A Composite and Wearable Sensor Kit for Location-Aware Healthcare Monitoring and Real-Time Trauma Scoring for Survival Prediction
Abstract
:1. Introduction
1.1. Literature Review
1.1.1. The Physiological Parameters for Health Status Determination
1.1.2. Injury Severity and Trauma Scoring for Prediction of Survival Based on Physiological Parameters
- (1)
- Physiologic: RTS, APACHE, Emergency Trauma Score
- (2)
- Anatomical: AIS, ISS, NISS
- (3)
- Combined: TRISS, A Severity Characterization of Trauma (ASCOT), the International Classification of Diseases Injury Severity Score (ICISS)
1.1.3. Integration of Electronic Health Records with Injury and Trauma scores and Location Awareness
1.2. Problems and Challenges
1.2.1. Obtaining Vital Signs from the Composite Sensor Kit
1.2.2. Integrating Trauma and Injury Scores with Electronic Health Records.
1.2.3. Location Awareness to Trigger a Real-Time Incident Response
2. Materials and Methods
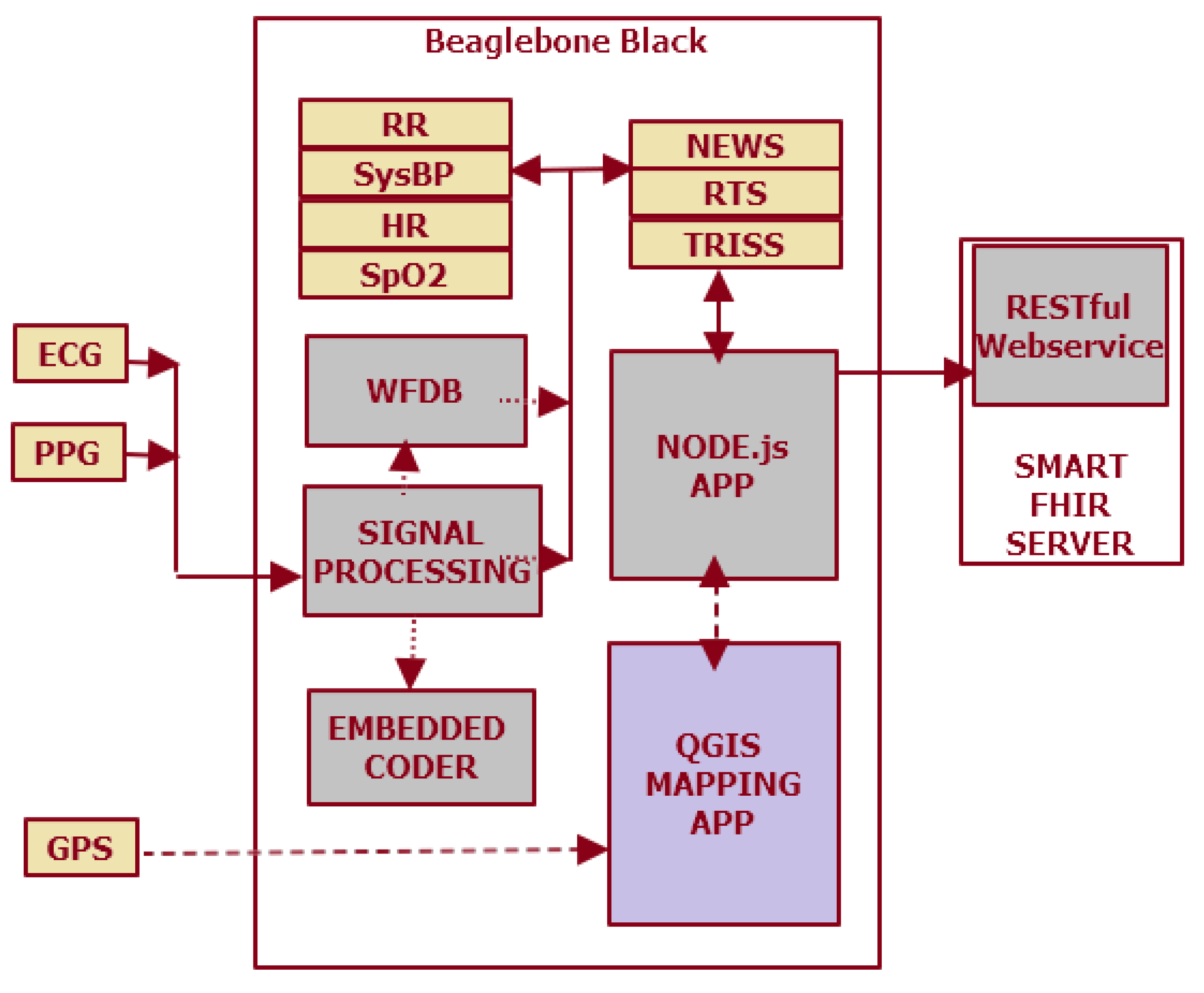
2.1. Composite Sensor Kit for Real-Time Multiparameter Physiological Data Acquisition
[z,p,k] = cheby2(n,Rs,Ws); % Filter Design
[sosbp,gbp] = zp2sos(z,p,k);
filtered_signal = filtfilt(sosbp, gbp, ecgsig); % Filter Signal
%Source: matlabcentral/answers/364788-ecg-signal-artifact-removing
- (1)
- ECG Sensor module
- (2)
- PPG (SpO2) sensor module
- (3)
- GPS module
- (4)
- Respiratory rate and blood pressure calculations
- Read the samples from the ECG and PPG sensor using the Adafruit GPIO library for BBB with a sampling frequency of 1024 Hz. At least a 3-millisecond interval should be present between the two samples.
- Use the ‘wrsamp -F 360 -G 1000 -i’ command from WFDB to convert these samples to a WFDB-compatible record where ‘1000’ is the gain. The WFDB record conversion sampling frequency is 360 Hz, which is different from the data acquisition sampling frequency of 1024 Hz. ECG strips are analyzed in batches of 10 s intervals.
- Use the ‘gqrs -r ecg_samples_file -m 1’ command to obtain the QRS complexes from the samples. The threshold set is set to ‘1 mV’, and a qrs annotation file is generated.
