Hybridization Capture-Based Next-Generation Sequencing to Evaluate Coding Sequence and Deep Intronic Mutations in the NF1 Gene
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Capture Probe Set Design
2.3. Targeted Capture Library Construction and Next-Generation Sequencing
2.4. Bioinformatic Analysis of Next-Generation Sequencing Data
2.5. In Silico Predictions
2.6. Confirmatory Sanger Sequencing
3. Results
3.1. Sequencing Statistics
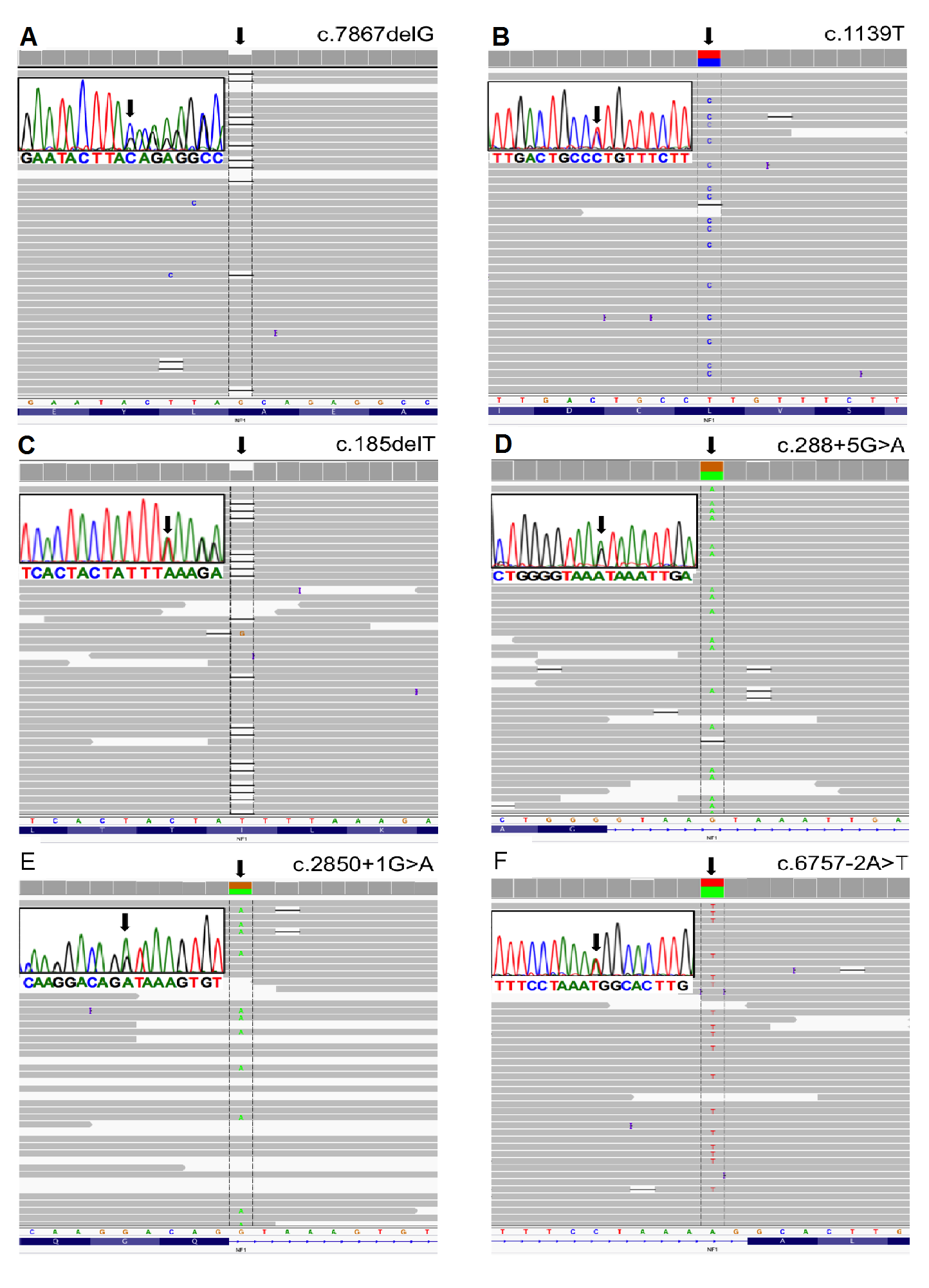
3.2. Mutation Detection
4. Discussion
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Uusitalo, E.; Leppävirta, J.; Koffert, A.; Suominen, S.; Vahtera, J.; Vahlberg, T.; Pöyhönen, M.; Peltonen, J.; Peltonen, S. Incidence and mortality of neurofibromatosis: A total population study in Finland. J. Investig. Dermatol. 2015, 135, 904–906. [Google Scholar] [CrossRef] [PubMed]
- Cunha, K.S.G.; Geller, M. Advances in Neurofibromatosis Research; Nova Science Publishers Inc.: Hauppauge, NY, USA, 2011. [Google Scholar]
- Pasmant, E.; Parfait, B.; Luscan, A.; Goussard, P.; Briand-Suleau, A.; Laurendeau, I.; Fouveaut, C.; Leroy, C.; Montadert, A.; Wolkenstein, P.; et al. Neurofibromatosis type 1 molecular diagnosis: What can NGS do for you when you have a large gene with loss of function mutations? Eur. J. Hum. Genet. EJHG 2015, 23, 596–601. [Google Scholar] [CrossRef] [PubMed]
- Clementi, M.; Barbujani, G.; Turolla, L.; Tenconi, R. Neurofibromatosis-1: A maximum likelihood estimation of mutation rate. Hum. Genet. 1990, 84, 116–118. [Google Scholar] [CrossRef] [PubMed]
- De Luca, A.; Schirinzi, A.; Buccino, A.; Bottillo, I.; Sinibaldi, L.; Torrente, I.; Ciavarella, A.; Dottorini, T.; Porciello, R.; Giustini, S.; et al. Novel and recurrent mutations in the NF1 gene in Italian patients with neurofibromatosis type 1. Hum. Mutat. 2004, 23, 629. [Google Scholar] [CrossRef] [PubMed]
- Griffiths, S.; Thompson, P.; Frayling, I.; Upadhyaya, M. Molecular diagnosis of neurofibromatosis type 1: 2 years experience. Fam. Cancer 2007, 6, 21–34. [Google Scholar] [CrossRef] [PubMed]
- Uusitalo, E.; Hammais, A.; Palonen, E.; Brandt, A.; Mäkelä, V.-V.; Kallionpää, R.; Jouhilahti, E.-M.; Pöyhönen, M.; Soini, J.; Peltonen, J.; et al. Neurofibromatosis type 1 gene mutation analysis using sequence capture and high-throughput sequencing. Acta Derm. Venereol. 2014, 94, 663–666. [Google Scholar] [CrossRef] [PubMed]
- Upadhyaya, M. The Molecular Biology of Neurofibromatosis Type 1; Morgan & Claypool: Williston, VT, USA, 2014. [Google Scholar]
