Acute Care for Elders (ACE) Team Model of Care: A Clinical Overview
Abstract
:1. Introduction
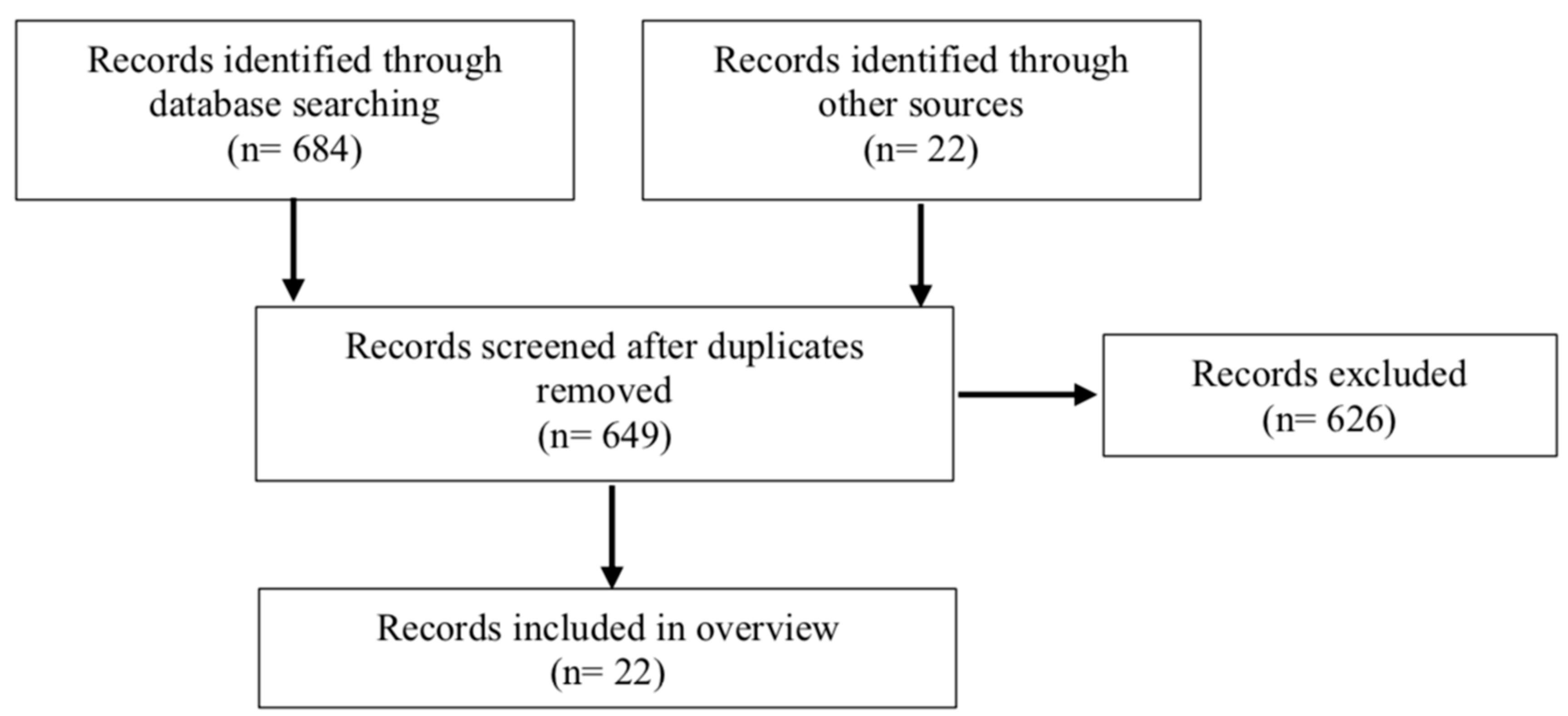
2. Methods
3. Results
3.1. Studies from ACE Units: Geriatric Processes of Care
3.2. Studies from ACE Units: Function and Mobility Outcomes
3.3. Studies from ACE Units: Additional Outcomes
3.4. Studies from ACE Units: Healthcare Utilization
3.5. Studies from ACE Services
4. Discussion
5. Conclusions
Funding
Acknowledgments
Conflicts of Interest
References
- Institute of Medicine Committee on Quality of Health Care in America. To Err is Human: Building a Safer Health System; Kohn, L.T., Corrigan, J.M., Donaldson, M.S., Eds.; National Academies Press (US): Washington, DC, USA, 2000. [Google Scholar]
- Institute of Medicine Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century; National Academies Press (US): Washington, DC, USA, 2001. [Google Scholar]
- Palmer, R.M.; Landefeld, C.S.; Kresevic, D.; Kowal, J. A medical unit for the acute care of the elderly. J. Am. Geriatr. Soc. 1994, 42, 545–552. [Google Scholar] [CrossRef] [PubMed]
- Landefeld, C.S.; Palmer, R.M.; Kresevic, D.M.; Fortinsky, R.H.; Kowal, J. A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients. N. Engl. J. Med. 1995, 332, 1338–1344. [Google Scholar] [CrossRef] [PubMed]
- Grant, M.J.; Booth, A. A typology of reviews: An analysis of 14 review types and associated methodologies. Health Inf. Libr. J. 2009, 26, 91–108. [Google Scholar] [CrossRef] [PubMed]
- Perez-Zepeda, M.U.; Gutierez-Robledo, L.M.; Sanchez-Garcia, S.; Juarez-Cedillo, T.; Gonzalez, J.J.; Franco-Marina, F.; Garcia-Pena, C. Comparison of a geriatric unit with a general ward in Mexican elders. Arch. Gerontol. Geriatr. 2012, 54, e370–e375. [Google Scholar] [CrossRef] [PubMed]
- Covinsky, K.E.; King, J.T., Jr.; Quinn, L.M.; Siddique, R.; Palmer, R.; Kresevic, D.M.; Fortinsky, R.H.; Kowal, J.; Landefeld, C.S. Do acute care for elders units increase hospital costs? A cost analysis using the hospital perspective. J. Am. Geriatr. Soc. 1997, 45, 729–734. [Google Scholar] [CrossRef] [PubMed]
- Stewart, M.; Suchak, N.; Scheve, A.; Popat-Thakkar, V.; David, E.; Laquinte, J.; Gloth, F.M., 3rd. The impact of a geriatrics evaluation and management unit compared to standard care in a community teaching hospital. Md. Med. J. 1999, 48, 62–67. [Google Scholar] [PubMed]
- Counsell, S.R.; Holder, C.M.; Liebenauer, L.L.; Palmer, R.M.; Fortinsky, R.H.; Kresevic, D.M.; Quinn, L.M.; Allen, K.R.; Covinsky, K.E.; Landefeld, C.S. Effects of a multicomponent intervention on functional outcomes and process of care in hospitalized older patients: A randomized controlled trial of Acute Care for Elders (ACE) in a community hospital. J. Am. Geriatr. Soc. 2000, 48, 1572–1581. [Google Scholar] [CrossRef] [PubMed]
