Sleep Quality and Chronotype Differences between Elite Athletes and Non-Athlete Controls
Abstract
:1. Introduction
2. Results
2.1. Participants
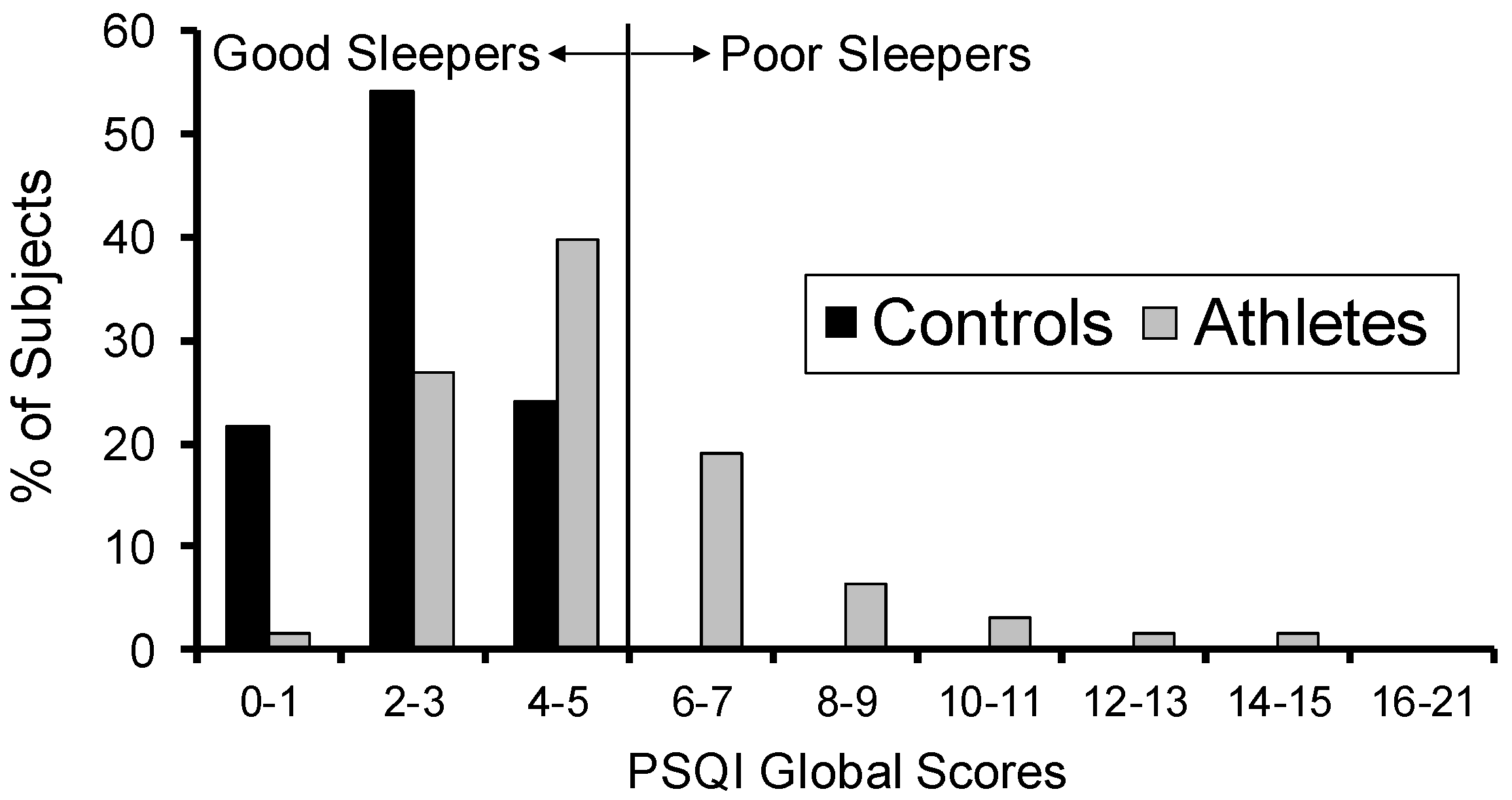
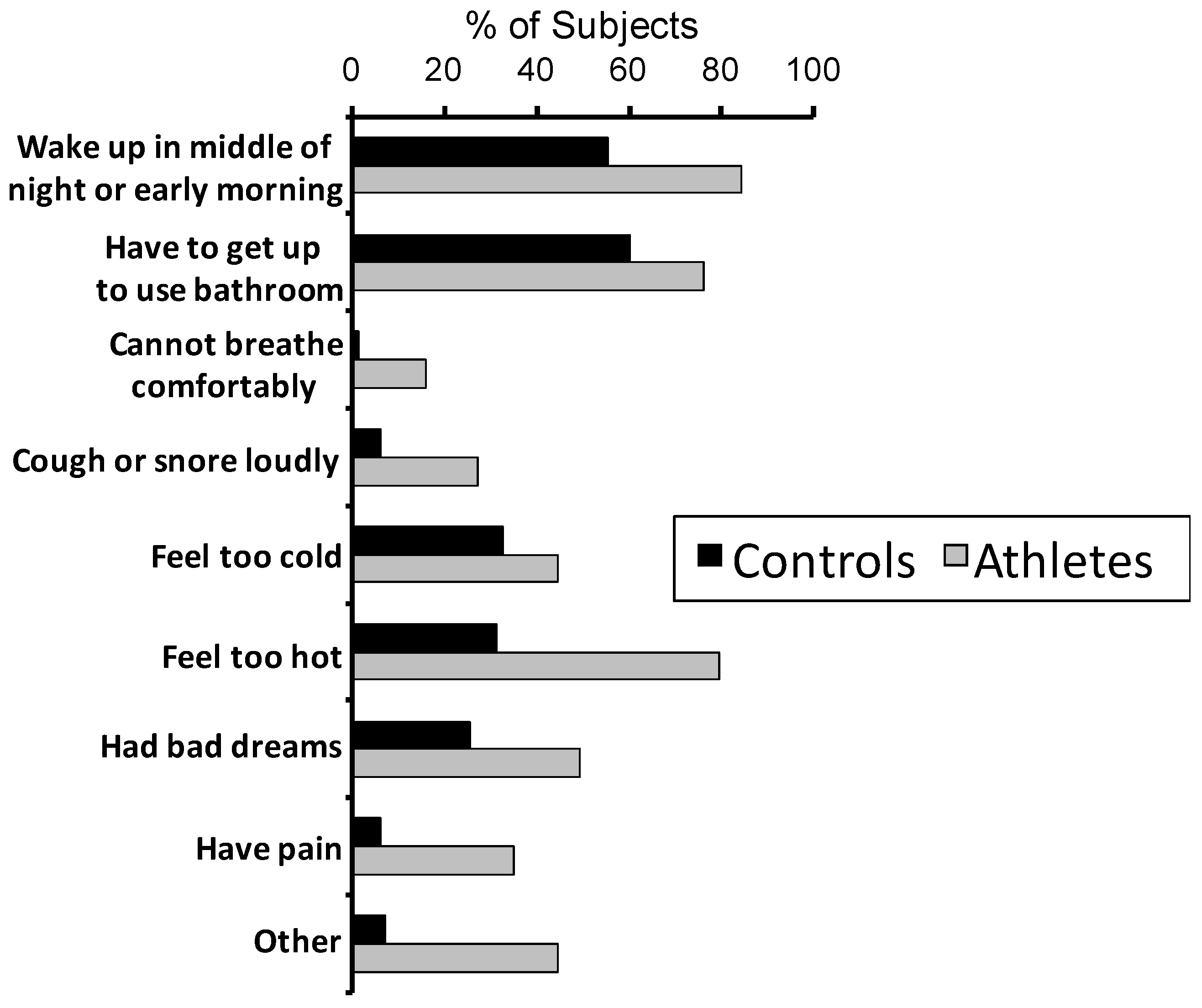
2.2. Sleep
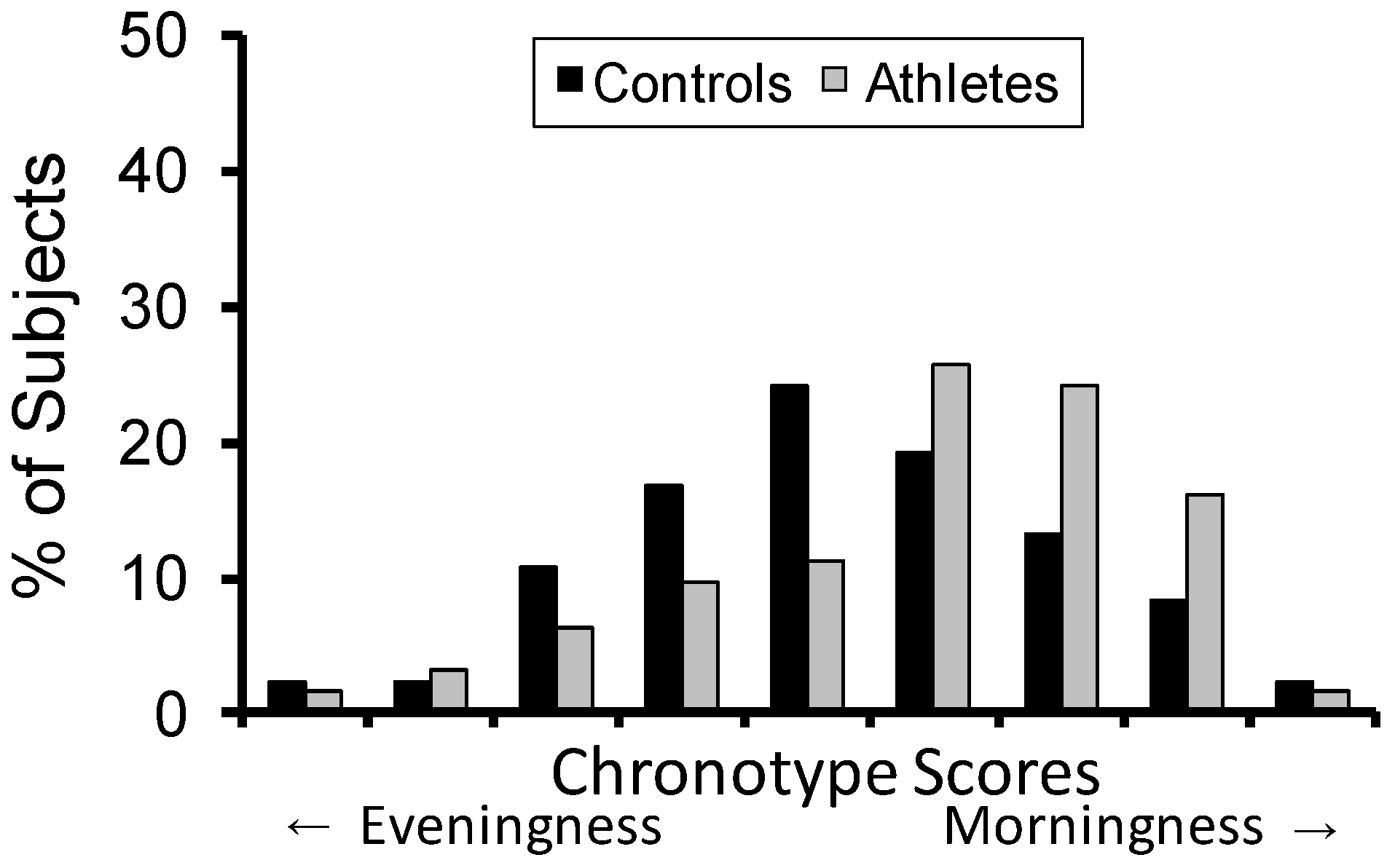
2.3. Chronotype
3. Discussion
3.1. Study Findings
3.2. Limitations
4. Materials and Methods
4.1. Participants
4.2. Questionnaires
4.3. Statistical Analyses
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| PSQI | Pittsburgh Sleep Quality Index |
| AMES | Athlete Morningness Eveningness Scale |
| CSM | Composite Scale of Morningness |
References
- Spiegel, K.; Leproult, R.; Van Cauter, E. Impact of sleep debt on metabolic and endocrine function. Lancet 1999, 354, 1435–1439. [Google Scholar] [CrossRef]
- McHill, A.; Wright, K. Role of sleep and circadian disruption on energy expenditure and in metabolic predisposition to human obesity and metabolic disease. Obes. Rev. 2017, 18, 15–24. [Google Scholar] [CrossRef] [PubMed]
- Knowles, O.E.; Drinkwater, E.J.; Urwin, C.S.; Lamon, S.; Aisbett, B. Inadequate sleep and muscle strength: Implications for resistance training. J. Sci. Med. Sport 2018, 21, 959–968. [Google Scholar] [CrossRef] [PubMed]
- Martin, B.J. Effect of sleep deprivation on tolerance of prolonged exercise. Eur. J. Appl. Physiol. Occup. Physiol. 1981, 47, 345–354. [Google Scholar] [CrossRef] [PubMed]
- Martin, B.J.; Gaddis, G.M. Exercise after sleep deprivation. Med. Sci. Sports Exerc. 1980, 13, 220–223. [Google Scholar] [CrossRef]
- Oliver, S.J.; Costa, R.J.; Laing, S.J.; Bilzon, J.L.; Walsh, N.P. One night of sleep deprivation decreases treadmill endurance performance. Eur. J. Appl. Physiol. 2009, 107, 155–161. [Google Scholar] [CrossRef] [PubMed]