- Messiaen, L.M.; Callens, T.; Mortier, G.; Beysen, D.; Vandenbroucke, I.; Van Roy, N.; Speleman, F.; Paepe, A.D. Exhaustive mutation analysis of the NF1 gene allows identification of 95% of mutations and reveals a high frequency of unusual splicing defects. Hum. Mutat. 2000, 15, 541–555. [Google Scholar] [CrossRef]
- Flanagan, S.E.; Xie, W.; Caswell, R.; Damhuis, A.; Vianey-Saban, C.; Akcay, T.; Darendeliler, F.; Bas, F.; Guven, A.; Siklar, Z.; et al. Next-Generation Sequencing Reveals Deep Intronic Cryptic ABCC8 and HADH Splicing Founder Mutations Causing Hyperinsulinism by Pseudoexon Activation. Am. J. Hum. Genet. 2013, 92, 131–136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stumpf, D.A.; Alksne, J.F.; Annegers, J.F.; Brown, S.S.; Conneally, P.M.; Housman, D.; Leppert, M.F.; Miller, J.P.; Moss, M.L.; Pileggi, A.J.; et al. Neurofibromatosis. Conference statement. National Institutes of Health Consensus Development Conference. Arch Neurol. 1988, 45, 575–578. [Google Scholar]
- Ars, E.; Kruyer, H.; Morell, M.; Pros, E.; Serra, E.; Ravella, A.; Estivill, X.; Lázaro, C. Recurrent mutations in the NF1 gene are common among neurofibromatosis type 1 patients. J. Med. Genet. 2003, 40, e82. [Google Scholar] [CrossRef] [PubMed]
- Forzan, M. Functional Splicing Assay mediante l’utilizzo di minigeni plasmidici nel gene NF1. Ph.D. Thesis, Università degli Studi di Padova, Padova, Italy, 2010. [Google Scholar]
- Mattocks, C.; Baralle, D.; Tarpey, P. Automated comparative sequence analysis identifies mutations in 89% of NF1 patients and confirms a mutation cluster in exons 11–17 distinct from the GAP related domain. Br. Med. J. 2004, 41, e48. [Google Scholar] [CrossRef]
- Van Minkelen, R.; van Bever, Y.; Kromosoeto, J.N.R.; Withagen-Hermans, C.J.; Nieuwlaat, A.; Halley, D.J.J.; van den Ouweland, A.M.W. A clinical and genetic overview of 18 years neurofibromatosis type 1 molecular diagnostics in the Netherlands. Clin. Genet. 2014, 85, 318–327. [Google Scholar] [CrossRef] [PubMed]
- Balla, B.; Árvai, K.; Horváth, P.; Tobiás, B.; Takács, I.; Nagy, Z.; Dank, M.; Fekete, G.; Kósa, J.P.; Lakatos, P. Fast and robust next-generation sequencing technique using ion torrent personal genome machine for the screening of neurofibromatosis type 1 (NF1) gene. J. Mol. Neurosci. MN 2014, 53, 204–210. [Google Scholar] [CrossRef] [PubMed]
- Chou, L.-S.; Liu, C.-S.J.; Boese, B.; Zhang, X.; Mao, R. DNA sequence capture and enrichment by microarray followed by next-generation sequencing for targeted resequencing: Neurofibromatosis type 1 gene as a model. Clin. Chem. 2010, 56, 62–72. [Google Scholar] [CrossRef] [PubMed]
