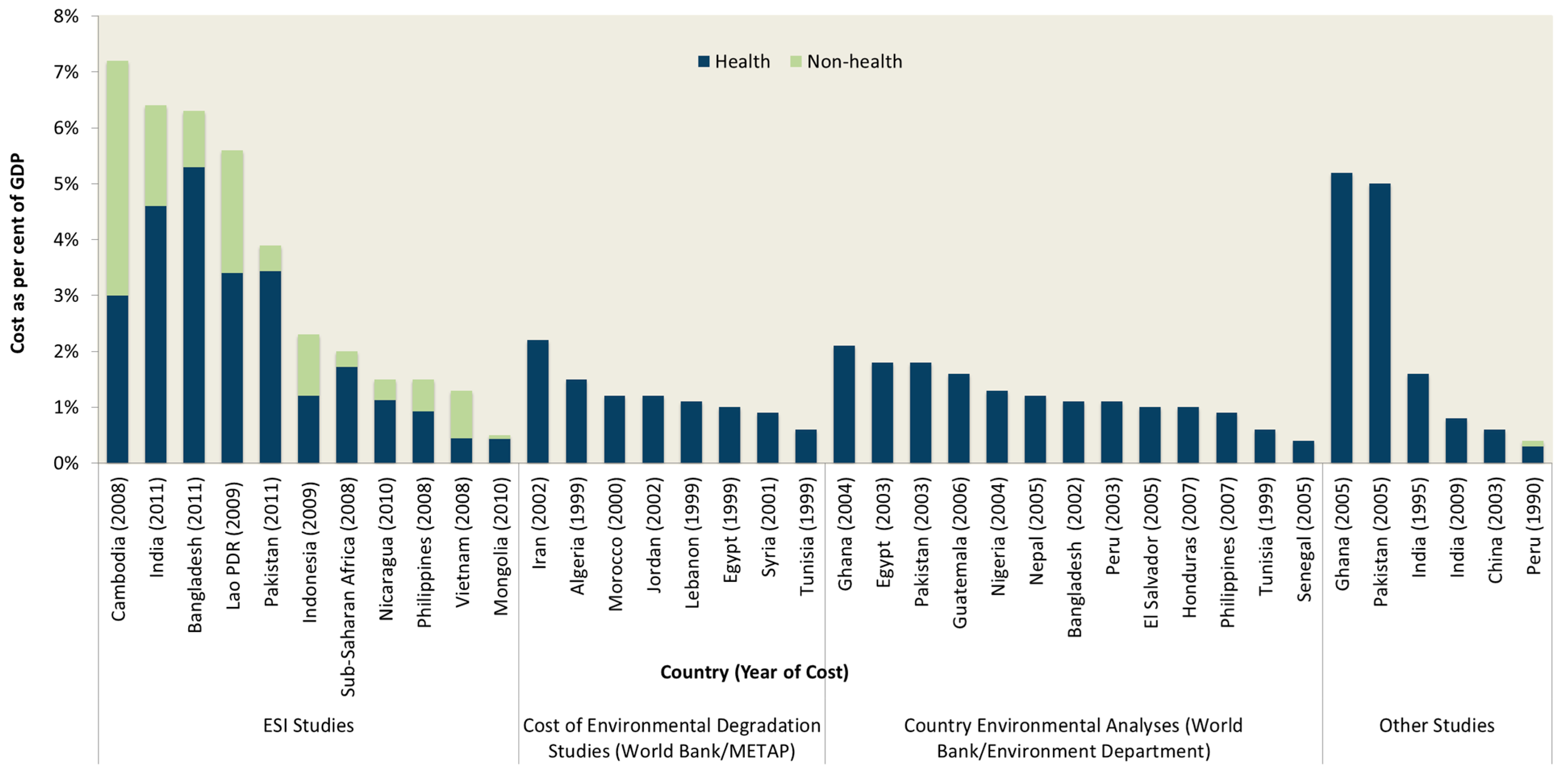
3.2.4. Financial and Economic Consequences
3.3. Effectiveness of Intervention Options
- Technology options and WASH practices cover the type of hardware, equipment and associated behaviors of WASH services. Not all water or sanitation technologies perform the same function, so they can be classified by the service level they provide.
- Service delivery models cover the components of WASH service implementation. These include the approach to strengthening the supply chain, the approach to generating demand for WASH, the choice of implementing agency or WASH provider, and the extent of integration of WASH programs with other interventions.
- Strengthening the enabling environment for WASH service delivery includes measures to strengthen capacity, legal framework, policy and planning, resource allocation, monitoring and evaluation, and other interventions to provide a stronger foundation for implementing the technology and service delivery models.
3.3.1. Effectiveness of Technologies and Practices
3.3.2. Effectiveness of Service Delivery Models
3.3.3. Effectiveness of the Enabling Environment
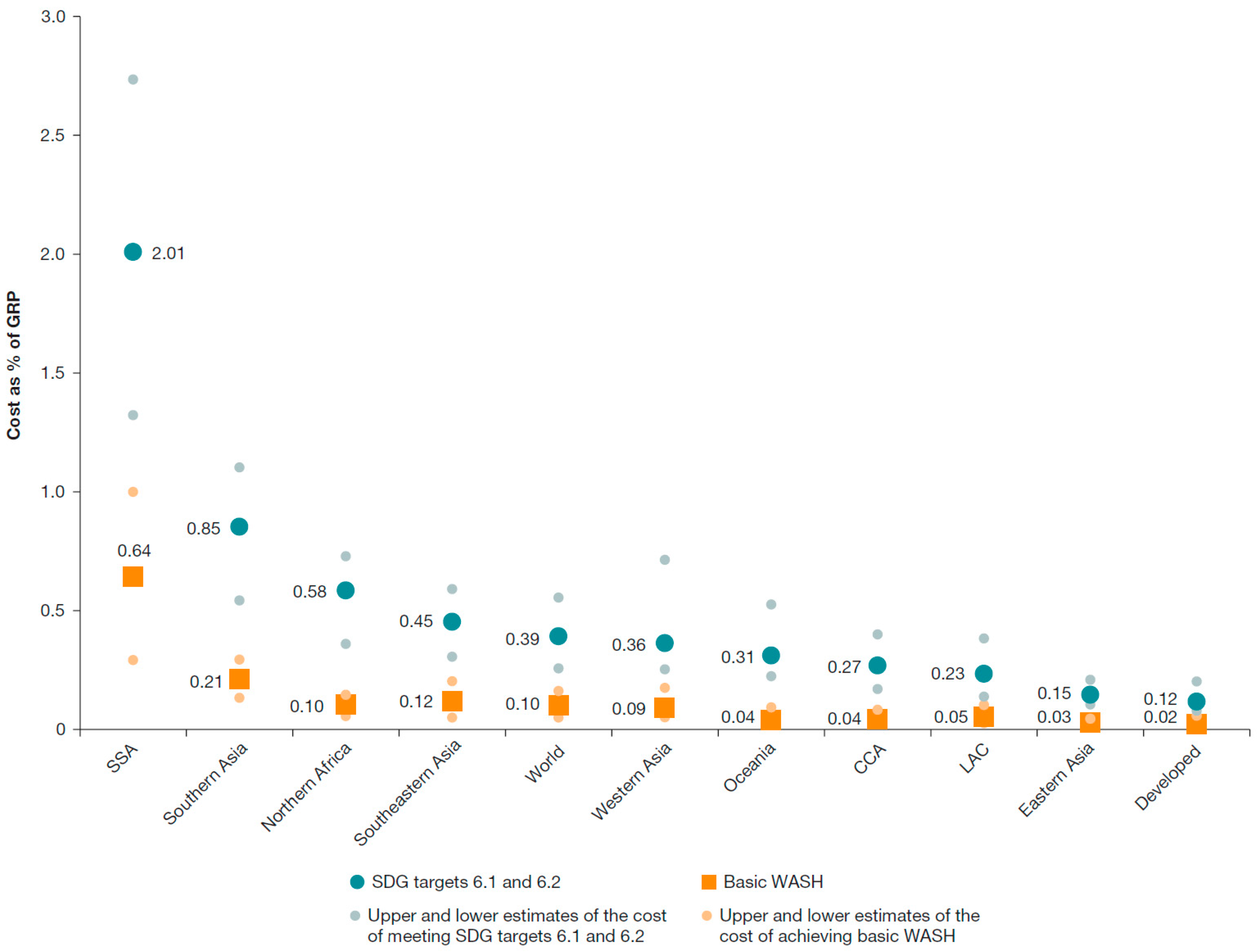
3.4. Intervention Costs, Benefits, Efficiency, and Sustainability
3.4.1. Costs
3.4.2. Benefits
3.4.3. Intervention Efficiency: Cost-Benefit Analysis
- Generate estimates of cost and benefit in specific sites or field studies, for the purposes of either evaluating intervention performance or selecting a site for a future project [63].