- Dinges, D.F.; Pack, F.; Williams, K.; Gillen, K.A.; Powell, J.W.; Ott, G.E.; Aptowicz, C.; Pack, A.I. Cumulative sleepiness, mood disturbance, and psychomotor vigilance performance decrements during a week of sleep restricted to 4–5 hours per night. Sleep 1997, 20, 267–277. [Google Scholar] [PubMed]
- Van Dongen, H.P.A.; Maislin, G.; Mullington, J.M.; Dinges, D.F. The Cumulative Cost of Additional Wakefulness: Dose-Response Effects on Neurobehavioral Functions and Sleep Physiology From Chronic Sleep Restriction and Total Sleep Deprivation. Sleep 2003, 26, 117–126. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Samuels, C. Sleep, recovery, and performance: The new frontier in high-performance athletics. Phys. Med. Rehabil. Clin. N. Am. 2009, 20, 149–159. [Google Scholar] [CrossRef] [PubMed]
- Mah, C.D.; Mah, K.E.; Kezirian, E.J.; Dement, W.C. The effects of sleep extension on the athletic performance of collegiate basketball players. Sleep 2011, 34, 943–950. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, J.; Simon, R.D. Sleep extension improves serving accuracy: A study with college varsity tennis players. Physiol. Behav. 2015, 151, 541–544. [Google Scholar] [CrossRef] [PubMed]
- Swinbourne, R.; Miller, J.; Smart, D.; Dulson, D.K.; Gill, N. The Effects of Sleep Extension on Sleep, Performance, Immunity and Physical Stress in Rugby Players. Sports 2018, 6, 42. [Google Scholar] [CrossRef] [PubMed]
- Gupta, L.; Morgan, K.; Gilchrist, S. Does Elite Sport Degrade Sleep Quality? A Systematic Review. Sports Med. 2016, 47, 1317–1333. [Google Scholar] [CrossRef] [PubMed]
- Fullagar, H.H.; Skorski, S.; Duffield, R.; Hammes, D.; Coutts, A.J.; Meyer, T. Sleep and athletic performance: The effects of sleep loss on exercise performance, and physiological and cognitive responses to exercise. Sports Med. 2015, 45, 161–186. [Google Scholar] [CrossRef] [PubMed]