- Hutter, S.; Piro, R.M.; Waszak, S.M.; Kehrer-Sawatzki, H.; Friedrich, R.E.; Lassaletta, A.; Witt, O.; Korbel, J.O.; Lichter, P.; Schuhmann, M.U.; et al. No correlation between NF1 mutation position and risk of optic pathway glioma in 77 unrelated NF1 patients. Hum. Genet. 2016, 135, 469–475. [Google Scholar] [CrossRef] [PubMed]
- Maruoka, R.; Takenouchi, T.; Torii, C.; Shimizu, A.; Misu, K.; Higasa, K.; Matsuda, F.; Ota, A.; Tanito, K.; Kuramochi, A.; et al. The use of next-generation sequencing in molecular diagnosis of neurofibromatosis type 1: A validation study. Genet. Test. Mol. Biomark. 2014, 18, 722–735. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, S.; Dai, Y.; Liang, S.; Chen, H.; Wang, Y.; Tang, L.; Wu, J.; Huang, H. A novel mutation in NF1 is associated with diverse intra-familial phenotypic variation and astrocytoma in a Chinese family. J. Clin. Neurosci. Off. J. Neurosurg. Soc. Australas. 2016, 31, 182–184. [Google Scholar] [CrossRef] [PubMed]
- Calì, F.; Chiavetta, V.; Ruggeri, G.; Piccione, M.; Selicorni, A.; Palazzo, D.; Bonsignore, M.; Cereda, A.; Elia, M.; Failla, P.; et al. Mutation spectrum of NF1 gene in Italian patients with neurofibromatosis type 1 using Ion Torrent PGMTM platform. Eur. J. Med. Genet. 2016. [Google Scholar] [CrossRef] [PubMed]
- Mamanova, L.; Coffey, A.J.; Scott, C.E.; Kozarewa, I.; Turner, E.H.; Kumar, A.; Howard, E.; Shendure, J.; Turner, D.J. Target-enrichment strategies for next-generation sequencing. Nat. Methods 2010, 7, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Galindo-González, L.; Pinzón-Latorre, D.; Bergen, E.A.; Jensen, D.C.; Deyholos, M.K. Ion Torrent sequencing as a tool for mutation discovery in the flax (Linum usitatissimum L.) genome. Plant Methods 2015, 11, 19. [Google Scholar] [CrossRef] [PubMed]
- Valero, M.C.; Martín, Y.; Hernández-Imaz, E.; Marina Hernández, A.; Meleán, G.; Valero, A.M.; Javier Rodríguez-Álvarez, F.; Tellería, D.; Hernández-Chico, C. A highly sensitive genetic protocol to detect NF1 mutations. J. Mol. Diagn. JMD 2011, 13, 113–122. [Google Scholar] [CrossRef] [PubMed]
- Summerer, D.; Schracke, N.; Wu, H.; Cheng, Y.; Bau, S.; Stähler, C.F.; Stähler, P.F.; Beier, M. Targeted high throughput sequencing of a cancer-related exome subset by specific sequence capture with a fully automated microarray platform. Genomics 2010, 95, 241–246. [Google Scholar] [CrossRef] [PubMed]
- Chilamakuri, C.S.R.; Lorenz, S.; Madoui, M.-A.; Vodák, D.; Sun, J.; Hovig, E.; Myklebost, O.; Meza-Zepeda, L.A. Performance comparison of four exome capture systems for deep sequencing. BMC Genom. 2014, 15. [Google Scholar] [CrossRef] [PubMed]
