Effect of the Time of Salivary Contamination during Light Curing on Degree of Conversion and Microhardness of a Restorative Composite Resin
Abstract
:1. Introduction
2. Materials and Methods
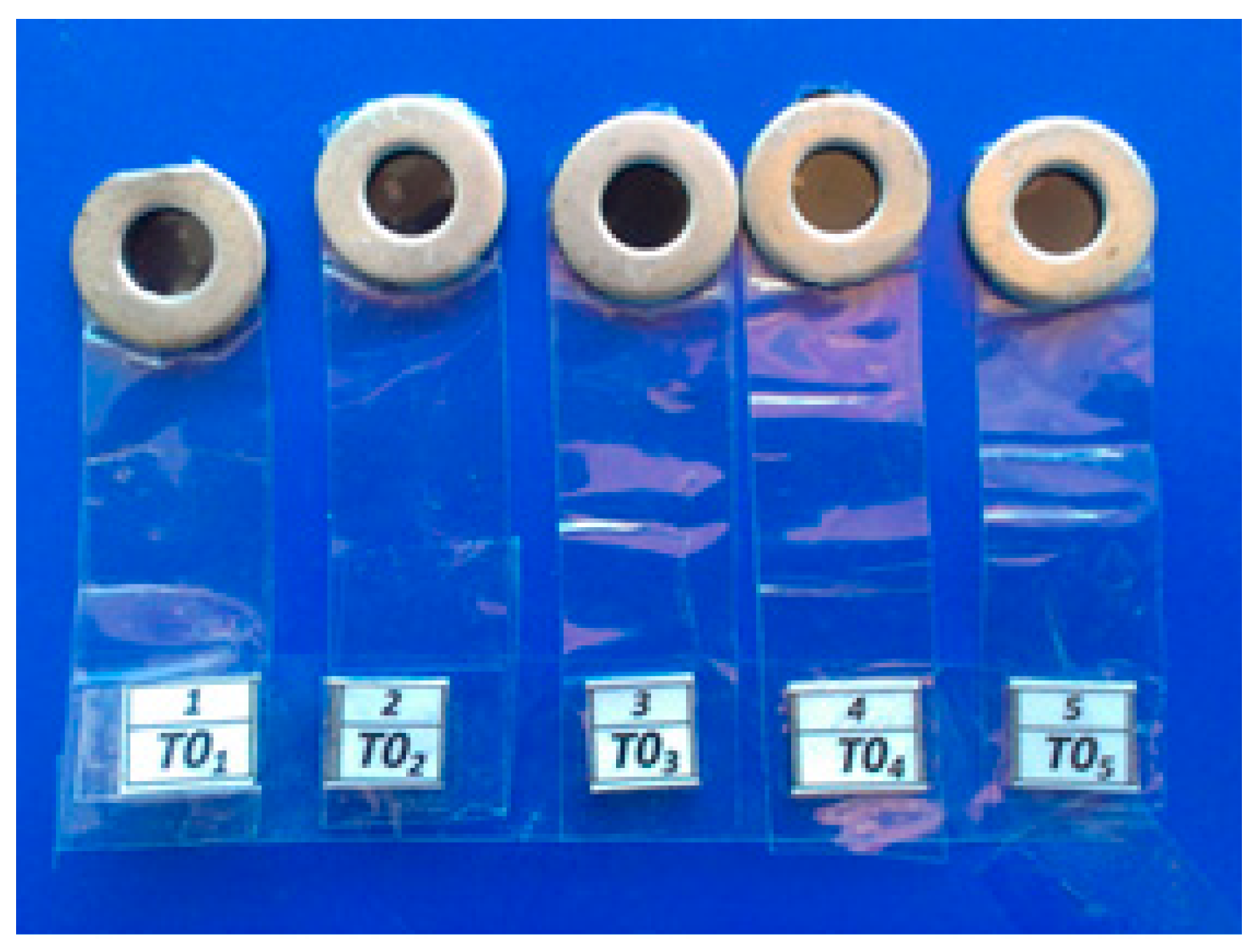
2.1. Sample Preparation
- T0: Samples were contaminated with human saliva before the start of light curing, and then light cured for 40 s (negative control).
