Qualitative and Quantitative Outcomes of a 1:1 Multidisciplinary Weight Management Clinic
Abstract
:1. Introduction
1.1. The Obesity Epidemic
1.2. The Problem—Wales
1.3. The Problem—Aneurin Bevan Health Board
1.4. The All Wales Obesity Pathway
1.5. Level 3 Service
1.6. The 1:1 Multidisciplinary Weight Management Clinic
1.7. Current Literature
1.8. Objectives
2. Methodology
| Key Items for Auditing | Question Number on Data Collection Form |
|---|---|
| Treatment length | 1 |
| Weight Loss | 2 |
| Preference of group or individual appointments | 3 |
| Activity levels | 4a |
| Confidence levels | |
| Diet improvement | |
| Usefulness of meeting Nurse | 4b |
| Usefulness of meeting Doctor | |
| Usefulness of meeting Dietitian | |
| Usefulness of meeting Counsellor | |
| Usefulness of meeting Physiotherapist | |
| Encouragement to lead healthy lifestyle | 5 |
| Health improvement | 6 |
| Medication change—blood pressure | 7 |
| Medication change—asthma | |
| Medication change—painkillers | |
| Medication change—cholesterol | |
| Medication change—diabetes/insulin | |
| Medication change—angina | |
| Medication change—antidepressants | |
| Medication change—Other/over-the-counter | |
| Recommendation of clinic to others | 8 |
| Employment status | 9a |
| Reduction in sick days | 9b |
| Suggestions for improvement of clinic | 10 |
| Any further comments | 11 |
2.1. Pilot Study
2.2. Scope
- -
- All active patients attending the MDWMC were eligible for interview—time since referral was not cause for exclusion.
- -
- New patients visiting clinic for the first occasion were excluded from interview.
- -
- Discharged patients, patients lapsing at six months, and patients who did not attend clinic were not interviewed.
2.3. Data Collection
2.4. Data Analysis
3. Results
3.1. How Long Have You Been Attending the Clinic?
| Category | <3 Months | 3–6 Months | 6–12 Months | >12 Months | No Response | Total |
|---|---|---|---|---|---|---|
| No. patients | 43 | 27 | 56 | 53 | 1 | 180 |
3.2. Have You Lost Weight since Attending the Clinic?
| Category | <3 Months | 3–6 Months | 6–12 Months | >12 Months | No Response | Total |
|---|---|---|---|---|---|---|
| Lost weight | 26 | 23 | 54 | 50 | 1 | 154 |
| Not lost weight | 17 | 4 | 2 | 3 | 0 | 26 |
| % Weight Loss | 5% | 10% | Total |