- Sabbagh, A.; Pasmant, E.; Imbard, A.; Luscan, A.; Soares, M.; Blanché, H.; Laurendeau, I.; Ferkal, S.; Vidaud, M.; Pinson, S.; et al. NF1 molecular characterization and neurofibromatosis type I genotype-phenotype correlation: The French experience. Hum. Mutat. 2013, 34, 1510–1518. [Google Scholar] [CrossRef] [PubMed]
- Ars, E.; Serra, E.; Garcia, J.; Kruyer, H.; Gaona, A.; Lazaro, C.; Estivill, X. Mutations affecting mRNA splicing are the most common molecular defects in patients with neurofibromatosis type 1. Hum. Mol. Genet. 2000, 9, 237. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Nettleton, D.; Ying, K. Copy number variation detection using next generation sequencing read counts. BMC Bioinform. 2014, 15, 109. [Google Scholar] [CrossRef] [PubMed]
- Abou Tayoun, A.N.; Tunkey, C.D.; Pugh, T.J.; Ross, T.; Shah, M.; Lee, C.C.; Harkins, T.T.; Wells, W.A.; Tafe, L.J.; Amos, C.I.; et al. A comprehensive assay for CFTR mutational analysis using next-generation sequencing. Clin. Chem. 2013, 59, 1481–1488. [Google Scholar] [CrossRef] [PubMed]
- Poliseno, L. (Ed.) Pseudogenes; Methods in Molecular Biology Series; Springer: New York, NY, USA, 2014; Volume 1167.
- Messiaen, L.; Wimmer, K. Mutation analysis of the NF1 gene by cDNA-based sequencing of the coding region. In Advances in Neurofibromatosis Research; Cunha, K.S.G., Geller, M., Eds.; Nova Science Publishers Inc.: New York, NY, USA, 2012; pp. 89–108. [Google Scholar]
- Wimmer, K.; Roca, X.; Beiglböck, H.; Callens, T.; Etzler, J.; Rao, A.R.; Krainer, A.R.; Fonatsch, C.; Messiaen, L. Extensive in silico analysis of NF1 splicing defects uncovers determinants for splicing outcome upon 5′ splice-site disruption. Hum. Mutat. 2007, 28, 599–612. [Google Scholar] [CrossRef] [PubMed]
- Svaasand, E.K.; Engebretsen, L.F.; Ludvigsen, T.; Brechan, W.; Sjursen, W. A Novel Deep Intronic Mutation Introducing a Cryptic Exon Causing Neurofibromatosis Type 1 in a Family with Highly Variable Phenotypes: A Case Study. Hered. Genet. Curr. Res. 2015, 4, 3. [Google Scholar] [CrossRef]
- Castellanos, E.; Rosas, I.; Solanes, A.; Bielsa, I.; Lázaro, C.; Carrato, C.; Hostalot, C.; Prades, P.; Roca-Ribas, F.; Blanco, I.; et al. In vitro antisense therapeutics for a deep intronic mutation causing Neurofibromatosis type 2. Eur. J. Hum. Genet. 2013, 21, 769–773. [Google Scholar] [CrossRef] [PubMed]
- Coutinho, G.; Xie, J.; Du, L.; Brusco, A.; Krainer, A.R.; Gatti, R.A. Functional significance of a deep intronic mutation in the ATM gene and evidence for an alternative exon 28a. Hum. Mutat. 2005, 25, 118–124. [Google Scholar] [CrossRef] [PubMed]
- Jian, X.; Boerwinkle, E.; Liu, X. In silico tools for splicing defect prediction: A survey from the viewpoint of end users. Genet. Med. 2014, 16, 497–503. [Google Scholar] [CrossRef] [PubMed]

