Helping Health Services to Meet the Needs of Young People with Chronic Conditions: Towards a Developmental Model for Transition
Abstract
:1. Introduction
2. Health Transition as One of Multiple, Interrelated Transitions
3. Developmentally Appropriate Transitional Care for Young People
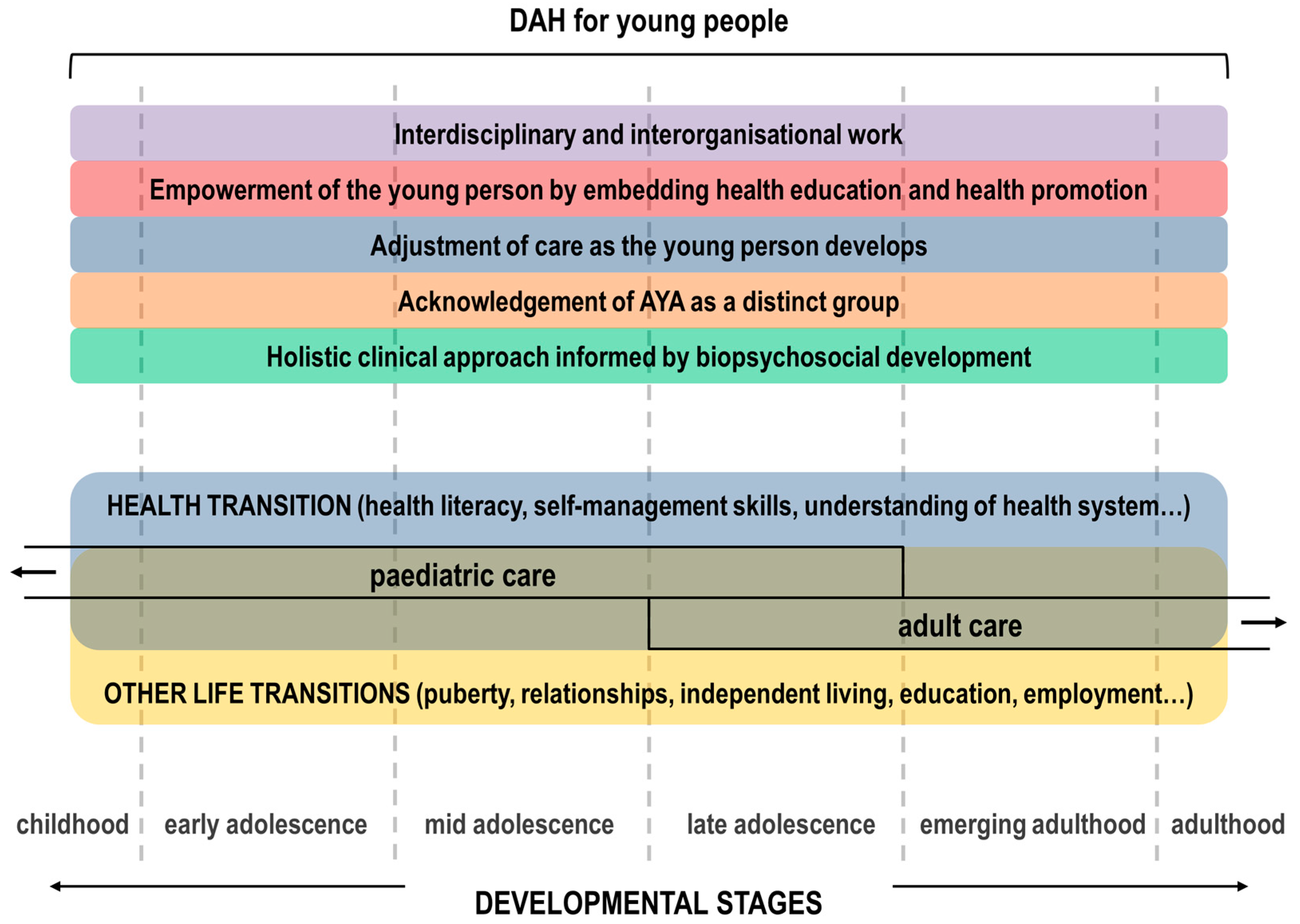
- Biopsychosocial development and holistic care. Key developmental milestones of AYAs at biological, psychological, social and vocational levels (across early, mid and late adolescence and emerging adulthood) inform clinical work by either (1) adopting a holistic clinical approach that looks beyond the physical aspect of one’s condition and integrates the biological psychological, social and vocational aspects of development; or (2) incorporating additional care components to otherwise standard paediatric/adult care. Family or trusted others are included as key stakeholders and/or active participants of healthcare provision for AYAs [15].
