Risk and Resilience Factors Related to Parental Bereavement Following the Death of a Child with a Life-Limiting Condition
Abstract
:1. Introduction
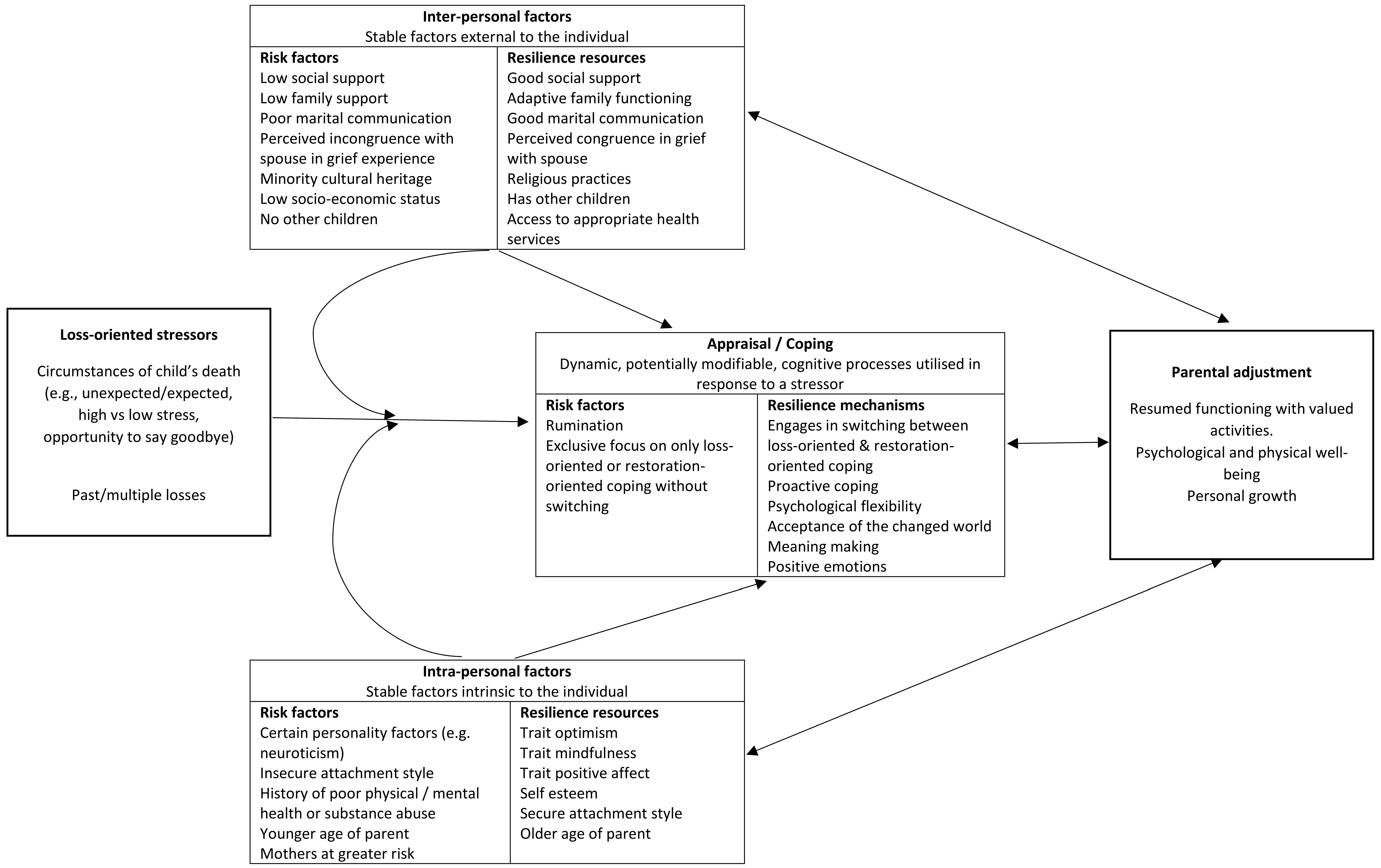
2. Parental Bereavement Following the Death of a Child with a Life-Limiting Condition
3. The Role of Risk and Resilience Factors in Parental Bereavement
4. Parental Bereavement Outcomes
5. Loss-Oriented Stressors
5.1. Circumstances Surrounding the Death
5.2. Multiple Losses
6. Inter-Personal Resources
6.1. Marital Factors
6.2. Social Support
6.3. Religious Practices
7. Intra-Personal Resources
7.1. Personality
7.2. Attachment Style
7.3. Gender
7.4. Predisposing Personal Vulnerabilities
8. Coping and Appraisal
9. Challenges to Carrying Out Bereavement Research
10. Future Directions for Research and Clinical Practice
11. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Genevro, J.L.; Marshall, T.; Miller, T.; Center for the Advancement of Health. Report on bereavement and grief research. Death Stud. 2004, 28, 491–575. [Google Scholar] [PubMed]
- Middleton, W.; Raphael, B.; Burnett, P.; Martinek, N. A longitudinal study comparing bereavement phenomena in recently bereaved spouses, adult children and parents. Aust. N. Z. J. Psychiatry 1998, 32, 235–241. [Google Scholar] [CrossRef] [PubMed]
- Stroebe, M.S.; Folkman, S.; Hansson, R.O.; Schut, H. The prediction of bereavement outcome: Development of an integrative risk factor framework. Soc. Sci. Med. 2006, 63, 2440–2451. [Google Scholar] [CrossRef] [PubMed]
- Hazzard, A.; Weston, J.; Gutterres, C. After a child’s death: Factors related to parental bereavement. J. Dev. Behav. Pediatr. 1992, 13, 24–30. [Google Scholar] [PubMed]
- Lundin, T. Long-term outcome of bereavement. Br. J. Psychiatry 1984, 145, 424–428. [Google Scholar] [CrossRef] [PubMed]
- Breen, L.J. The effect of caring on post-bereavement outcome: Research gaps and practice priorities. Prog. Palliat. Care 2012, 20, 27–30. [Google Scholar] [CrossRef]
- Floyd, F.J.; Mailick Seltzer, M.; Greenberg, J.S.; Song, J. Parental bereavement during mid-to-later life: Pre-to postbereavement functioning and intrapersonal resources for coping. Psychol. Aging 2013, 28, 402–413. [Google Scholar] [CrossRef] [PubMed]
- Song, J.; Floyd, F.J.; Seltzer, M.M.; Greenberg, J.S.; Hong, J. Long-term effects of child death on parents’ health-related quality of life: A dyadic analysis. Fam. Relat. 2010, 59, 269–282. [Google Scholar] [CrossRef] [PubMed]
- Gilliland, G.; Fleming, S. A comparison of spousal anticipatory grief and conventional grief. Death Stud. 1998, 22, 541–569. [Google Scholar] [PubMed]
- Eakes, G.G.; Burke, M.L.; Hainsworth, M.A. Middle-range theory of chronic sorrow. J. Nurs. Scholarsh. 1998, 30, 179–184. [Google Scholar] [CrossRef]
- Rini, A.; Loriz, L. Anticipatory mourning in parents with a child who dies while hospitalized. J. Pediatr. Nurs. 2007, 22, 272–282. [Google Scholar] [CrossRef] [PubMed]
- Stewart, D.E.; Yuen, T. A systematic review of resilience in the physically Ill. Psychosomatics 2011, 52, 199–209. [Google Scholar] [CrossRef] [PubMed]
- Zautra, A.J.; Hall, J.S.; Murray, K.E.; Resilience Solutions Group 1. Resilience: A new integrative approach to health and mental health research. Health Psychol. Rev. 2008, 2, 41–64. [Google Scholar] [CrossRef]
- Kumpfer, K.L. Factors and Processes Contributing to Resilience. In Resilience and Development; Glantz, M.D., Johnson, J.L., Eds.; Springer: New York, NY, USA, 2002; pp. 179–224. [Google Scholar]
- Cousins, L.A.; Kalapurakkel, S.; Cohen, L.L.; Simons, L.E. Topical review: Resilience resources and mechanisms in pediatric chronic pain. J. Pediatr. Psychol. 2015, 40, 840–845. [Google Scholar] [CrossRef] [PubMed]
