Pediatric Coccidioidomycosis Patients: Perceptions, Quality of Life and Psychosocial Factors
Abstract
:1. Introduction
1.1. Coccidioidomycosis
1.2. Diagnosing Coccidioidomycosis
1.3. Children with Coccidioidomycosis
1.4. Psychosocial Aspects of Coccidioidomycosis
1.5. Specific Aims
2. Research Design
2.1. Methods
2.2. Procedures
2.3. Data Collection from Primary Caregivers
- Detection
- (1)
- How (and where/by whom) is coccidioidomycosis detected by child patients, their families and their healthcare systems?
- (2)
- What causes delays in diagnosis?
- Access to Care
- (3)
- What barriers impede patients and families’ access to care/treatment?
- (4)
- What (information, support, etc.) do patients and families feel that they need?
- Experience
- (5)
- What difficulties (physical, psychosocial, etc.) do patients and families face as a result of having pediatric coccidioidomycosis?
- (6)
- What myths about coccidioidomycosis do patients and families currently hold?
2.4. Quality of Life Scales with Pediatric Patients
2.5. Drawing Task with Pediatric Patients
2.6. Child Illness Perception Questionnaire with Pediatric Patients
2.7. Child Coping Scale with Pediatric Patients
2.8. Triangulation between Data from Primary Caregivers and Pediatric Patients
3. Results
3.1. Participants
