Controlled Release of Vascular Endothelial Growth Factor from Heparin-Functionalized Gelatin Type A and Albumin Hydrogels
Abstract
:1. Introduction
2. Results and Discussion
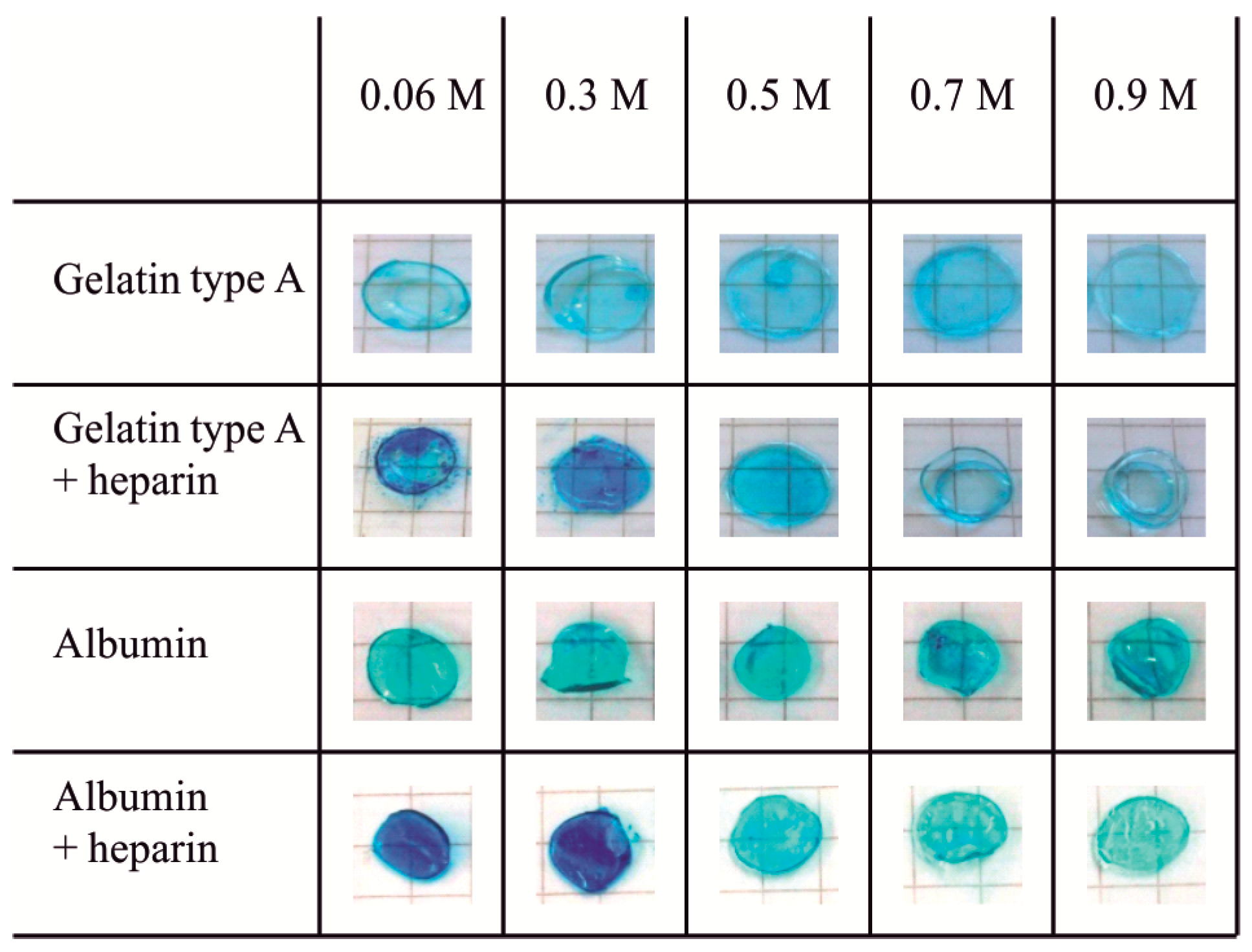
2.1. Heparin Functionalization of Hydrogels
2.2. Physicochemical Characterization of Biopolymer Hydrogels