- Yi, J.P.; Vitaliano, P.P.; Smith, R.E.; Yi, J.C.; Weinger, K. The role of resilience on psychological adjustment and physical health in patients with diabetes. Br. J. Health Psychol. 2008, 13, 311–325. [Google Scholar] [CrossRef] [PubMed]
- Bonanno, G.A. Loss, trauma, and human resilience: Have we underestimated the human capacity to thrive after extremely aversive events? Am. Psychol. 2004, 59, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Bonanno, G.A.; Papa, A.; O’Neill, K. Loss and human resilience. Appl. Prev. Psychol. 2001, 10, 193–206. [Google Scholar] [CrossRef]
- Cohen, S.; Wills, T.A. Stress, social support, and the buffering hypothesis. Psychol. Bull. 1985, 98, 310–357. [Google Scholar] [CrossRef] [PubMed]
- Stroebe, W.; Zech, E.; Stroebe, M.S.; Abakoumkin, G. Does social support help in bereavement? J. Soc. Clin. Psychol. 2005, 24, 1030–1050. [Google Scholar] [CrossRef]
- Cowles, K.V. Cultural perspectives of grief: An expanded concept analysis. J. Adv. Nurs. 1996, 23, 287–294. [Google Scholar] [CrossRef] [PubMed]
- Hendrickson, K.C. Morbidity, mortality, and parental grief: A review of the literature on the relationship between the death of a child and the subsequent health of parents. Palliat. Support. Care 2009, 7, 109–119. [Google Scholar] [CrossRef] [PubMed]
- Stroebe, M.; Schut, H.; Stroebe, W. Health outcomes of bereavement. Lancet 2007, 370, 1960–1973. [Google Scholar] [CrossRef]
- Cacciatore, J.; Lacasse, J.R.; Lietz, C.A.; McPherson, J. A parent’s tears: Primary results from the traumatic experiences and resiliency study. Omega (Westport) 2014, 68, 183–205. [Google Scholar] [CrossRef]
- Rosenberg, A.R.; Baker, K.S.; Syrjala, K.; Wolfe, J. Systematic review of psychosocial morbidities among bereaved parents of children with cancer. Pediatr. Blood Cancer 2012, 58, 503–512. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Precht, D.H.; Mortensen, P.B.; Olsen, J. Mortality in parents after death of a child in Denmark: A nationwide follow-up study. Lancet 2003, 361, 363–367. [Google Scholar] [CrossRef]
- Li, J.; Laursen, T.M.; Precht, D.H.; Olsen, J.; Mortensen, P.B. Hospitalization for mental illness among parents after the death of a child. N. Engl. J. Med. 2005, 352, 1190–1196. [Google Scholar] [CrossRef] [PubMed]
- Rogers, C.H.; Floyd, F.J.; Seltzer, M.M.; Greenberg, J.; Hong, J. Long-term effects of the death of a child on parents’ adjustment in midlife. J. Fam. Psychol. 2008, 22, 203–211. [Google Scholar] [CrossRef] [PubMed]
- Prigerson, H.G.; Maciejewski, P.K. Grief and acceptance as opposite sides of the same coin: Setting a research agenda to study peaceful acceptance of loss. Br. J. Psychiatry 2008, 193, 435–437. [Google Scholar] [CrossRef] [PubMed]
- Najman, J.M.; Vance, J.C.; Boyle, F.; Embleton, G.; Foster, B.; Thearle, J. The impact of a child death on marital adjustment. Soc. Sci. Med. 1993, 37, 1005–1010. [Google Scholar] [CrossRef]
- Corden, A.; Sloper, P.; Sainsbury, R. Financial effects for families after the death of a disabled or chronically ill child: A neglected dimension of bereavement. Child Care Health Dev. 2002, 28, 199–204. [Google Scholar] [CrossRef] [PubMed]
- Bryant, R.A. Prolonged grief: Where to after diagnostic and statistical manual of mental disorders, 5th edition? Curr. Opin. Psychiatry 2014, 27, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Wakefield, J.C. The DSM-5 debate over the bereavement exclusion: Psychiatric diagnosis and the future of empirically supported treatment. Clin. Psychol. Rev. 2013, 33, 825–845. [Google Scholar] [CrossRef] [PubMed]
- Boelen, P.A.; Smid, G.E. The traumatic grief inventory self-report version (TGI-SR): Introduction and preliminary psychometric evaluation. J. Loss Trauma 2017, 22, 196–212. [Google Scholar] [CrossRef]