- Fietze, I.; Strauch, J.; Holzhausen, M.; Glos, M.; Theobald, C.; Lehnkering, H.; Penzel, T. Sleep quality in professional ballet dancers. Chronobiol. Int. 2009, 26, 1249–1262. [Google Scholar] [CrossRef] [PubMed]
- Swinbourne, R.; Gill, N.; Vaile, J.; Smart, D. Prevalence of poor sleep quality, sleepiness and obstructive sleep apnoea risk factors in athletes. Eur. J. Sport Sci. 2016, 16, 850–858. [Google Scholar] [CrossRef] [PubMed]
- Monma, T.; Ando, A.; Asanuma, T.; Yoshitake, Y.; Yoshida, G.; Miyazawa, T.; Ebine, N.; Takeda, S.; Omi, N.; Satoh, M.; et al. Sleep disorder risk factors among student athletes. Sleep Med. 2017, 44, 76–81. [Google Scholar] [CrossRef] [PubMed]
- Tuomilehto, H.; Vuorinen, V.-P.; Penttilä, E.; Kivimäki, M.; Vuorenmaa, M.; Venojärvi, M.; Airaksinen, O.; Pihlajamäki, J. Sleep of professional athletes: Underexploited potential to improve health and performance. J. Sports Sci. 2016, 35, 704–710. [Google Scholar] [CrossRef] [PubMed]
- Mollicone, D.J.; Van Dongen, H.P.; Dinges, D.F. Optimizing sleep/wake schedules in space: Sleep during chronic nocturnal sleep restriction with and without diurnal naps. Acta Astronaut. 2007, 60, 354–361. [Google Scholar] [CrossRef]
- Watson, N.F.; Badr, M.S.; Belenky, G.; Bliwise, D.L.; Buxton, O.M.; Buysse, D.; Dinges, D.F.; Gangwisch, J.; Grandner, M.A.; Kushida, C.; et al. Recommended amount of sleep for a healthy adult: A joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. J. Clin. Sleep Med. 2015, 11, 591–592. [Google Scholar] [PubMed]
- Leeder, J.; Glaister, M.; Pizzoferro, K.; Dawson, J.; Pedlar, C. Sleep duration and quality in elite athletes measured using wristwatch actigraphy. J. Sports Sci. 2012, 30, 541–545. [Google Scholar] [CrossRef] [PubMed]
