From Consultation to Application: Practical Solutions for Improving Maternal and Neonatal Outcomes for Adolescent Aboriginal Mothers at a Local Level
Abstract
:1. Introduction
1.1. Setting the Scene
1.1.1. Teen Pregnancy in Western Australia
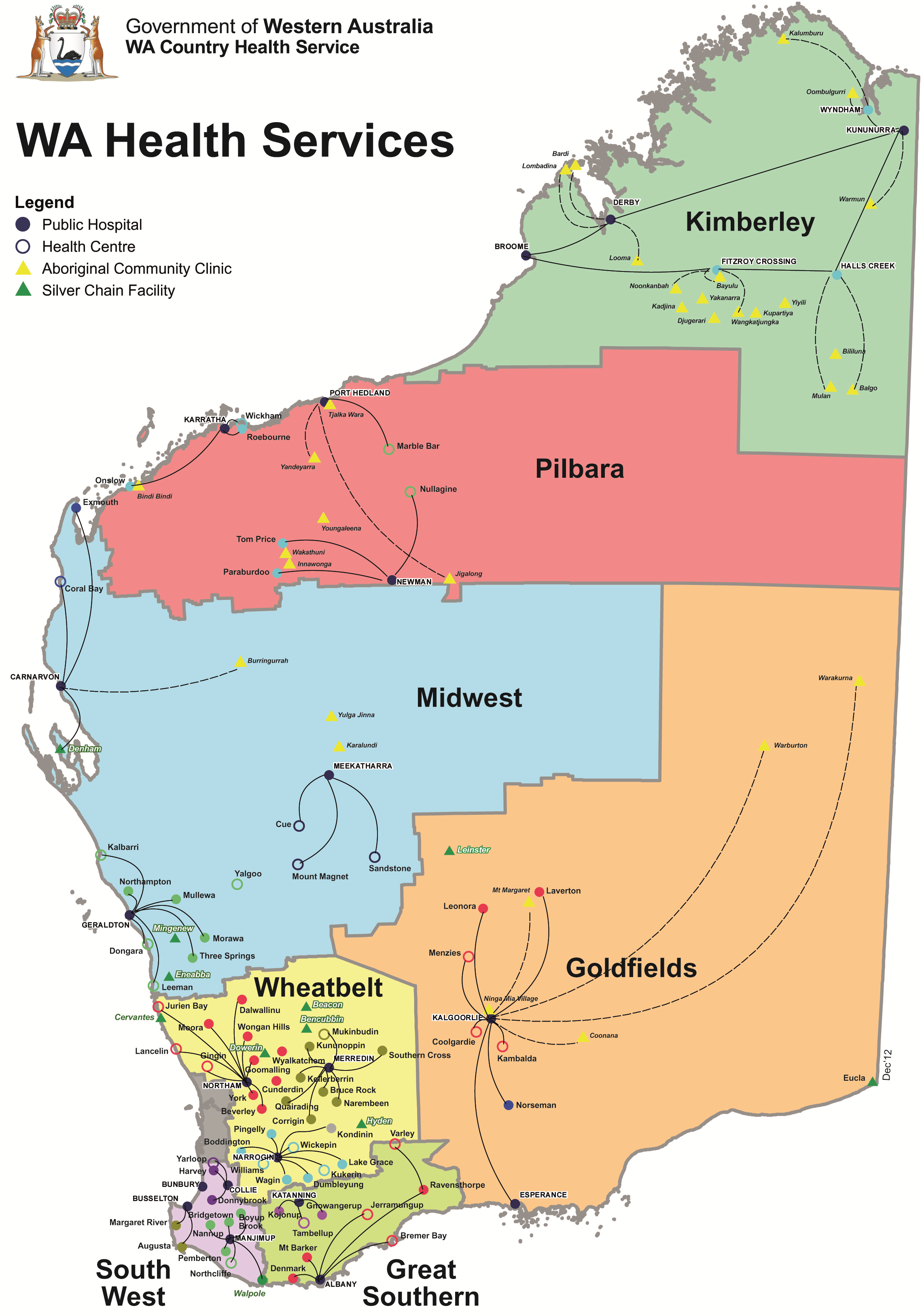
1.1.2. Context of the Geographical Environment on Access to Health
1.1.3. Context of Adolescent Pregnancy
Why Teenage Pregnancy Occurs?