- Valdimarsdottir, U.; Helgason, A.R.; Furst, C.J.; Adolfsson, J.; Steineck, G. Awareness of husband’s impending death from cancer and long-term anxiety in widowhood: A nationwide follow-up. Palliat. Med. 2004, 18, 432–443. [Google Scholar] [CrossRef] [PubMed]
- Grande, G.E.; Farquhar, M.C.; Barclay, S.I.; Todd, C.J. Caregiver bereavement outcome: relationship with hospice at home, satisfaction with care, and home death. J. Palliat. Care 2004, 20, 69–77. [Google Scholar] [PubMed]
- Goodenough, B.; Drew, D.; Higgins, S.; Trethewie, S. Bereavement outcomes for parents who lose a child to cancer: Are place of death and sex of parent associated with differences in psychological functioning? Psycho-Oncology 2004, 13, 779–791. [Google Scholar] [CrossRef] [PubMed]
- Harper, M.; O’Connor, R.C.; O’Carroll, R.E. Factors associated with grief and depression following the loss of a child: A multivariate analysis. Psychol. Health. Med. 2014, 19, 247–252. [Google Scholar] [CrossRef] [PubMed]
- Castro, S.I.; Rocha, J.C. The moderating effects of previous losses and emotional clarity on bereavement outcome. J. Loss Trauma 2013, 18, 248–259. [Google Scholar] [CrossRef]
- Cherney, P.M.; Verhey, M.P. Grief among gay men associated with muitiple losses from aids. Death Stud. 1996, 20, 115–132. [Google Scholar] [CrossRef] [PubMed]
- Mercer, D.L.; Evans, J.M. The impact of multiple losses on the grieving process: An exploratory study. J. Loss Trauma 2006, 11, 219–227. [Google Scholar] [CrossRef]
- Parkes, C.M. Determinants of outcome following bereavement. Omega (Westport) 1976, 6, 303–323. [Google Scholar] [CrossRef]
- Sanders, C.M. Risk factors in bereavement outcome. J. Soc. Issues 1988, 44, 97–111. [Google Scholar] [CrossRef]
- Wijngaards-de Meij, L.; Stroebe, M.; Schut, H.; Stroebe, W.; Van den Bout, J.; Van der Heijden, P.G.; Dijkstra, I. Patterns of attachment and parents’ adjustment to the death of their child. Personal. Soc. Psychol. Bull. 2007, 33, 537–548. [Google Scholar] [CrossRef] [PubMed]
- Root, B.L.; Exline, J.J. The role of continuing bonds in coping with grief: Overview and future directions. Death Stud. 2014, 38, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Wing, D.G.; Burge-Callaway, K.; Rose Clance, P.; Armistead, L. Understanding gender differences in bereavement following the death of an infant: Implications of or treatment. Psychotherapy 2001, 38, 60–73. [Google Scholar] [CrossRef]
- Dyregrov, A.; Gjestad, R. Sexuality following the loss of a child. Death Stud. 2011, 35, 289–315. [Google Scholar] [CrossRef] [PubMed]
- Buyukcan-Tetik, A.; Finkenauer, C.; Schut, H.; Stroebe, M.; Stroebe, W. The impact of bereaved parents’ perceived grief similarity on relationship satisfaction. J. Fam. Psychol. 2017, 31, 409–419. [Google Scholar] [CrossRef] [PubMed]
- Stroebe, M.; Schut, H. Family matters in bereavement: Toward an integrative intra-interpersonal coping model. Perspect. Psychol. Sci. 2015, 10, 873–879. [Google Scholar] [CrossRef] [PubMed]
- Lang, A.; Gottlieb, L.N.; Amsel, R. Predictors of husbands’ and wives’ grief reactions following infant death: The role of marital intimacy. Death Stud. 1996, 20, 33–57. [Google Scholar] [CrossRef] [PubMed]
- Kamm, S.; Vandenberg, B. Grief communication, grief reactions and marital satisfaction in bereaved parents. Death Stud. 2001, 25, 569–582. [Google Scholar] [CrossRef] [PubMed]
- Sloper, P. Predictors of distress in parents of children with cancer: A prospective study. J. Pediatr. Psychol. 2000, 25, 79–91. [Google Scholar] [CrossRef] [PubMed]
- Waldrop, D.P. Caregiver grief in terminal illness and bereavement: A mixed-methods study. Health Soc. Work 2007, 32, 197–206. [Google Scholar] [CrossRef] [PubMed]