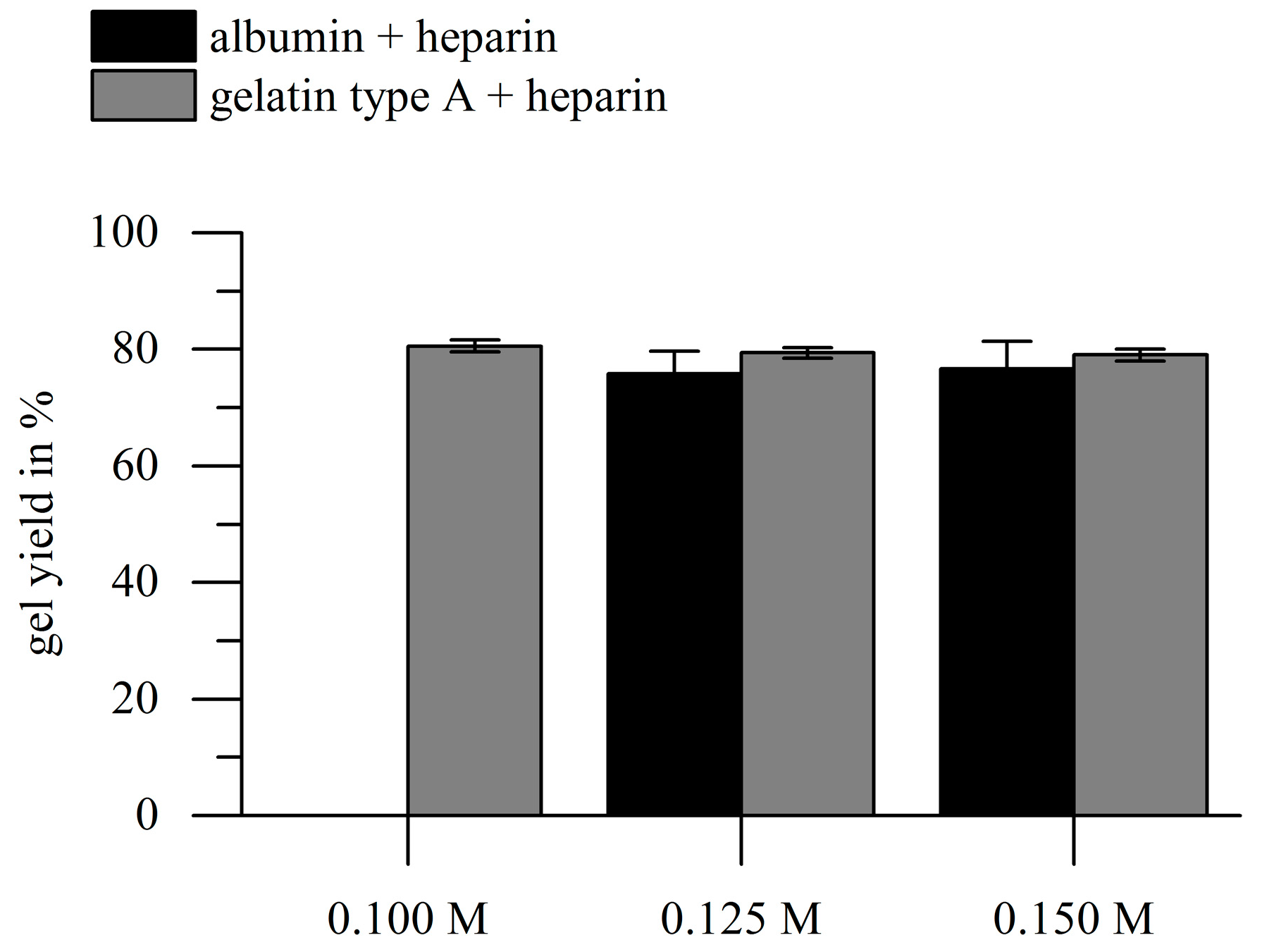
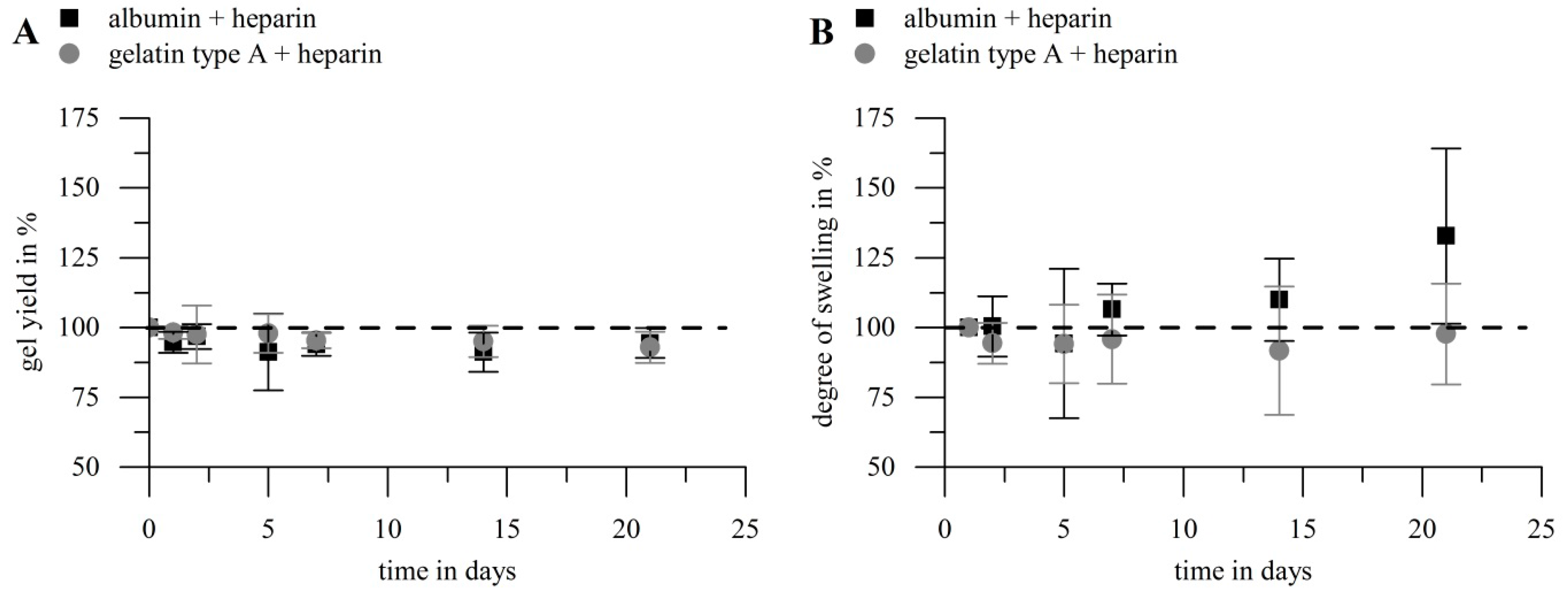
2.2.1. Gel Yield
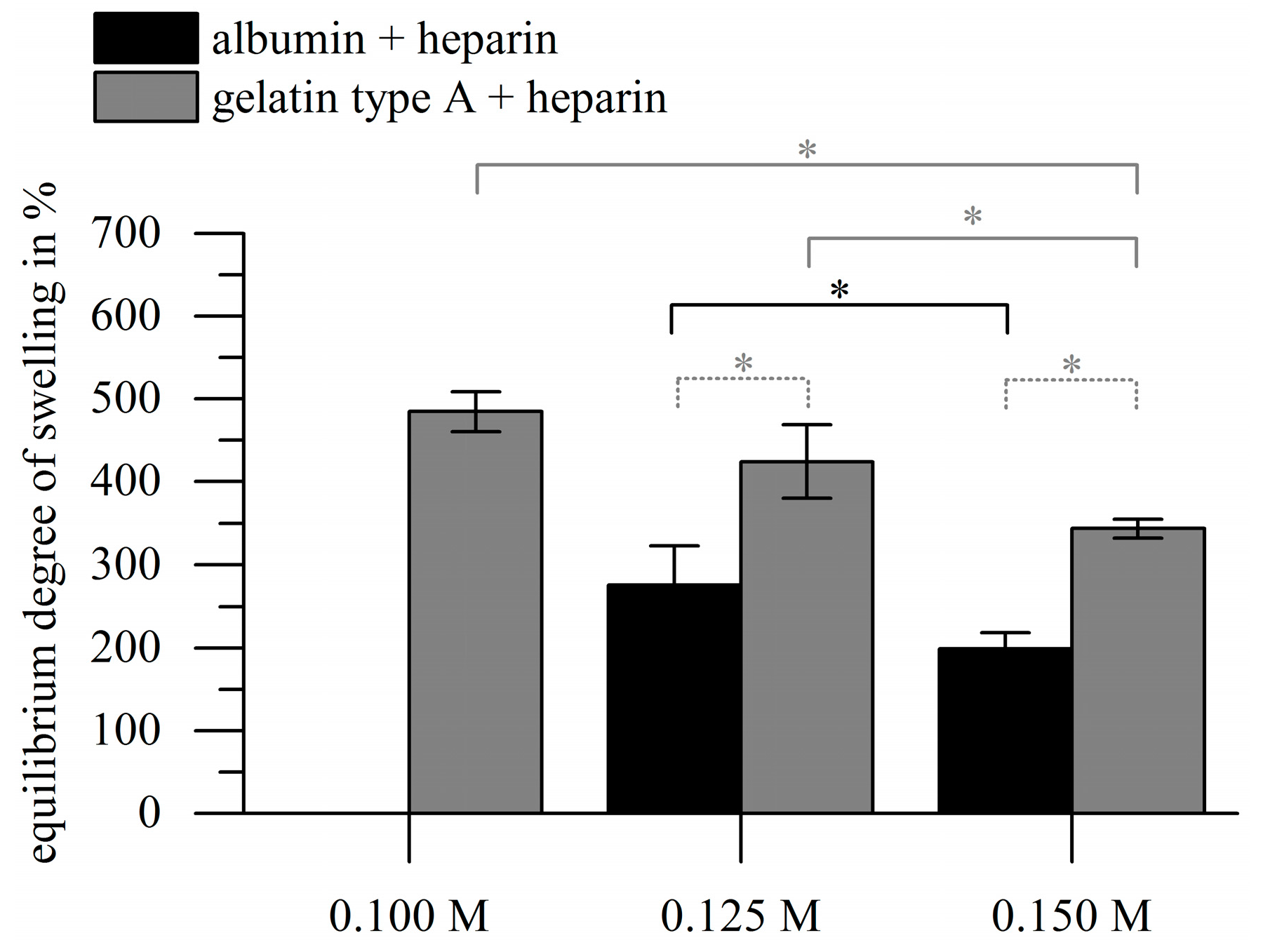
2.2.2. Swelling Kinetics and Equilibrium Degree of Swelling
2.2.3. Hydrolytic Stability of Hydrogels
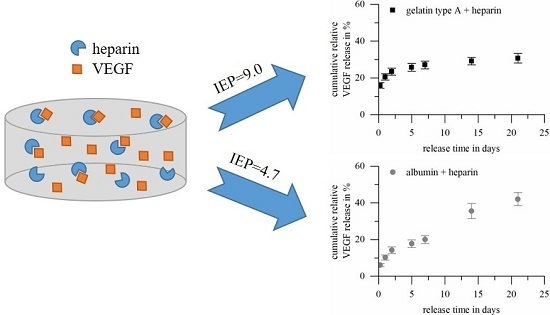