Supporting Adolescents Regardless of Causal Factors
2. Method
- (1)
- The Young Aboriginal Women’s Voices on Pregnancy Care project was conducted as a descriptive qualitative research study with data collection undertaken using a culturally sensitive, semi-structured interview schedule incorporating a personal and conversational manner known as yarning [52]. Data was analysed using standard qualitative analysis techniques, identifying themes and sub-topics. A total of 84 individual or group interviews were conducted with 28 women in the target group (16–21 years) and 56 senior and elder Aboriginal women and non-Aboriginal service providers in locations across WA, including six out of the eight health regions. The field researchers were an Aboriginal cultural consultant highly experienced in working with young Aboriginal mothers in her role as an Aboriginal Health Worker and a non-Aboriginal researcher with extensive experience in conducting interviews with Aboriginal people. Study approval was granted by the Western Australian Aboriginal Health Ethics Committee (WAAHEC) (2013:443) and the Western Australian Country Health Service (WACHS) (2013:05), Women’s and Newborns Health Service (2013-038EW), and North and South Metropolitan Health Services Human Research Ethics Committees (HREC) (reciprocal approval). Research approval was also granted by the Kimberley Aboriginal Health Planning Forum Research Sub-Committee.
- (2)
- The Aboriginal Women’s Patient Journeys project was a feasibility study to determine what an integrated model of care for Aboriginal women in WA during pregnancy might include. Over 140 health professionals from 53 different organizations across WA participated in either focus groups or individual interviews. To identify themes, each focus group or interview printed record and taped transcript was analysed and common themes and topics were then translated into a matrix to allow comparison across regions. These matrices were reviewed by the research team for confirmation of content and to conclude what similarities and contrasts were apparent across regions. The data was analysed according to standard qualitative data analysis protocols. Ethics approval for this project was obtained from WAAHEC (2013:500) and WACHS HREC (2013:21). The King Edward Memorial Hospital HREC committee assessed the project as a quality improvement project, thus it was entered into Governance Evidence Knowledge Outcomes (GEKO) Safety and Quality database as a quality audit. Express written permission was obtained from the Chief Executive Officer or Board for every ACCHS or AMS involved.
2.1. Applying the Research Findings
- Young Aboriginal women need pregnancy care that supports them during a vulnerable time in their lives and respects their choice, privacy and confidentiality at all times and in all service settings.
- Aboriginal family relationships are crucial to encouraging early and ongoing antenatal engagement by young Aboriginal women. Services need to build relationships with influential local women Elders/community members to support knowledge exchange of pregnancy and childbirth and local cultural practices; dissemination of information about pregnancy care and available services throughout communities; and assistance with identification of young pregnant women to encourage engagement with health care.
- Dedicated spaces are required where women can come together safely to “yarn” (talk).
- Culturally safe models of care (with continuity of carer) provided by culturally competent health professionals and other health service staff are needed to maintain relationships with young pregnant women.
- Adolescents moving between communities were viewed as being most at risk of not accessing antenatal care. Women who need to relocate to give birth are at risk of falling through service gaps and having negative pregnancy and birthing experiences as a result.
- A documented patient relocation pathway is required to support young Aboriginal women to feel safe. This includes securing appropriate transport from and back to home communities; assistance for escort/support people to be present for the duration of the pregnant woman’s relocation (including changes of support people over that time); accommodation options and social support services at the relocation site, including access to an Aboriginal Liaison Officer/Community Care or Health Worker; detailed information about the cultural practices/expectations of individual Aboriginal women forwarded by the home community health service staff for the information of health service staff at the relocation site.