- Collins, A.; Hennessy-Anderson, N.; Hosking, S.; Hynson, J.; Remedios, C.; Thomas, K. Lived experiences of parents caring for a child with a life-limiting condition in Australia: A qualitative study. Palliat. Med. 2016, 30, 950–959. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Hoberman, H.M. Positive events and social supports as buffers of life change stress. J. Appl. Soc. Psychol. 1983, 13, 99–125. [Google Scholar] [CrossRef]
- Hogan, B.E.; Linden, W.; Najarian, B. Social support interventions: Do they work? Clin. Psychol. Rev. 2002, 22, 381–440. [Google Scholar] [CrossRef]
- Decinque, N.; Monterosso, L.; Dadd, G.; Sidhu, R.; Macpherson, R.; Aoun, S. Bereavement support for families following the death of a child from cancer: experience of bereaved parents. J. Psychosoc. Oncol. 2006, 24, 65–83. [Google Scholar] [CrossRef] [PubMed]
- Klass, D. The Spiritual Lives of Bereaved Parents; Psychology Press: Hove, UK, 1999. [Google Scholar]
- Reilly-Smorawski, B.; Armstrong, A.V.; Catlin, E.A. Bereavement support for couples following death of a baby: Program development and 14-year exit analysis. Death Stud. 2002, 26, 21–37. [Google Scholar] [CrossRef] [PubMed]
- Aho, A.L.; Tarkka, M.-T.; Åstedt-Kurki, P.; Sorvari, L.; Kaunonen, M. Evaluating a bereavement follow-up intervention for grieving fathers and their experiences of support after the death of a child—A pilot study. Death Stud. 2011, 35, 879–904. [Google Scholar] [CrossRef] [PubMed]
- Raitio, K.; Kaunonen, M.; Aho, A.L. Evaluating a bereavement follow-up intervention for grieving mothers after the death of a child. Scand. J. Caring Sci. 2015, 29, 510–520. [Google Scholar] [CrossRef] [PubMed]
- Cacciatore, J. Effects of support groups on post traumatic stress responses in women experiencing stillbirth. Omega (Westport) 2007, 55, 71–90. [Google Scholar] [CrossRef] [PubMed]
- Kreicbergs, U.C.; Lannen, P.; Onelov, E.; Wolfe, J. Parental grief after losing a child to cancer: Impact of professional and social support on long-term outcomes. J. Clin. Oncol. 2007, 25, 3307–3312. [Google Scholar] [CrossRef] [PubMed]
- Schwab, R. Bereaved parents and support group participation. Omega (Westport) 1996, 32, 49–61. [Google Scholar] [CrossRef]
- Ashton, W.A.; Fuehrer, A. Effects of gender and gender role identification of participant and type of social support resource on support seeking. Sex Roles 1993, 28, 461–476. [Google Scholar] [CrossRef]
- Mickelson, K.D. Seeking Social Support: Parents in Electronic Support Groups; Lawrence Erbaum Associates, Inc.: Mahwah, NJ, USA, 1997; pp. 157–178. [Google Scholar]
- Stroebe, W.; Stroebe, M.S. Bereavement and Health: The Psychological and Physical Consequences of Partner Loss; Cambridge University Press: Cambridge, UK, 1987. [Google Scholar]
- Cook, A.S.; Oltjenbruns, K.A. Dying and Grieving: Life Span and Family Perspectives; Holt, Rinehart, and Winston: New York, NY, USA, 1989; p. 491. [Google Scholar]
- Rosenblatt, P.C. Grief across Cultures: A Review and Research Agenda. In Handbook of Bereavement Research and Practice: Advances in Theory and Intervention; Stroebe, M.S., Hansson, R.O., Schut, H., Stroebe, W., Eds.; American Psychological Association: Washington, DC, USA, 2008; pp. 207–222. [Google Scholar]
- Katon, W.; Kleinman, A.; Rosen, G. Depression and somatization: A review: Part I. Am. J. Med. 1982, 72, 127–135. [Google Scholar] [CrossRef]
- Institute of Medicine (US) Committee for the Study of Health Consequences of the Stress of Bereavement. Bereavement: Reactions, Consequences, and Care; Osterweis, M., Solomon, F., Green, M., Eds.; National Academies Press (US): Washington, DC, USA, 1984. [Google Scholar]
- Rider, J.; Hayslip, B. Ambiguity of Loss, Anticipatory Grief, and Boundary Ambiguity in Caregiver Spouses and Parents; University of Texas: Denton, TX, USA, 1993. [Google Scholar]