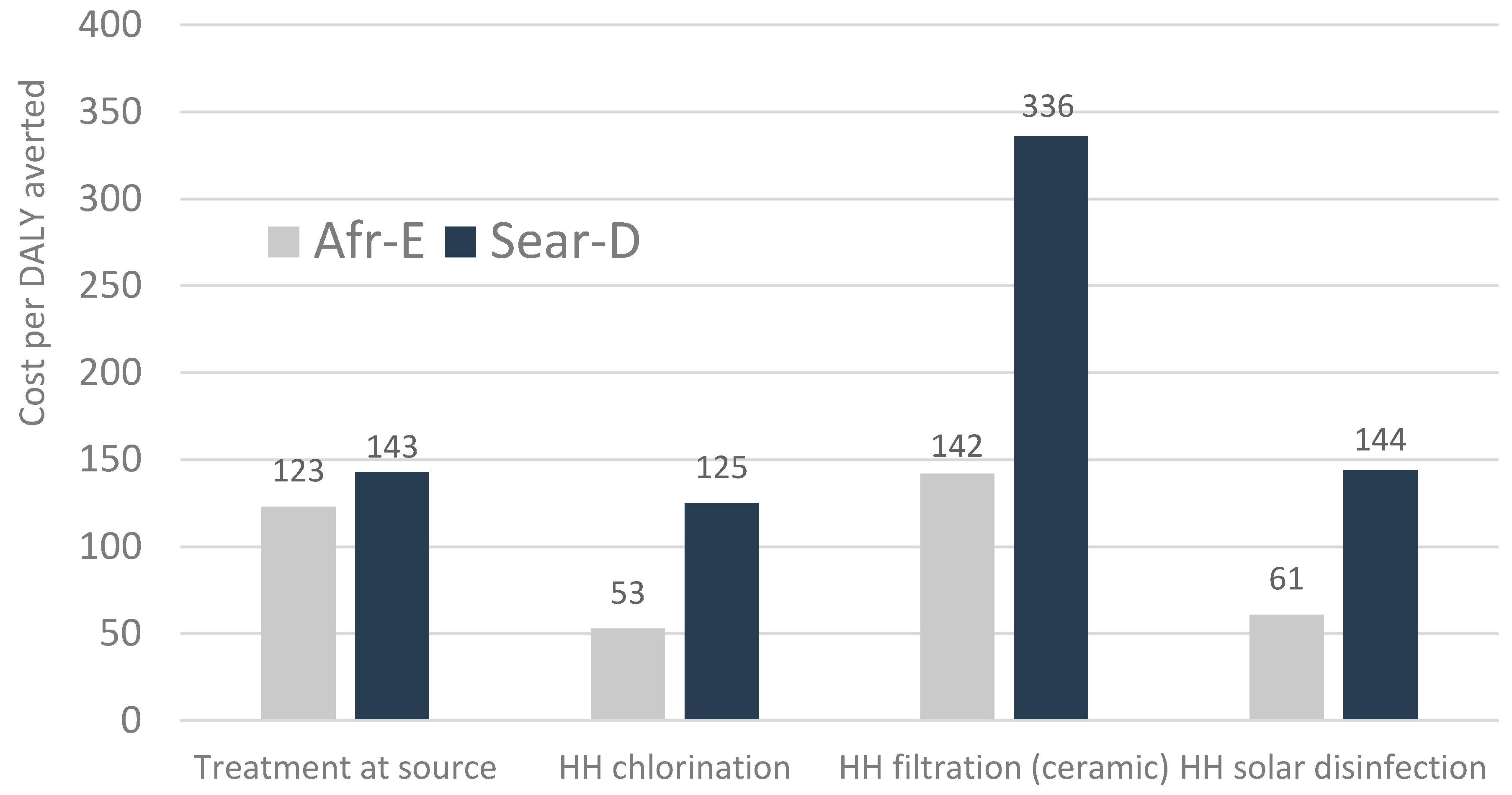
3.4.4. Intervention Efficiency: Cost-Effectiveness Analysis
3.4.5. Sustainability
4. Discussion
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| BAT | Bottleneck analysis tool |
| CATS | Community approach to total sanitation |
| CCT | Conditional-cash transfer |
| CDD | Community driven development |
| CEA | Cost-effectiveness analysis |
| CI | Confidence interval |
| CLTS | Community-led total sanitation |
| DALY | Disability-adjusted life-year |
| DHS | Demographic and Health Survey |
| GDP | Gross domestic product |
| HLY | Healthy life-year |
| HWTS | Household water treatment and storage |
| HWWS | Handwashing with soap |
| JMP | WHO/UNICEF Joint monitoring programme |
| MDG | Millennium Development Goal |
| MHM | Menstrual hygiene management |
| OBA | Output-based-aid |
| OECD | Organisation for Economic Co-operation and Development |
| RBA | Results-based approach |
| SDG | Sustainable development goal |
| SPA | Service provision assessment |
| STH | Soil-transmitted helminth |
| UN | United Nations |
| UNHCR | Office of the United Nations High Commissioner for Refugees |
| UNICEF | United Nations International Children’s Emergency Fund |
| WASH | Water, sanitation, and hygiene |
| WHO | World Health Organization |
| WTP | Willingness-to-pay |
References
- Human Rights Council. Resolution Adopted by the Human Rights Council. 18/1. The Human Right to Safe Drinking Water and Sanitation. Available online: http://www.worldwatercouncil.org/fileadmin/wwc/Right_to_Water/Human_Rights_Council_Resolution_cotobre_2011.pdf (accessed on 29 February 2016).
- WHO; UNICEF. Post 2015 Wash Targets and Indicators; WHO/UNICEF Joint Monitoring Programme for Water Supply and Sanitation; WHO: Geneva, Switzerland; UNICEF: New York, NY, USA, 2013. [Google Scholar]
- World Health Organization; UNICEF. Rapid Assessment of Drinking-Water Quality (Radwq). A Handbook for Implementation; World Health Organization: Geneva, Switzerland; UNICEF: New York, NY, USA, 2012. [Google Scholar]
- World Health Organization; UNICEF. Meeting the MDG Drinking Water and Sanitation Target. The Urban and Rural Challenge of the Decade; WHO/UNICEF Joint Monitoring Programme for Water Supply and Sanitation; WHO: Geneva, Switzerland; UNICEF: New York, NY, USA, 2006. [Google Scholar]
- Roaf, V.; Khalfan, A.; Langford, M. Monitoring Implementation of the Right to Water: A Framework for Developing Indicators; Heinrich Böll Foundation: Berlin, Germany, 2005. [Google Scholar]
- Moriarty, P.; Batchelor, C.; Fonseca, C.; Klutse, A.; Naafs, A.; Nyarko, A.; Pezon, K.; Potter, A.; Reddy, A.; Snehalata, R. Ladders for Assessing and Costing Water Service Delivery; WASHCost Working Paper 2; IRC International Water and Sanitation Centre: The Hague, The Netherlands, 2010. [Google Scholar]
- Potter, A.; Klutse, A.; Snehalatha, M.; Batchelor, C.; Uandela, A.; Naafs, A.; Fonseca, C.; Moriarty, P. Assessing Sanitation Service Levels; WASHCost Working Paper 3; IRC International Water and Sanitation Centre: The Hague, The Netherlands, 2010. [Google Scholar]
- Onda, K.; LoBuglio, J.; Bartram, J. Global access to safe water: Accounting for water quality and the resulting impact on MDG progress. Int. J. Environ. Res. Public Health 2012, 9, 880–894. [Google Scholar] [CrossRef] [PubMed]
- Stanton, B.; Clemens, J. Twenty-four hour recall, knowledge-attitude-practice questionnaires, and direct observations of sanitary practices: A comparative study. Bull. World Health Organ. 1987, 65, 217–222. [Google Scholar] [PubMed]
- Human Rights Council. The Human Right to Safe Drinking Water and Sanitation; Eighteenth Session, Agenda Item 3. Available online: http://www2.ohchr.org/english/bodies/hrcouncil/docs/18session/A-HRC-18-33_en.pdf (accessed on 20 May 2016).