| Patient Number | Gender | Age | Family History | Number of Skin Neurofibromas | Superficial Plexiform Neurofibroma | Number of Café-au-Lait Macules | Inguinal/Axillary Freckling |
|---|---|---|---|---|---|---|---|
| NF.01 | Female | 46 | No | 200–499 | Yes | 3 | Yes |
| NF.14 | Female | 54 | Yes | 500–1000 | Yes | 20 | Yes |
| NF.19 | Female | 26 | No | 500–1000 | No | 35 | Yes |
| NF.26 | Male | 52 | Yes | >1000 | No | 3 | Yes |
| NF.27 | Female | 55 | Yes | >1000 | No | 4 | Yes |
| NF.42 | Male | 47 | No | 200–499 | No | 9 | Yes |
| NF.54 | Female | 32 | No | 200–499 | No | 12 | Yes |
| NF.63 | Female | 48 | Yes | 500–1000 | No | 12 | Yes |
| NF.78 | Female | 13 | Yes | <10 | No | 44 | Yes |
| NF.83 | Male | 48 | No | >1000 | Yes | 8 | Yes |
| NF.84 | Female | 45 | Yes | 200–499 | Yes | 28 | Yes |
| NF.85 | Male | 24 | Yes | 200–499 | Yes | 48 | Yes |
| NF.87 | Male | 34 | Yes | 200–499 | No | 6 | Yes |
| NF.91 | Male | 72 | No | >1000 | No | 2 | Yes |
| NF.96 | Male | 41 | Yes | 100–199 | No | 17 | No |
| Patient Number | Location | Sequences (5′–3′) | Tm | Amplicon |
|---|---|---|---|---|
| NF.01 | Intron 11 | F: TAATGAGCCAGGGCATTGTACC | 66 °C | 385 pb |
| R: CTTTCACCAAGTACACTGAGGC | 66 °C | |||
| NF.19 * | Exon 1 | F: CACAGACCCTCTCCTTGCCTCTTC | 71 °C | 243 pb |
| R: TACCTCCCCTCACCTACTCTGTCC | 68 °C | |||
| NF.26 NF.27 | Exon 43 | F: TGCTGTTTGGCATTAGCAAAGT | 62 °C | 302 pb |
| R: TGTTACCAATAACACAGTCCATGC | 68 °C | |||
| NF.42 | Exon 37 | F: ATACCGGGCCTAGCAATCGC | 64 °C | 133 pb |
| R: TTGGTGTACTCCCTGACCCAGG | 70 °C | |||
| NF.54 | Exon 2 | F: AGCAGAACACACATACCAAAGTCAG | 72 °C | 158 pb |
| R: AATTCCCCAAAACACAGTAACCCAA | 72 °C | |||
| NF.63 | Exon 3/Intron 3 | F: GATGTGTGTTGATTGGTAGCAGA | 66 °C | 245 pb |
| R: GGACTGTCCTCTTGGTCCACA | 66 °C | |||
| NF.78 | Exon 54 | F: CTTGGCAGGCTACACTGGT | 60 °C | 158 pb |
| R: ACTTAAAGACAGGCACGAAGGT | 64 °C | |||
| NF.83 | Exon 21 | F: AAGAAATTTGACACTCGGCTGAT | 64 °C | 483 pb |
| R: TGCTGACAGGTGTATCTGCG | 62 °C | |||
| NF.85 NF.84 NF.14 | Exon 10 | F: AGCTGGATTTTACTGCCATTTGTG | 68 °C | 233 pb |
| R: TAAAGTGTTGGTTGTTGTGAGGG | 66 °C | |||
| NF.91 NF.87 | Exon 21/Intron 21 | F: CCTGCTCTGTATCCAATGCTAT | 64 °C | 133 pb |
| R: GCTTATTTCAAACAAGTCACTCT | 62 °C | |||
| NF.96 | Intron 45/Exon 46 | F: AGCTAGCTACCAAGATCACCA | 62 °C | 297 pb |
| R: ACACTGATACCCAAAATGAATGC | 64 °C |
| Chromosome | Percentage (%) |
|---|---|
| Chr2 | 1.72 |
| Chr12 | 0.84 |
| Chr14 | 1.27 |
| Chr15 | 2.57 |
| Chr17 | 83.94 |
| Chr18 | 1.09 |
| Chr21 | 1.06 |
| Chr22 | 1.81 |
| Other chromosomes | 5.71 |