2.3. Loading and Release of Vascular Endothelial Growth Factor
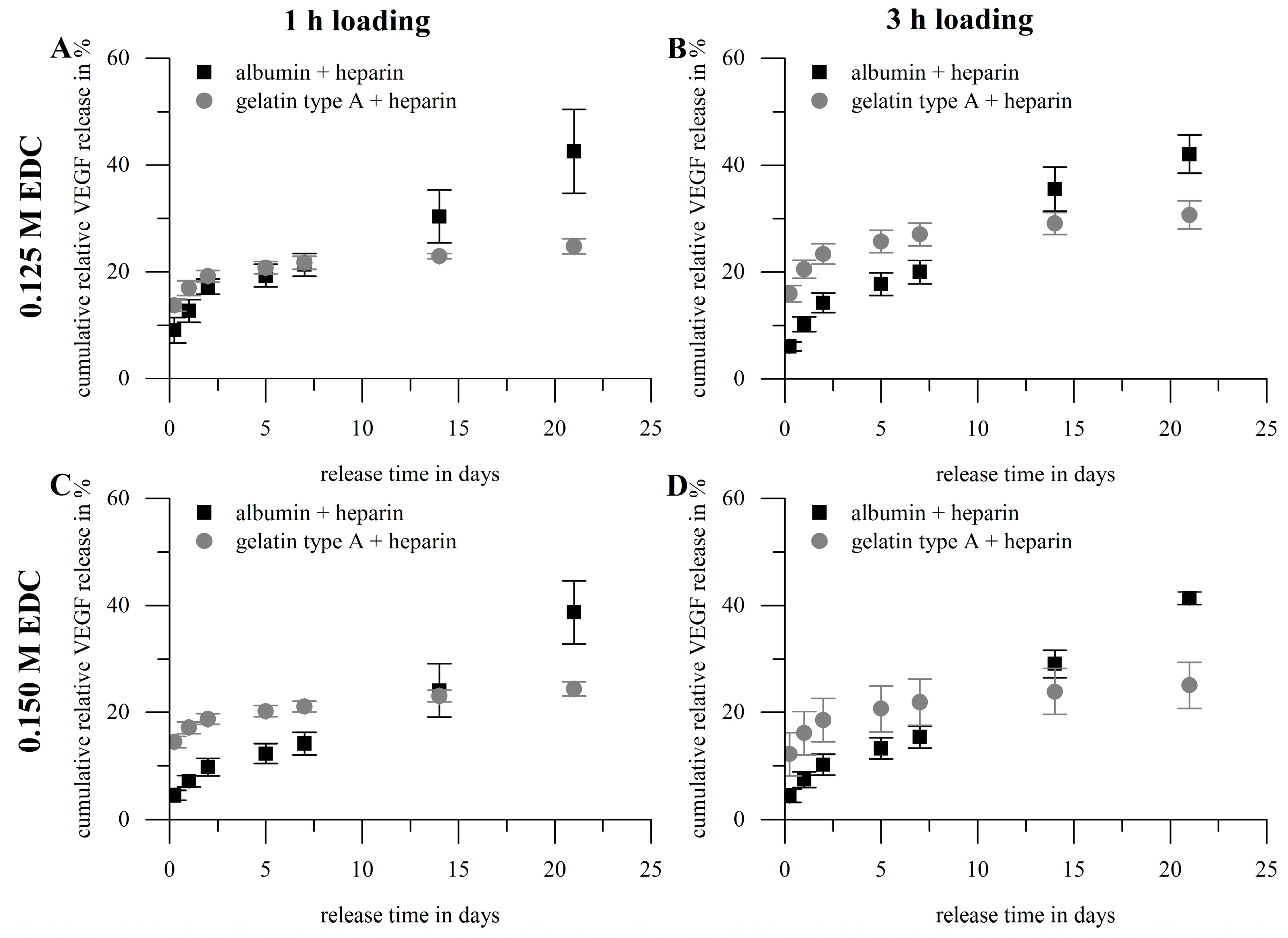
- The loading efficiency (Figure 7A) of albumin-based hydrogels was in the range of 76.0–87.2% and significantly higher compared to the loading efficiency of gelatin type A-based gels in the range of 35.6–51.6%. The loading efficiency of both hydrogel types decreased with increasing loading time, while no general significant effect for the crosslinker concentration was observed. The highest loading was achieved at 1 h and 0.15 M EDC for albumin-based gels and 1 h and 0.125 M EDC for gelatin-based materials.