- Asplund, K.; Gustafson, Y.; Jacobsson, C.; Bucht, G.; Wahlin, A.; Peterson, J.; Blom, J.O.; Angquist, K.A. Geriatric-based versus general wards for older acute medical patients: A randomized comparison of outcomes and use of resources. J. Am. Geriatr. Soc. 2000, 48, 1381–1388. [Google Scholar] [CrossRef] [PubMed]
- Saltvedt, I.; Mo, E.S.; Fayers, P.; Kaasa, S.; Sletvold, O. Reduced mortality in treating acutely sick, frail older patients in a geriatric evaluation and management unit. A prospective randomized trial. J. Am. Geriatr. Soc. 2002, 50, 792–798. [Google Scholar] [CrossRef] [PubMed]
- Naglie, G.; Tansey, C.; Kirkland, J.L.; Ogilvie-Harris, D.J.; Detsky, A.S.; Etchells, E.; Tomlinson, G.; O'Rourke, K.; Goldlist, B. Interdisciplinary inpatient care for elderly people with hip fracture: A randomized controlled trial. CMAJ 2002, 167, 25–32. [Google Scholar]
- Allen, K.R.; Hazelett, S.E.; Palmer, R.R.; Jarjoura, D.G.; Wickstrom, G.C.; Weinhardt, J.A.; Lada, R.; Holder, C.M.; Counsell, S.R. Developing a stroke unit using the acute care for elders intervention and model of care. J. Am. Geriatr. Soc. 2003, 51, 1660–1667. [Google Scholar] [CrossRef] [PubMed]
- Jayadevappa, R.; Chhatre, S.; Weiner, M.; Raziano, D.B. Health resource utilization and medical care cost of acute care elderly unit patients. Value Health 2006, 9, 186–192. [Google Scholar] [CrossRef] [PubMed]
- Zelada, M.A.; Salinas, R.; Baztan, J.J. Reduction of functional deterioration during hospitalization in an acute geriatric unit. Arch. Gerontol. Geriatr. 2009, 48, 35–39. [Google Scholar] [CrossRef] [PubMed]
- Malone, M.L.; Vollbrecht, M.; Stephenson, J.; Burke, L.; Pagel, P.; Goodwin, J.S. AcuteCare for Elders (ACE) tracker and e-Geriatrician: Methods to disseminate ACE concepts to hospitals with no geriatricians on staff. J. Am. Geriatr. Soc. 2010, 58, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Flood, K.L.; Brown, C.J.; Carroll, M.B.; Locher, J.L. Nutritional processes of care for older adults admitted to an oncology-acute care for elders unit. Crit. Rev. Oncol. Hematol. 2011, 78, 73–78. [Google Scholar] [CrossRef] [PubMed]
- Barnes, D.E.; Palmer, R.M.; Kresevic, D.M.; Fortinksy, R.H.; Kowal, J.; Chren, M.-M.; Landefeld, C.S. Acute Care For Elders Units Produced Shorter Hospital Stays At Lower Cost While Maintaining Patients’ Functional Status. Health Aff. 2012, 31, 1227–1236. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahmed, N.; Taylor, K.; McDaniel, Y.; Dyer, C.B. The role of an Acute Care for the Elderly unit in achieving hospital quality indicators while caring for frail hospitalized elders. Popul. Health Manag. 2012, 15, 236–240. [Google Scholar] [CrossRef] [PubMed]