| Patient Number | Exon/Intron (NG_009018.1) | DNA Mutation gDNA Level (NG_009018.1) | DNA Mutation cDNA Level (NM_000267.3) | Predicted Protein (NP_000258.1) | Mutation Type | Variant Effect | References |
|---|---|---|---|---|---|---|---|
| NF.01 | IVS11 | g.29530107A > G | c.1260 + 1604A > G | p.N420_S421insLTT* (also noted as p.S421LfsX4) | Substitution | Splicing (deep intronic mutation) | Valero et al. [24]; Sabbagh et al. [27]; van Minkelen et al. [15] |
| NF.26 NF.27 | E43 | g.29664504C > G | c.6483C > G | p.Y2161* | Substitution | Splicing b | Ars et al. [28] |
| NF.42 | E37 | g.29653014dup | c.4949dupA | p.Y1650* | Duplication | Frameshift truncation | Mattocks et al. [14]; van Minkelen et al. [15] |
| NF.54 | E2 | g.29483125del | c.185delT | p.L62* | Deletion | Frameshift truncation | Forzan [13] |
| NF.63 | IVS3 | g.29486116G > A | c.288 + 5G > A | p.(?) | Substitution | Splicing | ND |
| NF.78 | E54 | g.29684347del | c.7867delG | p.A2623Qfs*35 | Deletion | Frameshift truncation | ND |
| NF.83 | E21 | g.29556173T > G | c.2540T > G | p.L847R | Substitution | Missense | van Minkelen et al. [15]; De Luca et al. [5]; Cali et al. [21] |
| NF.85 NF.84 NF.14 | E10 | g.29528131T > C | c.1139T > C | p.L380P | Substitution | Missense | van Minkelen et al. [15] |
| NF.91 NF.87 | IVS21 | g.29556484G > A | c.2850 + 1G > A | p.(?) | Substitution | Splicing | Ars et al. [28] van Minkelen et al. [15] |
| NF.96 | IVS45 | g.29665720A > T | c.6757 − 2A > T | p.(?) | Substitution | Splicing | Pasmant et al. [3] |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cunha, K.S.; Oliveira, N.S.; Fausto, A.K.; De Souza, C.C.; Gros, A.; Bandres, T.; Idrissi, Y.; Merlio, J.-P.; De Moura Neto, R.S.; Silva, R.; et al. Hybridization Capture-Based Next-Generation Sequencing to Evaluate Coding Sequence and Deep Intronic Mutations in the NF1 Gene. Genes 2016, 7, 133. https://doi.org/10.3390/genes7120133
Cunha KS, Oliveira NS, Fausto AK, De Souza CC, Gros A, Bandres T, Idrissi Y, Merlio J-P, De Moura Neto RS, Silva R, et al. Hybridization Capture-Based Next-Generation Sequencing to Evaluate Coding Sequence and Deep Intronic Mutations in the NF1 Gene. Genes. 2016; 7(12):133. https://doi.org/10.3390/genes7120133
Chicago/Turabian StyleCunha, Karin Soares, Nathalia Silva Oliveira, Anna Karoline Fausto, Carolina Cruz De Souza, Audrey Gros, Thomas Bandres, Yamina Idrissi, Jean-Philippe Merlio, Rodrigo Soares De Moura Neto, Rosane Silva, and et al. 2016. "Hybridization Capture-Based Next-Generation Sequencing to Evaluate Coding Sequence and Deep Intronic Mutations in the NF1 Gene" Genes 7, no. 12: 133. https://doi.org/10.3390/genes7120133