- The burst release (release within the first 24 h; Figure 7B) was lower for albumin-based hydrogels (7.1–12.7%) compared to gelatin type A-based gels (16.1–20.5%); that correlates to 8.1–15.4% of the loaded cargo for albumin-based gels and 32.9–56.8% for gelatin-based gels, respectively. Albumin-based gels showed the lowest bust release after 1 h loading and crosslinking with 0.15 M EDC, and a negative correlation between burst release and crosslinker concentration; while gelatin-based gels showed a similar burst release at 1 h loading and 0.125 M EDC and 3 h loading and 0.15 M EDC.
- Cumulative release of VEGF (release within 21 days; Figure 7C) from albumin-heparin gels was in the range of 38.7–42.5%, and therefore significantly higher than for gelatin-heparin gels (24.4–30.7%). The cumulative releases correlate to 44.4–55.4% of the loaded cargo for albumin-based gels and 47.9–85.0% for gelatin-based gels, respectively. Neither duration of loading, nor concentration of crosslinker did have significant impact on the cumulated release.
- The average release rates between day 7 and day 21 (Figure 7D) for albumin-based hydrogels were in the range of 1.3–1.6%, and again significantly higher compared to release rates of gelatin type A-heparin gels of 0.3–0.4%, with again no significant effect of loading time or crosslinker concentration.
- The remaining VEGF amount in the hydrogels after 21 days of release was only determined for gelatin-based hydrogels, since gelatin can be selectively degraded via collagenase without affecting the bioactivity of VEGF. For albumin no such an enzyme was available. The remaining VEGF-content in the gelatin-based gels was in the range of 7.2–9.8% and showed again no significant influence of loading time or crosslinker concentration.
3. Conclusions
4. Materials and Methods
4.1. Materials
4.2. Preparation of Heparin-Functionalized Hydrogels
4.3. Investigation of Heparin Functionalization
4.4. Gravimetric Characterization: Gel Yield and Degree of Swelling
4.5. Hydrolytic Stability of Hydrogels
4.6. Loading and Release of Vascular Endothelial Growth Factor
4.7. Statistical Analysis
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Morais, J.M.; Papadimitrakopoulos, F.; Burgess, D.J. Biomaterials/tissue interactions: Possible solutions to overcome foreign body response. AAPS J. 2010, 12, 188–196. [Google Scholar] [CrossRef] [PubMed]
- Novosel, E.C.; Kleinhans, C.; Kluger, P.J. Vascularization is the key challenge in tissue engineering. Adv. Drug Deliv. Rev. 2011, 63, 300–311. [Google Scholar] [CrossRef] [PubMed]
- Bos, G.W.; Scharenborg, N.M.; Poot, A.A.; Engbers, G.H.M.; Beugeling, T.; van Aken, W.G.; Feijen, J. Endothelialization of crosslinked albumin-heparin gels. Thromb Haemost. 1999, 82, 1757–1763. [Google Scholar] [PubMed]
- Giol, E.D.; Schaubroeck, D.; Kersemans, K.; de Vos, F.; van Vlierberghe, S.; Dubruel, P. Bio-inspired surface modification of pet for cardiovascular applications: Case study of gelatin. Colloid Surf. B 2015, 134, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Crombez, M.; Chevallier, P.; Gaudreault, R.C.; Petitclerc, E.; Mantovani, D.; Laroche, G. Improving arterial prosthesis neo-endothelialization: Application of a proactive vegf construct onto ptfe surfaces. Biomaterials 2005, 26, 7402–7409. [Google Scholar] [CrossRef] [PubMed]
- Hatano, T.; Miyamoto, S.; Kawakami, O.; Yamada, K.; Hashimoto, N.; Tabata, Y. Acceleration of aneurysm healing by controlled release of basic fibroblast growth factor with the use of polyethylene terephthalate fiber coils coated with gelatin hydrogel. Neurosurgery 2003, 53, 393–400. [Google Scholar] [CrossRef] [PubMed]
- Takaoka, R.; Hikasa, Y.; Tabata, Y. Vascularization around poly(tetrafluoroethylene) mesh with coating of gelatin hydrogel incorporating basic fibroblast growth factor. J. Biomater. Sci. Polym. Ed. 2009, 20, 1483–1494. [Google Scholar] [CrossRef] [PubMed]
- Censi, R.; di Martino, P.; Vermonden, T.; Hennink, W.E. Hydrogels for protein delivery in tissue engineering. J. Control. Release 2012, 161, 680–692. [Google Scholar] [CrossRef] [PubMed]
