Social Media Usage for Patients and Healthcare Consumers: A Literature Review
Abstract
:1. Introduction
1.1. Background
1.2. State-of-the Art & Aim
2. Materials and Methods
2.1. Criteria for Considering the Studies
2.2. Search Strategy
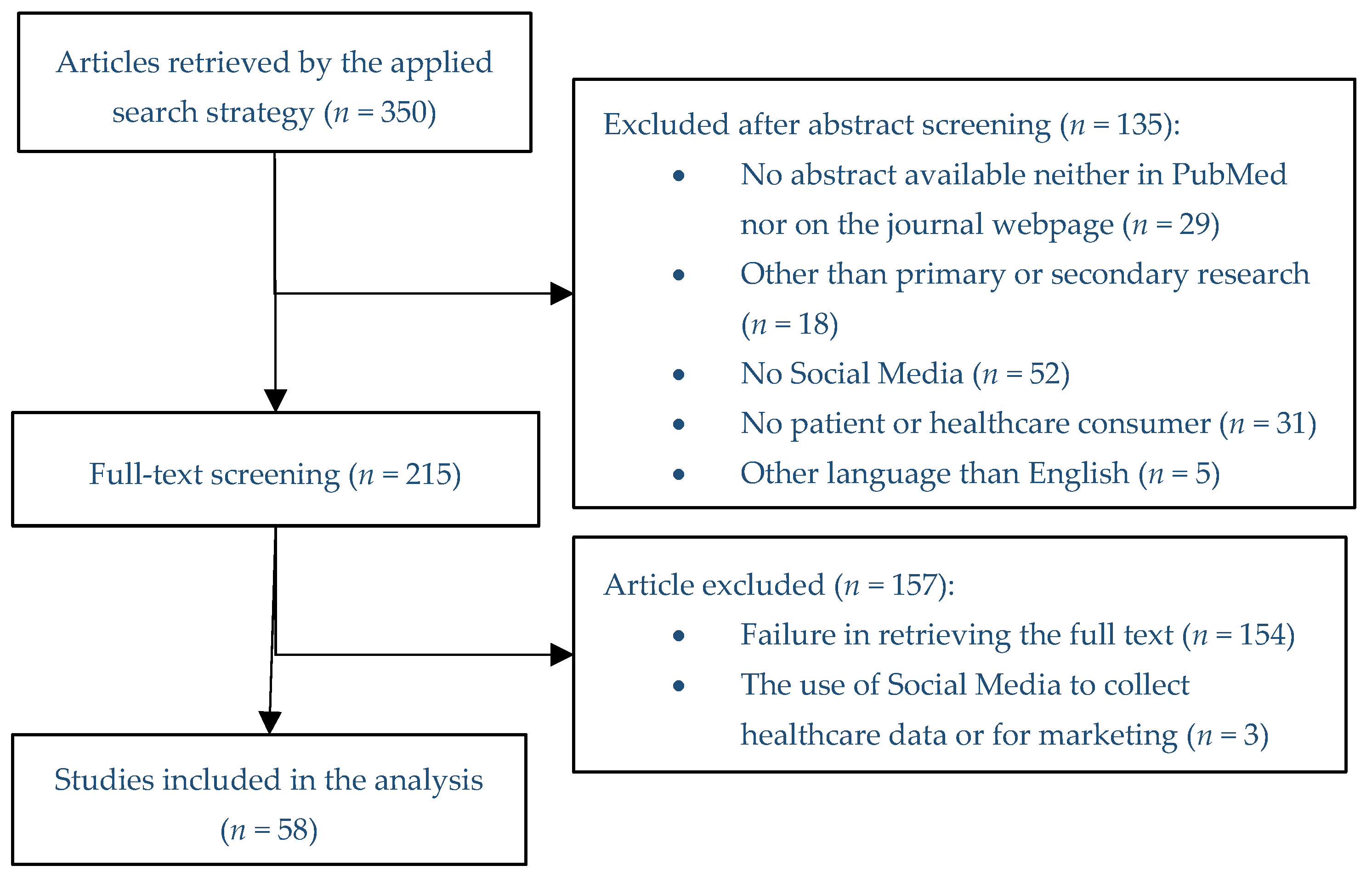
2.3. Selection of the Studies
2.4. Analysis
3. Results
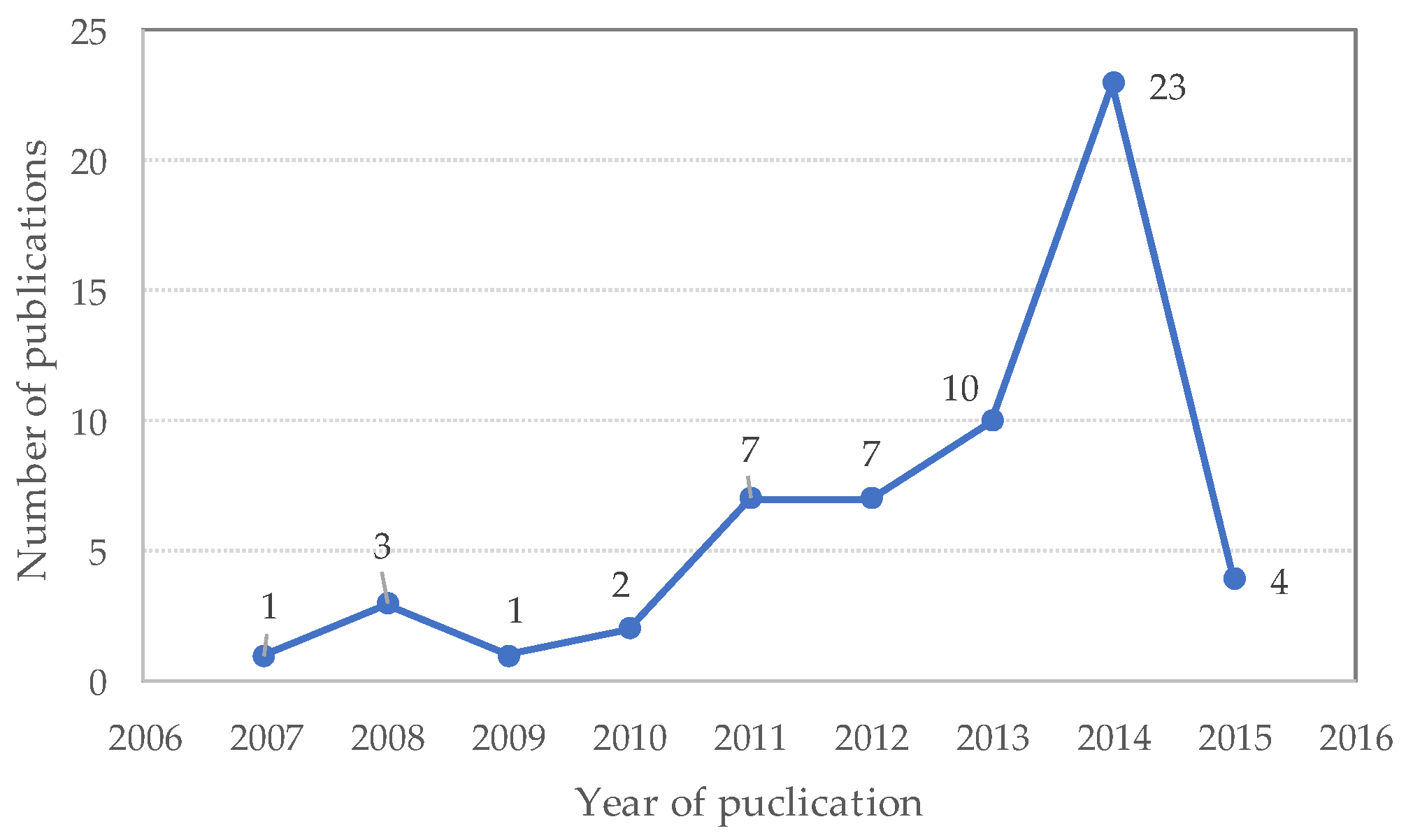
3.1. Eligible Studies
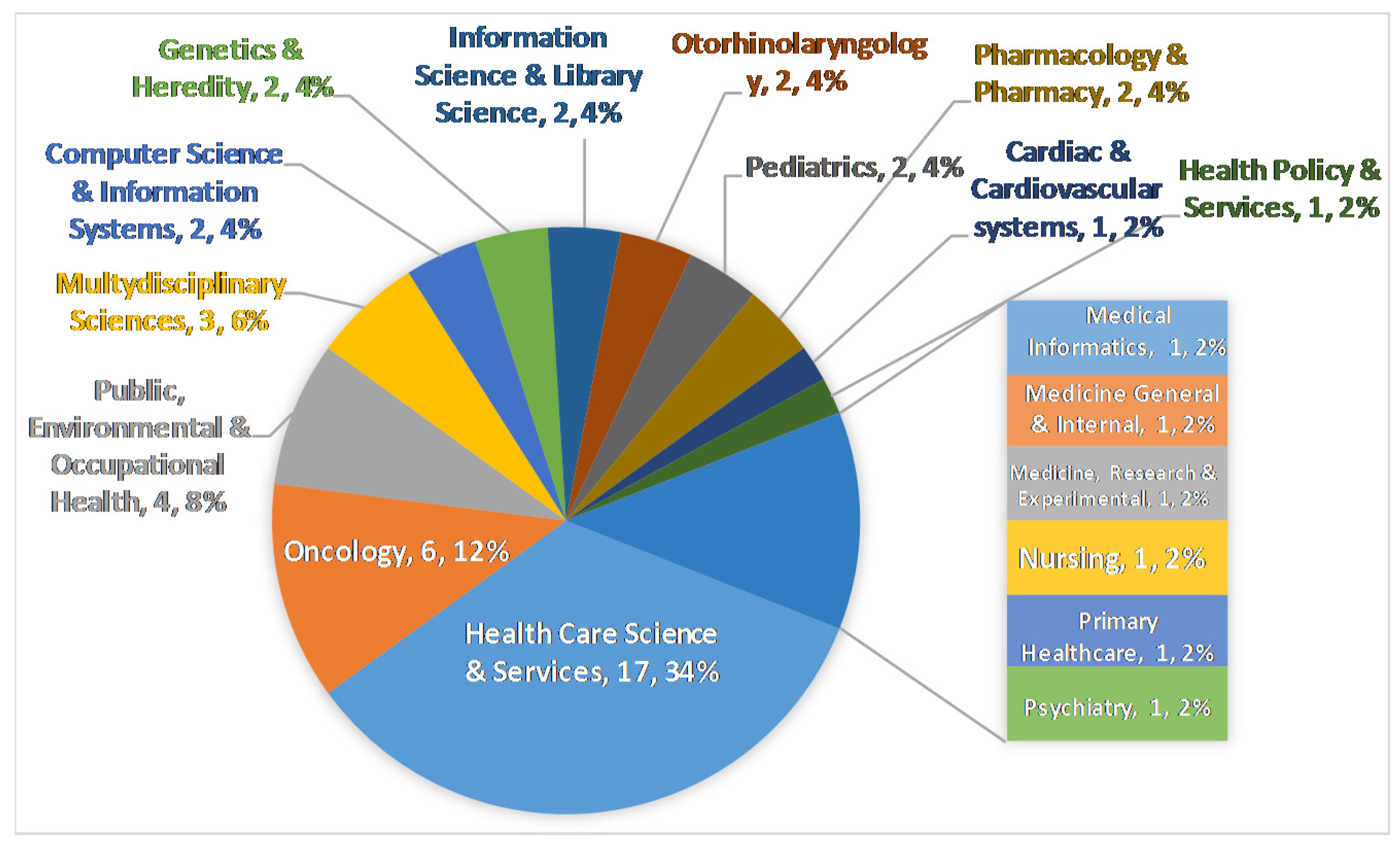
3.2. Analysis of Eligible Studies
4. Discussion
4.1. Network Characteristics
4.2. Influence Behavior
4.3. Medical Information
4.4. Study Limitations
4.5. Future Research Directions
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Hesse, B.; O’Connell, M.; Augustson, E.; Chou, W.; Shaikh, A.; Rutten, L. Realizing the promise of Web 2.0: Engaging community intelligence. J. Health Commun. 2011, 16, 10–31. [Google Scholar] [CrossRef] [PubMed]
- Reis, S.; Visser, A.; Frankel, R. Health information and communication technology in healthcare communication: The good, the bad, and the transformative. Patient Educ. Couns. 2013, 93, 359–362. [Google Scholar] [CrossRef] [PubMed]
- Van De Belt, T.; Engelen, L.; Berben, S.; Schoonhoven, L. Definition of Health 2.0 and Medicine 2.0: A systematic review. J. Med. Internet Res. 2010, 12, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Adams, S. Revisiting the online health information reliability debate in the wake of “web 2.0”: An inter-disciplinary literature and website review. Int. J. Med. Inform. 2010, 79, 391–400. [Google Scholar] [CrossRef] [PubMed]
- Smith, C. Consumer language, patient language, and thesauri: A review of the literature. J. Med. Libr. Assoc. 2011, 99, 135–144. [Google Scholar] [CrossRef] [PubMed]
- Finch, T.; Mort, M.; May, C.; Mair, F. Telecare: Perspectives on the changing role of patients and citizens. J. Telemed. Telecare 2005, 11, 51–53. [Google Scholar] [CrossRef] [PubMed]