- Lastella, M.; Roach, G.D.; Halson, S.L.; Sargent, C. Sleep/wake behaviours of elite athletes from individual and team sports. Eur. J. Sport Sci. 2015, 15, 94–100. [Google Scholar] [CrossRef] [PubMed]
- Sargent, C.; Halson, S.; Roach, G.D. Sleep or swim? Early-morning training severely restricts the amount of sleep obtained by elite swimmers. Eur. J. Sport Sci. 2014, 14 (Suppl. 1), S310–S315. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, S.; Bird, S.; Jacobson, G.; Driller, M. Sleep and stress hormone responses to training and competition in elite female athletes. Eur. J. Sport Sci. 2018, 18, 611–618. [Google Scholar] [CrossRef] [PubMed]
- American Academy of Sleep Medicine. International Classification of Sleep Disorders (ICSD-3), 3rd ed.; AASM Resource Library: Darien, IL, USA, 2014. [Google Scholar]
- Fowler, P.; Duffield, R.; Vaile, J. Effects of simulated domestic and international air travel on sleep, performance, and recovery for team sports. Scand. J. Med. Sci. Sports 2015, 25, 441–451. [Google Scholar] [CrossRef] [PubMed]
- Samuels, C.H. Jet lag and travel fatigue: A comprehensive management plan for sport medicine physicians and high-performance support teams. Clin. J. Sport Med. 2012, 22, 268–273. [Google Scholar] [CrossRef] [PubMed]
- Kerkhof, G.A. Inter-individual differences in the human circadian system: A review. Biol. Psychol. 1985, 20, 83–112. [Google Scholar] [CrossRef]
- Tankova, I.; Adan, A.; Buela-Casal, G. Circadian typology and individual differences. A review. Personal. Individ. Differ. 1994, 16, 671–684. [Google Scholar] [CrossRef]
- Facer-Childs, E.; Brandstaetter, R. The impact of circadian phenotype and time since awakening on diurnal performance in athletes. Curr. Biol. 2015, 25, 518–522. [Google Scholar] [CrossRef] [PubMed]