2.2. Identifying Actions for Implementation
3. Discussion
4. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Fraser, A.M.; Brockert, J.E.; Ward, R.H. Association of young maternal age with adverse reproductive outcomes. N. Engl. J. Med. 1995, 332, 1113–1117. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.K.; Wen, S.W.; Fleming, N.; Demissie, K.; Rhoads, G.G.; Walker, M. Teenage pregnancy and adverse birth outcomes: A large population based retrospective cohort study. Int. J. Epidemiol. 2007, 36, 368–373. [Google Scholar] [CrossRef] [PubMed]
- Smith, G.C.; Pell, J.P. Teenage pregnancy and risk of adverse perinatal outcomes associated with first and second births: Population based retrospective cohort study. Br. Med. J. 2001, 323. [Google Scholar] [CrossRef]
- Lewis, L.N.; Hickey, M.; Doherty, D.A.; Skinner, S.R. How do pregnancy outcomes differ in teenage mothers? A Western Australian study. Med. J. Aust. 2009, 190, 537–541. [Google Scholar] [PubMed]
- Gavin, A.R.; Lindhorst, T.; Lohr, M.J. The prevalence and correlates of depressive symptoms among adolescent mothers: Results from a 17-year longitudinal study. Women Health 2011, 51, 525–545. [Google Scholar] [CrossRef] [PubMed]
- Shaw, E.; Levitt, C.; Wong, S.; Kaczorowski, J.; McMaster University Postpartum Research Group. Systematic Review of the Literature on Postpartum Care: Effectiveness of Postpartum Support to Improve Maternal Parenting, Mental Health, Quality of Life, and Physical Health. Birth 2006, 33, 210–220. [Google Scholar] [CrossRef] [PubMed]
- Olsson, C.A.; Horwill, E.; Moore, E.; Eisenberg, M.E.; Venn, A.; O’Loughlin, C.; Patton, G.C. Social and Emotional Adjustment Following Early Pregnancy in Young Australian Women: A Comparison of Those Who Terminate, Miscarry, or Complete Pregnancy. J. Adolesc. Health 2014, 54, 698–703. [Google Scholar] [CrossRef] [PubMed]
- Boden, J.M.; Fergusson, D.M.; John Horwood, L. Early motherhood and subsequent life outcomes. J. Child Psychol. Psychiatry 2008, 49, 151–160. [Google Scholar] [CrossRef] [PubMed]
- Quinlivan, J.A.; Petersen, R.W.; Gurrin, L.C. Adolescent pregnancy: Psychopathology missed. Aust. N. Z. J. Psychiatry 1999, 33, 864–868. [Google Scholar] [CrossRef] [PubMed]
- Quinlivan, J.A.; Tan, L.H.; Steele, A.; Black, K. Impact of demographic factors, early family relationships and depressive symptomatology in teenage pregnancy. Aust. N. Z. J. Psychiatry 2004, 38, 197–203. [Google Scholar] [CrossRef] [PubMed]
- Murphy, E.; Best, E. The Aboriginal maternal and infant health service: A decade of achievement in the health of women and babies in NSW. NSW Public Health Bull. 2012, 23, 68–72. [Google Scholar] [CrossRef] [PubMed]
- McCalman, J.; Searles, A.; Bainbridge, R.; Ham, R.; Mein, J.; Neville, J.; Campbell, S.; Tsey, K. Empowering families by engaging and relating Murri way: A grounded theory study of the implementation of the Cape York Baby Basket Program. BMC Pregnancy Childbirth 2015, 15. [Google Scholar] [CrossRef] [PubMed]
- Raatikainen, K.; Heiskanen, N.; Verkasalo, P.K.; Heinonen, S. Good outcome of teenage pregnancies in high-quality maternity care. Eur. J. Public Health 2006, 16, 157–161. [Google Scholar] [CrossRef] [PubMed]
- Larkins, S.L.; Priscilla Page, R.; Panaretto, K.S.; Mitchell, M.; Alberts, V.; McGinty, S.; Craig Veitch, P. The transformative potential of young motherhood for disadvantaged Aboriginal and Torres Strait Islander women in Townsville, Australia. Med. J. Aust. 2011, 194, 551–555. [Google Scholar] [PubMed]
- Reibel, T.; Morrison, L.; Griffin, D.; Chapman, L.; Woods, H. Young Aboriginal women’s voices on pregnancy care: Factors encouraging antenatal engagement. Women Birth 2015, 28, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Sheeran, N.; Jones, L.; Rowe, J. Motherhood as the Vehicle for Change in Australian Adolescent Women of Preterm and Full-Term Infants. J. Adolesc. Res. 2016, 31, 700–724. [Google Scholar] [CrossRef]
- Brand, G.; Morrison, P.; Down, B. How do health professionals support pregnant and young mothers in the community? A selective review of the research literature. Women Birth 2014, 27, 174–178. [Google Scholar] [CrossRef] [PubMed]
- Osborne, K.; Baum, F.; Brown, L. What Works? A Review of Actions Addressing the Social and Economic Determinants of Indigenous Health; Issues Paper No. 7 Produced for the Closing the Gap Clearing House; Australian Institute of Health and Welfare: Canberra, Australia, 2013.