- Kelly, L.; Jenkinson, C.; Ziebland, S. Measuring the effects of online health information for patients: Item generation for an e-health impact questionnaire. Patient Educ. Couns. 2013, 93, 433–438. [Google Scholar] [CrossRef] [PubMed]
- Ziebland, S.; Wyke, S. Health and illness in a connected world: How might sharing experiences on the internet affect people’s health? Milbank Q. 2012, 90, 219–249. [Google Scholar] [CrossRef] [PubMed]
- Knight, E.; Werstine, R.; Rasmussen-Pennington, D.; Fitzsimmons, D.; Petrella, R. Physical therapy 2.0: Leveraging social media to engage patients in rehabilitation and health promotion. Phys. Ther. 2015, 95, 389–396. [Google Scholar] [CrossRef] [PubMed]
- Hamm, M.; Shulhan, J.; Williams, G.; Milne, A.; Scott, S.; Hartling, L. A systematic review of the use and effectiveness of social media in child health. BMC Pediatr. 2014, 14, 138. [Google Scholar] [CrossRef] [PubMed]
- Devi, S. Facebook friend request from a patient? Lancet 2011, 377, 1141–1142. [Google Scholar]
- Street, J.; Braunack-Mayer, A.; Facey, K.; Ashcroft, R.; Hiller, J. Virtual community consultation? Using the literature and weblogs to link community perspectives and health technology assessment. Health Expect. 2008, 11, 189–200. [Google Scholar] [CrossRef] [PubMed]
- Heilman, J.; Kemmann, E.; Bonert, M.; Chatterjee, A.; Ragar, B.; Beards, G.; Iberri, D.; Harvey, M.; Grover, S.; Lodge, D. Wikipedia: A key tool for global public health promotion. J. Med. Internet Res. 2011, 13, e14. [Google Scholar] [CrossRef] [PubMed]
- Leithner, A.; Maurer-Ertl, W.; Glehr, M.; Friesenbichler, J.; Leithner, K.; Windhager, R. Wikipedia and osteosarcoma: A trustworthy patients’ information? J. Am. Med. Inform. Assoc. 2010, 17, 373–374. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.; The Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 7, e1000097. [Google Scholar]