- Rosenthal, L.; Day, R.; Gerhardstein, R.; Meixner, R.; Roth, T.; Guido, P.; Fortier, J. Sleepiness/alertness among healthy evening and morning type individuals. Sleep Med. 2001, 2, 243–248. [Google Scholar] [CrossRef]
- Kunorozva, L.; Stephenson, K.J.; Rae, D.E.; Roden, L.C. Chronotype and PERIOD3 variable number tandem repeat polymorphism in individual sports athletes. Chronobiol. Int. 2012, 29, 1004–1010. [Google Scholar] [CrossRef] [PubMed]
- Silva, A.; Queiroz, S.S.; Winckler, C.; Vital, R.; Sousa, R.A.; Fagundes, V.; Tufik, S.; de Mello, M.T. Sleep quality evaluation, chronotype, sleepiness and anxiety of Paralympic Brazilian athletes: Beijing 2008 Paralympic Games. Br. J. Sports Med. 2012, 46, 150–154. [Google Scholar] [CrossRef] [PubMed]
- Lastella, M.; Roach, G.D.; Halson, S.L.; Sargent, C. The Chronotype of Elite Athletes. J. Hum. Kinet. 2016, 54, 219–225. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsunoda, K.; Hotta, K.; Mutsuzaki, H.; Tachibana, K.; Shimizu, Y. Sleep Status in Male Wheelchair Basketball Players on a Japanese National Team. J. Sleep Disord. Ther. 2015, 4, 210. [Google Scholar] [CrossRef]
- Driller, M.W.; Mah, C.D.; Halson, S.L. Development of the athlete sleep behavior questionnaire: A tool for identifying maladaptive sleep practices in elite athletes. Sleep Sci. 2018, 11, 37–44. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wittmann, M.; Dinich, J.; Merrow, M.; Roenneberg, T. Social jetlag: Misalignment of biological and social time. Chronobiol. Int. 2006, 23, 497–509. [Google Scholar] [CrossRef] [PubMed]
- Kerkhof, G.A.; Van Dongen, H.P. Morning-type and evening-type individuals differ in the phase position of their endogenous circadian oscillator. Neurosci. Lett. 1996, 218, 153–156. [Google Scholar] [CrossRef]
