Acupoint Activation: Response in Microcirculation and the Role of Mast Cells
Abstract
:1. Introduction
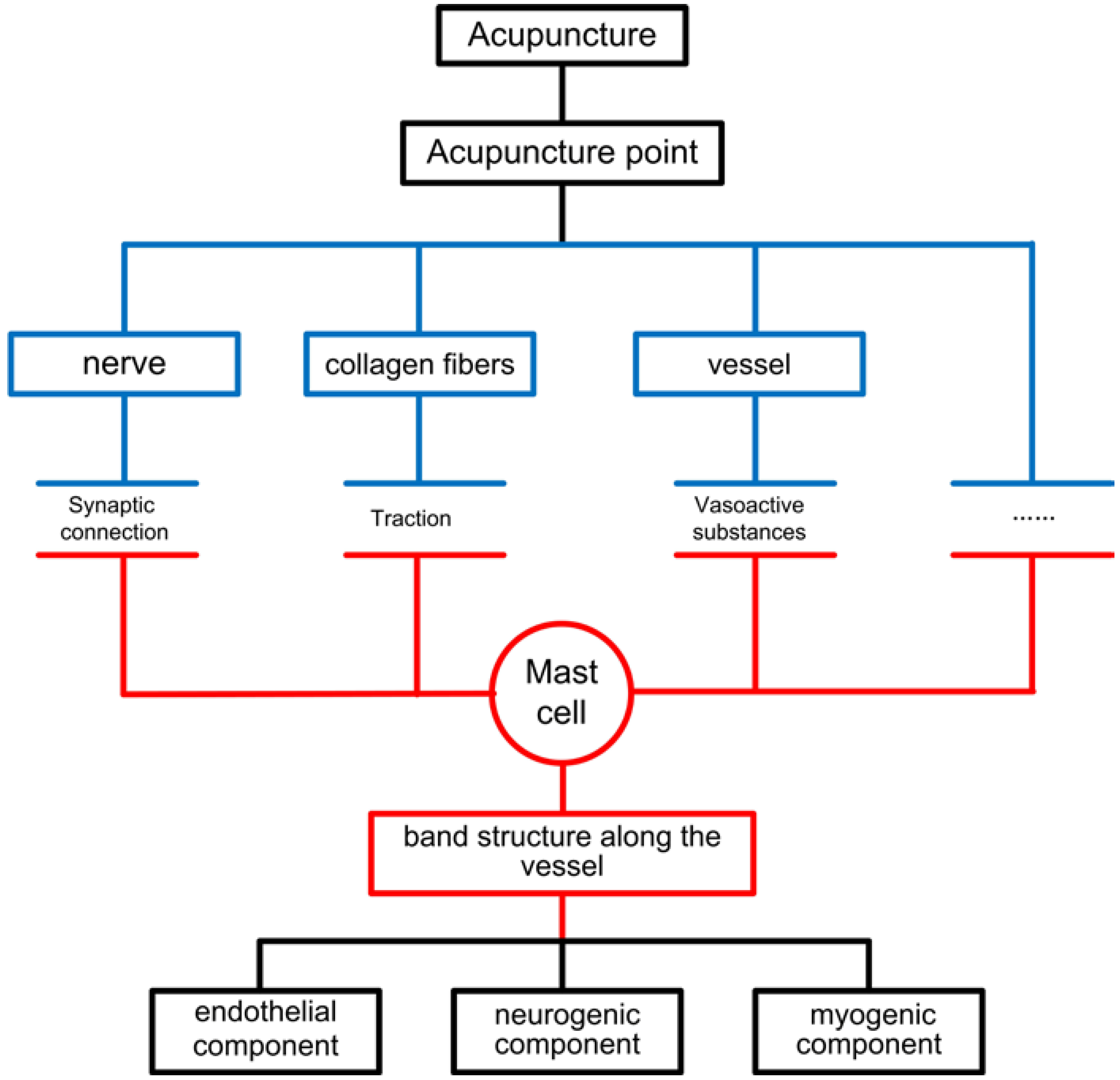
2. Acupoint Stimulation and Corresponding Response in Microcirculation
3. Mast Cells Play an Important Role in Acupoint Activation and Microcirculatory Response
4. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Wang, G.J.; Ayati, M.H.; Zhang, W.B. Meridian studies in China: A systematic review. J. Acupunct. Meridian Stud. 2010, 3, 1–9. [Google Scholar] [PubMed]
- Su, Y.S.; Yang, Z.K.; Xin, J.J.; He, W.; Shi, H.; Wang, X.Y.; Hu, L.; Jing, X.H.; Zhu, B. Somatosensory nerve fibers mediated generation of De-qi in manual acupuncture and local moxibustion-like stimuli-modulated gastric motility in rats. Evid. Based Complement. Alternat. Med. 2014. [Google Scholar] [CrossRef]
- Zhu, S.P.; Luo, L.; Zhang, L.; Shen, S.X.; Ren, X.X.; Guo, M.W.; Yang, J.M.; Shen, X.Y.; Xu, Y.S.; Ji, B. Acupuncture De-qi: From characterization to underlying mechanism. Evid. Based Complement. Alternat. Med. 2013, 2013, 518784. [Google Scholar] [PubMed]
- Yu, D.T.; Jones, A.Y. Physiological changes associated with de qi during electroacupuncture to LI4 and LI11: A randomised, placebo-controlled trial. Acupunct. Med. 2013, 31, 143–150. [Google Scholar] [CrossRef] [PubMed]
- Lundeberg, T. To be or not to be: The needling sensation (De qi) in acupuncture. Acupunct. Med. 2013, 31, 129–131. [Google Scholar]
- Leung, A.Y.; Park, J.; Schulteis, G.; Duann, J.R.; Yaksh, T. The electrophysiology of de qi sensations. J. Altern. Complement. Med. 2006, 12, 743–750. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.R.; Li, G.L.; Zhang, G.F.; Huang, Y.; Wang, S.X.; Lu, N. Brain areas involved in acupuncture needling sensation of De qi: A single-photon emission computed tomography (SPECT) study. Acupunct. Med. 2012, 30, 316–323. [Google Scholar] [CrossRef] [PubMed]
- Zhuo, L.S. Discussion of relation between acupuncture methods and the directions of qi in meridians. Chin. Acupunct. Moxib. 2011, 31, 846–849. [Google Scholar]
- Lai, X.S.; Tong, Z. A study on the classification and the “catching” of the “arrived qi” in acupuncture. J. Tradit. Chin. Med. 2010, 30, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Park, J.E.; Ryu, Y.H.; Liu, Y.; Jung, H.J.; Kim, A.R.; Jung, S.Y.; Choi, S.M. A literature review of de qi in clinical studies. Acupunct. Med. 2013, 31, 132–142. [Google Scholar] [CrossRef] [PubMed]
- Litscher, G.; Wang, L.; Huber, E.; Nilsson, G. Changed skin blood perfusion in the fingertip following acupuncture needle introduction as evaluated by Laser Doppler Perfusion Imaging. Laser Med. Sci. 2002, 17, 19–25. [Google Scholar]