- Use the ‘rdann -a qrs -r ecg_samples_file’ command, which uses the ‘qrs’ annotation file to find the R-peaks.
- Find the number of samples between the R-peak and the next available PPG peak, and calculate the time corresponding to the sampling interval, which would give the PTT value that is used to determine the systolic BP. At 360 Hz, the WFDB sampling frequency interval between two consecutive samples would be approximately 2.75 milliseconds.
- Use ‘edr -r edr_samples_file -i qrs_file -f 0 -t 0.16:0’ to generate the EDR samples for a value of ‘0.16’, corresponding to 10 s time frames and corresponding to the ‘qrs’ annotation file. This would give the average respiratory rate over a 10 s interval.
2.2. Physionet MIMIC II Database for Statistical Analysis
2.3. Trauma and Injury Severity Scoring for the Probability of Survival Prediction
- RR (breaths per minute) score
- PPG (%) score
- Any Supplemental Oxygen score (Yes/No)
- Temperature in °C (°F) scale
- Systolic BP score
- HR (beats per minute) score
- AVPU score
- Best Motor Response (values: None to maximum 6)
- 6—Obeys command
- 5—Localizes pain
- 4—Normal withdrawal (flexion)
- 3—Abnormal withdrawal (flexion): decorticate
- 2—Abnormal withdrawal (extension): de-cerebrate
- None (flaccid)
- Best Verbal Response (values: None to maximum 5)
- 5—Oriented
- 4—Confused conversation
- 3—Inappropriate words
- 2—Incomprehensible sounds
- None
- Eye Opening (values: None to maximum 4)
- 4—Spontaneous
- 3—To speech
- 2—To pain
- None
2.4. Location Awareness Additions to the Wearable Sensor Kit Using the GIS Application and the GPS Module
- (1)
- To match geographical maps with GPS coordinates;
- (2)
- To generate a heatmap of the roads traveled, based on GPS track recordings;
- (3)
- To download road map data from an online repository of shapefiles and transform it into a network of roads;
- (4)
- To store the road network in a database;
- (5)
- To generate own records of journeys using a GPS tracking device log of the route traversed;
- (6)
- To implement a map-matching algorithm to match GPS track recordings to an existing road network using shapefiles.
