The Concept of Missing Incidents in Persons with Dementia
Abstract
:1. Introduction
2. Methodology
3. Results and Discussion
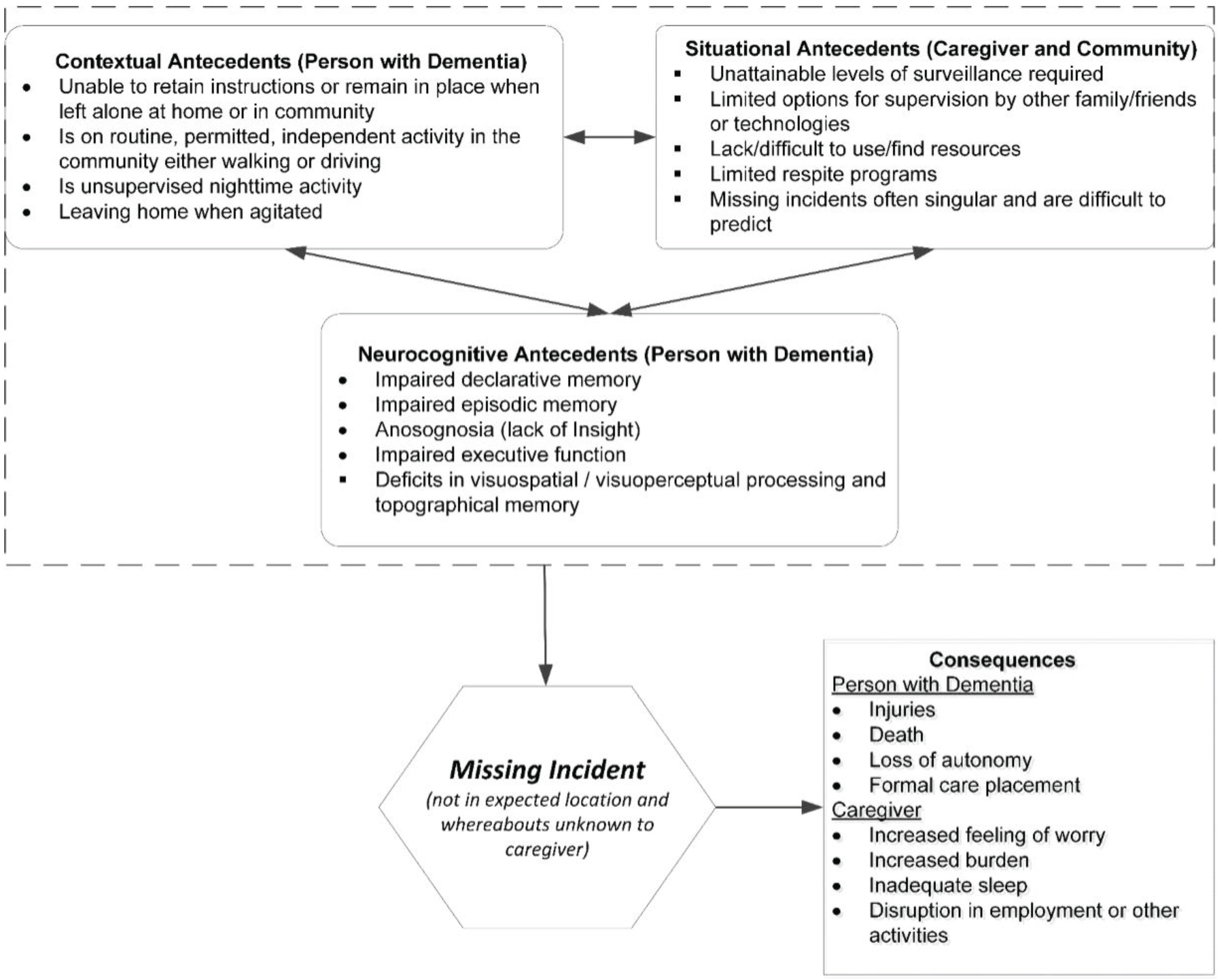
3.1. Antecedents
3.1.1. Contextual Antecedents
3.1.2. Situational Antecedents
3.1.3. Neurocognitive Antecedents
3.2. Missing Incident
3.3. Consequences
3.3.1. Consequences to PWD
3.3.2. Consequences to Caregiver
4. Conclusions

Acknowledgements
Author Contributions
Conflicts of Interest
References
- Rowe, M.A.; Vandeveer, S.S.; Greenblum, C.A.; List, C.N.; Fernandez, R.M.; Mixson, N.E.; Ahn, H.C. Persons with dementia missing in the community: Is it wandering or something unique? BMC Geriatr. 2011. [Google Scholar] [CrossRef] [PubMed]
- Algase, D.L.; Moore, D.H.; Vandeweerd, C.; Gavin-Dreschnack, D.J. Mapping the maze of terms and definitions in dementia-related wandering. Aging Ment. Health 2007, 11, 686–698. [Google Scholar] [CrossRef] [PubMed]
- Alzheimer’s Association. 2011 Alzheimer’s disease facts and figures. Alzheimers Dement. 2011, 7, 208–244. [Google Scholar]
- Bowen, M.E.; McKenzie, B.; Steis, M.; Rowe, M. Prevalence of and antecedents to dementia-related missing incidents in the community. Dement. Geriatr. Cogn. Disord. 2011, 31, 406–412. [Google Scholar] [CrossRef] [PubMed]
- Rowe, M.A.; Bennett, V. A look at deaths occurring in persons with dementia lost in the community. Am. J. Alzheimers Dis. Other Demen. 2003, 18, 343–348. [Google Scholar] [CrossRef] [PubMed]
- McShane, R.; Gedling, K.; Keene, J.; Fairburn, C.; Jacoby, R.; Hope, T. Getting lost in dementia: A longitudinal study of a behavioral symptom. Int. Psychogeriatr. 1998, 10, 253–260. [Google Scholar] [CrossRef] [PubMed]
- Kwok, T.C.; Yuen, K.S.; Ho, F.K.; Chan, W.M. Getting lost in the community: A phone survey on the community-dwelling demented people in Hong Kong. Int. J. Geriatr. Psychiatry 2010, 25, 427–432. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, D.; ni Mhaolain, A.; Crosby, L.; Ryan, D.; Lacey, L.; Coen, R.F.; Walsh, C.; Coakley, D.; Walsh, J.B.; Cunningham, C.; et al. Determinants of the desire to institutionalize in Alzheimer’s caregivers. Am. J. Alzheimers Dis. Other Demen. 2011, 26, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Rowe, M.A.; Glover, J.C. Antecedents, descriptions and consequences of wandering in cognitively-impaired adults and the Safe Return (SR) program. Am. J. Alzheimers Dis. Other Demen. 2001, 16, 344–352. [Google Scholar] [CrossRef] [PubMed]
- Rowe, M.A.; Greenblum, C.A.; Boltz, M.; Galvin, J.E. Missing drivers with dementia: Antecedents and recovery. J. Am. Geriatr. Soc. 2012, 60, 2063–2069. [Google Scholar] [CrossRef] [PubMed]