- T2: Samples were contaminated with human saliva 2 s after the start of light curing.
- T5: Samples were contaminated with human saliva 5 s after the start of light curing.
- T10: Samples were contaminated with human saliva 10 s after the start of light curing.
- T15: Samples were contaminated with human saliva 15 s after the start of light curing.
- T20: Samples were contaminated with human saliva 20 s after the start of light curing.
- T30: Samples were contaminated with human saliva 30 s after the start of light curing.
- T40: Samples were light cured for 40 s, before being contaminated with human saliva (positive control).
2.2. Microhardness and Degree of Conversion Measurements
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Son, S.; Roh, H.-M.; Hur, B.; Kwon, Y.-H.; Park, J.-K. The effect of resin thickness on polymerization characteristics of silorane-based composite resin. Restor. Dent. Endod. 2014, 39, 310–318. [Google Scholar] [CrossRef] [PubMed]
- Silva, E.M.D.; Almeida, G.S.; Poskus, L.T.; Guimarães, J.G.A. Relationship between the degree of conversion, solubility and salivary sorption of a hybrid and a nanofilled resin composite. J. Appl. Oral Sci. 2008, 16, 161–166. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yokesh, C.A.; Hemalatha, P.; Muthalagu, M.; Justin, M.R. Comparative evaluation of the depth of cure and degree of conversion of two bulk fill flowable composites. J. Clin. Diagn. Res. 2017, 11, ZC86–ZC89. [Google Scholar] [CrossRef] [PubMed]
- Tarle, Z.; Meniga, A.; Šutalo, J. Correlation between degree of conversion and light transmission through resin composite samples. Acta Stomatol. Croat. 1995, 29, 9–14. [Google Scholar]
- Camargo, E.J.D.; Moreschi, E.; Baseggio, W.; Cury, J.A.; Pascotto, R.C. Composite depth of cure using four polymerization techniques. J. Appl. Oral Sci. 2009, 17, 446–450. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morgan, L.F.; Teixeira, K.I.; Vasconcellos, W.A.; Albuquerque, R.C.; Cortés, M.E. Correlation between the cytotoxicity of self-etching resin cements and the degree of conversion. Indian J. Dent. Res. 2015, 26, 284. [Google Scholar] [PubMed]
- Park, J.-K.; Kim, T.-H.; Ko, C.-C.; Garcia-Godoy, F.; Kim, H.-I.; Kwon, Y.H. Effect of staining solutions on discoloration of resin nanocomposites. Am. J. Dent. 2010, 23, 39. [Google Scholar] [PubMed]
- Ciccone-Nogueira, J.C.; Borsatto, M.C.; Souza-Zaron, W.C.D.; Ramos, R.P.; Palma-Dibb, R.G. Microhardness of composite resins at different depths varying the post-irradiation time. J. Appl. Oral Sci. 2007, 15, 305–309. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miletic, V. Dental Composite Materials for Direct Restorations; Springer: New York, NY, USA, 2017. [Google Scholar]
- Ramanitya, A.; Indrani, D.; Herda, E. Under-surface hardness of light-cured nanofilled resin composites of different shades. J. Phys. Conf. Ser. 2017, 884, 012108. [Google Scholar] [CrossRef] [Green Version]
- Say, E.; Civelek, A.; Nobecourt, A.; Ersoy, M.; Guleryuz, C. Wear and microhardness of different resin composite materials. Oper. Dent. 2003, 28, 628–634. [Google Scholar] [PubMed]