- Laborde, S.; Guillén, F.; Dosseville, F.; Allen, M.S. Chronotype, sport participation, and positive personality-trait-like individual differences. Chonobiol. Int. 2015, 32, 942–951. [Google Scholar]
- Dunican, I.C.; Martin, D.T.; Halson, S.L.; Reale, R.J.; Dawson, B.T.; Caldwell, J.A.; Jones, M.J.; Eastwood, P.R. The Effects of the Removal of Electronic Devices for 48 hours on Sleep in Elite Judo Athletes. J. Strength Cond. Res. 2017, 31, 2832–2839. [Google Scholar] [CrossRef] [PubMed]
- Unruh, M.L.; Redline, S.; An, M.W.; Buysse, D.J.; Nieto, F.J.; Yeh, J.L.; Newman, A.B. Subjective and objective sleep quality and aging in the sleep heart health study. J. Am. Geriat. Soc. 2008, 56, 1218–1227. [Google Scholar] [CrossRef] [PubMed]
- Tucker, A.M.; Dinges, D.F.; Van Dongen, H. Trait interindividual differences in the sleep physiology of healthy young adults. J. Sleep Res. 2007, 16, 170–180. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lewy, A.J.; Sack, R.L. The dim light melatonin onset as a marker for circadian phase position. Chronobiol. Int. 1989, 6, 93–102. [Google Scholar] [CrossRef] [PubMed]
- Laing, E.E.; Möller-Levet, C.S.; Poh, N.; Santhi, N.; Archer, S.N.; Dijk, D.J. Blood transcriptome based biomarkers for human circadian phase. eLife 2017, 6, e20214. [Google Scholar] [CrossRef] [PubMed]
- Satterfield, B.C.; Wisor, J.P.; Field, S.A.; Schmidt, M.A.; Van Dongen, H.P. TNFα G308A polymorphism is associated with resilience to sleep deprivation-induced psychomotor vigilance performance impairment in healthy young adults. Brain Behav. Immun. 2015, 47, 66–74. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Buysse, D.J.; Reynolds, C.F., III; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Horne, J.A.; Ostberg, O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int. J. Chronobiol. 1975, 4, 97–110. [Google Scholar]