- Chung, J.C.; Lai, C.K. Elopement among community-dwelling older adults with dementia. Int. Psychogeriatr. 2011, 23, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Tu, M.; Pai, M.C. Getting lost for the first time in patients with Alzheimer’s disease. Int. Psychogeriatr. 2006, 18, 565–570. [Google Scholar] [CrossRef] [PubMed]
- Hunt, L.A.; Brown, A.E.; Gilman, I.P. Drivers with dementia and outcomes of becoming lost while driving. Am. J. Occup. Ther. 2010, 64, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Walker, A.E.; Livingston, G.; Cooper, C.A.; Katona, C.L.; Kitchen, G.L. Caregivers’ experience of risk in dementia: The LASER-AD study. Aging Ment. Health 2006, 10, 532–538. [Google Scholar] [CrossRef] [PubMed]
- Mahoney, D.F. Vigilance. Evolution and definition for caregivers of family members with Alzheimer’s disease. J. Gerontol. Nurs. 2003, 29, 24–30. [Google Scholar] [CrossRef] [PubMed]
- Lach, H.W.; Chang, Y.P. Caregiver perspectives on safety in home dementia care. West J. Nurs. Res. 2007, 29, 993–1014. [Google Scholar] [CrossRef] [PubMed]
- Alzheimer’s Association. 2013 Alzheimer’s disease facts and figures. Alzheimers Dement. 2013, 9, 208–245. [Google Scholar]
- Black, S.E.; Gauthier, S.; Dalziel, W.; Keren, R.; Correia, J.; Hew, H.; Binder, C. Canadian Alzheimer’s disease caregiver survey: Baby-boomer caregivers and burden of care. Int. J. Geriatr. Psychiatry 2010, 25, 807–813. [Google Scholar] [CrossRef] [PubMed]
- Fingerman, K.L.; Pillemer, K.A.; Silverstein, M.; Suitor, J.J. The baby boomers’ intergenerational relationships. Gerontologist 2012, 52, 199–209. [Google Scholar] [CrossRef] [PubMed]
- Rowe, M.A.; Ahn, H.; Benito, A.P.; Stone, H.; Wilson, A.; Kairalla, J. Injuries and unattended home exits in persons with dementia: A 12-month prospective study. Am. J. Alzheimers Dis. Other Demen. 2010, 25, 27–31. [Google Scholar] [CrossRef] [PubMed]
- Chiu, Y.C.; Algase, D.; Liang, J.; Liu, H.C.; Lin, K.N. Conceptualization and measurement of getting lost behavior in persons with early dementia. Int. J. Geriatr. Psychiatry 2005, 20, 760–768. [Google Scholar] [CrossRef] [PubMed]
- Houston, A.M.; Brown, L.M.; Rowe, M.A.; Barnett, S.D. The informal caregivers’ perception of wandering. Am. J. Alzheimers Dis. Other Demen. 2011, 26, 616–622. [Google Scholar] [CrossRef] [PubMed]
- Leicht, H.; Berwig, M.; Gertz, H.J. Anosognosia in Alzheimer’s disease: The role of impairment levels in assessment of insight across domains. J. Int. Neuropsychol. Soc. 2010, 16, 463–473. [Google Scholar] [CrossRef] [PubMed]