- Kaplan, A.M.; Haenlein, M. Users of the world, unite! The challenges and opportunities of Social Media. Bus. Horiz. 2010, 53, 59–68. [Google Scholar] [CrossRef]
- Hamm, M.; Chisholm, A.; Shulhan, J.; Milne, A.; Scott, S.; Given, L.; Hartling, L. Social media use among patients and caregivers: A scoping review. BMJ Open 2013, 3, e002819. [Google Scholar] [CrossRef] [PubMed]
- Canese, K.; Weis, S. PubMed: The Bibliographic Database. In The NCBI Handbook [Internet], 2nd ed.; National Center for Biotechnology Information (US): Bethesda, MD, USA, 2013. [Google Scholar]
- Popay, J.; Roberts, H.; Sowden, A.; Petticrew, M.; Arai, L.; Rodgers, M.; Britten, N.; Roen, K.; Duffy, S. Guidance on the conduct of narrative synthesis in systematic reviews. A product from the ESRC Methods Programme Version. Prod. ESRC Method Program. Version 2006, 1, 1–92. [Google Scholar]
- Jäntschi, L.; Bolboacă, S. Exact Probabilities and Confidence Limits for Binomial Samples: Applied to the Difference between Two Proportions. Sci. World J. 2010, 10, 865–878. [Google Scholar] [CrossRef] [PubMed]
- Hale, T.; Pathipati, A.; Zan, S.; Jethwani, K. Representation of health conditions on Facebook: Content analysis and evaluation of user engagement. J. Med. Internet Res. 2014, 16, e182. [Google Scholar] [CrossRef] [PubMed]
- Laurent, M.R.; Vickers, T. Seeking health information online: Does Wikipedia matter? J. Am. Med. Inform. Assoc. 2009, 16, 471–479. [Google Scholar] [CrossRef] [PubMed]
- Seltzer, E.; Stolley, M.; Mensah, E.; Sharp, L. Social networking site usage among childhood cancer survivors—A potential tool for research recruitment? J. Cancer Surviv. 2014, 8, 349–354. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Chung, D. Characteristics of cancer blog users. J. Med. Libr. Assoc. 2007, 95, 445–450. [Google Scholar] [CrossRef] [PubMed]
- Neal, D.; McKenzie, P. Putting the pieces together: Endometriosis blogs, cognitive authority, and collaborative information behavior. J. Med. Libr. Assoc. 2011, 99, 127–134. [Google Scholar] [CrossRef] [PubMed]