- Vermonden, T.; Censi, R.; Hennink, W.E. Hydrogels for protein delivery. Chem. Rev. 2012, 112, 2853–2888. [Google Scholar] [CrossRef] [PubMed]
- Kretlow, J.D.; Klouda, L.; Mikos, A.G. Injectable matrices and scaffolds for drug delivery in tissue engineering. Adv. Drug Deliv. Rev. 2007, 59, 263–273. [Google Scholar] [CrossRef] [PubMed]
- Zhu, J.; Marchant, R.E. Design properties of hydrogel tissue-engineering scaffolds. Expert Rev. Med. Device 2011, 8, 607–626. [Google Scholar] [CrossRef] [PubMed]
- Rose, J.B.; Pacelli, S.; Haj, A.J.E.; Dua, H.S.; Hopkinson, A.; White, L.J.; Rose, F.R.A.J. Gelatin-based materials in ocular tissue engineering. Materials 2014, 7, 3106–3135. [Google Scholar] [CrossRef] [PubMed]
- Santoro, M.; Tatara, A.M.; Mikos, A.G. Gelatin carriers for drug and cell delivery in tissue engineering. J. Control. Release 2014, 190, 210–218. [Google Scholar] [CrossRef] [PubMed]
- Devi, N.; Deka, C.; Maji, T.K.; Kakati, D.K. Gelatin and gelatin: Polyelectrolyte complexes: Drug delivery. In Encyclopedia of Biomedical Polymers and Polymeric Biomaterials; CRC Press: Boca Raton, FL, USA, 2015; pp. 3557–3569. [Google Scholar]
- Foox, M.; Zilberman, M. Drug delivery from gelatin-based systems. Expert Opin. Drug Deliv. 2015, 12, 1547–1563. [Google Scholar] [CrossRef] [PubMed]
- Tabata, Y.; Ikada, Y. Protein release from gelatin matrices. Adv. Drug Deliv. Rev. 1998, 31, 287–301. [Google Scholar] [CrossRef]
- Young, S.; Wong, M.; Tabata, Y.; Mikos, A.G. Gelatin as a delivery vehicle for the controlled release of bioactive molecules. J. Control. Release 2005, 109, 256–274. [Google Scholar] [CrossRef] [PubMed]
- Elzoghby, A.O. Gelatin-based nanoparticles as drug and gene delivery systems: Reviewing three decades of research. J. Control. Release 2013, 172, 1075–1091. [Google Scholar] [CrossRef] [PubMed]
- Mariod, A.A.; Fadul, H. Review: Gelatin, source, extraction and industrial applications. Acta Sci. Pol. Technol. Aliment. 2013, 12, 135–147. [Google Scholar] [CrossRef]
- Schrieber, R.; Gareis, H. Gelatine Handbook—Theory and Industrial Practice; WILEY-VCH Verlag GmbH & Co. KGaA: Weinheim, Germany, 2007. [Google Scholar]
- Yamamoto, M.; Ikada, Y.; Tabata, Y. Controlled release of growth factors based on biodegradation of gelatin hydrogel. J. Biomater. Sci. Polym. Ed. 2001, 12, 77–88. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, M.; Tabata, Y.; Ikada, Y. Growth factor release from gelatin hydrogel for tissue engineering. J. Bioact. Compat. Polym. 1999, 14, 474–489. [Google Scholar] [CrossRef]
- Tabata, Y.; Hijikata, S.; Ikada, Y. Enhanced vascularization and tissue granulation by basic fibroblast growth-factor impregnated in gelatin hydrogels. J. Control. Release 1994, 31, 189–199. [Google Scholar] [CrossRef]
- Tabata, Y.; Ikada, Y. Vascularization effect of basic fibroblast growth factor released from gelatin hydrogels with different biodegradabilities. Biomaterials 1999, 20, 2169–2175. [Google Scholar] [CrossRef]
- Layman, H.; Spiga, M.-G.; Brooks, T.; Pham, S.; Webster, K.A.; Andreopoulos, F.M. The effect of the controlled release of basic fibroblast growth factor from ionic gelatin-based hydrogels on angiogenesis in a murine critical limb ischemic model. Biomaterials 2007, 28, 2646–2654. [Google Scholar] [CrossRef] [PubMed]
- Kimura, Y.; Tabata, Y. Controlled release of stromal-cell-derived factor-1 from gelatin hydrogels enhances angiogenesis. J. Biomat. Sci. Polym. Ed. 2010, 21, 37–51. [Google Scholar] [CrossRef] [PubMed]
- Muniruzzaman, M.; Tabata, Y.; Ikada, Y. Complexation of basic fibroblast growth factor with gelatin. J. Biomater. Sci. Polym. Ed. 1998, 9, 459–473. [Google Scholar] [CrossRef]
- Li, X.W.; Ma, C.; Xie, X.H.; Sun, H.C.; Liu, X.H. Pulp regeneration in a full-length human tooth root using a hierarchical nanofibrous microsphere system. Acta Biomater. 2016, 35, 57–67. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Qu, T.J.; Ding, C.; Ma, C.; Sun, H.C.; Li, S.R.; Liu, X.H. Injectable gelatin derivative hydrogels with sustained vascular endothelial growth factor release for induced angiogenesis. Acta Biomater. 2015, 13, 88–100. [Google Scholar] [CrossRef] [PubMed]