- WHO; UNICEF. Progress on Drinking Water and Sanitation: 2015 Update and MDG Assessment; WHO/UNICEF Joint Monitoring Programme for Water Supply and Sanitation; WHO: Geneva, Switzerland; UNICEF: New York, NY, USA, 2015. [Google Scholar]
- WHO; UNICEF. Progress on Drinking Water and Sanitation. 2012 Update; World Health Organization: Geneva, Switzerland; UNICEF: New York, NY, USA, 2012. [Google Scholar]
- WHO; UNICEF. Progress on Drinking Water and Sanitation. 2010 Update; WHO/UNICEF Joint Monitoring Programme for Water Supply and Sanitation; WHO: Geneva, Switzerland; UNICEF: New York, NY, USA, 2010. [Google Scholar]
- Blackett, I.; Hawkins, P. The Missing Link in Sanitation Service Delivery. A Review of Fecal Sludge Management in 12 Cities; Water and Sanitation Program Research Brief; World Bank: Washington, DC, USA, 2014. [Google Scholar]
- Freeman, M.; Stocks, M.; Cumming, O.; Jeandron, A.; Higgins, J.; Wolf, J.; Pruss-Ustun, A.; Bonjour, S.; Hunter, P.; Fewtrell, L.; et al. Hygiene and health: Systematic review of handwashing practices worldwide and update of health effects. Trop. Med. Int. Health 2014, 19, 906–916. [Google Scholar] [CrossRef] [PubMed]
- Biran, A.; Rabie, T.; Schmidt, W.; Juvekar, S.; Hirve, S.; Curtis, V. Comparing the performance of indicators of hand-washing practices in rural Indian households. Trop. Med. Int. Health 2008, 13, 278–285. [Google Scholar] [CrossRef] [PubMed]
- WHO; UNICEF. Progress on Drinking Water and Sanitation. 2013 Update; WHO/UNICEF Joint Monitoring Programme for Water Supply and Sanitation; WHO: Geneva, Switzerland; UNICEF: New York, NY, USA, 2013. [Google Scholar]
- WHO; UNICEF. Progress on Drinking Water and Sanitation. 2014 Update; WHO/UNICEF Joint Monitoring Programme for Water Supply and Sanitation; WHO: Geneva, Switzerland; UNICEF: New York, NY, USA, 2014. [Google Scholar]
- Loevensohn, M.; Mehta, L.; Cuming, K.; Nicol, A.; Cumming, O.; Ensink, J. The cost of a knowledge silo: A systematic re-review of water, sanitation and hygiene interventions. Health Policy Plan. 2015, 30, 660–674. [Google Scholar] [CrossRef] [PubMed]
- Strickland, G. Hunter’s Tropical Medicine and Emerging Infectious Diseases, 8th ed.; W.B. Saunders Company: Philadelphia, PA, USA, 2000. [Google Scholar]
- Burton, M.J.; Mabey, D. The global burden of trachoma: A review. PLoS Negl. Trop. Dis. 2009, 3, e460. [Google Scholar] [CrossRef] [PubMed]
- Rabie, T.; Curtis, V. Handwashing and risk of respiratory infections: A quantitative systematic review. Trop. Med. Int. Health 2006, 11, 258–267. [Google Scholar] [CrossRef] [PubMed]
- Semmelweis, I. The Etiology, Concept and Prophylaxis of Childbed Fever; The University of Wisconsin Press: Madison, WI, USA, 1983. [Google Scholar]
- Blencowe, H.; Cousens, S.; Mullany, L.; Lee, A.; Kerber, K.; Wall, S. Clean birth and postnatal care practices to reduce neonatal deaths from sepsis and tetanus: A systematic review and delphi estimation of mortality effect. BMC Public Health 2011, 11, S11. [Google Scholar] [CrossRef] [PubMed]
- Rhee, V.; Mullany, L.; Khatry, S.; Katz, J.; LeClerq, S.; Darmstadt, G.; Tielsch, J. Maternal and birth attendant hand washing and neonatal mortality in southern Nepal. Arch. Pediatr. Adolesc. Med. 2008, 162, 603–608. [Google Scholar] [CrossRef] [PubMed]
- Benova, L.; Cumming, O.; Campbell, O. Systematic review and meta-analysis: Association between water and sanitation environment and maternal mortality. Trop. Med. Int. Health 2014, 19, 368–387. [Google Scholar] [CrossRef] [PubMed]
- Pickering, A.; Djebbari, H.; Lopez, C.; Coulibaly, M.; Alzua, M. Effect of a community-led sanitation intervention on child diarrhoea and child growth in rural Mali: A cluster-randomised controlled trial. Lancet Glob. Health 2015, 3, E701–E711. [Google Scholar] [CrossRef]
- Curtis, V.; Cairncross, S. Effect of washing hands with soap on diarrhoea risk in the community: A systematic review. Lancet Infect. Dis. 2003, 3, 275–281. [Google Scholar] [CrossRef]
- Ilahi, N.; Grimard, F. Public infrastructure and private costs: Water supply and time allocation of women in rural Pakistan. Econ. Dev. Cult. Chang. 2000, 49, 45–75. [Google Scholar] [CrossRef]
- Popkin, B.; D’Anci, K.; Rosenberg, I. Water, hydration and health. Nutr. Rev. 2010, 68, 439–458. [Google Scholar] [CrossRef] [PubMed]
- Atia, A.; Buchman, A. Oral rehydration solutions in non-cholera diarrhea: A review. Am. J. Gastroenterol. 2009, 104, 2596–2604. [Google Scholar] [CrossRef] [PubMed]
- Murcott, S. Arsenic Contamination in the World: An International Sourcebook; IWA Publishing: London, UK, 2012. [Google Scholar]
- Naujokas, M.; Anderson, B.; Ahsan, H.; Aposhian, H.; Graziano, J.; Thompson, C.; Suk, W. The broad scope of health effects from chronic arsenic exposure: Update on a worldwide public health problem. Environ. Health Perspect. 2013, 121, 295–302. [Google Scholar] [CrossRef] [PubMed]
- Ahern, M.; Kovats, R.; Wilkinson, P.; Few, R.; Matthies, F. Global health impacts of floods: Epidemiologic evidence. Epidemiol. Rev. 2005, 27, 36–46. [Google Scholar] [CrossRef] [PubMed]
- Jafari, N.; Shahsanai, A.; Memarzadeh, M.; Loghmani, A. Prevention of communicable diseases after disaster: A review. J. Res. Med. Sci. 2011, 16, 956–962. [Google Scholar] [PubMed]
- Prüss-Üstun, A.; Bartram, J.; Clasen, T.; Colford, J.; Cumming, O.; Curtis, V.; Bonjour, S.; Dangour, A.; De France, J.; Fewtrell, L.; et al. Burden of diarrheal disease from inadequate water, sanitation and hygiene in low- and middle-income countries: A retrospective analysis of data from 145 countries. Trop. Med. Int. Health 2014, 19, 894–905. [Google Scholar] [CrossRef] [PubMed]
- Prüss-Ustun, A.; Corvalan, C. How much disease burden can be prevented by environmental interventions? Epidemiol. Soc. 2006, 18, 167–178. [Google Scholar]
- Lanata, C.; Fischer-Walker, C.; Olascoaga, A.; Torres, C.; Aryee, M.; Black, R. Global causes of diarrheal disease mortality in children <5 years of age: A systematic review. PLoS ONE 2013, 8, e72788. [Google Scholar]
- Hales, S.; Kovats, S.; Lloyd, S.; Campbell-Lendrum, D. Quantitative Risk Assessment of the Effects of Climate Change on Selected Causes of Death, 2030s and 2050s; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Ali, M.; Nelson, A.; Lopez, A.; Sack, D. Updated global burden of cholera in endemic countries. PLoS Negl. Trop. Dis. 2015, 9, e0003832. [Google Scholar] [CrossRef] [PubMed]
- Taylor, D.; Kahawita, T.; Cairncross, S.; Ensink, J. The impact of water, sanitation and hygiene interventions to control cholera: A systematic review. PLoS ONE 2015, 10, e0135676. [Google Scholar] [CrossRef] [PubMed]
- Jasper, C.; Le, T.; Bartram, J. Water and sanitation in schools: A systematic review of the health and educational outcomes. Int. J. Environ. Res. Public Health 2012, 9, 2272–2287. [Google Scholar] [CrossRef] [PubMed]
- Pullan, R.; Smith, J.; Jasrasaria, R.; Brooker, S. Global numbers of infection and disease burden of soil transmitted helminth infections in 2010. Parasites Vectors 2014, 7. [Google Scholar] [CrossRef] [PubMed]