- Postolache, T.T.; Hung, T.M.; Rosenthal, R.N.; Soriano, J.J.; Montes, F.; Stiller, J.W. Sports chronobiology consultation: From the lab to the arena. Clin. Sports Med. 2005, 24, 415–456. [Google Scholar] [CrossRef] [PubMed]
- Torsvall, L.; Åkerstedt, T. A diurnal type scale: Construction, consistency and validation in shift work. Scand. J. Work Environ. Health 1980, 6, 283–290. [Google Scholar] [CrossRef] [PubMed]
- Smith, C.S.; Reilly, C.; Midkiff, K. Evaluation of three circadian rhythm questionnaires with suggestions for an improved measure of morningness. J. Appl. Psychol. 1989, 74, 728. [Google Scholar] [CrossRef] [PubMed]
| Athletes | Controls | ||||
|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | t | df | p | |
| Bedtime (HH:MM ± min) | 22:56 ± 57 | 22:45 ± 50 | 1.15 | 144 | 0.25 |
| Sleep latency (min) | 21.5 ± 16.9 | 15.2 ± 12.9 | 2.47 | 92 | 0.015 * |
| Sleep duration (h) | 8.1 ± 1.0 | 8.0 ± 0.7 | 0.23 | 108 | 0.82 |
| Getting up time (HH:MM ± min) | 07:44 ± 67 | 07:32 ± 55 | 1.17 | 144 | 0.24 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bender, A.M.; Van Dongen, H.P.A.; Samuels, C.H. Sleep Quality and Chronotype Differences between Elite Athletes and Non-Athlete Controls. Clocks & Sleep 2019, 1, 3-12. https://doi.org/10.3390/clockssleep1010002
Bender AM, Van Dongen HPA, Samuels CH. Sleep Quality and Chronotype Differences between Elite Athletes and Non-Athlete Controls. Clocks & Sleep. 2019; 1(1):3-12. https://doi.org/10.3390/clockssleep1010002
Chicago/Turabian StyleBender, Amy M., Hans P. A. Van Dongen, and Charles H. Samuels. 2019. "Sleep Quality and Chronotype Differences between Elite Athletes and Non-Athlete Controls" Clocks & Sleep 1, no. 1: 3-12. https://doi.org/10.3390/clockssleep1010002