- Pant, S.; Deshmukh, A.; Murugiah, K.; Kumar, G.; Sachdeva, R.; Mehta, J. Assessing the credibility of the “YouTube approach” to health information on acute myocardial infarction. Clin. Cardiol. 2012, 35, 281–285. [Google Scholar] [CrossRef] [PubMed]
- Biggs, T.; Bird, J.; Harries, P.; Salib, R. YouTube as a source of information on rhinosinusitis: The good, the bad and the ugly. J. Laryngol. Otol. 2013, 127, 749–754. [Google Scholar] [CrossRef] [PubMed]
- Stamelou, M.; Edwards, M.; Espay, A.; Fung, V.; Hallett, M.; Lang, A.; Hallett, M. Movement disorders on YouTube—Caveat spectator. N. Engl. J. Med. 2011, 365, 1160–1161. [Google Scholar] [CrossRef] [PubMed]
- Dubey, D.; Amritphale, A.; Sawhney, A.; Dubey, D.; Srivastav, N. Analysis of YouTube as a source of information for West Nile Virus infection. Clin. Med. Res. 2014, 12, 129–132. [Google Scholar] [CrossRef] [PubMed]
- Mazanderani, F.; O’Neill, B.; Powell, J. “People power” or “pester power”? YouTube as a forum for the generation of evidence and patient advocacy. Patient Educ. Couns. 2013, 93, 420–425. [Google Scholar] [CrossRef] [PubMed]
- Miller, E.; Pole, A. Diagnosis blog: Checking up on health blogs in the blogosphere. Am. J. Public Health 2010, 100, 1514–1519. [Google Scholar] [CrossRef] [PubMed]
- De Viron, S.; Suggs, L.; Brand, A.; Van Oyen, H. Communicating genetics and smoking through social media: Are we there yet? J. Med. Internet Res. 2013, 15, e198. [Google Scholar] [CrossRef] [PubMed]
- Schumacher, K.; Stringer, K.; Donohue, J.; Yu, S.; Shaver, A.; Caruthers, R.; Zikmund-Fisher, B.; Fifer, C.; Goldberg, C.; Russell, M. Social media methods for studying rare diseases. Pediatrics 2014, 133, e1345–1353. [Google Scholar] [CrossRef] [PubMed]
- Van Der Velden, M.; El Emam, K. “Not all my friends need to know”: A qualitative study of teenage patients, privacy, and social media. J. Am. Med. Inform. Assoc. 2013, 20, 16–24. [Google Scholar] [CrossRef] [PubMed]