- Brooker, S.; Clements, A.; Bundy, D. Global epidemiology, ecology and control of soil-transmitted helminth infections. Adv. Parasitol. 2006, 62, 221–261. [Google Scholar] [PubMed]
- Lozano, R.; Naghavi, M.; Foreman, K.; Lim, S.; Shibuya, K. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the global burden of disease study 2010. Lancet 2010, 380, 2095–2128. [Google Scholar] [CrossRef]
- WHO. Working to Overcome the Global Impact of Neglected Tropical Diseases: First WHO Report on Neglected Tropical Diseases; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Victora, C.; Adair, L.; Fall, C.; Hallal, P.; Martorell, R.; Richter, L.; Sachdev, H.; Maternal and Child Undernutrition Study Group. Maternal and child undernutrition: Consequences for adult health and human capital. Lancet 2008, 371, 340–357. [Google Scholar] [CrossRef]
- Hotez, P.; Bundy, D.; Beegle, K.; Brooker, S.; Drake, L.; de Silva, N.; Montresor, A.; Engels, D.; Jukes, M.; Chitsulo, L.; et al. Helminth infections: Soil-transmitted helminth infections and schistosomiasis. In Disease Control Priorities in Developing Countries, 2nd ed.; Jamison, D., Breman, J., Measham, A., Alleyne, G., Claeson, M., Evans, D., Jha, P., Mills, A., Musgrove, P., Eds.; Oxford University Press: Oxford, UK; World Bank: New York, NY, USA, 2006. [Google Scholar]
- Black, R.; Victora, C.; Walker, S.; Bhutta, Z.; Christian, P.; de Onis, M.; Ezzati, M.; Grantham-McGregor, S.; Katz, J.; Martorell, R.; et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013, 382, 427–451. [Google Scholar] [CrossRef]
- Black, R.; Allen, L.; Bhutta, Z.; Caulfield, L.; de Onis, M.; Ezzati, M.; Mathers, C.; Rivera, J.; Maternal and Child Undernutrition Study Group. Maternal and child undernutrition: Global and regional exposures and health consequences. Lancet 2008, 371, 243–260. [Google Scholar] [CrossRef]
- United Nations Children’s Fund. Strategy for Improved Nutrition of Children and Women in Developing Countries: A Unicef policy Review; UNICEF: New York, NY, USA, 1990. [Google Scholar]
- Fishman, S.; Caulfield, L.; de Onis, M.; Blössner, M.; Hyder, A.; Mullany, L.; Black, R. Childhood and maternal underweight. In Comparative Quantification of Health Risks: Global and Regional Burden of Disease Due to Selected Major Risk Factors; Ezzati, M., Rodgers, A., Lopez, A., Murray, C., Eds.; World Health Organization: Geneva, Switzerland, 2004; Volume 2. [Google Scholar]
- Prüss-Üstun, A.; Corvalan, C. Preventing Disease through Healthy Environments: Towards an Estimate of the Environmental Burden of Disease; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- Lin, A.; Arnold, B.; Afreen, S.; Goto, R.; Mohammad Nurul Huda, T.; Haque, R.; Raqib, R.; Unicomb, L.; Ahmed, T.; Colford, J.; et al. Household environmental conditions are associated with enteropathy and impaired growth in rural Bangladesh. Am. J. Trop. Med. Hyg. 2013, 89, 130–137. [Google Scholar] [CrossRef] [PubMed]
- Checkley, W.; Buckley, G.; Gilman, R.; Assis, A.; Guerrant, R.; Morris, S.; Molbak, K.; Valentiner-Branth, P.; Lanata, C.; Black, R. Multi-country analysis of the effects of diarrhoea on childhood stunting. Int. J. Epidemiol. 2008, 37, 816–830. [Google Scholar] [CrossRef] [PubMed]
- Guerrant, R.; Oriá, R.; Moore, S.; Oriá, M.; Lima, A. Malnutrition as an enteric infectious disease with long-term effects on child development. Nutr. Rev. 2008, 66, 487–505. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.; Cairncross, S.; Ensink, J. Water, sanitation, hygiene and enteric infections in children. Arch. Dis. Child. 2013. [Google Scholar] [CrossRef] [PubMed]
- Humphrey, J. Child undernutrition, tropical enteropathy, toilets, and handwashing. Lancet 2009, 3754, 1032–1035. [Google Scholar] [CrossRef]
- Kotloff, K.; Nataro, J.; Blackwelder, W.; Nasrin, D.; Farag, T.; Panchalingam, S.; Wu, Y.; Sow, S.; Sur, D.; Breiman, R. Burden and aetiology of diarrhoeal disease in infants and young children in developing countries (the global enteric multicenter study, gems): A prospective, case-control study. Lancet 2013, 382, 209–222. [Google Scholar] [CrossRef]
- Salazar-Lindo, E.; Allen, S.; Brewster, D.; Elliott, E.; Fasano, A.; Phillips, A.; Sanderson, I.; Tarr, P. Intestinal infections and environmental enteropathy: Working group report of the second world congress of pediatric gastroenterology, hepatology, and nutrition. J. Pediatr. Gastroenterol. Nutr. 2004, 39, S662–S669. [Google Scholar] [CrossRef] [PubMed]
- Guerrant, R.; DeBoer, M.; Moore, S.; Scharf, R.; Lima, A. The impoverished gut—A triple burden of diarrhoea, stunting and chronic disease. Nat. Rev. Gastroenterol. Hepatol. 2013, 10, 220–229. [Google Scholar] [CrossRef] [PubMed]
- Özaltin, E.; Hill, K.; Subramanian, S. Association of maternal stature with offspring mortality, underweight, and stunting in low- to middle-income countries. JAMA 2010, 303, 1507–1516. [Google Scholar] [CrossRef] [PubMed]
- Hutton, G.; Rodriguez, U.-P.; Winara, A.; Nguyen, V.; Kov, P.; Chuan, L.; Blackett, I.; Weitz, A. Economic efficiency of sanitation interventions in Southeast Asia. J. Water Sanit. Hyg. Dev. 2014, 4, 23–36. [Google Scholar] [CrossRef]
- Cairncross, S. The Case for Marketing Sanitation. Field Note; Water and Sanitation Program, World Bank: Washington, DC, USA, 2004. [Google Scholar]
- Jenkins, M.; Curtis, V. Achieving the “good life”: Why some people want latrines in rural Benin. Soc. Sci. Med. 2005, 61, 2446–2459. [Google Scholar] [CrossRef] [PubMed]
- Fisher, J. For Her It’s the Big Issue. Putting Women at the Centre of Water Supply, Sanitation and Hygiene; Evidence Report; Water Supply and Sanitation Collaborative Council: Geneva, Switzerland, 2006. [Google Scholar]
- Howard, G.; Bartram, J. Domestic Water Quantity, Service Level and Health; WHO/SDE/WSH/03.02; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- Olajuyigbe, A. Some factors impacting on quantity of water used by households in a rapidly urbanizing state capital in South Western Nigeria. J. Sustain. Dev. Afr. 2010, 12, 321–337. [Google Scholar]
- Lokshin, M.; Yemtsov, R. Has rural infrastructure rehabilitation in georgia helped the poor? World Bank Econ. Rev. 2005, 19, 311–333. [Google Scholar] [CrossRef]
- Koolwal, G.; Van de Walle, D. Access to water, women’s work, and child outcomes. Econ. Dev. Cult. Chang. 2013, 61, 369–405. [Google Scholar] [CrossRef]
- Jenkins, M.; Scott, B. Behavioral indicators of household decision-making and demand for sanitation and potential gains from social marketing in Ghana. Soc. Sci. Med. 2007, 64, 2427–2442. [Google Scholar] [CrossRef] [PubMed]
- Adukia, A. Sanitation and Education. Ph.D. Thesis, Harvard University, Harvard, UK, 2012. [Google Scholar]
- Sebastian, A.; Hoffmann, V.; Adelman, S. Menstrual management in low-income countries: Needs and trends. Waterlines 2013, 32, 135–153. [Google Scholar] [CrossRef]
- Sumpter, C.; Torondel, B. A systematic review of the health and social effects of menstrual hygiene management. PLoS ONE 2013, 8, e62004. [Google Scholar] [CrossRef] [PubMed]