- Zhu, P.; Tao, F.; Hao, J.; Sun, Y.; Jiang, X. Prenatal life events stress: Implications for preterm birth and infant birthweight. Am. J. Obstet. Gynecol. 2010, 203, 34.e1–34.e8. [Google Scholar] [CrossRef] [PubMed]
- O’Leary, C.M.; Nassar, N.; Kurinczuk, J.; Bower, C. The effect of maternal alcohol consumption on fetal growth and preterm birth. BJOG Int. J. Obstet. Gynaecol. 2009, 116, 390–400. [Google Scholar] [CrossRef] [PubMed]
- Cnattingius, S. The epidemiology of smoking during pregnancy: Smoking prevalence, maternal characteristics, and pregnancy outcomes. Nicotine Tob. Res. 2004, 6, S125–S140. [Google Scholar] [CrossRef] [PubMed]
- Brown, S.J.; Weetra, D.; Glover, K.; Bucksin, M.; Ah Kit, J.; Leane, C.; Mitchell, A.; Stuart-Butler, D.; Turner, M.; Gartland, D.; et al. Improving Aboriginal Women’s Experiences of Antenatal Care: Findings from the Aboriginal Families Study in South Australia. Birth 2015, 42, 27–37. [Google Scholar] [CrossRef] [PubMed]
- Bar-Zeev, S.; Barclay, L.; Kruske, S.; Kildea, S. Factors affecting the quality of antenatal care provided to remote dwelling Aboriginal women in northern Australia. Midwifery 2014, 30, 289–296. [Google Scholar] [CrossRef] [PubMed]
- Krahe, K. Give Indigenous Australian Women and Infants a Chance at Life: Addressing the Disparity in Maternal-Infant Health Outcomes. 2016. Available online: http://globalvoices.org.au/research/kaitlyn-oecd-research-paper (accessed on 29 August 2016).
- Kildea, S.; Kruske, S.; Barclay, L.; Tracy, S. “Closing the Gap”: How maternity services can contribute to reducing poor maternal infant health outcomes for Aboriginal and Torres Strait Islander women. Rural Remote Health 2010, 10, 1383. [Google Scholar] [PubMed]
- Bertilone, C.; McEvoy, S.; Gower, D.; Naylor, N.; Doyle, J.; Swift-Otero, V. Elements of Cultural Competence in an Australian Aboriginal Maternity Program. Women Birth 2016, 16. [Google Scholar] [CrossRef] [PubMed]
- Dietsch, E.; Martin, T.; Shackleton, P.; Daview, C.; McLeod, M.; Alston, M. Australian Aboriginal kinship: A means to enhance maternal well-being. Women Birth 2011, 24, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Kruske, S. Culturally Competent Maternity Care for Aboriginal and Torres Strait Women Report; Prepared on Behalf of the Maternity Services Inter-Jurisdictional Committee for the Australian Health Ministers’ Advisory Council; Commonwealth of Australia: Canberra, Australia, 2012. [Google Scholar]
- Josif, C.M.; Barclay, L.; Kruske, S.; Kildea, S. “No more strangers”: Investigating the experiences of women, midwives and others during the establishment of a new model of maternity care for remote dwelling Aboriginal women in northern Australia. Midwifery 2014, 30, 147–162. [Google Scholar] [CrossRef] [PubMed]
- Kelly, J.; West, R.; Gamble, J.; Sidebotham, M.; Carson, V.; Duffy, E. “She knows how we feel”: Australian Aboriginal and Torres Strait Islander childbearing women’s experience of Continuity of Care with an Australian Aboriginal and Torres Strait Islander midwifery study. Women Birth 2014, 27, 157–162. [Google Scholar] [CrossRef] [PubMed]
- Dudgeon, P.; Wright, M.; Coffin, J. Talking it, and Walking it; cultural competence. J. Aust. Indig. Issues 2010, 13, 29–44. [Google Scholar]
- Hatem, M.; Sandall, J.; Devane, D.; Soltani, H.; Gates, S. “Midwife-Led versus Other Models of Care for Childbearing Women”, Cochrane Database of Systematic Referrals, Issue 4. Available online: http://mrw.interscience.wiley.com/cochrane/clsrev/articles/CD004667/frame.html (accessed on 3 October 2016).