3.2. Exploratory Interviews
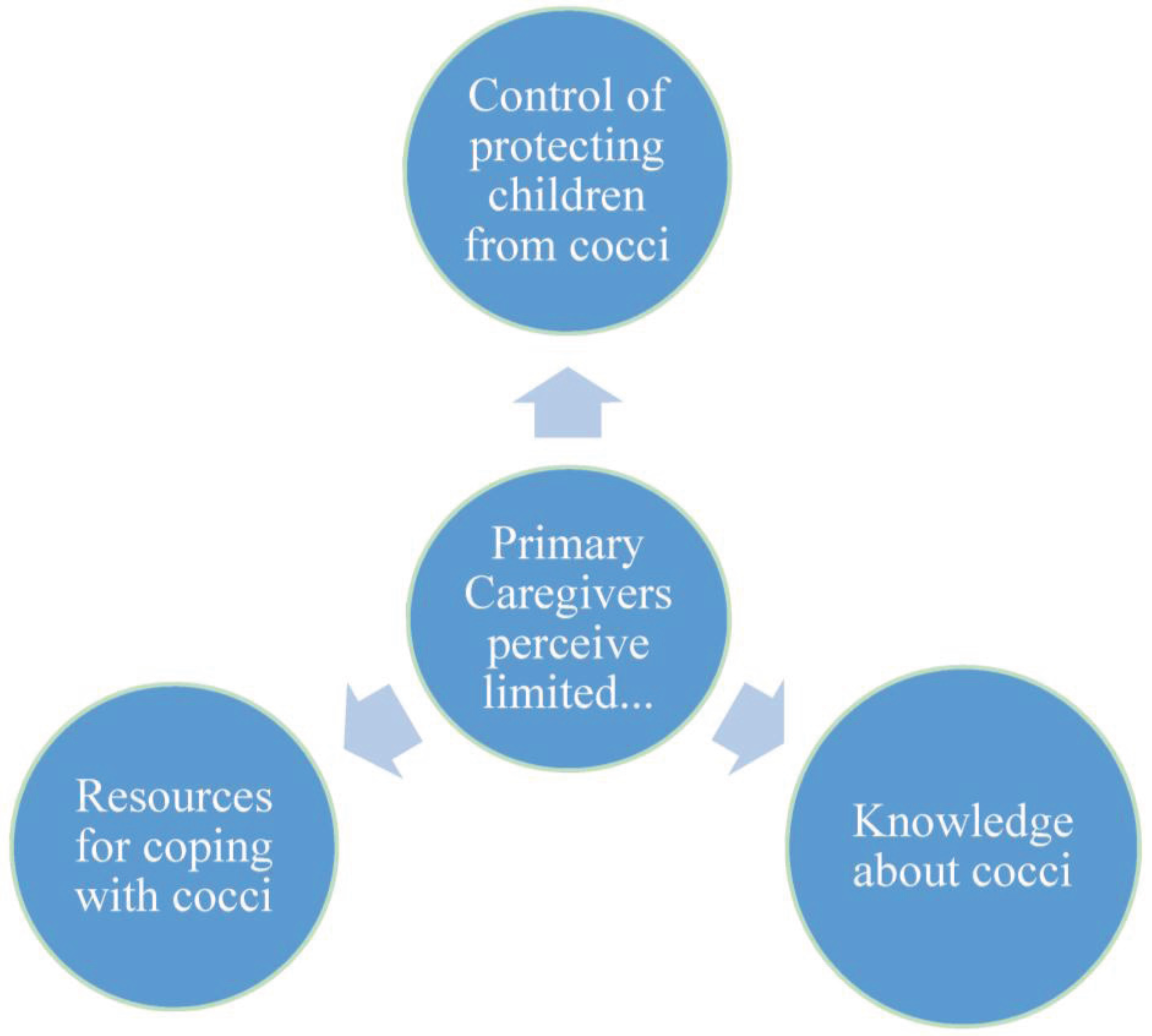
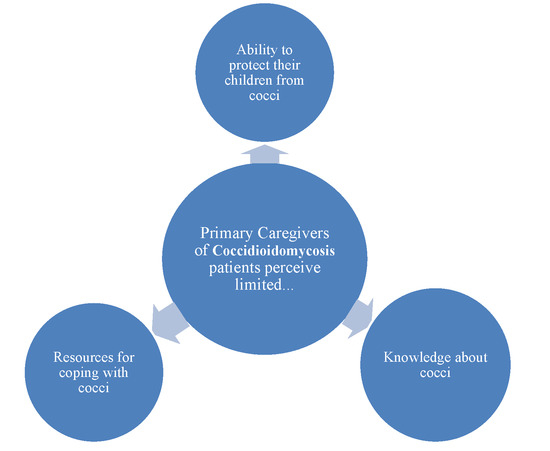
3.2.1. Lack of Control
3.2.2. Lack of Knowledge
I mean I heard about it [Valley Fever] but it’s like this myth through this valley one person will says this little thing about it or somebody nobody really, really discussed (.) you know and especially in the hospital [beyond the specialist clinic]; you ask them they have no clue what valley fever really even is...you hear like I said it’s a myth you’d hear someone say ‘oh my great uncle 20 years ago got it, or this that and the other. Never really anything significant.—Parent H.
3.2.3. Limited Resources
“I was you know disability family disability doesn’t pay (laughs) so the amount of what I actually got on my paycheck was it a financial strain? Oh hell yeah in between driving um (.) Dad coming back and forth the whole time I was up there me not having my wages while I was up there um food because food at children’s is expensive you know hers is taken care of mines not um so I mean that’s so I was lucky they’re were able to do the ’fridgerator for me and there and stuff so it did help I’d go to the grocery store and pick up a few things here and there but um man the cost was bad (.) it was hard.”—Parent C.