- Harwood, D.G.; Sultzer, D.L.; Wheatley, M.V. Impaired insight in Alzheimer disease: Association with cognitive deficits, psychiatric symptoms, and behavioral disturbances. Neuropsychiatry Neuropsychol. Behav. Neurol. 2000, 13, 83–88. [Google Scholar] [PubMed]
- Chiu, Y.C.; Algase, D.; Whall, A.; Liang, J.; Liu, H.C.; Lin, K.N.; Wang, P.N. Getting lost: Directed attention and executive functions in early Alzheimer’s disease patients. Dement. Geriatr. Cogn. Disord. 2004, 17, 174–180. [Google Scholar] [CrossRef] [PubMed]
- Alegret, M.; Boada-Rovira, M.; Vinyes-Junque, G.; Valero, S.; Espinosa, A.; Hernandez, I.; Modinos, G.; Rosende-Roca, M.; Mauleon, A.; Becker, J.T.; et al. Detection of visuoperceptual deficits in preclinical and mild Alzheimer’s disease. J. Clin. Exp. Neuropsychol. 2009, 31, 860–867. [Google Scholar] [CrossRef] [PubMed]
- Guerin, F.; Belleville, S.; Ska, B. Characterization of visuoconstructional disabilities in patients with probable dementia of Alzheimer’s type. J. Clin. Exp. Neuropsychol. 2002, 24, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Iachini, I.; Iavarone, A.; Senese, V.P.; Ruotolo, F.; Ruggiero, G. Visuospatial memory in healthy elderly, AD and MCI: A review. Curr. Aging Sci. 2009, 2, 43–59. [Google Scholar] [CrossRef] [PubMed]
- Adduri, C.A.; Marotta, J.J. Mental rotation of faces in healthy aging and Alzheimer’s disease. PLoS ONE 2009, 4, e6120. [Google Scholar] [CrossRef] [PubMed]
- Guariglia, C.C.; Nitrini, R. Topographical disorientation in Alzheimer’s disease. Arq. Neuropsiquiatr. 2009, 67, 967–972. [Google Scholar] [CrossRef] [PubMed]
- Cheng, P.J.; Pai, M.C. Dissociation between recognition of familiar scenes and of faces in patients with very mild Alzheimer disease: An event-related potential study. Clin. Neurophysiol. 2010, 121, 1519–1525. [Google Scholar] [CrossRef] [PubMed]
- Albert, S.G.; Nakra, B.R.; Grossberg, G.T.; Caminal, E.R. Drinking behavior and vasopressin responses to hyperosmolality in Alzheimer’s disease. Int. Psychogeriatr. 1994, 6, 79–86. [Google Scholar] [CrossRef] [PubMed]
- Koester, R.J.; Stooksbury, D.E. Behavioral profile of possible Alzheimer’s disease patients in Virginia search and rescue incidents. Wilderness Environ. Med. 1995, 6, 34–43. [Google Scholar] [CrossRef]
- Rowe, M.A.; Fehrenbach, N. Injuries sustained by community-dwelling individuals with dementia. Clin. Nurs. Res. 2004, 13, 98–110. [Google Scholar] [CrossRef] [PubMed]
- Rowe, M.A.; Feinglass, N.G.; Wiss, M.E. Persons with dementia who become lost in the community: A case study, current research, and recommendations. Mayo Clin. Proc. 2004, 79, 1417–1422. [Google Scholar] [CrossRef] [PubMed]