- Hsiu, H.; Hsu, W.C.; Chang, S.L.; Hsu, C.L.; Huang, S.M.; Lin, Y.Y.W. Microcirculatory effect of different skin contacting pressures around the blood pressure. Physiol. Meas. 2008, 29, 1421–1434. [Google Scholar] [PubMed]
- Litscher, G. Bioengineering assessment of acupuncture, part 2: Monitoring of microcirculation. Crit. Rev. Biomed. Eng. 2006, 34, 273–294. [Google Scholar] [CrossRef] [PubMed]
- Rezaei, S.; Khorsand, A.; Jamali, J. Characterisation of human skin impedance at acupuncture point PC4 Ximen and pericardium meridian using the four-electrode method. Acupunct. Med. 2012, 30, 127–131. [Google Scholar] [CrossRef] [PubMed]
- Ahn, A.C.; Park, M.; Shaw, J.R.; McManus, C.A.; Kaptchuk, T.J.; Langevin, H.M. Electrical impedance of acupuncture meridians: The relevance of subcutaneous collagenous bands. PLoS One 2010, 5. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.B.; Tian, Y.Y.; Li, H.; Tian, J.H.; Luo, M.F.; Xu, F.L.; Wang, G.J.; Huang, T.; Xu, Y.H.; Wang, R.H. A discovery of low hydraulic resistance channel along meridians. J. Acupunct. Meridian Stud. 2008, 1, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Li, H.Y.; Yang, J.F.; Chen, M.; Xu, L.; Wang, W.C.; Wang, F.; Tong, J.B.; Wang, C.Y. Visualized regional hypodermic migration channels of interstitial fluid in human beings: are these ancient meridians? J. Altern. Complement. Med. 2008, 14, 621–628. [Google Scholar] [CrossRef]
- Li, H.Y.; Chen, M.; Yang, J.F.; Yang, C.Q.; Xu, L.; Wang, F.; Tong, J.B.; Lv, Y.; Suonan, C. Fluid flow along venous adventitia in rabbits: Is it a potential drainage system complementary to vascular circulations? PLoS One 2012, 7. [Google Scholar] [CrossRef]
- Yao, W.; Li, Y.; Ding, G. Interstitial fluid flow: The mechanical environment of cells and foundation of meridians. Evid. Based Complement. Alternat. Med. 2012. [Google Scholar] [CrossRef]
- Hsieh, C.L.; Chang, Y.M.; Tang, N.Y.; Lin, I.H.; Liu, C.H.; Lin, J.G.; Jin, R. Time course of changes in nail fold microcirculation induced by acupuncture stimulation at the Waiguan acupoints. Am. J. Chin. Med. 2006, 34, 777–785. [Google Scholar] [CrossRef] [PubMed]
- Hsiu, H.; Huang, S.M.; Chao, P.T.; Jan, M.Y.; Hsu, T.L.; Wang, W.K.; Wang, Y.Y.L. Microcirculatory characteristics of acupuncture points obtained by laser Doppler flowmetry. Physiol. Meas. 2007, 28, N77–N86. [Google Scholar] [CrossRef] [PubMed]
- Niimi, H.; Yuwono, H.S. Asian traditional medicine: from molecular biology to organ circulation. Clin. Hemorheol. Microcirc. 2000, 23, 123–125. [Google Scholar] [PubMed]