- Acknowledgement of AYA as a distinct group. Developmental needs of AYAs inform distinct ways of interacting and communicating with them, in terms of (1) what, when and how information is given to and gathered from them; and (2) official communication materials and means (such as appointment letters or text message reminders). Specific/tailored services, spaces and pathways are provided. The distinct needs of the service (e.g., need for longer appointments) and those of the health professionals looking after AYAs (e.g., training in adolescent health) are acknowledged and addressed [15].
- Adjustment of care as the young person develops. The starting point of DAH is a developmental assessment, covering all areas of AYA development and actively involving parents/carers and/or trusted others. Routine follow-up developmental assessments are then undertaken and used to inform the tailoring of particular aspects of clinical work and service delivery as the young person grows up [15].
- Empowerment of the young person by embedding health education and health promotion. AYAs are routinely provided with (1) informal education on self-management skills and (2) health promotion information and lifestyle behaviour change advice relevant to each stage of development to enable AYAs to make informed choices. Health education and health promotion delivered in the context of DAH services is informed by, but not limited to, a health transition agenda. The approach to health education and health promotion delivered in the context of DAH is based on promoting active engagement and autonomy-enabling practices without creating relations of dependency with the service/clinical team [15].
- Interdisciplinary and interorganisational work. Effective multidisciplinary work both within and across services, teams, specialities and organisations [15].
- Was the intervention concerned with changing the approach to clinical work based on key developmental milestones of AYAs from early adolescence through to emerging adulthood?
- Were the family or AYA’s trusted others included in service provision?
- Was the individual and service level communication strategy tailored to developmental needs?
- Were AYA-specific/tailored services, spaces and pathways provided or engaged with as part of the intervention?
- Were the needs of staff delivering the intervention dealt with (adolescent health training, availability of resources) as part of the intervention?
- Were routine and follow-up biopsychosocial developmental assessments (and tools) built into the intervention and used to inform dynamic changes in clinical work and service delivery as AYAs develop?
- Was the intervention concerned with supporting effective multidisciplinary work both within and across services, teams, specialities and organisations?
4. Outcome Indicators of Transition
5. Conclusions
Acknowledgments
Conflicts of Interest
References
- Campbell, F.; Biggs, K.; Aldiss, S.K.; O’Neill, P.M.; Clowes, M.; McDonagh, J.; While, A.; Gibson, F. Transition of care for adolescents from paediatric services to adult health services. Cochrane Database Syst. Rev. 2016, 4, CD009794. [Google Scholar] [CrossRef] [PubMed]
- Barbero, G.J. Leaving the pediatrician for the internist. Ann. Intern. Med. 1982, 96, 673–674. [Google Scholar] [CrossRef]
- American Academy of Pediatrics; American Academy of Family Physicians; American College of Physicians, Transitions Clinical Report Authoring Group. Supporting the Health Care Transition From Adolescence to Adulthood in the Medical Home. Pediatrics 2011, 128, 182–200. [Google Scholar] [CrossRef]
- National Institute for Health and Care Excellence (NICE) NICE guidelines [NG43]. Transition from Children’s to Adults’ Services for Young People Using Health or Social Care Services. Available online: https://www.nice.org.uk/guidance/ng43 (accessed on 31 July 2017).