- Hope, T.; Keene, J.; McShane, R.H.; Fairburn, C.G.; Gedling, K.; Jacoby, R. Wandering in dementia: A longitudinal study. Int. Psychogeriatr. 2001, 13, 137–147. [Google Scholar] [CrossRef] [PubMed]
- Di Mattei, V.E.; Prunas, A.; Novella, L.; Marcone, A.; Cappa, S.F.; Sarno, L. The burden of distress in caregivers of elderly demented patients and its relationship with coping strategies. Neurol. Sci. 2008, 29, 383–389. [Google Scholar] [CrossRef] [PubMed]
- Lim, Y.M.; Son, G.R.; Song, J.A.; Beattie, E. Factors affecting burden of family caregivers of community-dwelling ambulatory elders with dementia in Korea. Arch Psychiatr. Nurs. 2008, 22, 226–234. [Google Scholar] [CrossRef] [PubMed]
- McCurry, S.M.; Logsdon, R.G.; Teri, L.; Gibbons, L.E.; Kukull, W.A.; Bowen, J.D.; McCormick, W.C.; Larson, E.B. Characteristics of sleep disturbance in community-dwelling Alzheimer’s disease patients. J. Geriatr. Psychiatry Neurol. 1999, 12, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Spring, H.J.; Rowe, M.A.; Kelly, A. Improving caregivers’ well-being by using technology to manage nighttime activity in persons with dementia. Res. Gerontol. Nurs. 2009, 2, 39–48. [Google Scholar] [CrossRef] [PubMed]
- Creese, J.; Bedard, M.; Brazil, K.; Chambers, L. Sleep disturbances in spousal caregivers of individuals with Alzheimer’s disease. Int. Psychogeriatr. 2008, 20, 149–161. [Google Scholar] [CrossRef] [PubMed]
- McCurry, S.M.; Logsdon, R.G.; Teri, L.; Vitiello, M.V. Sleep disturbances in caregivers of persons with dementia: Contributing factors and treatment implications. Sleep Med. Rev. 2007, 11, 143–153. [Google Scholar] [CrossRef] [PubMed]
- Rowe, M.A.; McCrae, C.S.; Campbell, J.M.; Benito, A.P.; Cheng, J. Sleep pattern differences between older adult dementia caregivers and older adult noncaregivers using objective and subjective measures. J. Clin. Sleep Med. 2008, 4, 362–369. [Google Scholar] [PubMed]
- Ohayon, M.M.; Roth, T. Place of chronic insomnia in the course of depressive and anxiety disorders. J. Psychiatr. Res. 2003, 37, 9–15. [Google Scholar] [CrossRef]
- Spira, A.P.; Friedman, L.; Flint, A.; Sheikh, J.I. Interaction of sleep disturbances and anxiety in later life: Perspectives and recommendations for future research. J. Geriatr. Psychiatry Neurol. 2005, 18, 109–115. [Google Scholar] [CrossRef] [PubMed]
- Spira, A.P.; Friedman, L.; Beaudreau, S.A.; Ancoli-Israel, S.; Hernandez, B.; Sheikh, J.; Yesavage, J. Sleep and physical functioning in family caregivers of older adults with memory impairment. Int. Psychogeriatr. 2010, 22, 306–311. [Google Scholar] [CrossRef] [PubMed]