- Heilman, J.; West, A. Wikipedia and medicine: Quantifying readership, editors, and the significance of natural language. J. Med. Internet Res. 2015, 17, e62. [Google Scholar] [CrossRef] [PubMed]
- Farič, N.; Potts, H. Motivations for contributing to health-related articles on Wikipedia: an interview study. J. Med. Internet Res. 2014, 16, e260. [Google Scholar] [CrossRef] [PubMed]
- Valdez, R.; Guterbock, T.; Thompson, M.; Reilly, J.; Menefee, H.; Bennici, M.; Williams, I.; Rexrode, D. Beyond traditional advertisements: Leveraging Facebook’s social structures for research recruitment. J. Med. Internet Res. 2014, 16, e243. [Google Scholar] [CrossRef] [PubMed]
- De Vries, N.; Carlson, J.; Moscato, P. A data-driven approach to reverse engineering customer engagement models: Towards functional constructs. PLoS ONE 2014, 9, e102768. [Google Scholar]
- Moreno, M.; Grant, A.; Kacvinsky, L.; Moreno, P.; Fleming, M. Older adolescents’ views regarding participation in Facebook research. J. Adolesc. Health 2012, 51, 439–444. [Google Scholar] [CrossRef] [PubMed]
- Kontos, E.; Blake, K.; Chou, W.; Prestin, A. Predictors of eHealth usage: Insights on the digital divide from the Health Information National Trends Survey 2012. J. Med. Internet Res. 2014, 16, e172. [Google Scholar] [CrossRef] [PubMed]
- Tennant, B.; Stellefson, M.; Dodd, V.; Chaney, B.; Chaney, D.; Paige, S.; Alber, J. eHealth literacy and Web 2.0 health information seeking behaviors among baby boomers and older adults. J. Med. Internet Res. 2015, 17, e70. [Google Scholar] [CrossRef] [PubMed]
- Connolly, K.; Crosby, M. Examining e-Health literacy and the digital divide in an underserved population in Hawaii. Hawaii J. Med. Public Health 2014, 73, 44–48. [Google Scholar] [PubMed]