- Hwang, J.H.; Kim, I.G.; Lee, J.Y.; Piao, S.; Lee, D.S.; Lee, T.S.; Ra, J.C.; Lee, J.Y. Therapeutic lymphangiogenesis using stem cell and vegf-c hydrogel. Biomaterials 2011, 32, 4415–4423. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, S.; Kubo, T.; Ijima, H. Heparin-conjugated gelatin as a growth factor immobilization scaffold. J. Biosci. Bioeng. 2013, 115, 562–567. [Google Scholar] [CrossRef] [PubMed]
- Pacelli, S.; Acosta, F.; Chakravarti, A.R.; Samanta, S.G.; Whitlow, J.; Modaresi, S.; Ahmed, R.P.H.; Rajasingh, J.; Paul, A. Nanodiamond-based injectable hydrogel for sustained growth factor release: Preparation, characterization and in vitro analysis. Acta Biomater. 2017, 58, 479–491. [Google Scholar] [CrossRef] [PubMed]
- Kumorek, M.; Kubies, D.; Filova, E.; Houska, M.; Kasoju, N.; Mazl Chanova, E.; Matejka, R.; Kryslova, M.; Bacakova, L.; Rypacek, F. Cellular responses modulated by fgf-2 adsorbed on albumin/heparin layer-by-layer assemblies. PLoS ONE 2015, 10, e0125484. [Google Scholar] [CrossRef] [PubMed]
- Bos, G.W.; Scharenborg, N.M.; Poot, A.A.; Engbers, G.H.M.; Terlingen, J.G.A.; Beugeling, T.; van Aken, W.G.; Feijen, J. Adherence and proliferation of endothelial cells on surface-immobilized albumin-heparin conjugate. Tissue Eng. 1998, 4, 267–279. [Google Scholar] [CrossRef] [PubMed]
- Cremers, H.F.M.; Verrijk, R.; Noteborn, H.P.J.M.; Kwon, G.; Bae, Y.H.; Kim, S.W.; Feijen, J. Adriamycin loading and release characteristics of albumin-heparin conjugate microspheres. J. Control. Release 1994, 29, 143–155. [Google Scholar] [CrossRef]
- Elcin, Y.M.; Dixit, V.; Gitnick, G. Controlled release of endothelial cell growth factor from chitosan-albumin microspheres for localized angiogenesis: In vitro and in vivo studies. Artif. Cells Blood Substit. Immobil. Biotechnol. 1996, 24, 257–271. [Google Scholar] [CrossRef] [PubMed]
- Elzoghby, A.O.; Samy, W.M.; Elgindy, N.A. Albumin-based nanoparticles as potential controlled release drug delivery systems. J. Control. Release 2012, 157, 168–182. [Google Scholar] [CrossRef] [PubMed]
- Baler, K.; Michael, R.; Szleifer, I.; Ameer, G.A. Albumin hydrogels formed by electrostatically triggered self-assembly and their drug delivery capability. Biomacromolecules 2014, 15, 3625–3633. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Kieltyka, R.E.; Jesse, W.; Norder, B.; Korobko, A.V.; Kros, A. Thiolated human serum albumin cross-linked dextran hydrogels as a macroscale delivery system. Soft Matter 2014, 10, 4869–4874. [Google Scholar] [CrossRef] [PubMed]
- Hirose, M.; Tachibana, A.; Tanabe, T. Recombinant human serum albumin hydrogel as a novel drug delivery vehicle. Mater. Sci. Eng. C 2010, 30, 664–669. [Google Scholar] [CrossRef]
- Sun, Y.; Huang, Y. Disulfide-crosslinked albumin hydrogels. J. Mater. Chem. B 2016, 4, 2768–2775. [Google Scholar] [CrossRef]
- Scott, J.; Dorling, J. Differential staining of acid glycosaminoglycans (mucopolysaccharides) by alcian blue in salt solutions. Histochemistry 1965, 5, 221–233. [Google Scholar] [CrossRef] [PubMed]
- Meloun, B.; Moravek, L.; Kostka, V. Complete amino acid sequence of hunman serum albumin. FEBS Lett. 1975, 58, 134–137. [Google Scholar] [CrossRef]
- Adhirajan, N.; Thanavel, R.; Naveen, N.; Uma, T.S.; Babu, M. Functionally modified gelatin microspheres as a growth factor’s delivery system: Development and characterization. Polym. Bull. 2014, 71, 1015–1030. [Google Scholar] [CrossRef]
- Wissink, M.; Beernink, R.; Poot, A.; Engbers, G.; Beugeling, T.; van Aken, W.; Feijen, J. Improved endothelialization of vascular grafts by local release of growth factor from heparinized collagen matrices. J. Control. Release 2000, 64, 103–114. [Google Scholar] [CrossRef]
- Hoch, E.; Schuh, C.; Hirth, T.; Tovar, G.E.; Borchers, K. Stiff gelatin hydrogels can be photo-chemically synthesized from low viscous gelatin solutions using molecularly functionalized gelatin with a high degree of methacrylation. J. Mater. Sci. Mater. Med. 2012, 23, 2607–2617. [Google Scholar] [CrossRef] [PubMed]