- (1)
- An accurate GPS track recording of the journey containing a log of GPS coordinates which would identify the roads that were followed on the journey.
- (2)
- An accurate database of road maps mapped to global geographical coordinates.
- (3)
- A suitable algorithm to match the GPS coordinates against the road map database.
2.5. FHIR Application for the Composite Sensor Kit
3. Results and Discussion
3.1. Workflow from Data Acquisition to Location Tracking
3.1.1. Signal Processing of Physiological Parameters
wtrec = zeros(size(wtrans));
wtrec(4:5,:) = wtrans (4:5,:);
y = imodwt(wtrec,’sym4’);
y = abs(y).^2;
[qrspeaks, locs] = findpeaks(y, tm,’MinPeakHeight’, 0.1, ‘MinPeakDistance’,0.150);
Hd = designfilt(‘lowpassfir’,’FilterOrder’,20,’CutoffFrequency’,150,
‘DesignMethod’,’window’,’Window’,{@kaiser,4},’SampleRate’,1024);
y1 = filter(Hd,ecg033array(:,2));
sgf = sgolayfilt(ecg033array(:,2),3,51);
y1 = filtfilt(Hd,ecg033array(:,2));
3.1.2. Correlation and Regression of Trauma Scores and their Predictors
3.1.3. Shortest Route Calculation Using GNSS/GIS Algorithms
4. Conclusions
Funding
Acknowledgments
Conflicts of Interest
References
- Nguyen, H.H.; Mirza, F.; Naeem, M.A.; Nguyen, M. (2017) A review on IoT healthcare monitoring applications and a vision for transforming sensor data into real-time clinical feedback. In Proceedings of the 2017 IEEE 21st International Conference on Computer Supported Cooperative Work in Design (CSCWD 2017), Wellington, New Zealand, 26–28 April 2017. [Google Scholar]
- Tu, H.T.; Chen, Z.; Swift, C.; Churilov, L.; Guo, R.; Liu, X.; Yan, B. Smartphone electrographic monitoring for atrial fibrillation in acute ischemic stroke and transient ischemic attack. Int. J. Stroke 2017, 12, 786–789. [Google Scholar] [CrossRef] [PubMed]
- Richer, R.; Blank, P.; Schuldhaus, D.; Eskofier, B.M. Real-Time ECG and EMG Analysis for Biking Using Android-Based Mobile Devices. In Proceedings of the 2014 11th International Conference on Wearable and Implantable Body Sensor Networks, Zurich, Switzerland, 16–19 June 2014; pp. 104–108. [Google Scholar] [CrossRef]
- Holcomb, J.B.; Salinas, J.; McManus, J.M.; Miller, C.C.; Cooke, W.H.; Convertino, V.A. Manual vital signs reliably predict need for life-saving interventions in trauma patients. J. Trauma 2005, 59, 821–828; discussion 828–829. [Google Scholar] [CrossRef] [PubMed]
- Charlton, P.; Birrenkott, D.A.; Bonnici, T.; Pimentel, M.A.F.; Johnson, A.E.W.; Alastruey, J.; Tarassenko, L.; Watkinson, P.J.; Beale, R.; Clifton, D.A. Breathing Rate Estimation from the Electrocardiogram and Photoplethysmogram: A Review. IEEE Rev. Biomed. Eng. 2018, 11, 2–20. [Google Scholar] [CrossRef] [PubMed]
- Sbiti-Rohr, D.; Kutz, A.; Christ-Crain, M.; Thomann, R.; Zimmerli, W.; Hoess, C.; Henzen, C.; Mueller, B.; Schuetz, P. The National Early Warning Score (NEWS) for outcome prediction in emergency department patients with community-acquired pneumonia: results from a 6-year prospective cohort study. BMJ Open 2016, 6, e011021. [Google Scholar] [CrossRef] [PubMed]