- Lugasi, T.; Achille, M.; Stevenson, M. Patients’ perspective on factors that facilitate transition from child-centered to adult-centered health care: A theory integrated metasummary of quantitative and qualitative studies. J. Adolesc. Health 2011, 48, 429–440. [Google Scholar] [CrossRef] [PubMed]
- Hepburn, C.M.; Cohen, E.; Bhawra, J.; Weiser, N.; Hayeems, R.Z.; Guttmann, A. Health system strategies supporting transition to adult care. Arch. Dis. Child. 2015, 100, 559–564. [Google Scholar] [CrossRef] [PubMed]
- Sonneveld, H.M.; Strating, M.M.H.; van Staa, A.L.; Nieboer, A.P. Gaps in transitional care: What are the perceptions of adolescents, parents and providers? Transitional care—Perceptions of adolescents, parents and providers. Child Care Health Dev. 2013, 39, 69–80. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, A.; Sawyer, S. Transition from pediatric to adult services: Are we getting it right? Curr. Opin. Pediatr. August 2008, 20, 403–409. [Google Scholar] [CrossRef] [PubMed]
- Scal, P. Improving health care transition services: Just grow up, will you please. JAMA Pediatr. 2016, 170, 197–199. [Google Scholar] [CrossRef] [PubMed]
- Shaw, K.L.; Southwood, T.R.; McDonagh, J.E. User perspectives of transitional care for adolescents with juvenile idiopathic arthritis. Rheumatology 2004, 43, 770–778. [Google Scholar] [CrossRef] [PubMed]
- Boisen, K.A.; Hertz, P.G.; Blix, C.; Teilmann, G. Is HEADS in our heads? Health risk behavior is not routinely discussed with young people with chronic conditions. Int. J. Adolesc. Med. Health 2016, 28, 429–435. [Google Scholar] [CrossRef] [PubMed]
- Stinson, J.; Kohut, S.A.; Spiegel, L.; White, M.; Gill, N.; Colbourne, G.; Sigurdson, S.; Duffy, K.W.; Tucker, L.; Stringer, E.; et al. A systematic review of transition readiness and transfer satisfaction measures for adolescents with chronic illness. Int. J. Adolesc. Med. Health 2014, 26, 159–174. [Google Scholar] [CrossRef] [PubMed]
- Sawyer, S.M. Developmentally appropriate healthcare for young people with chronic illness: Questions of philosophy, policy, and practice. Pediatr. Pulmonol. 2003, 36, 363–365. [Google Scholar] [CrossRef] [PubMed]
- Farre, A.; Wood, V.; Rapley, T.; Parr, J.R.; Reape, D.; McDonagh, J.E. Developmentally appropriate healthcare for young people: A scoping study. Arch. Dis. Child. 2014. [Google Scholar] [CrossRef] [PubMed]
- Farre, A.; Wood, V.; McDonagh, J.E.; Parr, J.R.; Reape, D.; Rapley, T.; on behalf of the Transition Collaborative Group. Health professionals’ and managers’ definitions of developmentally appropriate healthcare for young people: Conceptual dimensions and embedded controversies. Arch. Dis Child. 2016, 101, 628–633. [Google Scholar] [CrossRef] [PubMed]
- Sawyer, S.M.; Afifi, R.A.; Bearinger, L.H.; Blakemore, S.-J.; Dick, B.; Ezeh, A.C.; Patton, G.C. Adolescence: A foundation for future health. Lancet 2012, 379, 1630–1640. [Google Scholar] [CrossRef]
- Viner, R. Life stage: Adolescence. In Annual Report of the Chief Medical Officer 2012, Our Children Deserve Better: Prevention Pays; Davies, S.C., Ed.; Department of Health: London, UK, 2013; Chapter 8; pp. 1–11. [Google Scholar]
- Blakemore, S.-J.; Burnett, S.; Dahl, R.E. The role of puberty in the developing adolescent brain. Hum. Brain Mapp. 2010, 31, 926–933. [Google Scholar] [CrossRef] [PubMed]
- Berenbaum, S.A.; Beltz, A.M.; Corley, R. The Importance of Puberty for Adolescent Development. Adv. Child. Dev. Behav. 2015, 48, 53–92. [Google Scholar] [CrossRef] [PubMed]
- Sawyer, S.M.; Aroni, R.A. Self-management in adolescents with chronic illness. What does it mean and how can it be achieved? Med. J. Aust. 2005, 183, 405–409. [Google Scholar] [PubMed]
- Jenkins, R.R. Adolescent medicine in the USA: A perspective on progress and lessons learnt. Arch. Dis. Child. 2016, 101, 510–513. [Google Scholar] [CrossRef] [PubMed]
- Rosen, D.S.; Goldenring, J.M. Getting into adolescent heads: An essential update. Contemp. Pediatr. 2004, 21, 64–90. [Google Scholar]
- Doukrou, M.; Segal, T.Y. Fifteen-minute consultation: Communicating with young people—How to use HEEADSSS, a psychosocial interview for adolescents. Arch. Dis. Child.—Educ. Pract. 2017. [Google Scholar] [CrossRef] [PubMed]
- Ambresin, A.-E.; Bennett, K.; Patton, G.C.; Sanci, L.A.; Sawyer, S.M. Assessment of Youth-Friendly Health Care: A Systematic Review of Indicators Drawn From Young People’s Perspectives. J. Adolesc. Health 2013, 52, 670–681. [Google Scholar] [CrossRef] [PubMed]
- Department of Health. You’re Welcome: Quality Criteria for Young People Friendly Services 2011. Available online: https://www.gov.uk/government/publications/quality-criteria-for-young-people-friendly-health-services (accessed on 10 October 2017).