- Australian Bureau of Statistics (2015) Births, Australia, 2014. Available online: http://www.abs.gov.au/AUSSTATS/[email protected]/DetailsPage/3301.02014?OpenDocument (accessed on 29 August 2016).
- Australian Institute of Health and Welfare. Australian Burden of Disease Study: Impact and Causes of Illness and Death in Aboriginal and Torres Strait Islander People 2011; Australian Burden of Disease Study Series No. 6. Cat. No. BOD 7; AIHW: Canberra, Austraila, 2016.
- Farrant, B.M.; Shepherd, C.C.J. Maternal ethnicity, stillbirth and neonatal death risk in Western Australia 1998–2010. Aust. N. Z. J. Obstet. Gynaecol. 2016, 56, 532–536. [Google Scholar] [CrossRef] [PubMed]
- Middleton, P.F. Preventing Infants Deaths among Aboriginal and Teenage Women in South Australia; The University of Adelaide: Adelaide, Australia, 2009. [Google Scholar]
- Fairthorne, J.; Walker, R.; De Klerk, N.; Shepherd, C. Early mortality from external causes in Aboriginal mothers: A retrospective cohort study. BMC Public Health 2016, 16. [Google Scholar] [CrossRef] [PubMed]
- Steering Committee for the Review of Government Service Provision. Overcoming Indigenous Disadvantage: Key Indicators; Australian Productivity Commission: Canberra, Australia, 2014.
- Arabena, K. Preachers, policies and power: The reproductive health of adolescent Aboriginal and Torres Strait Islander peoples in Australia. Health Promot. J. Aust. 2006, 17, 85–90. [Google Scholar]
- Zubrick, S.; Lawrence, D.; Silburn, S.; Blair, E.; Milroy, H.; Wilkes, E.; Eades, S.; D’Antoine, H.; Read, A.; Ishiguchi, P.; et al. The Western Australian Aboriginal Child Health Survey: The Health of Aboriginal Children and Young People; Perth Telethon Institute for Child health Research: Subiaco, Australia, 2004; Volume 1. [Google Scholar]
- WA Department of Health, WA Country Health Service. 2008. Available online: http://www.wacountry.health.wa.gov.au/fileadmin/sections/publications/Publications_by_topic_type/Maps/WACHS_M_Regions.pdf (accessed on 2 July 2016).
- Congress of Aboriginal and Torres Strait Islander Nurses and Midwives (CATSINaM). Towards a Shared Understanding of Terms and Concepts: Strengthening Nursing and Midwifery Care of Aboriginal and Torres Strait Islander Peoples, CATSINaM, Canberra. 2013. Available online: http://catsinam.org.au/static/uploads/files/catsinam-cultural-terms-2014-wfwxifyfbvdf.pdf (accessed on 3 October 2016).