- Long, W.B.; Bachulis, B.L.; Hynes, G.D. Accuracy and relationship of mechanisms of injury, trauma score, and injury severity score in identifying major trauma. Am. J. Surg. 1986, 151, 581–584. [Google Scholar] [CrossRef]
- Silva, I.; Moody, G. An Open-source Toolbox for Analysing and Processing PhysioNet Databases in MATLAB and Octave. J. Open Res. Softw. 2014, 2, e27. [Google Scholar] [CrossRef] [PubMed]
- Goldberger, A.L.; Amaral, L.A.N.; Glass, L.; Hausdorff, J.M.; Ivanov, P.C.; Mark, R.G.; Mietus, J.E.; Moody, G.B.; Peng, C.-K.; Stanley, H.E. PhysioBank, PhysioToolkit, and PhysioNet. Compon. New Res. Resour. Complex Physiol. Signals 2000, 101, e215–e220. [Google Scholar]
- Aminiahidashti, H.; Bozorgi, F.; Montazer, S.H.; Baboli, M.; Firouzian, A. Comparison of APACHE II and SAPS II Scoring Systems in Prediction of Critically Ill Patients’ Outcome. Emergency 2017, 5, e4. [Google Scholar] [PubMed]
- Linn, S. The injury severity score—Importance and uses. Ann. Epidemiol. 1995, 5, 440–446. [Google Scholar] [CrossRef]
- Skaga, N.O.; Eken, T.; Søvik, S. Validating performance of TRISS, TARN and NORMIT survival prediction models in a Norwegian trauma population. Acta Anaesthesiol. Scand. 2018, 62, 253–266. [Google Scholar] [CrossRef] [PubMed]
- Penn-Barwell, J.G.; Bishop, J.R.B.; Midwinter, M.J. Refining the Trauma and Injury Severity Score (TRISS) to Measure the Performance of the UK Combat Casualty Care System. Mil. Med. 2018, 183, e442–e447. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mandel, J.C.; Kreda, D.A.; Mandl, K.D.; Kohane, I.S.; Ramoni, R.B. SMART on FHIR: a standards-based, interoperable apps platform for electronic health records. J. Am. Med. Inform. Assoc. 2016, 23, 899–908. [Google Scholar] [CrossRef] [PubMed]
- Lockwood, C.; Conroy-Hiller, T.; Page, T. Vital signs. JBI Libr. Syst. Rev. 2004, 2, 1–38. [Google Scholar] [PubMed]
- Hart, J. Association between heart rate variability and manual pulse rate. J. Can. Chiropract. Assoc. 2013, 57, 243–250. [Google Scholar]
- Healey, J.A.; Picard, R.W. Detecting stress during real-world driving tasks using physiological sensors. IEEE Trans. Intell. Transport. Syst. 2005, 6, 156–166. [Google Scholar] [CrossRef]
- Staessen, J.; O’Brien, E.; Thijs, L.; Fagard, R. Modern approaches to blood pressure measurement. Occup. Environ. Med. 2000, 57, 510–520. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mower, W.R.; Myers, G.; Nicklin, E.L.; Kearin, K.T.; Baraff, L.J.; Sachs, C. Pulse oximetry as a fifth vital sign in emergency geriatric assessment. Acad. Emerg. Med. 1998, 5, 858–865. [Google Scholar] [CrossRef] [PubMed]
- Garthe, E.; States, J.D.; Mango, N.K. Abbreviated injury scale unification: The case for a unified injury system for global use. J. Trauma 1999, 47, 309–323. [Google Scholar] [CrossRef] [PubMed]
- Schluter, P.J. The Trauma and Injury Severity Score (TRISS) revised. Injury 2011, 42, 90–96. [Google Scholar] [CrossRef] [PubMed]