- Oster, E.; Thornton, R. Menstruation, sanitary products, and school attendance: Evidence from a randomized evaluation. Am. Econ. J. Appl. Econ. 2011, 3, 91–100. [Google Scholar] [CrossRef]
- Schlosser, C.; Strzepek, K.; Gao, X.; Gueneau, A.; Fant, C.; Paltsev, S.; Rasheed, B.; Smith-Greico, T.; Blanc, E.; Jacoby, H.; et al. The Future of Global Water Stress: An Integrated Assessment; MIT Joint Program on the Sciene and Policy of Global Change: Cambridge, MA, USA, 2014. [Google Scholar]
- Sadoff, C.; Hall, J.; Grey, D.; Aerts, J.; Ait-Kadi, M.; Brown, C.; Cox, A.; Dadson, S.; Garrick, D.; Kelman, J.; et al. Securing Water, Sustaining Growth: Report of the GWP/OECD Task Force on Water Security and Sustainable Growth; University of Oxford: Oxford, UK, 2015. [Google Scholar]
- Scott, C.; Shah, T. Groundwater overdraft reduction through agricultural energy policy: Insights from India and Mexico. Int. J. Water Resour. Dev. 2004, 20, 149–164. [Google Scholar] [CrossRef]
- Corcoran, E.; Nellemann, C.; Baker, E.; Bos, R.; Osborn, D.; Savelli, H. Sick Water? The Central Role of Wastewater Management in Sustainable Development. A Rapid Response Assessment; United Nations Environment Programme, UN HABITAT, GRIDArendal: Arendal, Norway, 2011. [Google Scholar]
- Rabalais, N.N.; Turner, R.E. Coastal Hypoxia: Consequences for living Resources and Ecosystems; American Geophysical Union: Washington, DC, USA, 2013. [Google Scholar]
- Turner, R.; Rabalais, N. Changes in Mississippi River water quality this century and implications for coastal food webs. Bioscience 1991, 41, 140–147. [Google Scholar] [CrossRef]
- Sofıa Dutto, M.; Lopez Abbate, M.; Biancalana, F.; Berasategui, A.; Hoffmeyer, M. The impact of sewage on environmental quality and the mesozooplankton community in a highly eutrophic estuary in Argentina. J. Mar. Sci. 2012, 69, 399–409. [Google Scholar]
- World Bank. The Philippines: Country Environmental Analysis; World Bank: Washington, DC, USA, 2009. [Google Scholar]
- Hutton, G. Global Costs and Benefits of drinking-Water Supply and Sanitation Interventions to Reach the MDG Target and Universal Coverage; Report No. WHO/HSE/WSH/12.01; World Health Organization: Geneva, Switzerland, 2012. [Google Scholar]
- Waddington, H.; Snilstveit, B.; White, H.; Fewtrell, L. Water, Sanitation and Hygiene Interventions to Combat Childhood Diarrhea in Developing Countries; The International Initiative for Impact Evaluation (3iE): New Delhi, India, 2009. [Google Scholar]
- Wolf, J.; Prüss-Üstun, A.; Cumming, O.; Bartram, J.; Bonjour, S.; Cairncross, S.; Clasen, T.; Colford, J.M.; Curtis, V.; France, J.; et al. Assessing the impact of drinking-water and sanitation on diarrhoeal disease in low- and middle-income countries: A systematic review and regression analysis. Trop. Med. Int. Health 2014, 8, 928–942. [Google Scholar] [CrossRef] [PubMed]
- Van den Berg, C.; Danilenko, A. The IBNET Water Supply and Sanitation Performance Blue Book: The International Benchmarking Network of Water and Sanitation Utilities (IBNET) Databook; Water and Sanitation Program, World Bank: Washingon, DC, USA, 2010. [Google Scholar]
- Hunter, P.R.; Zmirou-Navier, D.; Hartemann, P. Estimating the impact on health of poor reliability of drinking water interventions in developing countries. Sci. Total Environ. 2009, 407, 2621–2624. [Google Scholar] [CrossRef] [PubMed]
- Clasen, T.; Haller, L.; Walker, D.; Bartram, J.; Cairncross, S. Cost-effectiveness of water quality interventions for preventing diarrhoeal disease in developing countries. J. Water Health 2007, 5, 599–608. [Google Scholar] [CrossRef] [PubMed]
- Baker, K.K.; O’Reilly, C.E.; Levine, M.M.; Kotloff, K.L.; Nataro, J.P.; Ayers, T.L.; Farag, T.H.; Nasrin, D.; Blackwelder, W.C.; Wu, Y.; et al. Sanitation and hygiene-specific risk factors for moderate-to-severe diarrhea in young children in the global enteric multicenter study, 2007–2011: Case-control study. PLoS Med. 2016, 13, e1002010. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Biran, A.; Jenkins, M.; Dabrase, P.; Bhagwat, I. Patterns and determinants of communal latrine usage in urban poverty pockets in Bhopal, India. Trop. Med. Int. Health 2011, 16, 854–862. [Google Scholar] [CrossRef] [PubMed]
- Norman, G.; Pedley, S.; Takkouche, B. Effects of sewerage on diarrhoea and enteric infections: A systematic review and meta-analysis. Lancet Infect. Dis. 2010, 10, 536–544. [Google Scholar] [CrossRef]
- Strunz, E.C.; Addiss, D.G.; Stocks, M.E.; Ogden, S.; Utzinger, J.; Freeman, M.C. Water, sanitation, hygiene, and soil-transmitted helminth infection: A systematic review and meta-analysis. PLoS Med. 2014, 14, e1001620. [Google Scholar] [CrossRef] [PubMed]
- Stocks, M.E.; Ogden, S.; Haddad, D.; Addiss, D.G.; McGuire, C.; Freeman, M.C. Effect of water, sanitation, and hygiene on the prevention of trachoma: A systematic review and meta-analysis. PLoS Med. 2014, 11, e1001605. [Google Scholar] [CrossRef] [PubMed]
- Dangour, A.D.; Watson, L.; Cumming, O.; Boisson, S.; Che, Y.; Velleman, Y.; Cavill, S.; Allen, E.; Uauy, R. Interventions to improve water quality and supply, sanitation and hygiene practices, and their effects on the nutritional status of children. Cochrane Database Syst. Rev. 2013, 8. [Google Scholar] [CrossRef]
- Clasen, T.; Boisson, S.; Routray, P.; Torondel, B.; Bell, M.; Cumming, O.; Ensink, J.; Freeman, M.; Jenkins, M.; Odagiri, M.; et al. Effectiveness of a rural sanitation programme on diarrhoea, soil-transmitted helminth infection, and child malnutrition in Odisha, India: A cluster-randomised trial. Lancet Glob. Health 2014, 2, e645–e653. [Google Scholar] [CrossRef]
- Patil, S.R.; Arnold, B.F.; Salvatore, A.L.; Briceno, B.; Ganguly, S.; Colford, J.M., Jr.; Gertler, P.J. The effect of India’s total sanitation campaign on defecation behaviors and child health in rural Madhya Pradesh: A cluster randomized controlled trial. PLoS Med. 2014, 11. [Google Scholar] [CrossRef] [PubMed]
- Hammer, J.; Spears, D. Village Sanitation and Children’s Human Capital Evidence from a Randomized Experiment by the Maharashtra Government; Policy Research Working Paper 5580; World Bank: Washington, DC, USA, 2013. [Google Scholar]
- Cameron, L.; Shah, M.; Olivia, S. Impact Evaluation of a Large-Scale Rural Sanitation Project in Indonesia; Policy Research Working Paper 6360; World Bank: Washington, DC, USA, 2013. [Google Scholar]
- Briceno, B.; Coville, A.; Martinez, S. Promoting Handwashing and Sanitation: A Crossover Randomized Experiment in Rural Tanzania; Working Paper; Water and Sanitation Program, World Bank: Washington, DC, USA, 2014. [Google Scholar]
- Spears, D.; Lamba, S. Effects of Early-Life Exposure to Sanitation on Childhood Cognitive Skills: Evidence from India’s Total Sanitation Campaign; World Bank: Washington, DC, USA, 2013. [Google Scholar]
- The Cochrane Library. Available online: http://www.thecochranelibrary.com (accessed on 29 February 2016).