- Thompson, G. Meeting the needs of adolescent parents and their children. Paediatr. Child Health 2016, 21, 273. [Google Scholar] [PubMed]
- SmithBattie, I. The vulnerabilities of teenage mothers: Challenging prevailing assumptions. Adv. Nurs. Sci. 2011, 23, 29–40. [Google Scholar] [CrossRef]
- Skinner, S.R.; Smith, J.; Fenwick, J.; Hendriks, J.; Fyfe, S.; Dendall, G. Pregnancy and protection: Perceptions, attitudes and experiences of Australian female adolescents. Women Birth 2011, 22, 50–56. [Google Scholar] [CrossRef] [PubMed]
- Lockyer, S.; Kite, E. Teenage pregnancies in East Pilbara Aboriginal communities. Aborig. Isl. Health Work. J. 2005, 30, 26–29. [Google Scholar]
- Heywood, W.; Patrick, K.; Smith, A.M.; Pitts, M.K. Associations between early first sexual intercourse and later sexual and reproductive outcomes: A systematic review of population-based data. Arch. Sex. Behav. 2015, 44, 531–569. [Google Scholar] [CrossRef] [PubMed]
- Marino, J.; Lewis, L.; Bateson, D.; Hickey, M.; Skinner, S. Teenage mothers. Aust. Fam. Physician 2016, 45, 712–717. [Google Scholar] [PubMed]
- Ritter, T.; Dore, A.; McGeechan, K. Contraceptive knowledge and attitudes among 14–24-year-olds in New South Wales, Australia. Aust. N. Z. J. Public Health 2015, 39, 267–269. [Google Scholar] [CrossRef] [PubMed]
- Marriott, R.; Ferguson-Hill, S. Perinatal and Infant Mental Health and Wellbeing. In Working Together: Aboriginal and Torres Strait Islander Mental Health and Wellbeing Principles and Practice, 2nd ed.; Dudgeon, P., Milroy, H., Walker, R., Eds.; Commonwealth of Australia, ACT: Canberra, Australia, 2014. [Google Scholar]
- Ruedinger, E.; Cox, J.E. Adolescent childbearing: Consequences and interventions. Curr. Opin. Pediatr. 2012, 24, 446–452. [Google Scholar] [CrossRef] [PubMed]
- Bessarab, D.; Ng’andu, B. Yarning about yarning as a legitimate method in indigenous research. Int. J. Crit. Indig. Stud. 2010, 3, 37–50. [Google Scholar]
- Reibel, T.; Walker, R. Antenatal services for Aboriginal women: The relevance of cultural competence. Qual. Prim. Care 2010, 18, 65–74. [Google Scholar] [PubMed]
| Pregnancy Topic | Summary of Participant Identified Strategies |
|---|---|
| Pre-Pregnancy Participants were asked what they understood about the local context in which service providers worked and who to speak with to develop knowledge of the community. |
|
| Pregnancy Participants were asked to consider what was needed to engage with young women early in pregnancy. |
|
| Relocation/Preparing to Birth Participants were asked to consider how they might go about planning relocation in consultation with the young woman. |
|
| Discharge/Relocation to Home Community Participants were asked to consider how they might go about planning and documenting a discharge for a young women for her return to the community. |
|
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reibel, T.; Wyndow, P.; Walker, R. From Consultation to Application: Practical Solutions for Improving Maternal and Neonatal Outcomes for Adolescent Aboriginal Mothers at a Local Level. Healthcare 2016, 4, 90. https://doi.org/10.3390/healthcare4040090
Reibel T, Wyndow P, Walker R. From Consultation to Application: Practical Solutions for Improving Maternal and Neonatal Outcomes for Adolescent Aboriginal Mothers at a Local Level. Healthcare. 2016; 4(4):90. https://doi.org/10.3390/healthcare4040090
Chicago/Turabian StyleReibel, Tracy, Paula Wyndow, and Roz Walker. 2016. "From Consultation to Application: Practical Solutions for Improving Maternal and Neonatal Outcomes for Adolescent Aboriginal Mothers at a Local Level" Healthcare 4, no. 4: 90. https://doi.org/10.3390/healthcare4040090