- Hargreaves, D.S.; McDonagh, J.E.; Viner, R.M. Validation of You’re Welcome Quality Criteria for Adolescent Health Services Using Data from National Inpatient Surveys in England. J. Adolesc. Health 2013, 52, 50–57. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization towards Adolescent-Responsive Health Systems: Steering the Transition from Adolescent-Friendly Projects to Adolescent-Responsive Health Systems. Available online: http://apps.who.int/adolescent/second-decade/section6/page8/sdolescent-responsiveness.html (accessed on 23 March 2017).
- Fair, C.; Cuttance, J.; Sharma, N.; Maslow, G.; Wiener, L.; Betz, C.; Porter, J.; McLaughlin, S.; Gilleland-Marchak, J.; Renwick, A. International and interdisciplinary identification of health care transition outcomes. JAMA Pediatr. 2016, 170, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Sharma, N.; O’Hare, K.; Antonelli, R.C.; Sawicki, G.S. Transition Care: Future Directions in Education, Health Policy, and Outcomes Research. Acad. Pediatr. 2014, 14, 120–127. [Google Scholar] [CrossRef] [PubMed]
- Hale, D.R.; Bevilacqua, L.; Viner, R.M. Adolescent Health and Adult Education and Employment: A Systematic Review. Pediatrics 2015, 136, 128–140. [Google Scholar] [CrossRef] [PubMed]
- Maslow, G.R.; Haydon, A.; McRee, A.-L.; Ford, C.A.; Halpern, C.T. Growing Up With a Chronic Illness: Social Success, Educational/Vocational Distress. J. Adolesc. Health 2011, 49, 206–212. [Google Scholar] [CrossRef] [PubMed]
- Pinquart, M. Achievement of Developmental Milestones in Emerging and Young Adults With and Without Pediatric Chronic Illness--A Meta-Analysis. J. Pediatr. Psychol. 2014. [Google Scholar] [CrossRef] [PubMed]
- Fredericks, E.M.; Dore-Stites, D.; Well, A.; Magee, J.C.; Freed, G.L.; Shieck, V.; James Lopez, M. Assessment of transition readiness skills and adherence in pediatric liver transplant recipients. Pediatr. Transpl. 2010, 14, 944–953. [Google Scholar] [CrossRef] [PubMed]
- Carlsen, K.; Haddad, N.; Gordon, J.; Phan, B.L.; Pittman, N.; Benkov, K.; Dubinsky, M.C.; Keefer, L. Self-efficacy and Resilience Are Useful Predictors of Transition Readiness Scores in Adolescents with Inflammatory Bowel Diseases. Inflamm. Bowel Dis. 2017, 23, 341–346. [Google Scholar] [CrossRef] [PubMed]
- Stollon, N.; Zhong, Y.; Ferris, M.; Bhansali, S.; Pitts, B.; Rak, E.; Kelly, M.; Kim, S.; van Tilburg, M.A. Chronological age when healthcare transition skills are mastered in adolescents/young adults with inflammatory bowel disease. World J. Gastroenterol. 2017, 23, 3349. [Google Scholar] [CrossRef] [PubMed]
- Gray, W.N.; Holbrook, E.; Morgan, P.J.; Saeed, S.A.; Denson, L.A.; Hommel, K.A. Transition readiness skills acquisition in adolescents and young adults with inflammatory bowel disease: Findings from integrating assessment into clinical practice. Inflamm. Bowel Dis. 2015, 21, 1125–1131. [Google Scholar] [CrossRef] [PubMed]
- Fishman, L.N.; Barendse, R.M.; Hait, E.; Burdick, C.; Arnold, J. Self-management of older adolescents with inflammatory bowel disease: A pilot study of behavior and knowledge as prelude to transition. Clin. Pediatr. 2010, 49, 1129–1133. [Google Scholar] [CrossRef] [PubMed]
- Whitfield, E.P.; Fredericks, E.M.; Eder, S.J.; Shpeen, B.H.; Adler, J. Transition readiness in pediatric patients with inflammatory bowel disease: A patient survey of self-management skills. J. Pediatr. Gastroenterol. Nutr. 2015, 60, 36. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.S.; Tobin, A.; Tompane, T. Clinicians poorly assess health literacy-related readiness for transition to adult care in adolescents with inflammatory bowel disease. Clin. Gastroenterol. Hepatol. 2012, 10, 626–632. [Google Scholar] [CrossRef] [PubMed]