- Smets, H. Quantifying the affordability standard. In The Human Right to Water: Theory, Practice and Prospects; Cambridge University Press: Cambridge, UK, 2012. [Google Scholar]
- Schmidt, W.-P.; Cairncross, S. Household water treatment in poor populations: Is there enough evidence for scaling up now? Environ. Sci. Technol. 2009, 43, 986–992. [Google Scholar] [CrossRef] [PubMed]
- Curtis, V.; Kanki, B.; Cousens, S.; Diallo, I.; Kpozehouen, A.; Sangare; Nikiema, M. Evidence of behaviour change following a hygiene promotion programme in Burkina Faso. Bull. World Health Organ. 2001, 79, 518–527. [Google Scholar] [PubMed]
- Galiani, S.; Gertler, P.; Ajzenman, N.; Orsola-Vidal, A. Promoting handwashing behavior: The effects of large-scale community and school-level interventions. Health Econ. 2015. [Google Scholar] [CrossRef] [PubMed]
- Nicholson, J.A.; Naeeni, M.; Hoptroff, M.; Matheson, J.R.; Roberts, A.J.; Taylor, D.; Sidibe, M.; Weir, A.J.; Damle, S.G.; Wright, R.L. An investigation of the effects of a hand washing intervention on health outcomes and school absence using a randomised trial in Indian urban communities. Trop. Med. Int. Health 2013, 19, 284–292. [Google Scholar] [CrossRef] [PubMed]
- Sy, J.; Warner, R.; Jamieson, J. Tapping the Markets: Opportunities for Domestic Investments in Water and Sanitation for the Poor; World Bank: Washington, DC, USA, 2014. [Google Scholar]
- UNICEF. Community Approaches to Total Sanitation; UNICEF DPP Field Notes; UNICEF: New York, NY, USA, 2009. [Google Scholar]
- Sanitation Marketing Toolkit. Water and Sanitation Program, World Bank: Washington, DC, USA; Available online: https://wsp.org/toolkit/toolkit-home (accessed on 29 February 2016).
- Patil, S.; Arnold, B.; Salvatore, A.; Briceno, B.; Colford, J.; Gertler, P. A Randomized, Controlled Study of A Rural Sanitation Behavior Change Program in Madhya Pradesh, India; World Bank: Washington, DC, USA, 2013. [Google Scholar]
- Perez, E.; Cardosi, J.; Coombes, Y.; Devine, J.; Grossman, A.; Kullmann, C.; Kumar, C.A.; Mukherjee, N.; Prakash, M.; Robiarto, A.; et al. What Does It Take to Scale Up Rural Sanitation? Water and Sanitation Program, World Bank: Washoington, DC, USA, 2012. [Google Scholar]
- Guiteras, R.; Levinsohn, J.; Mobarak, A.M. Encouraging sanitation investment in the developing world: A cluster-randomized trial. Science 2015, 348, 903–906. [Google Scholar] [CrossRef] [PubMed]
- Winpenny, J. The Evidence Base for Payment by Results in Water, Sanitation and Hygiene; Department for International Development (DFID): London, UK, 2013. [Google Scholar]
- Mumssen, Y.; Johannes, L.; Kumar, G. Output-Based Aid: Lessons Learned and Best Practices; Water and Sanitation Program, World Bank: Washington, DC, USA, 2010. [Google Scholar]
- World Bank Global Program for Output Based Aid (GPOBA). Available online: http://www.oba-data.org (accessed on 31 March 2014).
- World Bank Program for Results Instrument. Available online: http://www.worldbank.org/en/programs/program-for-results-financing# (accessed on 29 February 2016).
- Devoto, F.; Duflo, E.; Dupas, P.; Pariente, W.; Pons, V. Happiness on Tap: Piped Water Adoption in Urban Morocco; Paper No. w16933; National Bureau of Economic Research: Cambridge, MA, USA, 2011. [Google Scholar]
- Shah, N.B. Microfinance Loans to Increase Sanitary Latrine Sales: Evidence from A Randomized Trial in Rural Cambodia; Policy Brief; International Development Enterprises: Phnom Penh, Cambodia, 2013. [Google Scholar]
- Rosensweig, F.; Perez, E.; Robinson, A. Policy and Sector Reform to Accelerate Access to Improved Rural Sanitation; Water and Sanitation Program Working Paper; World Bank: Washiongton, DC, USA, 2012. [Google Scholar]
- African Ministers Council on Water (AMCOW). Pathways to Progress: Transitioning to Country-Led Service Delivery Pathways to Meet Africa’s Water Supply and Sanitation Targets; Amcow Country Status Overviews, Regional Synthesis Report; Water and Sanitation Program, African Development Bank, World Bank: Washington, DC, USA, 2011. [Google Scholar]
- Water and Sanitation Program (WSP). Turning Finances into Services for the Future: A Regional Synthesis of the Service Delivery Assessments for Water Supply and Sanitation in East Asia and the Pacific; World Bank: Washington, DC, USA, 2015. [Google Scholar]
- Water and Sanitation Program (WSP). Linking Service Delivery Processes and Outcomes in Rural Sanitation: Findings from 56 Districts in India; Water and Sanitation Program, World Bank: Washington, DC, USA, 2013. [Google Scholar]
- United Nations Children’s Fund. Wash Bottleneck Analysis Tool (WASH-BAT); UNICEF: New York, NY, USA, 2014. [Google Scholar]
- World Health Organization. UN-Water Global Analysis and Assessment of Sanitation and Drinking-Water. The Challenge of Extending and Sustaining Services; WHO: Geneva, Switzerland, 2012. [Google Scholar]
- Hutton, G.; Varughese, M. The Costs of Meeting the 2030 sustainable Development Goal Targets on Drinking Water, Sanitation, And Hygiene; Water and Sanitation Program, World Bank: Washington, DC, USA, 2016. [Google Scholar]
- Organisation for Economic Cooperation and Development (OECD). Feasible Financing Strategies for Water Supply and Sanitation; Organisation for Economic Cooperation and Development: Paris, France, 2007. [Google Scholar]
- Organisation for Economic Cooperation and Development (OECD). Meeting the Challenge of Financing Water and Sanitation: Tools and Approaches; Organisation for Economic Cooperation and Development: Paris, France, 2011. [Google Scholar]
- Whittington, D.; Hanemann, W.M.; Sadoff, C.; Jeuland, M. The challenge of improving water and sanitation services in less developed countries. Found. Trends Microecon. 2009, 4, 469–607. [Google Scholar] [CrossRef]
- Burr, P.; Fonseca, C. Applying A Life-Cycle Costs Approach to Water: Costs and Service Levels in Rural and Small Town Areas in Andhra Pradesh (India), Burkina Faso, Ghana and Mozambique; Working Paper 8; IRC International Water and Sanitation Centre: The Hague, The Netherlands, 2013. [Google Scholar]
- Dodane, P.; Mbéguéré, M.; Sow, O.; Strande, L. Capital and operating costs of full-scale fecal sludge management and wastewater treatment systems in dakar, senegal. Environ. Sci. Technol. 2012, 46, 3705–3711. [Google Scholar] [CrossRef] [PubMed]
- Hutton, G. Global costs and benefits of reaching universal coverage of sanitation and drinking-water supply. J. Water Health 2013, 11, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Pattanayak, S.; Poulos, C.; Yang, J.; Patil, S. How valuable are environmental health interventions? Evaluation of water and sanitation programmes in India. Bull. World Health Organ. 2010, 88, 535–542. [Google Scholar] [CrossRef] [PubMed]
- Hutton, G.; Rodriguez, U.; Napitupulu, L.; Thang, P.; Kov, P. Economic Impacts of Sanitation in Southeast Asia; Water and Sanitation Program, World Bank: Washington, DC, USA, 2008. [Google Scholar]
- Van Houtven, G.; Pattanayak, S.; Yang, J. Meta-analysis of willingness to pay estimates for access to improved drinking water. In Research Triangle Institute Working Paper; RTI: NC, USA, 2011. [Google Scholar]