- Pargament, K.I. The Psychology of Religion and Coping: Theory, Research, Practice; Guilford Press: New York, NY, USA, 2001. [Google Scholar]
- Walsh, K.; King, M.; Jones, L.; Tookman, A.; Blizard, R. Spiritual beliefs may affect outcome of bereavement: Prospective study. BMJ 2002, 324, 1551. [Google Scholar] [CrossRef] [PubMed]
- Stroebe, M.S. Commentary: Religion in coping with bereavement: Confidence of convictions or scientific scrutiny? Int. J. Psychol. Relig. 2004, 14, 23–36. [Google Scholar] [CrossRef]
- Sanders, C.M. A comparison of adult bereavement in the death of a spouse, child, and parent. Omega (Westport) 1980, 10, 303–322. [Google Scholar] [CrossRef]
- Robinson, T.; Marwit, S.J. An investigation of the relationship of personality, coping, and grief intensity among bereaved mothers. Death Stud. 2006, 30, 677–696. [Google Scholar] [CrossRef] [PubMed]
- Boelen, P.A. Optimism in prolonged grief and depression following loss: A three-wave longitudinal study. Psychiatry Res. 2015, 227, 313–317. [Google Scholar] [CrossRef] [PubMed]
- Moskowitz, J.T.; Folkman, S.; Acree, M. Do positive psychological states shed light on recovery from bereavement? Findings from a 3-year longitudinal study. Death Stud. 2003, 27, 471–500. [Google Scholar] [CrossRef] [PubMed]
- Bonanno, G.A.; Burton, C.L. Regulatory flexibility: An individual differences perspective on coping and emotion regulation. Perspect. Psychol. Sci. 2013, 8, 591–612. [Google Scholar] [CrossRef] [PubMed]
- Cacciatore, J.; Flint, M. ATTEND: Toward a mindfulness-based bereavement care model. Death Stud. 2012, 36, 61–82. [Google Scholar] [CrossRef] [PubMed]
- Boyraz, G.; Horne, S.G.; Sayger, T.V. Finding meaning in loss: The mediating role of social support between personality and two construals of meaning. Death Stud. 2012, 36, 519–540. [Google Scholar] [CrossRef] [PubMed]
- Baddeley, J.L.; Singer, J.A. Telling losses: Personality correlates and functions of bereavement narratives. J. Res. Personal. 2008, 42, 421–438. [Google Scholar] [CrossRef]
- Wijngaards-de Meij, L.; Stroebe, M.; Schut, H.; Stroebe, W.; Van den Bout, J.; Van der Heijden, P.; Dijkstra, I. Neuroticism and attachment insecurity as predictors of bereavement outcome. J. Res. Personal. 2007, 41, 498–505. [Google Scholar] [CrossRef]
- Scheier, M.F.; Carver, C.S. Optimism, coping, and health: Assessment and implications of generalized outcome expectancies. Health Psychol. 1985, 4, 219–247. [Google Scholar] [CrossRef] [PubMed]
- Nolen-Hoeksema, S.; Larson, J. Coping with Loss; Lawrence Erlbaum Associates, Inc.: Mahwah, NJ, USA, 1999. [Google Scholar]
- Carver, C.S.; Scheier, M.F.; Segerstrom, S.C. Optimism. Clin. Psychol. Rev. 2010, 30, 879–889. [Google Scholar] [CrossRef] [PubMed]
- Avvenuti, G.; Baiardini, I.; Giardini, A. Optimism’s explicative role for chronic diseases. Front. Psychol. 2016, 7, 295. [Google Scholar] [CrossRef] [PubMed]
- Nes, L.S.; Segerstrom, S.C. Dispositional optimism and coping: A meta-analytic review. Personal. Soc. Psychol. Rev. 2006, 10, 235–251. [Google Scholar] [CrossRef] [PubMed]
- Brissette, I.; Scheier, M.F.; Carver, C.S. The role of optimism in social network development, coping, and psychological adjustment during a life transition. J. Personal. Soc. Psychol. 2002, 82, 102–111. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, E.; Sakamoto, S.; Ono, Y.; Fujihara, S.; Kitamura, T. Hopelessness in a community population: Factorial structure and psychosocial correlates. J. Soc. Psychol. 1998, 138, 581–590. [Google Scholar] [CrossRef] [PubMed]
- Folkman, S. The case for positive emotions in the stress process. Anxiety Stress Coping 2008, 21, 3–14. [Google Scholar] [CrossRef] [PubMed]