- Alam, N.; Hobbelink, E.L.; van Tienhoven, A.J.; van de Ven, P.M.; Jansma, E.P.; Nanayakkara, P.W.B. The impact of the use of the Early Warning Score (EWS) on patient outcomes: A systematic review. Resuscitation 2014, 85, 587–594. [Google Scholar] [CrossRef] [PubMed]
- Riordan, W.P., Jr.; Norris, P.R.; Jenkins, J.M.; Morris, J.A., Jr. Early Loss of Heart Rate Complexity Predicts Mortality Regardless of Mechanism, Anatomic Location, or Severity of Injury in 2178 Trauma Patients. J. Surg. Res. 2009, 156, 283–289. [Google Scholar] [CrossRef] [PubMed]
- Cooke, W.H.; Salinas, J.; McManus, J.G.; Ryan, K.L.; Rickards, C.A.; Holcomb, J.B.; Convertino, V.A. Heart period variability in trauma patients may predict mortality and allow remote triage. Aviat. Space Environ. Med. 2006, 77, 1107–1112. [Google Scholar] [PubMed]
- Domingues, C.D.A.; Coimbra, R.; Poggetti, R.S.; Nogueira, L.D.S.; de Sousa, R.M.C. New Trauma and Injury Severity Score (TRISS) adjustments for survival prediction. World J. Emerg. Surg. 2018, 13, 12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barnard, E.B.G.; Hunt, P.A.F.; Lewis, P.E.H.; Smith, J.E. The outcome of patients in traumatic cardiac arrest presenting to deployed military medical treatment facilities: Data from the UK Joint Theatre Trauma Registry. J. R. Army Med. Corps 2017, 164, 150–154. [Google Scholar] [CrossRef] [PubMed]
- Mackenzie, R.; Sutcliffe, R. Pre-hospital Care: The Trapped Patient. J. R. Army Med. Corps 2000, 146, 39–46. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Richesson, R.L.; Andrews, J.E.; Krischer, J.P. Use of SNOMED CT to Represent Clinical Research Data: A Semantic Characterization of Data Items on Case Report Forms in Vasculitis Research. J. Am. Med. Inform. Assoc. JAMIA 2006, 13, 536–546. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fingerhut, L.A.; Warner, M. The ICD-10 injury mortality diagnosis matrix. Injury Prev. 2006, 12, 24–29. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- ICD-NCHS. ICD Injury Matrices ICD-10. 2006. Available online: https://www.cdc.gov/nchs/injury/injury_matrices.htm (accessed on 25 May 2018).
- ICD–9–CM. Recommended Framework for Presenting Injury Mortality Data. MMWR 46 (RR-14), 1997. Available online: https://www.cdc.gov/mmwr/preview/mmwrhtml/00049162.htm (accessed on 25 May 2018).
- Walinjkar, A.; Woods, J. Personalized wearable systems for real-time ECG classification and healthcare interoperability: Real-time ECG classification and FHIR interoperability. In Proceedings of the 2017 Internet Technologies and Applications (ITA), Wrexham, UK, 12–15 September 2017. [Google Scholar]
- Lee, S.; Tewolde, G.; Kwon, J. Design and implementation of vehicle tracking system using GPS/GSM/GPRS technology and smartphone application. In Proceedings of the 2014 IEEE World Forum on Internet of Things (WF-IoT), Seoul, Korea, 6–8 March 2014. [Google Scholar]
- Heartisans. Measure Your Blood Pressure. Anywhere. Anytime. 2017. Available online: https://www.heartisans.com/ (accessed on 10 September 2018).