- Flood, K.L.; Maclennan, P.A.; McGrew, D.; Green, D.; Dodd, C.; Brown, C.J. Effects of an acute care for elders unit on costs and 30-day readmissions. JAMA Intern. Med. 2013, 173, 981–987. [Google Scholar] [CrossRef] [PubMed]
- Borenstein, J.E.; Aronow, H.U.; Bolton, L.B.; Dimalanta, M.I.; Chan, E.; Palmer, K.; Zhang, X.; Rosen, B.; Braunstein, G.D. Identification and team-based interprofessional management of hospitalized vulnerable older adults. Nurs. Outlook 2016, 64, 137–145. [Google Scholar] [CrossRef] [PubMed]
- Ekerstad, N.; Karlson, B.W.; Dahlin Ivanoff, S.; Landahl, S.; Andersson, D.; Heintz, E.; Husberg, M.; Alwin, J. Is the acute care of frail elderly patients in a comprehensive geriatric assessment unit superior to conventional acute medical care? Clin. Interv. Aging 2017, 12, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Booth, K.A.; Simmons, E.E.; Viles, A.F.; Gray, W.A.; Kennedy, K.R.; Biswal, S.H.; Lowe, J.A.; Xhaja, A.; Kennedy, R.E.; Brown, C.J.; et al. Improving Geriatric Care Processes on Two Medical-Surgical Acute Care Units: A Pilot Study. J. Healthc. Qual. Off. Publ. Natl. Assoc. Healthc. Qual. 2018. [Google Scholar] [CrossRef] [PubMed]
- Wald, H.L.; Glasheen, J.J.; Guerrasio, J.; Youngwerth, J.M.; Cumbler, E.U. Evaluation of a hospitalist-run acute care for the elderly service. J. Hosp. Med. 2011, 6, 313–321. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yoo, J.W.; Kim, S.; Seol, H.; Kim, S.J.; Yang, J.M.; Ryu, W.S.; Min, T.J.; Choi, J.B.; Kwon, M.; Nakagawa, S. Effects of an internal medicine floor interdisciplinary team on hospital and clinical outcomes of seniors with acute medical illness. Geriatr. Gerontol. Int. 2013, 13, 942–948. [Google Scholar] [CrossRef] [PubMed]
- Hung, W.W.; Ross, J.S.; Farber, J.; Siu, A.L. Evaluation of the Mobile Acute Care of the Elderly (MACE) service. JAMA Intern. Med. 2013, 173, 990–996. [Google Scholar] [CrossRef] [PubMed]
- Coleman, E.A.; Smith, J.D.; Frank, J.C.; Eilertsen, T.B.; Thaire, J.N.; Kramer, A.M. Development and testing of a measure designated to assess the quality of care transitions. Int. J. Integr. Care 2002, 2, e02. [Google Scholar] [CrossRef] [PubMed]
- Glasgow, R.E. What does it mean to be pragmatic? Pragmatic methods, measures, and models to facilitate research translation. Health Educ. Behav. 2013, 40, 257–265. [Google Scholar] [CrossRef] [PubMed]
- Fulmer, T.; Mate, K.S.; Berman, A. The age-friendly health system imperative. J. Am. Geriatr. Soc. 2018, 66, 22–24. [Google Scholar] [CrossRef] [PubMed]
- Nurses Improving Care for Healthsystem Elders (NICHE). Available online: https://nicheprogram.org (accessed on 28 June 2018).