- McCracken, L.M.; Morley, S. The psychological flexibility model: A basis for integration and progress in psychological approaches to chronic pain management. J. Pain 2014, 15, 221–234. [Google Scholar] [CrossRef] [PubMed]
- Kashdan, T.B.; Rottenberg, J. Psychological flexibility as a fundamental aspect of health. Clin. Psychol. Rev. 2010, 30, 865–878. [Google Scholar] [CrossRef] [PubMed]
- Stroebe, M.; Schut, H. The dual process model of coping with bereavement: Rationale and description. Death Stud. 1999, 23, 197–224. [Google Scholar] [PubMed]
- Gupta, S.; Bonanno, G.A. Complicated grief and deficits in emotional expressive flexibility. J. Abnorm. Psychol. 2011, 120, 635–643. [Google Scholar] [CrossRef] [PubMed]
- Brown, K.W.; Ryan, R.M. The benefits of being present: Mindfulness and its role in psychological well-being. J. Personal. Soc. Psychol. 2003, 84, 822–848. [Google Scholar] [CrossRef] [PubMed]
- Cacciatore, J.; Thieleman, K.; Osborn, J.; Orlowski, K. Of the soul and suffering: Mindfulness-based interventions and bereavement. Clin. Soc. Work J. 2014, 42, 269–281. [Google Scholar] [CrossRef]
- Kearney, J.A.; Byrne, M.W. Understanding parental behavior in pediatric palliative care: Attachment theory as a paradigm. Palliat. Support. Care 2015, 13, 1559–1568. [Google Scholar] [CrossRef] [PubMed]
- Berant, E.; Mikulincer, M.; Florian, V. The association of mothers’ attachment style and their psychological reactions to the diagnosis of infant’s congenital heart disease. J. Soc. Clin. Psychol. 2001, 20, 208–232. [Google Scholar] [CrossRef]
- Berant, E.; Mikulincer, M.; Florian, V. Attachment style and mental health: A 1-year follow-up study of mothers of infants with congenital heart disease. Personal. Soc. Psychol. Bull. 2001, 27, 956–968. [Google Scholar] [CrossRef]
- Berant, E.; Mikulincer, M.; Shaver, P.R. Mothers’ attachment style, their mental health, and their children’s emotional vulnerabilities: A 7-year study of children with congenital heart disease. J. Personal. 2008, 76, 31–66. [Google Scholar] [CrossRef] [PubMed]
- Meert, K.L.; Donaldson, A.E.; Newth, C.J.; Harrison, R.; Berger, J.; Zimmerman, J.; Anand, K.; Carcillo, J.; Dean, J.M.; Willson, D.F. Complicated grief and associated risk factors among parents following a child’s death in the pediatric intensive care unit. Arch. Pediatr. Adolesc. Med. 2010, 164, 1045–1051. [Google Scholar] [CrossRef] [PubMed]
- Mikulincer, M.; Shaver, P. Mental representations and attachment security. In Interpersonal Cognition; Guilford Press: New York, NY, USA, 2005; pp. 233–266. [Google Scholar]
- Mikulincer, M.; Shaver, P.R. Attachment in Adulthood: Structure, Dynamics, and Change; Guilford Press: New York, NY, USA, 2007. [Google Scholar]
- Field, N.P.; Gao, B.; Paderna, L. Continuing bonds in bereavement: An attachment theory based perspective. Death Stud. 2005, 29, 277–299. [Google Scholar] [CrossRef] [PubMed]
- Bowlby, E.J.M. Attachment and Loss: Sadness and Depression; Basic Books: New York, NY, USA, 1980; Volume 3. [Google Scholar]
- Stroebe, M. Gender differences in adjustment to bereavement: An empirical and theoretical review. Rev. Gen. Psychol. 2001, 5, 62–83. [Google Scholar] [CrossRef]
- Lang, A.; Gottlieb, L. Parental grief reactions and marital intimacy following infant death. Death Stud. 1993, 17, 233–255. [Google Scholar] [CrossRef]
- Alam, R.; Barrera, M.; D’Agostino, N.; Nicholas, D.B.; Schneiderman, G. Bereavement experiences of mothers and fathers over time after the death of a child due to cancer. Death Stud. 2012, 36, 1–22. [Google Scholar] [CrossRef] [PubMed]
- Lobb, E.A.; Kristjanson, L.J.; Aoun, S.M.; Monterosso, L.; Halkett, G.K.; Davies, A. Predictors of complicated grief: A systematic review of empirical studies. Death Stud. 2010, 34, 673–698. [Google Scholar] [CrossRef] [PubMed]