- Eaton, C.K.; Davis, M.F.; Gutierrez-Colina, A.M.; LaMotte, J.; Blount, R.L.; Suveg, C. Different Demands, Same Goal: Promoting Transition Readiness in Adolescents and Young Adults With and Without Medical Conditions. J. Adolesc. Health 2017, 60, 727–733. [Google Scholar] [CrossRef] [PubMed]
- Pierce, J.S.; Aroian, K.; Schifano, E.; Milkes, A.; Schwindt, T.; Gannon, A.; Wysocki, T. Health Care Transition for Young Adults With Type 1 Diabetes: Stakeholder Engagement for Defining Optimal Outcomes. J. Pediatr. Psychol. 2017, 42, 970–982. [Google Scholar] [CrossRef] [PubMed]
- Klosky, J.L.; Cash, D.K.; Buscemi, J.; Lensing, S.; Garces-Webb, D.M.; Zhao, W.; Wiard, S.; Hudson, M.M. Factors influencing long-term follow-up clinic attendance among survivors of childhood cancer. J. Cancer Surviv. 2008, 2, 225. [Google Scholar] [CrossRef] [PubMed]
- Snow, R.; Fulop, N. Understanding issues associated with attending a young adult diabetes clinic: A case study. Diabet. Med. 2012, 29, 257–259. [Google Scholar] [CrossRef] [PubMed]
| Developmental Stage | Transitions |
|---|---|
| Early Adolescence 10–13 years | Biological (e.g., early puberty) |
| Psychological (e.g., concrete thinking to early moral concepts) | |
| Social (e.g., emotional separation from parents) | |
| Health (e.g., early self-management) | |
| Educational (e.g., primary to secondary school) | |
| Mid Adolescence 14–16 years | Biological (e.g., mid-late puberty) |
| Psychological (e.g., early abstract thinking) | |
| Social (e.g., strong peer identification) | |
| Health (e.g., increased self-management) | |
| Educational/Vocational (e.g., school to college) | |
| Late adolescence 17–19 years | Biological (e.g., completion of puberty) |
| Psychological (e.g., complex abstract thinking) | |
| Social (e.g., independent living and travel) | |
| Health (e.g., paediatric to adult healthcare) | |
| Educational/Vocational (e.g., college to further education or training) | |
| Emerging Adulthood 20–24 years | Biological (e.g., completion of brain development) |
| Psychological (e.g., exploration of self-identity) | |
| Social (e.g., independent living and financial independence) | |
| Health (e.g., autonomous self-management) | |
| Educational/Vocational (e.g., further education/training to employment) |
| Conceptual Dimensions of DAH for Young People [15] | Examples of How These Dimensions Are Translated into Practice |
|---|---|
| biopsychosocial development and holistic care |
|
| acknowledgement of young people as a distinct group | Acknowledgement of age and developmental stage-specific issues and how these may change during adolescence and young adulthood:
|
| adjustment of care as the young person develops | Flexibility in approach and acknowledgement of regression during active phases in relapsing conditions:
|
| empowerment of the young person by embedding health education and health promotion |
|
| interdisciplinary and interorganisational work |
|
| Domains of youth-friendly health care (YFHC) | Examples of Relevant Indicators |
|---|---|
| 1. Accessibility of health care | Location, affordability |
| 2. Staff attitude | Respectful, supportive, honest, trustworthy, friendly |
| 3. Communication | Clarity and provision of information, active listening, tone of communication |
| 4. Medical competency | Technical skills (procedures) |