- Health Resources & Services Administration. Geriatrics Workforce Enhancement Program. Available online: https://bhw.hrsa.gov/fundingopportunities/default.aspx?id=9f260dcc-0978-4c96-8a57-e0a767840ef0w (accessed on 28 June 2018).
- Callahan, K.E.; Tumosa, N.; Leipzig, R.M. Big ‘G’ and Little ‘g’ Geriatrics Education for Physicians. J. Am. Geriatr. Soc. 2017, 65, 2313–2317. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Agency for Healthcare Research and Quality RM. TeamSTEPPS 2.0. Web Site. Available online: https://www.ahrq.gov/teamstepps/instructor/index.html (accessed on 25 March 2018).
- Rasin-Waters, D.; Abel, V.; Kearney, L.K.; Zeiss, A. The integrated care team approach of the Integrated of the Department of Veterans Affairs (VA): Geriatric Primary Care. Arch. Clin. Neuropsychol. 2018, 33, 280–289. [Google Scholar] [CrossRef] [PubMed]
| Study Characteristics | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Type | Randomized controlled, prospective or retrospective cohort, observational, case-control, implementation, feasibility, or quality improvement full-text studies with an intervention and comparator group | Descriptive studies of the ACE unit model or patient population without a comparator group Abstracts, dissertations, and book chapters |
| Population | Patients aged ≥ 65 years | Non-geriatric patient population |
| Intervention | Contains core components of ACE model (geriatric assessment and management by an interprofessional team consisting of at least three different healthcare professionals targeting comprehensive geriatric care) Intervention delivered on a hospital unit to which patient was admitted for an acute illness | Geriatric consult or co-management models of care Intervention included an outpatient component (i.e., home evaluation, follow-up in a geriatric clinic) Intervention designed to target only one diagnosis (i.e., delirium) and not comprehensive geriatric care Intervention delivered in a non-acute care unit setting (i.e., emergency department) or on a unit to which a patient was transferred for a rehabilitation focus after stabilization of an acute illness |
| Comparator Group | Usual/routine hospital care in a similar patient population on the same or similar type of unit or service | No comparator or usual/outline care group |
| Outcome Measures | Patient related geriatric care process, clinical, satisfaction, quality of life, or healthcare utilization outcomes | Staff or provider educational or perception outcomes |
| Language | English | Non-English |
| Publication date | 1995 or later | Prior to 1995 |
| Study (Setting) | Design | Patient Population (Mean Age of ACE Cohort) | ACE vs. UC Attending Physicians (Sample Sizes) | Primary Outcome Measured (ACE vs. UC) | Secondary Outcome(s) Measured (ACE vs. UC) | Study and/or Intervention Limitations | Study Strengths and/or Intervention Innovations |
|---|---|---|---|---|---|---|---|
| Landefeld et al., 1995 [4] (university hospital, USA) | RCT | General medical patients aged ≥ 70 years (80.2) | Internists on ACE (327) and UC (324) units | Significantly improved ADL performance from baseline (p = 0.05) and admission (p = 0.009) to discharge | Significantly reduced PACF placement (14% vs. 22 %, p = 0.01) Significantly improved overall health status (p < 0.001) at discharge No difference in hospital charges | Utilized charges for cost analysis | Randomized Improved outcomes in subgroup and multivariate analyses |
| Covinsky et al., 1997 [7] (university hospital, USA) | RCT; Cost analysis from Landefeld et al., study | General medical patients aged ≥ 70 years (80.7) | Internists on ACE (326) and UC (324) units | No significant reduction in total costs per case ($6608 vs. $7240, p = 0.93) | No significant reduction in LOS (7.5 vs. 8.4 days, p = 0.449) Significantly reduced 90-day PACF use (24.1% vs. 32.3%, p = 0.034) | Total costs includes indirect costs Lacked power to determine significance in cost difference | Randomized Included ACE start-up costs, likely under-estimating long-term cost savings |