3.3. Primary Caregiver Survey Results
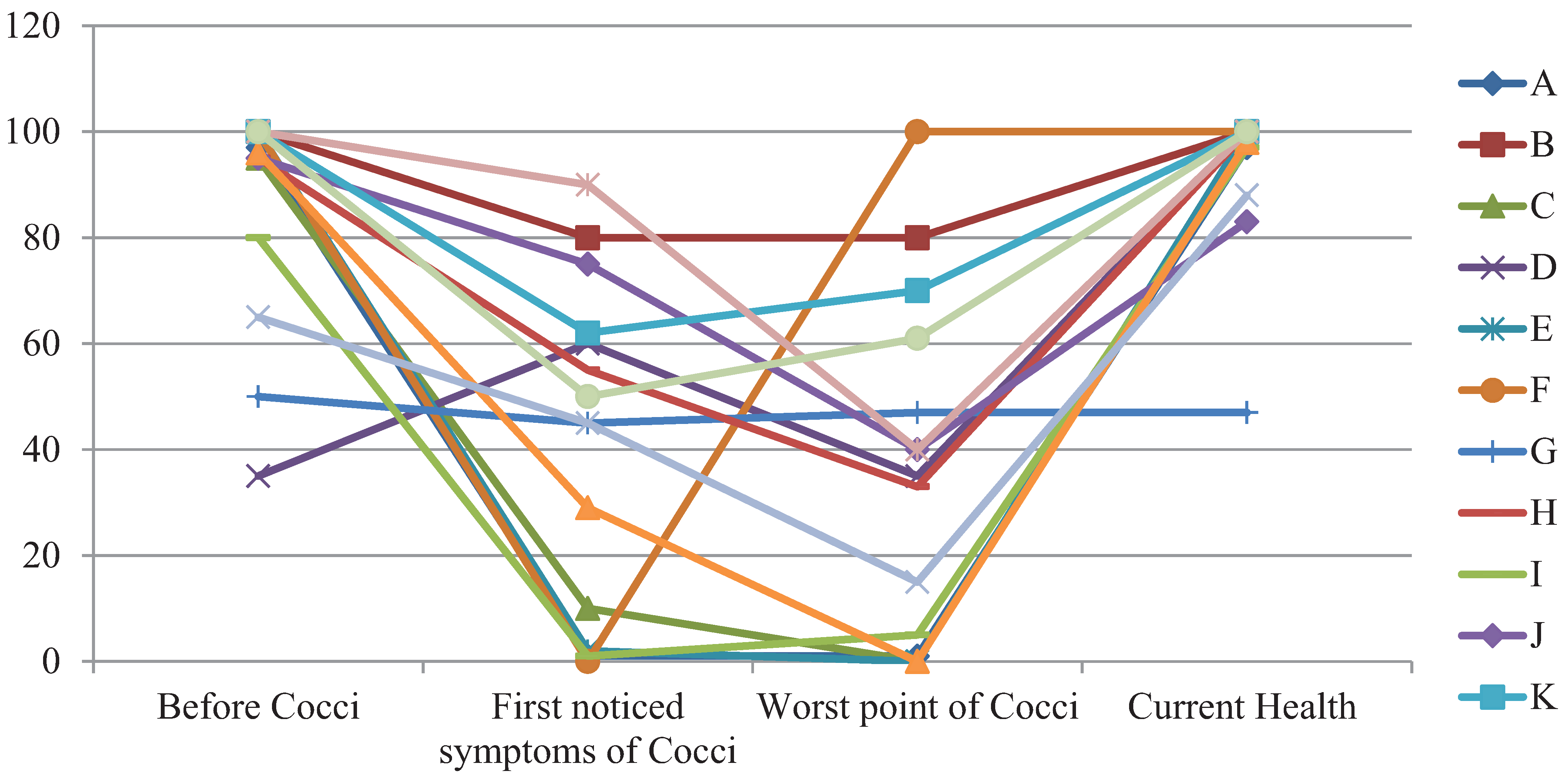
3.4. Children’s Quality Life Scale Results
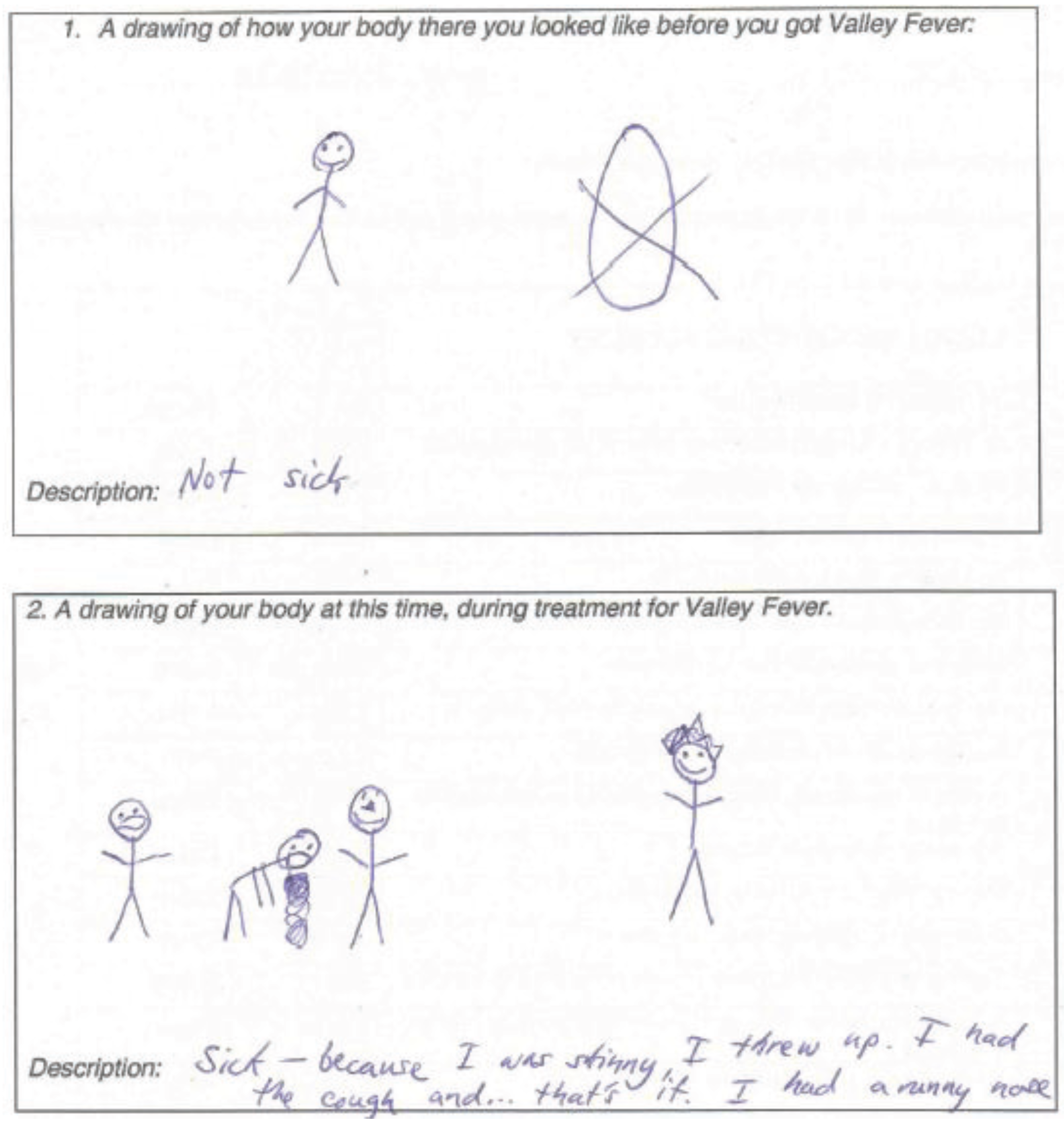
3.5. Children’s Drawing Task Results

3.6. Children’s Illness Perceptions
3.7. Children’s Coping Strategies

4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Johnson, L.; Gaab, E.M.; Sanchez, J.; Bui, P.Q.; Nobile, C.J.; Hoyer, K.K.; Peterson, M.W.; Ojcius, D.M. Valley fever: Danger lurking in a dust cloud. Microbes Infect. 2014, 16, 591–600. [Google Scholar] [CrossRef] [PubMed]
- Pappagianis, D. Coccidioidomycosis. Semin. Dermatol. 1993, 12, 301–309. [Google Scholar] [PubMed]
- Chiller, T.M.; Galgiani, J.N.; Stevens, D.A. Coccidioidomycosis. Infect. Dis. Clin. North Am. 2003, 17, 41–57. [Google Scholar] [CrossRef]
- Smith, C.E. Epidemiology of acute coccidioidomycosis with erythema nodosum (“San Joaquin” or “Valley Fever”). Am. J. Public Health Nation’s Health 1940, 30, 600–611. [Google Scholar] [CrossRef]
- Flaherman, V.J.; Hector, R.; Rutherford, G.W. Estimating severe coccidioidomycosis in California. Emerg. Infect. Dis. 2007, 13, 1087–1890. [Google Scholar] [CrossRef] [PubMed]
- Center for Infectious Diseases—Division of Communicable Disease Control, Infectious Diseases Branch—Surveillance and Statistics. Epidemiologic Summary of Coccidioidomycosis in California, 2009–2012. Available online: http://www.cdph.ca.gov/programs/sss/Documents/CocciEpiSummary09-12.pdf (accessed on 3 March 2015).