- Tsuru, H.; Kawakita, K. Acupuncture on the blood flow of various organs measured simultaneously by colored microspheres in rats. Evid. Based Complement. Alternat. Med. 2009, 6, 77–83. [Google Scholar] [CrossRef] [PubMed]
- Hsiu, H.; Hsu, W.C.; Chen, B.H.; Hsu, C.L. Differences in the microcirculatory effects of local skin surface contact pressure stimulation between acupoints and nonacupoints: Possible relevance to acupressure. Physiol. Meas. 2010, 31, 829–841. [Google Scholar] [CrossRef] [PubMed]
- Hsiu, H.; Hsu, W.C.; Hsu, C.L.; Jan, M.Y.; Wang-Lin, Y.Y. Effects of acupuncture at the Hoku acupoint on the pulsatile laser Doppler signal at the heartbeat frequency. Laser Med. Sci. 2009, 24, 553–560. [Google Scholar] [CrossRef]
- Sandberg, M.L.; Sandberg, M.K.; Dahl, J. Blood flow changes in the trapezius muscle and overlying skin following transcutaneous electrical nerve stimulation. Phys. Ther. 2007, 87, 1047–1055. [Google Scholar] [CrossRef] [PubMed]
- Kuo, T.C.; Chen, Z.S.; Chen, C.H.; Ho, F.M.; Lin, C.W.; Chen, Y.J. The physiological effect of DE QI during acupuncture. J. Health Sci. 2004, 50, 336–342. [Google Scholar] [CrossRef]
- Kuo, T.C.; Lin, C.W.; Ho, F.M. The soreness and numbness effect of acupuncture on skin blood flow. Am. J. Chin. Med. 2004, 32, 117–129. [Google Scholar] [PubMed]
- Bernardi, L.; Rossi, M.; Fratino, P.; Finardi, G.; Mevio, E.; Orlandi, C. Relationship between phasic changes in human skin blood flow and autonomic tone. Microvasc. Res. 1989, 37, 16–27. [Google Scholar] [CrossRef] [PubMed]
- Kvandal, P.; Landsverk, S.A.; Bernjak, A.; Stefanovska, A.; Kvernmo, H.D.; Kirkeboen, K.A. Low-frequency oscillations of the laser Doppler perfusion signal in human skin. Microvasc. Res. 2006, 72, 120–127. [Google Scholar] [CrossRef] [PubMed]
- Hsiu, H.; Hsu, W.C.; Hsu, C.L.; Huang, S.M. Assessing the effects of acupuncture by comparing needling the hegu acupoint and needling nearby nonacupoints by spectral analysis of microcirculatory laser Doppler signals. Evid. Based Complement. Alternat. Med. 2011. [Google Scholar] [CrossRef]
- Zhang, Y.Q.; Ding, Y.L.; Tian, Y.Y.; Huang, T.; Zhang, W.B.; Wang, G.J. Change of blood perfusion on contra-lateral lower limb after electro-Bian stone intervention. Jiangsu J. Trad. Chin. Med. 2010, 42, 48–49. [Google Scholar]
- Wang, G.J.; Zhang, Y.Q.; Wang, R.H.; Ding, Y.L.; Tian, Y.Y.; Huang, T.; Zhang, W.B. The study of interaction based on the thermostimulation. Chin. J. Basic Med. Trad. Chin. Med. 2010, 16, 803–804. [Google Scholar]