| Stewart et al., 1999 [8] (community teaching hospital, USA) | Prospective observational | General medical or surgical patients aged ≥ 75 years (86) | Internist or Surgeon on ACE (34) and UC (27) units | No significant difference in LOS (6.0 vs. 7.1 days, p = 0.06) | Significantly reduced charges ($6,223 vs. $10,042, p < 0.01) | Non-randomized Multiple significantly different baseline characteristics between cohorts and results unadjusted Utilized charges for cost analysis | ACE care for medical and surgical patients |
| Counsell et al., 2000 [9] (community teaching hospital, USA) | RCT | Community-dwelling general medical patients with LOS ≥ 2 days aged ≥ 70 years (80) | Internist or Family Practice attending on ACE (767) and UC (764) units | No significant difference in ADL performance at discharge Significant reduction in composite outcome (ADL decline or PACF placement; 34% vs. 40%, p = 0.027) | Significant increased use of nursing care plans (79% vs. 50%; p = 0.001), SW consults (50% vs. 43%, p = 0.012), and PT consults (42% vs. 36%, p = 0.027) Significant reduction in restraint use (2% vs. 6%; p = 0.001) Improved patient, caregiver, and provider satisfaction | ADL outcome may have been influenced by healthier patient population and shorter LOS than Landefeld et al., RCT | Randomized Large sample size Studied ACE in patients not on a teaching service |
| Asplund et al., 2000 [10] (university hospital, Sweden) | RCT | General medical patients aged ≥ 70 years (80.9) | Internist initially followed by Geriatrician on ACE (190) vs. Internist on UC (223) units | No significant difference in poor global outcome measure α 3 months post-discharge (RR 1.06; 95% CI 0.84–1.34) | Significantly reduced LOS (5.9 vs. 7.3 days, p = 0.002) No difference in readmissions or healthcare utilization at 3 months No significant difference in hospital mortality (4% vs. 3%) | Per-protocol analysis performed since majority of ineligible patients were due to inappropriate randomization processes | Randomized Evaluated function and well-being post-discharge |
| Salvedt et al., 2002 [11] (university hospital, Norway) | RCT | General medical patients meeting frailty criteria aged ≥ 75 years (81.8) | Geriatrician on ACE (127) vs. Internist or Medical Subspecialists on UC (127) units | Significantly reduced mortality at 3 (12% vs. 27%, p = 0.004) and 6 months (16% vs. 29%, p = 0.02) post-discharge | Significantly increased LOS (15 vs. 7 days, p < 0.001) Significantly more ACE patients with dementia, depression, and delirium diagnoses documented (38% vs. 7%, p < 0.001) | Non-USA based study may have influenced LOS Some ACE patients were transferred from other units | Randomized Targeted frail patients First to evaluated mortality as a primary outcome |
| Naglie et al., 2002 [12] (university hospital, Canada) | RCT | Patients with surgical hip fracture repair aged ≥ 70 years (83.8) | Geriatrician directed medical care on Ortho-ACE (141) vs. Internist directed medical care on Ortho-UC (138) units | No significant difference in composite outcome (% patients alive with no decline from baseline in ambulation, transfers, or place of residence 6 months post-surgery; adjusted OR 1.1, 95% CI 0.6–2.1) | Significant increase in % patients with composite outcome (alive with no decline from baseline in ambulation, transfers, or place of residence at 6 months) in analysis of cognitively impaired patients (47% vs. 24%, p = 0.03) Significantly increased LOS (29.2 vs. 20.9 days, p < 0.001) | Non-USA based study may have influenced LOS Did not evaluate in-hospital outcomes | Randomized design Extension of ACE to orthopedic surgery patients Twice weekly ACE rounds |