- Price, R.; Felix, C.; Andreou, P. Evaluation of a dual peak third generation LED curing light. Compend. Contin. Educ. Dent. 2005, 26, 331–332, 334, 336–338 passim; quiz 348. [Google Scholar] [PubMed]
- Abed, Y.; Sabry, H.; Alrobeigy, N. Degree of conversion and surface hardness of bulk-fill composite versus incremental-fill composite. Tanta Dent. J. 2015, 12, 71–80. [Google Scholar] [CrossRef]
- Knobloch, L.; Kerby, R.; Clelland, N.; Lee, J. Hardness and degree of conversion of posterior packable composites. Oper. Dent. 2004, 29, 642–649. [Google Scholar] [PubMed]
- Botha, F.; Botha, S. Effect of biological contamination on dentine bond strength of adhesive resins. SADJ 2003, 58, 143–147. [Google Scholar]
- Eiriksson, S.O.; Pereira, P.N.; Swift, E.J.; Heymann, H.O.; Sigurdsson, A. Effects of saliva contamination on resin–resin bond strength. Dent. Mater. 2004, 20, 37–44. [Google Scholar] [CrossRef]
- Taneja, S.; Kumari, M.; Bansal, S. Effect of saliva and blood contamination on the shear bond strength of fifth-, seventh-, and eighth-generation bonding agents: An in vitro study. J. Conserv. Dent. 2017, 20, 157. [Google Scholar] [CrossRef] [PubMed]
- Neelagiri, K.; Kundabala, M.; Shashi, R.A.; Thomas, M.S.; Parolia, A. Effects of saliva contamination and decontamination procedures on shear bond strength of self-etch dentine bonding systems: An in vitro study. J. Conserv. Dent. 2010, 13, 71. [Google Scholar] [PubMed]
- Furuse, A.Y.; Cunha, L.F.D.; Benetti, A.R.; Mondelli, J. Bond strength of resin–resin interfaces contaminated with saliva and submitted to different surface treatments. J. Appl. Oral Sci. 2007, 15, 501–505. [Google Scholar] [CrossRef] [PubMed]
- Fritz, U.B.; Finger, W.J.; Stean, H. Salivary contamination during bonding procedures with a one-bottle adhesive system. Quintessence Int. 1998, 29, 567–572. [Google Scholar] [PubMed]
- Sattabanasuk, V.; Shimada, Y.; Tagami, J. Effects of saliva contamination on dentin bond strength using all-in-one adhesives. J. Adhes. Dent. 2006, 8, 311–318. [Google Scholar] [PubMed]
- Munaga, S.; Chitumalla, R.; Kubigiri, S.K.; Rawtiya, M.; Khan, S.; Sajjan, P. Effect of saliva contamination on the shear bond strength of a new self-etch adhesive system to dentin. J. Conserv. Dent. 2014, 17, 31. [Google Scholar] [CrossRef] [PubMed]
- Yoo, H.M.; Oh, T.S.; Pereira, P.N.R. Effect of saliva contamination on the microshear bond strength of one-step self-etching adhesive systems to dentin. Oper. Dent. 2006, 31, 127–134. [Google Scholar] [CrossRef] [PubMed]
- Taskonak, B.; Sertgöz, A. Shear bond strengths of saliva contaminated ‘one-bottle’adhesives. J. Oral Rehabil. 2002, 29, 559–564. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Lee, K. The influence of salivary contamination on shear bond strength of dentin adhesive systems. Oper. Dent. 2004, 29, 437–442. [Google Scholar] [PubMed]
- Jacobsen, T.; Söderholm, K.-J. Some effects of water on dentin bonding. Dent. Mater. 1995, 11, 132–136. [Google Scholar] [CrossRef]