- Elwood, P.C.; Bayer, A.J.; Fish, M.; Pickering, J.; Mitchell, C.; Gallacher, J.E. Sleep disturbance and daytime sleepiness predict vascular dementia. J. Epidemiol. Community Health 2011, 65, 820–824. [Google Scholar] [CrossRef] [PubMed]
- Haimov, I.; Hanuka, E.; Horowitz, Y. Chronic insomnia and cognitive functioning among older adults. Behav. Sleep Med. 2008, 6, 32–54. [Google Scholar] [CrossRef] [PubMed]
- Alzheimer’s Association. 2012 Alzheimer’s disease facts and figures. Alzheimers Dement. 2012, 8, 131–168. [Google Scholar]
- The Metlife Caregiving Cost Study: Productivity Losses to U.S. Business; MetLife Mature Market Institute: Westport, CT, USA, 2006.
- Klein, D.A.; Steinberg, M.; Galik, E.; Steele, C.; Sheppard, J.M.; Warren, A.; Rosenblatt, A.; Lyketsos, C.G. Wandering behaviour in community-residing persons with dementia. Int. J. Geriatr. Psychiatry 1999, 14, 272–279. [Google Scholar] [CrossRef]
- Covinsky, K.E.; Eng, C.; Lui, L.Y.; Sands, L.P.; Sehgal, A.R.; Walter, L.C.; Wieland, D.; Eleazer, G.P.; Yaffe, K. Reduced employment in caregivers of frail elders: Impact of ethnicity, patient clinical characteristics, and caregiver characteristics. J. Gerontol. Ser. A 2001, 56, M707–M713. [Google Scholar] [CrossRef]
- McKenzie, B.; Bowen, M.E.; Keys, K.; Bulat, T. Safe home program: A suite of technologies to support extended home care of persons with dementia. Am. J. Alzheimers Dis. Other Demen. 2013, 28, 348–354. [Google Scholar] [CrossRef] [PubMed]
- Petonito, G.; Wuschert, G.W.; Carr, D.C.; Kinney, J.M.; Robbins, E.J.; Brown, J.S. Programs to locate missing and critically wandering elders: A critical review and a call for multiphasic evaluation. Gerontologist 2013, 53, 17–25. [Google Scholar] [CrossRef] [PubMed]
- Alzheimer’s Initiatives. Available online: www.iacp.org/alzheimers (accessed on 20 September 2015).
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rowe, M.; Houston, A.; Molinari, V.; Bulat, T.; Bowen, M.E.; Spring, H.; Mutolo, S.; McKenzie, B. The Concept of Missing Incidents in Persons with Dementia. Healthcare 2015, 3, 1121-1132. https://doi.org/10.3390/healthcare3041121
Rowe M, Houston A, Molinari V, Bulat T, Bowen ME, Spring H, Mutolo S, McKenzie B. The Concept of Missing Incidents in Persons with Dementia. Healthcare. 2015; 3(4):1121-1132. https://doi.org/10.3390/healthcare3041121
Chicago/Turabian StyleRowe, Meredeth, Amy Houston, Victor Molinari, Tatjana Bulat, Mary Elizabeth Bowen, Heather Spring, Sandra Mutolo, and Barbara McKenzie. 2015. "The Concept of Missing Incidents in Persons with Dementia" Healthcare 3, no. 4: 1121-1132. https://doi.org/10.3390/healthcare3041121