- Pilling, J.; Thege, B.K.; Demetrovics, Z.; Kopp, M.S. Alcohol use in the first three years of bereavement: A national representative survey. Subst. Abuse Treat. Prev. Policy 2012, 7, 3. [Google Scholar] [CrossRef] [PubMed]
- Pinquart, M.; Sörensen, S. Differences between caregivers and noncaregivers in psychological health and physical health: A meta-analysis. Psychol. Aging 2003, 18, 250–267. [Google Scholar] [CrossRef] [PubMed]
- Bunch, J. Recent bereavement in relation to suicide. J. Psychosom. Res. 1972, 16, 361–366. [Google Scholar] [CrossRef]
- Folkman, S. Revised coping theory and the process of bereavement. In Handbook of Bereavement Research: Consequences, Coping, and Care; Stroebe, M.S., Hansson, R.O., Stroebe, W., Schut, H., Eds.; American Psychological Association: Washington, DC, USA, 2001; pp. 563–584. [Google Scholar]
- Van der Houwen, K.; Stroebe, M.; Schut, H.; Stroebe, W.; Van den Bout, J. Mediating processes in bereavement: The role of rumination, threatening grief interpretations, and deliberate grief avoidance. Soc. Sci. Med. 2010, 71, 1669–1676. [Google Scholar] [CrossRef] [PubMed]
- Brammer, L.M.; Abrego, P.J. Intervention strategies for coping with transitions. J. Couns. Psychol. 1981, 9, 19–36. [Google Scholar] [CrossRef]
- Sohl, S.J.; Moyer, A. Refining the conceptualization of a future-oriented self-regulatory behavior: Proactive coping. Personal. Individ. Differ. 2009, 47, 139–144. [Google Scholar] [CrossRef] [PubMed]
- Aspinwall, L.G. Future-oriented thinking, proactive coping, and the management of potential threats to health and well-being. In The Oxford Handbook of Stress, Health and Coping; Folkman, S., Nathan, P.E., Eds.; Oxford University Press: Oxford, UK, 2011; pp. 334–365. [Google Scholar]
- Littlewood, J.L.; Cramer, D.; Hoekstra, J.; Humphrey, G. Gender differences in parental coping following their child’s death. Br. J. Guid. Couns. 1991, 19, 139–148. [Google Scholar] [CrossRef]
- Caserta, M.S.; Lund, D.A. Toward the development of an Inventory of Daily Widowed Life (IDWL): Guided by the dual process model of coping with bereavement. Death Stud. 2007, 31, 505–535. [Google Scholar] [CrossRef] [PubMed]
- Stroebe, M.S.; Schut, H. The dual process model of coping and bereavement: Overview and update. Grief Matters 2008, 11, 4. [Google Scholar]
- Wijngaards-de Meij, L.; Stroebe, M.; Schut, H.; Stroebe, W.; Bout, J.; Heijden, P.G.; Dijkstra, I. Parents grieving the loss of their child: Interdependence in coping. Br. J. Clin. Psychol. 2008, 47, 31–42. [Google Scholar] [CrossRef] [PubMed]
- Burke, K.; Muscara, F.; McCarthy, M.; Dimovski, A.; Hearps, S.; Anderson, V.; Walser, R. Adapting acceptance and commitment therapy for parents of children with life-threatening illness: Pilot study. Fam. Syst. Health 2014, 32, 122–127. [Google Scholar] [CrossRef] [PubMed]
- Thompson, R.W.; Arnkoff, D.B.; Glass, C.R. Conceptualizing mindfulness and acceptance as components of psychological resilience to trauma. Trauma Violence Abuse 2011, 12, 220–235. [Google Scholar] [CrossRef] [PubMed]
- Thieleman, K.; Cacciatore, J.; Hill, P.W. Traumatic bereavement and mindfulness: A preliminary study of mental health outcomes using the ATTEND Model. Clin. Soc. Work J. 2014, 42, 260–268. [Google Scholar] [CrossRef]
- Park, C.L. Making sense of the meaning literature: an integrative review of meaning making and its effects on adjustment to stressful life events. Psychol. Bull. 2010, 136, 257–301. [Google Scholar] [CrossRef] [PubMed]
- Keesee, N.J.; Currier, J.M.; Neimeyer, R.A. Predictors of grief following the death of one’s child: The contribution of finding meaning. J. Clin. Psychol. 2008, 64, 1145–1163. [Google Scholar] [CrossRef] [PubMed]