- El-Kalla, I.H.; García-Godoy, F. Saliva contamination and bond strength of single-bottle adhesives to enamel and dentin. Am. J. Dent. 1997, 10, 83–87. [Google Scholar] [PubMed]
- Kesar, N.; Madan, M.; Dua, P.; Saini, S.; Mangla, R.; Kumar, A. Comparative evaluation of shear bond strength of two adhesive systems before and after contamination with oral fluids: An in vitro study. Indian J. Dent. Sci. 2017, 9, 189. [Google Scholar] [CrossRef]
- Armadi, A.; Usman, M.; Suprastiwi, E. Effect of saliva and blood contamination after etching upon the shear bond strength between composite resin and enamel. J. Phys. Conf. Ser. 2017, 884, 012003. [Google Scholar] [CrossRef] [Green Version]
- Neves, A.D.; Discacciati, J.A.C.; Oréfice, R.L.; Jansen, W.C. Correlation between degree of conversion, microhardness and inorganic content in composites. Pesqui. Odontol. Bras. 2002, 16, 349–354. [Google Scholar] [CrossRef] [PubMed]
- Ferracane, J.L. Correlation between hardness and degree of conversion during the setting reaction of unfilled dental restorative resins. Dent. Mater. 1985, 1, 11–14. [Google Scholar] [CrossRef]
- Galvão, M.R.; Caldas, S.G.F.R.; Bagnato, V.S.; De Souza Rastelli, A.N.; De Andrade, M.F. Evaluation of degree of conversion and hardness of dental composites photo-activated with different light guide tips. Eur. J. Dent. 2013, 7, 86. [Google Scholar] [PubMed]
- Ilie, N.; Hickel, R. Quality of curing in relation to hardness, degree of cure and polymerization depth measured on a nano-hybrid composite. Am. J. Dent. 2007, 20, 263–268. [Google Scholar] [PubMed]
- Hansen, E.K.; Asmussen, E. Correlation between depth of cure and surface hardness of a light-activated resin. Scand. J. Dent. Res. 1993, 101, 62–64. [Google Scholar] [CrossRef] [PubMed]
- Sheikh, H.; Heymann, H.O.; Swift, E.J., Jr.; Ziemiecki, T.L.; Ritter, A.V. Effect of saliva contamination and cleansing solutions on the bond strengths of self-etch adhesives to dentin. J. Esthet. Restor. Dent. 2010, 22, 402–410. [Google Scholar] [CrossRef] [PubMed]
- Campoy, M.D.; Plasencia, E.; Vicente, A.; Bravo, L.A.; Cibrián, R. Effect of saliva contamination on bracket failure with a self-etching primer: A prospective controlled clinical trial. Am. J. Orthod. Dent. Orthop. 2010, 137, 679–683. [Google Scholar] [CrossRef] [PubMed]
- Van Dijken, J.W.; Hörstedt, P. Effect of the use of rubber dam versus cotton rolls on marginal adaptation of composite resin fillings to acid-etched enamel. Acta Odontol. Scand. 1987, 45, 303–308. [Google Scholar] [CrossRef] [PubMed]
- Smales, R. Rubber dam usage related to restoration quality and survival. Br. Dent. J. 1993, 174, 330. [Google Scholar] [CrossRef] [PubMed]
- Cajazeira, M.; De, T.S.; Maia, L. Influence of the operatory field isolation technique on tooth-colored direct dental restorations. Am. J. Dent. 2014, 27, 155–159. [Google Scholar] [PubMed]
- Brunthaler, A.; König, F.; Lucas, T.; Sperr, W.; Schedle, A. Longevity of direct resin composite restorations in posterior teeth: A review. Clin. Oral Investig. 2003, 7, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Hitmi, L.; Attal, J.-P.; Degrange, M. Influence of the time-point of salivary contamination on dentin shear bond strength of 3 dentin adhesive systems. J. Adhes. Dent. 1999, 1, 219–232. [Google Scholar] [PubMed]