- Rodríguez, R.; Mexicano, A.; Bila, J.; Cervantes, S.; Ponce, R. Feature Extraction of Electrocardiogram Signals by Applying Adaptive Threshold and Principal Component Analysis. J. Appl. Res. Technol. 2015, 13, 261–269. [Google Scholar] [CrossRef]
- Jochen, A. Key Concepts and Techniques in GIS; SAGE Publications: London, UK, 2007. [Google Scholar]
- Taouli, S.A.; Bereksi-Reguig, F. Noise and baseline wandering suppression of ECG signals by morphological filter. J. Med. Eng. Technol. 2010, 34, 87–96. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Ayub, S. Estimation of Blood Pressure by Using Electrocardiogram (ECG) and Photo-Plethysmogram (PPG). In Proceedings of the 2015 Fifth International Conference on Communication Systems and Network Technologies, Gwalior, India, 4–6 April 2015. [Google Scholar]
- George, B.; Moody, R.G.M.; Zoccola, A.; Mantero, S. Derivation of Respiratory Signals from Multi-lead ECGs. Comput. Cardiol. 1985, 12, 113–116. [Google Scholar]
- Ahmad, S.; Chen, S.; Soueidan, K.; Batkin, I.; Bolic, M.; Dajani, H.; Groza, V. Electrocardiogram-Assisted Blood Pressure Estimation. IEEE Trans. Biomed. Eng. 2012, 59, 608–618. [Google Scholar] [CrossRef] [PubMed]
- Dinh, A.; Luu, L.; Cao, T. Blood Pressure Measurement Using Finger ECG and Photoplethysmogram for IoT; Springer: Singapore, 2018. [Google Scholar]
- Goldberger, A.L.; Amaral, L.A.N.; Glass, L.; Hausdorff, J.M.; Ivanov, P.C.; Mark, R.G.; Mietus, J.E.; Moody, G.B.; Peng, C.K.; Stanley, H.E. PhysioBank, PhysioToolkit, and PhysioNet: Components of a new research resource for complex physiologic signals. Circulation 2000, 101, E215–E220. [Google Scholar] [CrossRef] [PubMed]
- Scott, D.J.; Lee, J.; Silva, I.; Park, S.; Moody, G.B.; Celi, L.A.; Mark, R.G. Accessing the public MIMIC-II intensive care relational database for clinical research. BMC Med. Inform. Decis. Mak. 2013, 13, 9. [Google Scholar] [CrossRef] [PubMed]
- Da Poian, Q.G.; Schwabedal, J. PhysioNet-Cardiovascular-Signal-Toolbox, Version 1.0.0; Zenodo: Geneva, Switzerland, 2018. [Google Scholar]
- Saeed, M.; Villarroel, M.; Reisner, A.T.; Clifford, G.; Lehman, L.-W.; Moody, G.; Heldt, T.; Kyaw, T.H.; Moody, B.; Mark, R.G. Multiparameter Intelligent Monitoring in Intensive Care II (MIMIC-II): A public-access intensive care unit database. Crit. Care Med. 2011, 39, 952–960. [Google Scholar] [CrossRef] [PubMed]
- Pirracchio, R. Mortality Prediction in the ICU Based on MIMIC-II Results from the Super ICU Learner Algorithm (SICULA) Project. Secondary Analysis of Electronic Health Records; Springer International Publishing: Cham, Switzerland, 2016; pp. 295–313. [Google Scholar]
- Domingues, C.D.A.; Nogueira, L.D.S.; Settervall, C.H.C.; Sousa, R.M.C.D. Performance of Trauma and Injury Severity Score(TRISS) adjustments: An integrative review. Revista da Escola de Enfermagem da USP 2015, 49, 138–146. [Google Scholar] [CrossRef] [PubMed]
- Gleason, S.; Gebre-Egziabher, D. GNSS Applications and Methods; Artech House: Norwood, MA, USA, 2009. [Google Scholar]
- GPS.js. 2018. Available online: https://www.npmjs.com/package/gps (accessed on 28 July 2018).
- RTKLIB. Wiki Page. Last Modified on 4 March 2018. Available online: http://wiki.openstreetmap.org/w/index.php?title=RTKLIB&oldid=1580925 (accessed on 5 June 2018).
- RTKLIB-Compatible GPS Devices. Wiki Page. Last Modified on 20 March 2018. Available online: http://wiki.openstreetmap.org/w/index.php?title=RTKLIB-compatible_GPS_devices&oldid=1591413 (accessed on 5 June 2018).
- Download OpenStreetMap Data for This Region: Essex. 2018. Available online: http://download.geofabrik.de/europe/great-britain/england/essex.html (accessed on 18 June 2018).
- OpenStreetMap Main Page. Last Modified 10 July 2014. Available online: https://wiki.openstreetmap.org/wiki/Main_Page (accessed on 10 September 2018).
- Assessment Scales. Wiki Page. Last Modified on 27 December 2012. Available online: http://wiki.hl7.org/index.php?title=Assessment_Scales (accessed on 21 June 2018).
- SNOWMED-International. SNOMED International SNOMED CT Browser. 2018. Available online: http://browser.ihtsdotools.org/ (accessed on 10 September 2018).