- Ganji, F.; Vasheghani-Farahani, S.; Vasheghani-Farahani, E. Theoretical description of hydrogel swelling: A review. Iran. Polym. J. 2010, 19, 375–398. [Google Scholar]
- Lai, J.Y.; Lu, P.L.; Chen, K.H.; Tabata, Y.; Hsiue, G.H. Effect of charge and molecular weight on the functionality of gelatin carriers for corneal endothelial cell therapy. Biomacromolecules 2006, 7, 1836–1844. [Google Scholar] [CrossRef] [PubMed]
- Kang, H.W.; Tabata, Y.; Ikada, Y. Effect of porous structure on the degradation of freeze-dried gelatin hydrogels. J. Bioact. Compat. Polym. 1999, 14, 331–343. [Google Scholar] [CrossRef]
- Kuijpers, A.J.; Engbers, G.H.M.; Feijen, J.; de Smedt, S.C.; Meyvis, T.K.L.; Demeester, J.; Krijgsveld, J.; Zaat, S.A.J.; Dankert, J. Characterization of the network structure of carbodiimide cross-linked gelatin gels. Macromolecules 1999, 32, 3325–3333. [Google Scholar] [CrossRef]
- Kuijpers, A.J.; Engbers, G.H.M.; Krijgsveld, J.; Zaat, S.A.J.; Dankert, J.; Feijen, J. Cross-linking and characterisation of gelatin matrices for biomedical applications. J. Biomater. Sci. Polym. Ed. 2000, 11, 225–243. [Google Scholar] [CrossRef]
- Coimbra, P.; Gil, M.H.; Figueiredo, M. Tailoring the properties of gelatin films for drug delivery applications: Influence of the chemical cross-linking method. Int. J. Biol. Macromol. 2014, 70, 10–19. [Google Scholar] [CrossRef] [PubMed]
- Ullm, S.; Krüger, A.; Tondera, C.; Gebauer, T.P.; Neffe, A.T.; Lendlein, A.; Jung, F.; Pietzsch, J. Biocompatibility and inflammatory response in vitro and in vivo to gelatin-based biomaterials with tailorable elastic properties. Biomaterials 2014, 35, 9755–9766. [Google Scholar] [CrossRef] [PubMed]
- Zhuang, C.; Tao, F.R.; Cui, Y.Z. Preparation and properties of gelatin films incorporated with n-hydroxysuccinimide-activated end-bit binary acid. Chem. Pap. 2016, 70, 505–514. [Google Scholar] [CrossRef]
- Ladewig, K. Drug delivery in soft tissue engineering. Expert Opin. Drug Deliv. 2011, 8, 1175–1188. [Google Scholar] [CrossRef] [PubMed]
- Patel, Z.S.; Ueda, H.; Yamamoto, M.; Tabata, Y.; Mikos, A.G. In vitro and in vivo release of vascular endothelial growth factor from gelatin microparticles and biodegradable composite scaffolds. Pharm. Res. 2008, 25, 2370–2378. [Google Scholar] [CrossRef] [PubMed]
- Hori, K.; Sotozono, C.; Hamuro, J.; Yamasaki, K.; Kimura, Y.; Ozeki, M.; Tabata, Y.; Kinoshita, S. Controlled-release of epidermal growth factor from cationized gelatin hydrogel enhances corneal epithelial wound healing. J. Control. Release 2007, 118, 169–176. [Google Scholar] [CrossRef] [PubMed]
- Kwon, G.S.; Bae, Y.H.; Cremers, H.; Feijen, J.; Kim, S.W. Release of proteins via ion-exchange from albumin-heparin microspheres. J. Control. Release 1992, 22, 83–93. [Google Scholar] [CrossRef]
- Niu, G.; Choi, J.S.; Wang, Z.; Skardal, A.; Giegengack, M.; Soker, S. Heparin-modified gelatin scaffolds for human corneal endothelial cell transplantation. Biomaterials 2014, 35, 4005–4014. [Google Scholar] [CrossRef] [PubMed]
- Ozawa, C.R.; Banfi, A.; Glazer, N.L.; Thurston, G.; Springer, M.L.; Kraft, P.E.; McDonald, D.M.; Blau, H.M. Microenvironmental vegf concentration, not total dose, determines a threshold between normal and aberrant angiogenesis. J. Clin. Investig. 2004, 113, 516–527. [Google Scholar] [CrossRef] [PubMed]


© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Claaßen, C.; Sewald, L.; Tovar, G.E.M.; Borchers, K. Controlled Release of Vascular Endothelial Growth Factor from Heparin-Functionalized Gelatin Type A and Albumin Hydrogels. Gels 2017, 3, 35. https://doi.org/10.3390/gels3040035
Claaßen C, Sewald L, Tovar GEM, Borchers K. Controlled Release of Vascular Endothelial Growth Factor from Heparin-Functionalized Gelatin Type A and Albumin Hydrogels. Gels. 2017; 3(4):35. https://doi.org/10.3390/gels3040035
Chicago/Turabian StyleClaaßen, Christiane, Lisa Sewald, Günter E. M. Tovar, and Kirsten Borchers. 2017. "Controlled Release of Vascular Endothelial Growth Factor from Heparin-Functionalized Gelatin Type A and Albumin Hydrogels" Gels 3, no. 4: 35. https://doi.org/10.3390/gels3040035