- Barghi, N.; Knight, G.; Berry, T. Comparing two methods of moisture control in bonding to enamel: A clinical study. Oper. Dent. 1991, 16, 130–135. [Google Scholar] [PubMed]
- Powers, J.M.; Finger, W.J.; Xie, J. Bonding of composite resin to contaminated human enamel and dentin. J. Prosthodont. 1995, 4, 28–32. [Google Scholar] [CrossRef] [PubMed]
- Johnson, M.E.; Burgess, J.O.; Hermesch, C.B.; Buikema, D.J. Saliva contamination of dentin bonding agents. Oper. Dent. 1994, 19, 205–210. [Google Scholar] [PubMed]
- Peschke, A.; Blunck, U.; Roulet, J. Influence of incorrect application of a water-based adhesive system on the marginal adaptation of Class V restorations. Am. J. Dent. 2000, 13, 239–244. [Google Scholar] [PubMed]
| Group | Microhardness (VHN) | |||
|---|---|---|---|---|
| Mean | Standard Deviation | Minimum | Maximum | |
| T0 | 108.82 | 15.58 | 85.50 | 144.00 |
| T2 | 103.64 | 3.74 | 97.50 | 110.00 |
| T5 | 105.62 | 14.07 | 89.90 | 142.00 |
| T10 | 101.59 | 6.87 | 87.90 | 112.00 |
| T15 | 109.53 | 7.05 | 97.70 | 120.00 |
| T20 | 114.74 | 18.47 | 101.60 | 163.30 |
| T30 | 102.76 | 5.60 | 96.20 | 115.30 |
| T40 | 107.78 | 9.61 | 100.80 | 132.20 |
| Group | Mean Rank | Χ2 | df | p-Value |
|---|---|---|---|---|
| T0 | 46.55 | 13.509 | 7 | 0.061 |
| T2 | 34.95 | |||
| T5 | 32.80 | |||
| T10 | 28.40 | |||
| T15 | 53.05 | |||
| T20 | 54.45 | |||
| T30 | 30.65 | |||
| T40 | 43.15 |
| Group | Degree of Conversion (%) | |||
|---|---|---|---|---|
| Mean | Standard Deviation | Minimum | Maximum | |
| T0 | 93.73 | 2.79 | 89.25 | 96.74 |
| T2 | 96.17 | 2.10 | 94.34 | 98.70 |
| T5 | 97.49 | 0.64 | 96.76 | 98.36 |
| T10 | 94.25 | 2.54 | 91.06 | 97.44 |
| T15 | 94.65 | 2.79 | 91.43 | 97.87 |
| T20 | 96.83 | 1.57 | 95.05 | 98.81 |
| T30 | 94.70 | 3.68 | 89.68 | 97.63 |
| T40 | 95.81 | 1.69 | 92.96 | 97.06 |
| Sum of Squares | df | Mean Square | F | p-Value | |
|---|---|---|---|---|---|
| Between groups | 61.637 | 7 | 8.805 | 1.541 | 0.189 |
| Within groups | 182.852 | 32 | 5.714 | - | - |
| Total | 244.489 | 39 | - | - | - |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sahebalam, R.; Boruziniat, A.; Mohammadzadeh, F.; Rangrazi, A. Effect of the Time of Salivary Contamination during Light Curing on Degree of Conversion and Microhardness of a Restorative Composite Resin. Biomimetics 2018, 3, 23. https://doi.org/10.3390/biomimetics3030023
Sahebalam R, Boruziniat A, Mohammadzadeh F, Rangrazi A. Effect of the Time of Salivary Contamination during Light Curing on Degree of Conversion and Microhardness of a Restorative Composite Resin. Biomimetics. 2018; 3(3):23. https://doi.org/10.3390/biomimetics3030023
Chicago/Turabian StyleSahebalam, Rasoul, Alireza Boruziniat, Fahimeh Mohammadzadeh, and Abdolrasoul Rangrazi. 2018. "Effect of the Time of Salivary Contamination during Light Curing on Degree of Conversion and Microhardness of a Restorative Composite Resin" Biomimetics 3, no. 3: 23. https://doi.org/10.3390/biomimetics3030023