| NEWS | RTS | TRISS | |
|---|---|---|---|
| Parameters used | Respiratory Rate Oxygen Saturations Supplemental Oxygen (Y/N) Temperature Systolic Blood Pressure Heart Rate AVPU Score | Glasgow Coma Scale (GCS): Eye + Verbal + Motor response score Systolic BP Respiratory Rate | Uses RTS and ISS ISS: (Anatomical injury scores for Head + Face + Chest + Abdomen injury) Severity of injury |
| Interpretation | NEWS 1–4: escalation of clinical care NEWS of 5–6 or a RED score: escalation to critical care NEWS ≥ 7: escalation to critical care with maximum competency | GCS of <15 warrants close attention GCS of <8 is of clinical concern RTS <= 2: critical care situation with less than 15% chance of survival | ISS of 75 and higher is critical with less chance of survival. Ps (blunt/penetrating) values (0 to 1): Values less than 0.15: less chance of survival |
| // Create a FHIR Observation object. |
| Observation observ= new Observation (); |
| // Assign a randomly generated Universal ID (UUID). |
| observ.setId(uuid) |
| // Set the Observation code according to a Coding System |
| // Coding System refers to RTS trauma score in SNOMED CT |
| observ.getCode() |
| .addCoding() |
| .setSystem(“http://snomed.info/sct”) |
| .setCode(“273885003”) |
| .setDisplay(“RTS Trauma Assessment”) |
| observ.setValue( |
| new QuantityDt() |
| .setValue(3) |
| // Set the Date and Time stamp for the observation |
| observ.setIssued( |
| new InstantDt(“2017-05-05T15:30:10+01:00”)) |
| // The Observation upload request above generated the following |
| // response in XML or JSON format after observation is logged to |
| // FHIR Servers. |
| <Bundle xmlns=“http://hl7.org/fhir”> |
| <id value=“ddde128-e4e2-481ee-9acb3-c5eebc2ec5e0”/> |
| <type value=“transaction-response”/> |
| <entry> |
| <response> |
| <status value=“201 Created”/> |
| <location value=“Observation/96728/_history/1”/> |
| <etag value=“1”/> |
| <lastModified value=“2017-05-05T15:30:10+01:00”/> |
| </response> |
| </entry> |
| </Bundle> |
| Scores and Correlation Measure | PsBlunt | NEWS | RTS | |
|---|---|---|---|---|
| PsBlunt | Pearson Correlation | 1 | 0.7950 ** | 0.0630 ** |
| Sig. (2-tailed) | 0.000 | 0.000 | ||
| N | 368721 | 368721 | 368721 | |
| NEWS | Pearson Correlation | 0.795 ** | 1 | −0.252 ** |
| Sig. (2-tailed) | 0.000 | 0.000 | ||
| N | 368721 | 368721 | 368721 | |
| RTS | Pearson Correlation | 0.063 ** | −0.252 ** | 1 |
| Sig. (2-tailed) | 0.000 | 0.000 | ||
| N | 368721 | 368721 | 368721 | |
| Model | R | R Square | Adjusted R Square | Std. Error of the Estimate |
|---|---|---|---|---|
| 1 | 0.968 a | 0.937 | 0.937 | 0.033065132300000 |
© 2018 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Walinjkar, A. A Composite and Wearable Sensor Kit for Location-Aware Healthcare Monitoring and Real-Time Trauma Scoring for Survival Prediction. Appl. Syst. Innov. 2018, 1, 35. https://doi.org/10.3390/asi1030035
Walinjkar A. A Composite and Wearable Sensor Kit for Location-Aware Healthcare Monitoring and Real-Time Trauma Scoring for Survival Prediction. Applied System Innovation. 2018; 1(3):35. https://doi.org/10.3390/asi1030035
Chicago/Turabian StyleWalinjkar, Amit. 2018. "A Composite and Wearable Sensor Kit for Location-Aware Healthcare Monitoring and Real-Time Trauma Scoring for Survival Prediction" Applied System Innovation 1, no. 3: 35. https://doi.org/10.3390/asi1030035