- Null, C.; Hombrado, J.G.; Meeks, R.; Edward, M.; Zwane, A.P. Willingness to Pay for Cleaner Water in Less Developed Countries: Systematic Review of Experimental Evidence; The International Initiative for Impact Evaluation (3iE): New Delhi, India, 2012. [Google Scholar]
- Guh, S.; Xingbao, C.; Poulos, C.; Qi, Z.; Jianwen, C.; von Seidlein, L.; Jichao, C.; Wang, X. Comparison of cost-of-illness with willingness-to-pay estimates to avoid shigellosis: Evidence from China. Health Policy Plan. 2008, 23, 125–136. [Google Scholar] [CrossRef] [PubMed]
- Orgill, J.; Shaheed, A.; Brown, J.; Jeuland, M. Water quality perceptions and willingness to pay for clean water in peri-urban Cambodian communities. J. Water Health 2013, 11, 489–506. [Google Scholar] [CrossRef] [PubMed]
- Whittington, D.; Pattanayak, S.; Yang, J.; Kumar, B. Household demand for improved piped water services in Kathmandu, Nepal. Water Policy 2002, 4, 531–556. [Google Scholar] [CrossRef]
- Kerstens, S.M.; Hutton, G.; Van Nes, A.; Firmansyah, I. Downstream Impacts of Water Pollution in the Upper Citarum River, West Java, Indonesia. Economic Assessment of Interventions to Improve Water Quality; Water and Sanitation Program, World Bank: Washington, DC, USA, 2013. [Google Scholar]
- Kremer, M.; Leino, J.; Miguel, E.; Zwane, A. Spring cleaning: A randomized evaluation of source water quality improvement. Q. J. Econ. 2011, 126, 145–205. [Google Scholar] [CrossRef] [PubMed]
- Cameron, J.; Jagals, P.; Hunter, P.; Pedley, S.; Pond, K. Economic assessments of small-scale drinking-water interventions in pursuit of MDG target 7c. Sci. Total Environ. 2011, 410–411, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Prihandrijanti, M.; Malisie, A.; Otterpohl, R. Cost-benefit analysis for centralized and decentralized wastewater treatment system (case study in Surabaya, Indonesia). In Efficient Management of Wastewater: Its Treatment and Reuse in Water-Scarce Countries; Al Baz, I., Otterpohl, R., Wendland, C., Eds.; Springer: Berlin/Heidelberg, Germany, 2008. [Google Scholar]
- Rheingans, R.; Kukla, M.; Faruque, A.S.G.; Sur, D.; Zaidi, A.K.; Nasrin, D.; Farag, T.H.; Levine, M.M.; Kotloff, K.L. Determinants of household costs associated with childhood diarrhea in 3 South Asian settings. Clin. Infect. Dis. 2012, 55, S327–S335. [Google Scholar] [CrossRef] [PubMed]
- Ferro, G.; Lentini, E.; Mercadier, A. Economies of scale in the water sector: A survey of the empirical literature. J. Water Sanit. Hyg. Dev. 2011, 1, 179–193. [Google Scholar] [CrossRef]
- Haller, L.; Hutton, G.; Bartram, J. Estimating the costs and health benefits of water and sanitation improvements at global level. J. Water Health 2007, 5, 467–480. [Google Scholar] [CrossRef] [PubMed]
- Günther, I.; Fink, G. Water and Sanitation to Reduce Child Mortality: The Impact and Cost of Water and Sanitation Infrastructure; World Bank: Washington, DC, USA, 2011. [Google Scholar]
- Borghi, J.; Guinness, L.; Ouedraogo, J.; Curtis, V. Is hygiene promotion cost-effective? A case study in Burkina Faso. Trop. Med. Int. Health 2002, 7, 960–969. [Google Scholar] [CrossRef] [PubMed]
- Randall, C. Potential societal and economic impacts of wastewater nutrient removal and recycling. Water Sci. Technol. 2003, 48, 11–17. [Google Scholar] [PubMed]
- Lise, W.; Van der Veeren, R. Cost-effective nutrient emission reductions in the Rhine river basin. Integr. Assess. 2002, 3, 321–342. [Google Scholar] [CrossRef]
- Franceys, R.; Pezon, C. Services Are Forever: The Importance of Capital Maintenance (Capmanex) in Ensuring Sustainable Wash Services; WASHCost Briefing Note 1b; IRC International Water and Sanitation Centre: The Hague, The Netherlands, 2010. [Google Scholar]
- Coffey, D.; Gupta, A.; Hathi, P.; Khurana, N.; Spears, D.; Srivastav, N.; Vyas, S. Revealed Preference for Open Defecation: Evidence from a New Survey in Rural North India; Research Institute for Compassionate Economics: Amston, CT, USA, 2014. [Google Scholar]
- Starkl, M.; Brunner, N.; Stenström, T.-A. Why do water and sanitation systems for the poor still fail? Policy analysis in economically advanced developing countries. Environ. Sci. Technol. 2013, 47, 6102–6110. [Google Scholar] [CrossRef] [PubMed]
- Foster, T. Predictors of sustainability for community-managed handpumps in sub-Saharan Africa: Evidence from Liberia, Sierra Leone and Uganda. Environ. Sci. Technol. 2013, 47, 12037–12046. [Google Scholar] [CrossRef] [PubMed]
- Vindigni, S.M.; Riley, P.L.; Jhung, M. Systematic review: Handwashing behaviour in low-to middle-income countries: Outcome measures and behaviour maintenance. Trop. Med. Int. Health 2011, 16, 466–477. [Google Scholar] [CrossRef] [PubMed]
- Lockwood, H.; Smits, S. Supporting Rural Water Supply. Moving towards A Service Delivery Approach; Practical Action Publishing Ltd.: Rugby, UK, 2011. [Google Scholar]
- Nelson, M.; Odum, H.; Brown, M.; Alling, A. “Living off the land”: Resource efficiency of wetland wastewater treatment. Adv. Space Res. 2001, 27, 1547–1556. [Google Scholar] [CrossRef]
- Préndeza, M.; Lara-González, S. Application of strategies for sanitation management in wastewater treatment plants in order to control/reduce greenhouse gas emissions. J. Environ. Manag. 2008, 88, 658–664. [Google Scholar] [CrossRef] [PubMed]
- Keller, J.; Hartley, K. Greenhouse gas production in wastewater treatment: Process selection is the major factor. Water Sci. Technol. 2003, 47, 43–48. [Google Scholar] [PubMed]
- Organisation for Economic Cooperation and Development (OECD). Strategic Financial Planning for Water Supply and Sanitation; Organisation for Economic Cooperation and Development: Paris, France, 2009. [Google Scholar]
- UN-Water. Investing in Water and Sanitation: Increasing Access, Reducing Inequalities; Special Report for the Sanitation and Water for All (SWA) High Level Meeting; Global-Level Analysis and Assessment of Sanitation and Drinking-Water (GLAAS); World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Camdessus, M. Financing Water for All; Report of the World Panel on Financing Water Infrastructure; World Water Council, Global Water Partnership: Marseille, France, 2003. [Google Scholar]
- Rodriguez, D.; van den Berg, C.; McMahon, A. Investing in Water Infrastructure: Capital, Operations and Maintenance; Water Papers; Water Partnership Program, World Bank: Washington, DC, USA, 2012. [Google Scholar]
- Mehta, M.; Fugelsnes, T.; Virjee, K. Financing the millennium development goals for water and sanitation: What will it take? Water Resour. Dev. 2005, 21, 239–252. [Google Scholar] [CrossRef]
- Hutton, G. Monitoring “Affordability” of Water and Sanitation Services After 2015: Review of Global Indicator Options; United Nations Office of the High Commissioner for Human Rights: Geneva, Switzerland, 2012. [Google Scholar]
- UNDP (United Nations Development Program). Beyond Scarcity: Power, Poverty and the Global Water Crisis; Human Development Report; UNDP: New York, NY, USA, 2006. [Google Scholar]
- Van Ginneken, M.; Netterstrom, U.; Bennett, A. More, Better, or Different Spending? Trends in Public Expenditure on Water and Sanitation in Sub-Saharan Africa; Water Partnership Program, World Bank: Washington, DC, USA, 2011. [Google Scholar]
| Service | Included | Excluded |