| 5. Guideline-driven care | Confidentiality, autonomy, transition to adult health care services, comprehensive care |
| 6. Age-appropriate environment | Flexibility of appointment times, separate physical space, teen-oriented health information, cleanliness, waiting time, continuity of care, privacy |
| 7. Involvement in own health care | Understanding of one’s medical condition and treatment; acquisition of self-management skills |
| 8. Health outcomes | Pain management, quality of life |
| Outcome | Campbell et al. 2016 [1] | Fair et al. 2015 [28] | Sharma et al. 2014 [29] | NICE 2016 [4] |
|---|---|---|---|---|
| Transition readiness, self efficacy | Transition readiness (TRAQ); Patient Activation Measure; Community Life Skills (CLSS); Self-care practice | Self-management; Adherence to medication/treatment | Transition readiness | Transition readiness; Self-efficacy (YP’s ability to undertake the activities they want to, as independently as possible) |
| Disease-specifc status | HbA1C | − | Condition-specific outcomes | Condition-specific outcomes |
| Well being | Personal Adjustment and role skills (PARS III); Peds Qol | Achieving optimal Quality of life (QoL) | QoL | Qol (health and social care indicators) |
| Knowledge of disease and treatment | MyHeart | Disease knowledge; Medication knowledge | − | − |
| Knowledge of transition | − | − | Transition knowledge | − |
| Transfer from paediatric to adult services | % young people successfully transferred to adult services | − | Gaps in medical care | Continuity of care (loss of contacts with services, lack of appropriate referral, satisfaction, interagency communication, clinical outcomes) |
| Healthcare utilisation | Patient initiated health care communication; Hospitalisation | Attending medical appointments; Having a medical home; Avoiding unnecessary hospitalisations | Health care utilisation; Gaps in medical care | Health and social care resource utilisation |
| Understanding health insurance | − | understanding health insurance options | Loss of health insurance; Health coverage issues | − |
| Having a social network | − | Having a social network of friends | − | − |
| Stage of Health Transition | Health Care Professional | Health System |
|---|---|---|
| Preparation | Use of transition care plans | Development of transition policy |
| Assessment of transition readiness | ||
| Young person/family education and counselling | Care coordination | |
| Transfer of care | Preparation of patient summary | Use of patient summary |
| Communication | Communication between paediatric-adult systems | |
| Post transfer | Intake policy for transferring patients | Quality of intake to adult care |
| Care coordination | ||
| Financial costs and savings |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Farre, A.; McDonagh, J.E. Helping Health Services to Meet the Needs of Young People with Chronic Conditions: Towards a Developmental Model for Transition. Healthcare 2017, 5, 77. https://doi.org/10.3390/healthcare5040077
Farre A, McDonagh JE. Helping Health Services to Meet the Needs of Young People with Chronic Conditions: Towards a Developmental Model for Transition. Healthcare. 2017; 5(4):77. https://doi.org/10.3390/healthcare5040077
Chicago/Turabian StyleFarre, Albert, and Janet E. McDonagh. 2017. "Helping Health Services to Meet the Needs of Young People with Chronic Conditions: Towards a Developmental Model for Transition" Healthcare 5, no. 4: 77. https://doi.org/10.3390/healthcare5040077