| Allen et al., 2003 [13] (community teaching hospital, USA) | Pre/post comparison | Acute stroke patients pre/post launch of ACE-like stroke unit; no age criteria reported (72) | Neurologist 1-year pre (622) vs. 1-year post (544) stroke unit utilizing ACE model | Significantly reduced LOS (3.8 vs. 4.6 days, p < 0.0001) | Significantly more patients discharged home (62% vs. 50%, p < 0.0001) Significantly increased proportion of patients without a readmission at 1-year (41% vs. 18%, p < 0.0001) Significantly reduced health system Medicare stroke-specific and risk-adjusted inpatient mortality (11.4% vs. 8.4%, p = 0.02) No significant difference in all-cause mortality (7% vs. 16%; p = 0.11) | Non-randomized Data from administrative database | ACE team model and processes used to develop an acute stroke unit |
| Jayadevappa et al., 2006 [14] (university hospital, USA) | Retrospective case-control | General medical patients admitted for CHF, UTI, or pneumonia aged ≥ 65 years (79.6) | Internist or Geriatrician on ACE (680) vs. Internist on UC (680) units | Significantly reduced LOS (4.9 vs. 5.9, p = 0.01) Significantly reduced mean costs ($13,586 vs. $15,039, p = 0.012) | Reduced annual readmissions after controlling for age, race, comorbidities, and number of prior admissions | Non-randomized Data from administrative database Costs estimated from a cost-to-charge ratio | Adjusted for prior admissions in analyzing readmission rate |
| Zelada et al., 2009 [15] (military teaching hospital, Peru) | Prospective observational | General medical patients aged ≥ 65 years (79.6) | Geriatrician on ACE (68) vs. Internist on UC (75) units | Significantly reduced ADL decline during hospitalization (19% vs. 40%, p = 0.013) | Increased OR for ADL decline in UC patients (4.24; 95% CI 1.50–11.9) Reduced LOS on ACE (7.5 vs. 9.92 days, p = 0.03) | Non-randomized Multiple significantly different baseline characteristics between cohorts | Once weekly ACE rounds |
| Malone et al., 2010 [16] (community hospital, USA) | Pre/post comparison | General medical or urology patients aged ≥ 65 years (no mean age reported) | Urology or Internist on medical-surgical units pre (478) vs. post (406) e-Geriatrician | Significantly reduced use of urinary catheters (26.2 vs. 20.1%, p = 0.03) Significantly increased physical therapy referrals (27.0% vs. 39.1%; p < 0.001) | No significant difference in use of physical restraints, social service assessments, high-risk medications, LOS, or 30-day readmissions | Non-randomized No formal tracking of whether recommendations made by geriatricians are followed | Use of EMR tool to disseminate ACE care Twice weekly e-Geriatrician in ACE rounds |
| Flood et al., 2011 [17] (university hospital, USA) | Retrospective chart review | Hematology-oncology patients with nutritional deficits aged ≥ 65 years (75.25) | Private Oncologist or Teaching attending with residents on Oncology-ACE (103) vs. UC (82) units | Significantly increased OR for receiving a formal nutrition consult (2.1, 95% CI 1.033–4.300) and nutritional supplements ordered (2.5; 95% CI 1.221–5.319) in adjusted analysis | Significantly increased proportion of patients receiving a nutrition consult (63.1% vs. 45.1%, p = 0.011) and an order for supplements (57.3% vs. 32.9%, p = 0.001) in unadjusted analysis | Non-randomized No standardized nutritional risk screening process on units Significantly more OACE cohort with low BMI No clinical outcomes measured | Extension of ACE model to hematology/oncology patients Evaluated role of ACE on nutritional processes of care |
| Barnes et al., 2012 [18] (university hospital, USA) | RCT (2nd RCT from same ACE unit in Landefeld et al., study) | Community-dwelling general medical patients aged ≥ 70 years (81) | Internists on ACE (858) and UC (774) units | Significantly reduced LOS (6.7 vs. 7.3 days, p = 0.004) Significantly reduced cost per patient ($9,477 vs. $10,451, p < 0.001) | No significant difference in ADL, IADL, or mobility performance at discharge | Gap between time study conducted (1993–1997) and publication (2012) | Randomized Large sample size |