- Hsiu, H.; Hsu, W.C.; Hsu, C.L.; Huang, S.M.; Hsu, T.L.; Wang, Y.Y. Spectral analysis on the microcirculatory laser Doppler signal of the acupuncture effect. Conf. Proc. IEEE Eng. Med. Biol. Soc. 2008. [Google Scholar] [CrossRef]
- Wang, G.; Tian, Y.; Jia, S.; Litscher, G.; Zhang, W. Evaluate laser needle effect on blood perfusion signals of contralateral hegu acupoint with wavelet analysis. Evid. Based Complement. Alternat. Med. 2012. [Google Scholar] [CrossRef]
- Li, X.; Li, Y.; Chen, J.; Zhou, D.; Liu, Y.; Li, Y.; Liu, J.; Guo, Y.; Guo, Y. The influence of skin microcirculation blood perfusion at zusanli acupoint by stimulating with lift-thrust reinforcing and reducing acupuncture manipulation methods on healthy adults. Evid. Based Complement. Alternat. Med. 2013. [Google Scholar] [CrossRef]
- Ji, S.M.; Yan, L. Mechanisms about the effect of different acupuncture manipulation methods on body temperature. Chin. Acupunct. Moxib. 2007, 27, 306–308. [Google Scholar]
- Huang, T.; Huang, X.; Zhang, W.; Jia, S.; Cheng, X.; Litscher, G. The influence of different acupuncture manipulations on the skin temperature of an acupoint. Evid. Based Complement. Alternat. Med. 2013. [Google Scholar] [CrossRef]
- Forssell, J.; Sideras, P.; Eriksson, C.; Malm-Erjefalt, M.; Rydell-Tormanen, K.; Ericsson, P.O.; Erjefalt, J.S. Interleukin-2-inducible T cell kinase regulates mast cell degranulation and acute allergic responses. Am. J. Respir. Cell. Mol. Biol. 2005, 32, 511–520. [Google Scholar] [CrossRef] [PubMed]
- Malaviya, R.; Ikeda, T.; Ross, E.; Abraham, S.N. Mast cell modulation of neutrophil influx and bacterial clearance at sites of infection through TNF-alpha. Nature 1996, 381, 77–80. [Google Scholar] [CrossRef] [PubMed]
- Echtenacher, B.; Mannel, D.N.; Hultner, L. Critical protective role of mast cells in a model of acute septic peritonitis. Nature 1996, 381, 75–77. [Google Scholar] [CrossRef] [PubMed]
- Lantz, C.S.; Boesiger, J.; Song, C.H.; Mach, N.; Kobayashi, T.; Mulligan, R.C.; Nawa, Y.; Dranoff, G.; Galli, S.J. Role for interleukin-3 in mast-cell and basophil development and in immunity to parasites. Nature 1998, 392, 90–93. [Google Scholar] [CrossRef] [PubMed]
- Gurish, M.F.; Austen, K.F. The diverse roles of mast cells. J. Exp. Med. 2001, 194, F1–F5. [Google Scholar] [CrossRef] [PubMed]
- Galli, S.J.; Nakae, S.; Tsai, M. Mast cells in the development of adaptive immune responses. Nat. Immunol. 2005, 6, 135–142. [Google Scholar] [CrossRef] [PubMed]
- Yao, W.; Yang, H.; Yin, N.; Ding, G. Mast cell-nerve cell interaction at acupoint: modeling mechanotransduction pathway induced by acupuncture. Int. J. Biol. Sci. 2014, 10, 511–519. [Google Scholar] [CrossRef] [PubMed]