- Davis, C.G.; Nolen-Hoeksema, S.; Larson, J. Making sense of loss and benefiting from the experience: Two construals of meaning. J. Personal. Soc. Psychol. 1998, 75, 561–574. [Google Scholar] [CrossRef] [PubMed]
- Lichtenthal, W.G.; Neimeyer, R.A.; Currier, J.M.; Roberts, K.; Jordan, N. Cause of death and the quest for meaning after the loss of a child. Death Stud. 2013, 37, 311–342. [Google Scholar] [CrossRef] [PubMed]
- Nolen-Hoeksema, S. Ruminative coping and adjustment to bereavement. In Handbook of Bereavement Research: Consequences, Coping, and Care; Stroebe, M.S., Hansson, R.O., Stroebe, W., Schut, H., Eds.; American Psychological Association: Washington, DC, USA, 2001. [Google Scholar]
- Eisma, M.C.; Stroebe, M.S.; Schut, H.A.; Stroebe, W.; Boelen, P.A.; Van den Bout, J. Avoidance processes mediate the relationship between rumination and symptoms of complicated grief and depression following loss. J. Abnorm. Psychol. 2013, 122, 961–970. [Google Scholar] [CrossRef] [PubMed]
- Nolen-Hoeksema, S.; Wisco, B.E.; Lyubomirsky, S. Rethinking rumination. Perspect. Psychol. Sci. 2008, 3, 400–424. [Google Scholar] [CrossRef] [PubMed]
- Chan, C.L.; Chow, A.Y.; Ho, S.M.; Tsui, Y.K.; Tin, A.F.; Koo, B.W.; Koo, E.W. The experience of Chinese bereaved persons: A preliminary study of meaning making and continuing bonds. Death Stud. 2005, 29, 923–947. [Google Scholar] [CrossRef] [PubMed]
- Stroebe, M.; Stroebe, W.; Schut, H. Bereavement research: Methodological issues and ethical concerns. Palliat. Med. 2003, 17, 235–240. [Google Scholar] [CrossRef] [PubMed]
- Stroebe, M.S.; Stroebe, W. Who participates in bereavement research? A review and empirical study. Omega (Westport) 1990, 20, 1–29. [Google Scholar] [CrossRef]
- Crocker, J.C.; Beecham, E.; Kelly, P.; Dinsdale, A.P.; Hemsley, J.; Jones, L.; Bluebond-Langner, M. Inviting parents to take part in paediatric palliative care research: a mixed-methods examination of selection bias. Palliat. Med. 2015, 29, 231–240. [Google Scholar] [CrossRef] [PubMed]
- Bonnano, G.; Boerner, K.; Wortman, C.B. Trajectories of grieving. In Handbook of Bereavement Research and Practice: Advances in Theory and Intervention; Stroebe, M.S., Hansson, R.O., Schut, H., Stroebe, W., Eds.; American Psychological Association: Washington, DC, USA, 2008. [Google Scholar]
- Endo, K.; Yonemoto, N.; Yamada, M. Interventions for bereaved parents following a child’s death: A systematic review. Palliat. Med. 2015, 29, 590–604. [Google Scholar] [CrossRef] [PubMed]
- Neimeyer, R.A.; Currier, J.M. Bereavement interventions: Present status and future horizons. Grief Matters 2008, 11, 18–22. [Google Scholar]
- Currier, J.M.; Neimeyer, R.A.; Berman, J.S. The effectiveness of psychotherapeutic interventions for bereaved persons: A comprehensive quantitative review. Psychol. Bull. 2008, 134, 648–661. [Google Scholar] [CrossRef] [PubMed]
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jaaniste, T.; Coombs, S.; Donnelly, T.J.; Kelk, N.; Beston, D. Risk and Resilience Factors Related to Parental Bereavement Following the Death of a Child with a Life-Limiting Condition. Children 2017, 4, 96. https://doi.org/10.3390/children4110096
Jaaniste T, Coombs S, Donnelly TJ, Kelk N, Beston D. Risk and Resilience Factors Related to Parental Bereavement Following the Death of a Child with a Life-Limiting Condition. Children. 2017; 4(11):96. https://doi.org/10.3390/children4110096
Chicago/Turabian StyleJaaniste, Tiina, Sandra Coombs, Theresa J. Donnelly, Norm Kelk, and Danielle Beston. 2017. "Risk and Resilience Factors Related to Parental Bereavement Following the Death of a Child with a Life-Limiting Condition" Children 4, no. 11: 96. https://doi.org/10.3390/children4110096