| Ahmed, et al., 2012 [19] (university hospital, USA) | Pre/post comparison | General medical patients aged ≥ 70 years (no mean age reported) | Geriatrician or Geriatric Consultant with Private Internist post (1096) vs. Private and Teaching Internist on UC (383) 1-year pre-ACE | Significant reduction in LOS (5.55 vs. 7.76 days; p = 0.001) and CMI adjusted LOS (5.16 vs. 6.40; p = 0.007) year 2 vs. baseline | No significant difference in direct costs Reduced readmission rate from baseline to years 1 and 2 combined (14.04% vs. 11.95%; no statistical analysis performed) | Non-randomized Baseline patients from multiple different units Unequal sample sizes and time periods in pre- vs. post-cohorts | Measured CMI adjusted LOS Measured direct costs |
| Perez-Zepeda et al., 2012 [6] (community hospitals, Mexico) | Prospective matched cohort | General medical patients with ≥ 1 targeted geriatric syndrome aged ≥ 60 years (72.6) | Geriatricians on ACE (70) vs. Internist on UC (140) units | Significantly lower adjusted OR of composite outcome (presence of ADL decline, pressure ulcer, delirium, or death; 0.27; 95% CI 0.10–0.70) | Significantly reduced OR for ADL decline (0.23; 95% CI 0.08–0.65) No significant difference in LOS (9.9 vs. 9.3 days, p = NS) No significant difference in adjusted OR for hospital mortality (1.50; 95% CI 0.31–7.18) | Non-randomized Small sample sizes for two-year study recruitment period | Targeted patients with existing geriatric syndromes |
| Flood et al., 2013 [20] (university hospital, USA) | Retrospective cohort | General medical patients aged ≥ 70 years (81.6) | Hospitalists on ACE (428) and UC (390) units | Significantly reduced variable direct costs ($2109 vs. $2480, p = 0.009) | Significantly reduced 30-day readmissions (7.9% vs. 12.8%, p = 0.02) No significant difference in discharge destination (p = 0.12) including death in hospital 1.4% vs. 1.8%) | Non-randomized Data from administrative database | Units had same attendings Measured variable direct costs Reduced costs despite short LOS |
| Borenstein, et al., 2016 [21] (university hospital, USA) | Cluster RCT of hospital units | General medical patients with geriatric risk factors aged ≥ 65 years (81.1) | Internist on medical units with (792) and without (592) ACE training and workflow redesign | Observed:Expected LOS ratio < 1 with ACE intervention and >1 on UC | Significantly reduced adjusted OR of any complication (0.45, 95% CI 0.21–0.98; p = 0.043) or transfer to ICU (0.45; 95% CI 0.25–0.79; p = 0.006) Significantly increased adjusted OR of discharge to PACF (1.43, 95% CI 1.06-1.93; p = 0.021) No significant difference in adjusted OR of hospital mortality (0.69, 95% CI 0.42–1.15; p = 0.16) | Non-randomized Amount of uptake of NICHE care protocols on control units unknown | Large sample size Redesigned workflows of all unit personnel to include ACE care processes |
| Ekerstad et al., 2017 [22] (community hospital, Sweden) | Prospective controlled | General medical patients with positive frailty screen aged ≥ 75 years (85.7) | Internist, Family Practitioner, and/or Geriatricians on ACE (206) vs. Internist on UC (202) units | Significantly reduced adjusted OR of decline in HRQOL (vision, ambulation, dexterity, emotion, cognition, pain dimensions) 3 months post-discharge | Significantly reduced 30-day readmission (19% vs. 28%, p = 0.048) Reduced adjusted 3-month mortality (HR 0.55, 95% CI 0.32–0.96) No significant difference in hospital mortality (4% vs. 5%, p = 0.6) | Reports trial is randomized but patients assigned to ACE or UC based on bed availability | Targeted older frail patients Evaluated quality of life |
| Booth et al., 2018 [23] (university hospital, USA) | Pre/post comparison | Orthopedic surgery or medical patients aged ≥ 65 years (74.4) | Orthopedic Surgeon or Hospitalist pre (48) vs. post (113) ACE workflow redesign | Significantly improved completion of geriatric screens for ADL (62.5% vs. 88.5%, p < 0.001) and delirium (4.2% vs. 96.5%, p < 0.001) | Significantly increased patients mobilized bed to chair (36.4% vs. 63.5%, p < 0.05) No significant difference in patients ambulating in hallway or delirium prevalence | Non-randomized Small and unequal sample sizes/time periods in cohorts limits ability to measure significance | Extension of ACE to orthopedic surgery patients Extension of ACE without geriatric specialist |