- Sa, Z.Y.; Huang, M.; Zhang, D.; Ding, G.H. Relationship between regional mast cell activity and peripheral nerve discharges during manual acupuncture stimulation of “Zusanli” (ST 36). Acupunct. Res. 2013, 38, 118–122. [Google Scholar]
- Huang, H.; Zhan, R.; Yu, X.J.; Zhang, D.; Li, W.M.; Ding, G.H. Effects of acupoint-nerve block on mast cell activity, manual acupuncture- and electroacupuncture-induced analgesia in adjuvant arthritis rats. Acupunc. Res. 2009, 34, 31–35. [Google Scholar]
- Zhang, D.; Ding, G.H.; Shen, X.Y.; Yao, W.; Zhang, Z.Y.; Zhang, Y.Q.; Lin, J.Y. Influence of mast cell function on the analgesic effect of acupuncture of “Zusanli” (ST 36) in rats. Acupunc. Res. 2007, 32, 147–152. [Google Scholar]
- Zhang, W.B.; Zhao, Y.; Kjell, F. Understanding propagated sensation along meridians by volume transmission in peripheral tissue. Chin. J. Integr. Med. 2013, 19, 330–339. [Google Scholar] [CrossRef] [PubMed]
- Luo, M.F.; Dong, X.T.; Song, X.J.; Jiang, J.; Zhann, J.L.; Han, Y. Study on the dynamic compound structure composed of mast cells, blood vessels, and nerves in rat acupoint. Evid. Based Complement. Alternat. Med. 2013. [Google Scholar] [CrossRef]
- Furuno, T.; Ito, A.; Koma, Y.; Watabe, K.; Yokozaki, H.; Bienenstock, J.; Nakanishi, M.; Kitamura, Y. The spermatogenic Ig superfamily/synaptic cell adhesion molecule mast-cell adhesion molecule promotes interaction with nerves. J. Immunol. 2005, 174, 6934–6942. [Google Scholar] [CrossRef] [PubMed]
- Albuquerque, A.A.; Leal-Cardoso, J.H.; Weinreich, D. Role of mast cell- and non-mast cell-derived inflammatory mediators in immunologic induction of synaptic plasticity. Braz. J. Med. Biol. Res. 1997, 30, 909–912. [Google Scholar] [CrossRef] [PubMed]
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, G.; Litscher, D.; Tian, Y.; Gaischek, I.; Jia, S.; Wang, L.; Zhang, W.; Litscher, G. Acupoint Activation: Response in Microcirculation and the Role of Mast Cells. Medicines 2014, 1, 56-63. https://doi.org/10.3390/medicines1010056
Wang G, Litscher D, Tian Y, Gaischek I, Jia S, Wang L, Zhang W, Litscher G. Acupoint Activation: Response in Microcirculation and the Role of Mast Cells. Medicines. 2014; 1(1):56-63. https://doi.org/10.3390/medicines1010056
Chicago/Turabian StyleWang, Guangjun, Daniela Litscher, Yuying Tian, Ingrid Gaischek, Shuyong Jia, Lu Wang, Weibo Zhang, and Gerhard Litscher. 2014. "Acupoint Activation: Response in Microcirculation and the Role of Mast Cells" Medicines 1, no. 1: 56-63. https://doi.org/10.3390/medicines1010056