- Blackstock, O.; Haughton, L.; Garner, R.; Horvath, K.; Norwood, C.; Cunningham, C. General and health-related Internet use among an urban, community-based sample of HIV-positive women: Implications for intervention development. AIDS Care 2015, 27, 536–544. [Google Scholar] [CrossRef] [PubMed]
- Tan, M.; Kok, K.; Ganesh, V.; Thomas, S. Patient information on breast reconstruction in the era of the world wide web. A snapshot analysis of information available on youtube.com. Breast 2014, 23, 33–37. [Google Scholar] [CrossRef] [PubMed]
- Bezner, S.; Hodgman, E.; Diesen, D.; Clayton, J.; Minkes, R.; Langer, J.; Chen, L. Pediatric surgery on YouTube™: Is the truth out there? J. Pediatr. Surg. 2014, 49, 586–589. [Google Scholar] [CrossRef] [PubMed]
- Yaylaci, S.; Serinken, M.; Eken, C.; Karcioglu, O.; Yilmaz, A.; Elicabuk, H.; Dal, O. Are YouTube videos accurate and reliable on basic life support and cardiopulmonary resuscitation? Emerg. Med. Australas. 2014, 26, 474–477. [Google Scholar] [CrossRef] [PubMed]
- Reavley, N.; Mackinnon, A.; Morgan, A.; Alvarez-Jimenez, M.; Hetrick, S.; Killackey, E.; Nelson, B.; Purcell, R.; Yap, M.B.H.; Jorm, A. Quality of information sources about mental disorders: A comparison of Wikipedia with centrally controlled web and printed sources. Psychol. Med. 2012, 42, 1753–1762. [Google Scholar] [CrossRef] [PubMed]


© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cordoş, A.-A.; Bolboacă, S.D.; Drugan, C. Social Media Usage for Patients and Healthcare Consumers: A Literature Review. Publications 2017, 5, 9. https://doi.org/10.3390/publications5020009
Cordoş A-A, Bolboacă SD, Drugan C. Social Media Usage for Patients and Healthcare Consumers: A Literature Review. Publications. 2017; 5(2):9. https://doi.org/10.3390/publications5020009
Chicago/Turabian StyleCordoş, Ariana-Anamaria, Sorana Daniela Bolboacă, and Cristina Drugan. 2017. "Social Media Usage for Patients and Healthcare Consumers: A Literature Review" Publications 5, no. 2: 9. https://doi.org/10.3390/publications5020009