| Study (Setting) | Design | Patient Population (Mean Age of ACE Cohort) | ACE vs. UC Attending Physicians (Sample Sizes) | Primary Outcome Measured (ACE vs. UC) | Secondary Outcome(s) Measured (ACE vs. UC) | Study and/or Intervention Limitations | Study Strengths and/or Intervention Innovations |
|---|---|---|---|---|---|---|---|
| Wald et al., 2011 [24] (university hospital, USA) | Retro-spective chart review of patients randomized at time of admission | General medical patients aged ≥ 70 years (80.5) | Hospitalist on ACE (122) vs. Hospitalist or General or Subspecialty Internist on UC (95) services | Significantly increased patients with documented recognition and treatment plan for functional (68.9% vs. 35.8%, p < 0.0001) and cognitive impairment (55.7% vs. 40%, p = 0.02) Significantly increased patients with DNAR orders (39.3% vs. 26.3%, p = 0.04) | No significant differences in use of physical restraints, sleep aids, falls, discharge location, LOS, charges, or 30-day readmissions | Hospitalist-ACE attendings rotated on UC services Intervention did not include geriatric training for nurses LOS and 30-day readmission rates low at baseline, limiting ability to improve | 30% of ACE patients located off unit and received ACE care Hospitalist-ACE delivered geriatric training to residents Extension of ACE without geriatric specialist |
| Yoo et al., 2013 [25] (university hospital, USA) | Prospective matched cohort | Community-dwelling general medical patients aged ≥ 65 years (no mean age reported; 43% of patients aged ≥ 80) | Internist on ACE (236) and UC (248) services | No significant difference delirium prevalence (23% vs. 21%, p = 0.34) | Significantly reduced LOS (6.1 vs. 6.8 days, p = 0.008) No significant difference in 30-day readmissions | Non-randomized Per-protocol and not intention-to-treat analysis UC physicians received geriatric education | Extension of ACE without geriatric specialist |
| Hung et al., 2013 [26] (university hospital, USA) | Prospective matched cohort | General medical patients aged ≥ 75 years (85.2) | Geriatrician on ACE (173) vs. Internist on UC (173) services | No significant difference in 30-day readmissions (15.4% vs. 22.4%, p = 0.21) Significantly fewer patients experiencing an adverse event (CAUTI, restraint use, fall, or pressure ulcer; 9.5% vs. 17.1%, p = 0.02) Significantly reduced LOS (4.6 vs. 6.8 days, p = 0.001) | Significantly improved 3-item CTM mean score (72.5 vs. 64.9, p = 0.01) No significant difference in discharge location, ADL or IADL performance 30 days post-discharge, overall health status, or HCAHPS top box satisfaction scores No significant difference in 30-day mortality (7.5% vs. 5.8%, p = 0.51) | Non-randomized ACE service only admitted patients receiving primary care in geriatric patient-centered medical home | Service includes geriatrician attending with allocated social worker and clinical nurse specialist |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Flood, K.L.; Booth, K.; Vickers, J.; Simmons, E.; James, D.H.; Biswal, S.; Deaver, J.; White, M.L.; Bowman, E.H. Acute Care for Elders (ACE) Team Model of Care: A Clinical Overview. Geriatrics 2018, 3, 50. https://doi.org/10.3390/geriatrics3030050
Flood KL, Booth K, Vickers J, Simmons E, James DH, Biswal S, Deaver J, White ML, Bowman EH. Acute Care for Elders (ACE) Team Model of Care: A Clinical Overview. Geriatrics. 2018; 3(3):50. https://doi.org/10.3390/geriatrics3030050
Chicago/Turabian StyleFlood, Kellie L., Katrina Booth, Jasmine Vickers, Emily Simmons, David H. James, Shari Biswal, Jill Deaver, Marjorie Lee White, and Ella H. Bowman. 2018. "Acute Care for Elders (ACE) Team Model of Care: A Clinical Overview" Geriatrics 3, no. 3: 50. https://doi.org/10.3390/geriatrics3030050