- Mac Lean, M.L. Coccidioidal Meningitis in Kings County. Available online: http://www.countyofkings.com/home/showdocument?id=732 (accessed on 3 March 2015).
- Galgiani, J.N. Coccidioidomycosis: Changing perceptions and creating opportunities for its control. Ann. N. Y. Acad. Sci. 2007, 1111, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Kirkland, T.N.; Fierer, J. Coccidioidomycosis: A reemerging infectious disease. Emerg. Infect. Dis. 1996, 2, 192–199. [Google Scholar] [CrossRef] [PubMed]
- Chu, J.H.; Feudtner, C.; Heydon, K.; Walsh, T.J.; Zaoutis, T.E. Hospitalizations for endemic mycoses: A population-based national study. Clin. Infect. Dis. 2006, 42, 822–825. [Google Scholar] [CrossRef] [PubMed]
- Connelly, M.B.; Zerella, J.T. Surgical management of coccidioidomycosis in children. J. Pediatr. Surg. 2000, 35, 1633–1634. [Google Scholar] [CrossRef] [PubMed]
- Fisher, B.T.; Chiller, T.M.; Prasad, P.A.; Beveridge, M.; Walsh, T.J.; Zaoutis, T.E. Hospitalizations for coccidioidomycosis at forty-one children’s hospitals in the United States. Pediatr. Infect. Dis. J. 2010, 29, 243–247. [Google Scholar] [CrossRef] [PubMed]
- McCarty, J.M.; Demetral, L.C.; Dabrowski, L.; Kahal, A.K.; Bowser, A.M.; Hahn, J.E. Pediatric coccidioidomycosis in central California: A retrospective case series. Clin. Infect. Dis. 2013, 56, 1179–1185. [Google Scholar] [CrossRef] [PubMed]
- Homans, J.D.; Spencer, L. Itraconazole treatment of nonmeningeal coccidioidomycosis in children: Two case reports and review of the literature. Pediatr. Infect. Dis. J. 2010, 29, 65–67. [Google Scholar] [CrossRef] [PubMed]
- Galgiani, J.N.; Ampel, N.M.; Blair, J.E.; Catanzaro, A.; Johnson, R.H.; Stevens, D.A.; Williams, P.L.; Infectious Diseases Society of America. Coccidioidomycosis. Clin. Infect. Dis. 2005, 41, 1217–1223. [Google Scholar] [CrossRef] [PubMed]
- Bercovitch, R.S.; Catanzaro, A.; Schwartz, B.S.; Pappagianis, D.; Watts, D.H.; Ampel, N.M. Coccidioidomycosis during pregnancy: A review and recommendations for management. Clin. Infect. Dis. 2011, 53, 363–368. [Google Scholar] [CrossRef] [PubMed]
- Smale, L.E.; Waechter, K.G. Dissemination of coccidioidomycosis in pregnancy. Am. J. Obstet. Gynecol. 1970, 107, 356–361. [Google Scholar] [PubMed]
- Galgiani, J.; Coull, B.; Kauffman, C.A.; Thorner, A.R. Coccidioidal Meningitis; Up to Date Online: Wellesley, MA, USA, 2004; Volume 12. [Google Scholar]
- Wack, E.E.; Ampel, N.M.; Galgiani, J.N.; Bronnimann, D.A. Coccidioidomycosis during pregnancy. An analysis of ten cases among 47,120 pregnancies. CHEST J. 1988, 94, 376–379. [Google Scholar] [CrossRef]
- Geertsma, F.; Ross, L.; Krogstad, P.; Cocci Study Group, California, CA, USA. Personal Communication, 2013.