|---|---|---|
| Water supply | Water for drinking; Other water uses in the home (cooking, hygiene, sanitation, cleaning, laundry); Treatment, safe handling and storage of water | Water for productive uses |
| Sanitation | Toilets and onsite excreta management; Management of fecal sludge; Sewerage or combined sewer-drainage systems | Separate gray water management; Industrial wastewater management; Storm water drainage; Solid waste management |
| Hygiene | Hand washing; Menstrual hygiene management | Food hygiene; Environmental hygiene and cleanliness measures; Other personal hygiene practices, including face and body cleansing |
| Service | First Service Level (Termed “Basic WASH”) | Higher Level Service (Termed “Safe WatSan”) |
|---|---|---|
| Water | Percentage of population using a protected community source or piped water 1 with a total collection time of 30 min or less for a roundtrip including queuing (termed “basic” water) | Percentage of population using safely managed drinking water services. “Safely managed” refers to an improved1 drinking water source on premises accessible to all members of the household, which delivers sufficient water to meet domestic needs, was functional >12 days in the last 2 weeks, meets WHO guideline values for E. coli, fluoride and arsenic, and is subject to a verified risk management plan [3]. |
| Sanitation and hygiene | Percentage of population not practicing open defecation. Percentage of population using a basic, private sanitation facility (termed “adequate” sanitation) 2 | Percentage of population using safely managed sanitation services including a hand washing facility with soap and water. “Safely managed” refers to safe capture of fecal waste with isolation or treatment with safe disposal/reuse, either on or off site. When off-site, fecal waste is safely extracted and conveyed to treatment and disposal sites. |
| Percentage of population with handwashing facilities with soap and water at home. |
| Region | Water Supply | Sanitation | Hygiene | WASH |
|---|---|---|---|---|
| Africa | 229,316 | 126,294 | 122,955 | 367,605 |
| America | 6441 | 2370 | 5026 | 11,519 |
| Eastern Mediterranean | 50,409 | 24,441 | 28,699 | 81,064 |
| Europe | 1676 | 352 | 1972 | 3564 |
| South & Southeast Asia | 207,773 | 123,279 | 131,519 | 363,904 |
| Western Pacific | 6448 | 3709 | 6690 | 14,160 |
| World | 502,061 | 280,443 | 296,860 | 841,818 |
| Baseline | Intervention | |||
|---|---|---|---|---|
| Baseline water | Improved community source | Piped water, non-continuous | Piped water, high quality | Filter and safe storage in the household |
| Unimproved source | 0.89 (0.78, 1.01) | 0.77 (0.64, 0.92) | 0.19 (0.07, 0.50) | 0.53 (0.41, 0.67) |
| Improved community source | 0.86 (0.72, 1.03) | 0.21 (0.08, 0.56) | 0.59 (0.49, 0.78) | |
| Basic piped water | 0.57 (0.09, 0.65) | 0.69 (0.51, 0.93) | ||
| Baseline sanitation | Improved sanitation, no sewer | Sewer connection | ||
| Unimproved sanitation | 0.84 (0.77, 0.91) | 0.31 (0.27, 0.36) | ||
| Improved sanitation, no sewer | 0.37 (0.31, 0.44) | |||
| Baseline hygiene | General hygiene education | Handwashing with soap | ||
| No hygiene education or handwashing | 0.76 (0.67, 0.86) | 0.60 (0.53, 0.68) | ||
| Cost Component | Full Cost | Minimal Cost |
|---|---|---|
| Opportunity cost of raw water supply | 0.05 | 0.00 (“steal it“) |
| Storage and transmission to treatment plant | 0.10 | 0.07 (minimum storage) |
| Treatment to drinking water standards | 0.10 | 0.04 (simple chlorination) |
| Distribution of water to households | 0.60 | 0.24 (PVC pipe) |
| Collection of wastewater from home and conveyance to wastewater treatment plant | 0.80 | 0.30 (condominial sewers) |
| Wastewater treatment | 0.30 | 0.15 (simple lagoon) |
| Damages associated with discharge of treated wastewater | 0.05 | 0.00 (“someone else’s problem“) |
| Total | 2.00 | 0.80 |
| Benefit | Water | Sanitation |
|---|---|---|
| Health: burden of disease | Averted cases of diarrhoeal disease; Reduced malnutrition, enteropathy, and malnutrition-related conditions (stunting) Less dehydration from lack of access to water; Less disaster-related health impacts | Averted cases of diarrheal disease; Averted cases of helminths, polio, and eye diseases; Reduced malnutrition, enteropathy, and malnutrition-related conditions (stunting); Less dehydration from insufficient water intake due to poor latrine access; Less disaster-related health impacts |
| Health: economic savings | Costs related to diseases such as health care, productivity losses and premature mortality | Costs related to diseases, such as health care, productivity losses, and premature mortality |
| Convenience time savings | Saved travel and waiting time for water collection | Saved travel and waiting time from having nearby private toilet |
| Educational benefits | Improved educational levels due to higher school enrolment and attendance rates from school water; Higher attendance and educational attainment due to improved health | Improved educational levels due to higher school enrolment and attendance rates from school sanitation; Higher attendance and educational attainment due to improved health |
| Social benefits | Leisure and non-use values of water resources and reduced effort of averted water hauling and gender impacts | Safety, privacy, dignity, comfort, status, prestige, aesthetics, gender impacts |
| Water access benefits | Pretreated water at lower costs leads to averted treatment costs for households | Less pollution of water supply and hence reduced water treatment costs |
| Reuse | Soil conditioner and fertilizer; Energy production; Safe use of wastewater | |
| Economic impacts | Incomes from more tourism and business investment; Employment opportunity in water provision; Rise in value of property | Incomes from more tourism and business investment; Employment opportunity in sanitation supply chain; Rise in value of property |
| Study and Intervention | Benefit-Cost Ratio |
|---|---|
| Whittington et al. (2009)—modeled approach | |
| Networked water and sewerage services | 0.65 |
| Deep borehole with public hand pump | 4.64 |
| Household water treatment (bio-sand filters) | 2.48 |
| Total sanitation campaign (South Asia) | 3.00 |
| Hutton (2013)—modeled approach | |
| Improved water supply (JMP definition) | 2.00 |
| Improved sanitation (JMP definition) | 5.50 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hutton, G.; Chase, C. The Knowledge Base for Achieving the Sustainable Development Goal Targets on Water Supply, Sanitation and Hygiene. Int. J. Environ. Res. Public Health 2016, 13, 536. https://doi.org/10.3390/ijerph13060536
Hutton G, Chase C. The Knowledge Base for Achieving the Sustainable Development Goal Targets on Water Supply, Sanitation and Hygiene. International Journal of Environmental Research and Public Health. 2016; 13(6):536. https://doi.org/10.3390/ijerph13060536
Chicago/Turabian StyleHutton, Guy, and Claire Chase. 2016. "The Knowledge Base for Achieving the Sustainable Development Goal Targets on Water Supply, Sanitation and Hygiene" International Journal of Environmental Research and Public Health 13, no. 6: 536. https://doi.org/10.3390/ijerph13060536