- Snyder, C.H. Coccidioidal meningitis presenting as memory loss. J. Am. Acad. Nurse Pract. 2005, 17, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Barnato, A.E.; Sanders, G.D.; Owens, D.K. Cost-effectiveness of a potential vaccine for Coccidioides immitis. Emerg. Infect. Dis. 2001, 7, 797–806. [Google Scholar] [CrossRef] [PubMed]
- Ravens-Sieberer, U.; Auquier, P.; Erhart, M.; Gosch, A.; Rajmil, L.; Bruil, J.; Czemy, L. The KIDSCREEN-27 quality of life measure for children and adolescents: Psychometric results from a cross-cultural survey in 13 European countries. Qual. Life Res. 2007, 16, 1347–1356. [Google Scholar] [CrossRef] [PubMed]
- Weinman, J.; Petrie, K.J.; Moss-Morris, R.; Horne, R. The illness perception questionnaire: A new method for assessing the cognitive representation of illness. Psychol. Health 1996, 11, 431–445. [Google Scholar] [CrossRef]
- Walker, C.; Papadopoulos, L.; Lipton, M.; Hussein, M. The importance of children’s illness beliefs: The children’s illness perception questionnaire (CIPQ) as a reliable assessment tool for eczema and asthma. Psychol. Health Med. 2006, 11, 100–107. [Google Scholar] [CrossRef] [PubMed]
- Pretzlik, U.; Sylva, K. Paediatric patients’ distress and coping during medical treatment: A self report measure. Arch. Dis. Child. 1999, 81, 525–527. [Google Scholar] [CrossRef] [PubMed]
- Spirito, A.; Stark, L.J.; Williams, C. Development of a brief checklist to assess coping in pediatric patients. J. Pediatr. Psychol. 1988, 13, 555–574. [Google Scholar] [CrossRef] [PubMed]
- Connor-Smith, J.K.; Compas, B.E.; Wadsworth, M.E.; Thomsen, A.H.; Saltzman, H. Responses to stress in adolescence: Measurement of coping and involuntary stress responses. J. Consult. Clin. Psychol. 2000, 68, 976–992. [Google Scholar] [CrossRef] [PubMed]
- Keefe, F.J.; Caldwell, D.S.; Queen, K.T.; Gil, K.M.; Martinez, S.; Crisson, J.E.; Nunley, J. Pain coping strategies in osteoarthritis patients. J. Consult. Clin. Psychol. 1987, 55, 208–212. [Google Scholar] [CrossRef] [PubMed]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Lucile Packard Foundation for Children’s Health. Kidsdata.org: A program of the Lucile Packard Foundation for Children’s Health. Available online: http://www.kidsdata.org (accessed on 1 May 2013).
- Uzark, K.; Jones, K.; Slusher, J.; Limbers, C.A.; Burwinkle, T.M.; Varni, J.W. Quality of life in children with heart disease as perceived by children and parents. Pediatrics 2008, 121, e1060–e1067. [Google Scholar] [CrossRef] [PubMed]
- Townsend, M.; Feeny, D.H.; Guyatt, G.H.; Furlong, W.J.; Seip, A.E.; Dolovich, J. Evaluation of the burden of illness for pediatric asthmatic patients and their parents. Ann. Allergy 1991, 67, 403–408. [Google Scholar] [PubMed]
- Myant, K.A.; Williams, J.M. Children’s concepts of health and illness: Understanding of contagious illnesses, non-contagious illnesses and injuries. J. Health Psychol. 2005, 10, 805–819. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal, and Coping; Springer Publishing Company: New York, NY, USA, 1984; Volume 725. [Google Scholar]
- Henderson, P.A.; Kelbey, T.J.; Engebretson, K.M. Effects of a stress-control program on children’s locus of control, self-concept, and coping behavior. School Couns. 1992, 40, 125–130. [Google Scholar]
- Smith, C.; Carlson, B.E. Stress, coping, and resilience in children and youth. Soc. Serv. Rev. 1997, 71, 231–256. [Google Scholar] [CrossRef]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gaab, E.M.; Naeem, F. Pediatric Coccidioidomycosis Patients: Perceptions, Quality of Life and Psychosocial Factors. Healthcare 2015, 3, 775-795. https://doi.org/10.3390/healthcare3030775
Gaab EM, Naeem F. Pediatric Coccidioidomycosis Patients: Perceptions, Quality of Life and Psychosocial Factors. Healthcare. 2015; 3(3):775-795. https://doi.org/10.3390/healthcare3030775
Chicago/Turabian StyleGaab, Erin Mary, and Fouzia Naeem. 2015. "Pediatric Coccidioidomycosis Patients: Perceptions, Quality of Life and Psychosocial Factors" Healthcare 3, no. 3: 775-795. https://doi.org/10.3390/healthcare3030775