|---|---|---|---|
| n | 45 | 46 | 124 |
| % | 36 | 37 | 73 |
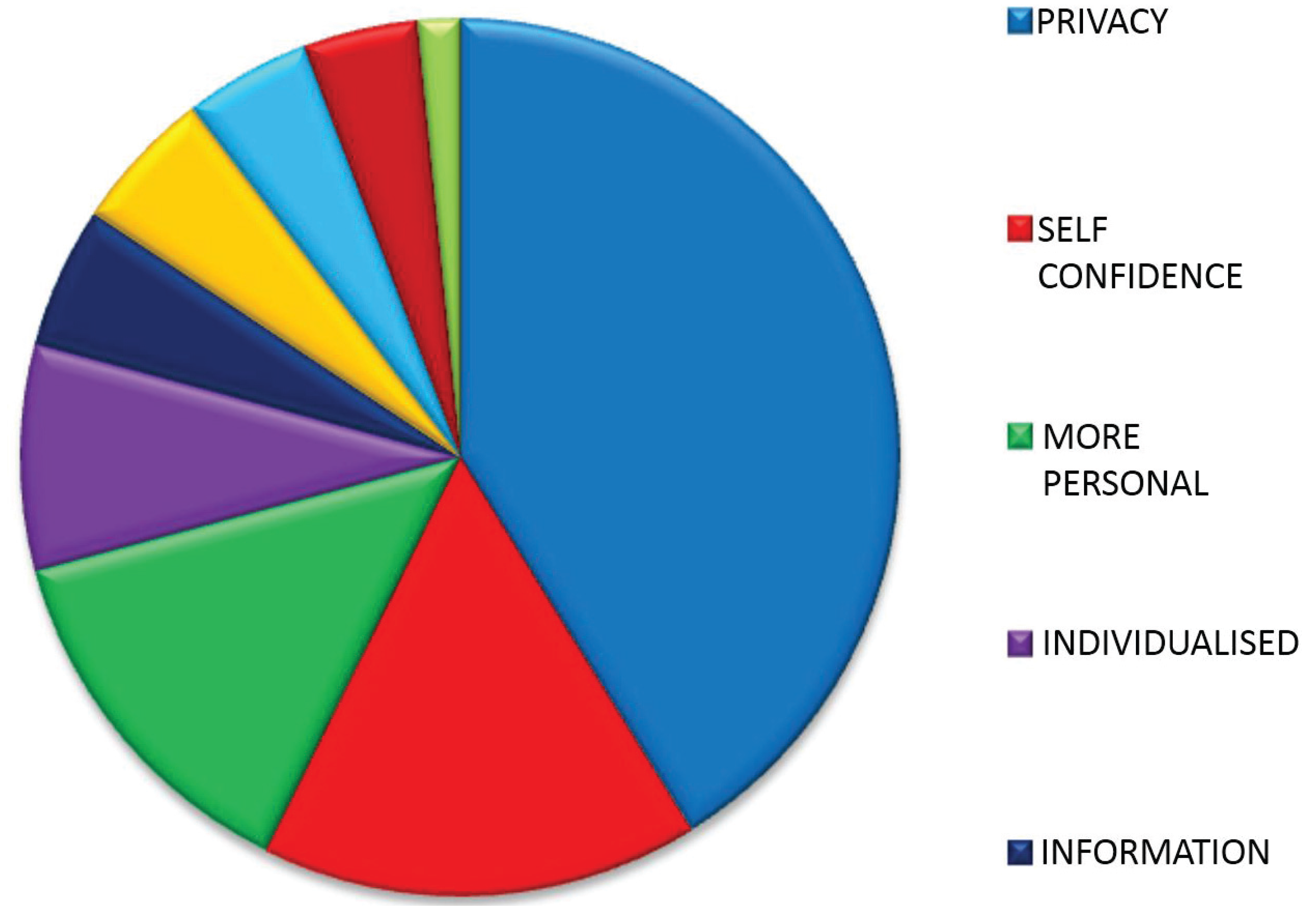
3.3. If You Were Offered a Choice of Appointment Type, Which Would You Choose—Individual Appointment or Group? Please Comment on Your Choice
Preference for Individual Appointments
| Category | n | % |
|---|---|---|
| Privacy | 79 | 41 |
| Self Confidence | 31 | 16 |
| More Personal | 26 | 14 |
| Personal Issues | 16 | 8 |
| Individualised Information | 10 | 5 |
| Both | 10 | 5 |
| Dislikes Groups | 9 | 5 |
| No Benefits | 8 | 4 |
| Takes Less Time | 3 | 2 |
| Total | 192 | 100 |
| Category | Meaning | Patient Quotes |
|---|---|---|
| Privacy | Desire a private arena to discuss their weight | “It’s more private” |
| “My weight is a private issue” | ||
| “I prefer to talk in private as I suffer from panic attacks” | ||
| Self Confidence | Feel uncomfortable discussing weight in front of other patients | “I’m embarrassed to talk about my weight in a group” |
| “I wouldn’t have the confidence to speak up in a group” | ||
| More Personal | Prefer to establish a personal relationship with healthcare professional | “I like building up a rapport with the clinicians” |
| “As I get to know the clinicians I feel I can open up more” | ||
| Personal Issues | Wish to discuss issues which they feel are personal to them | “My weight is a personal issue and I need the full attention of a healthcare professional” |
| “You can focus on personal issues in an individual appointment” | ||
| Individualised Information | Seek information which they feel needs tailoring to their individual situation | “I prefer talking to clinicians” |
| “Hearing the information face to face makes it seem more important” | ||
| Both | Would like to attend individual appointments and groups | “It would be good to attend a group as well later on” |
| “I’d like to attend a group as well to help keep me motivated on a more regular basis” | ||
| Dislikes Groups | Dislike group settings | “I don’t like groups” |
| No Benefits | Have not benefitted from groups in past | “I haven’t benefitted from groups in the past” |
| “Individual appointments are more motivating” | ||
| Takes Less Time | Individual appointments take less time to address issues | “It takes less time” |
3.4. Lifestyle Change

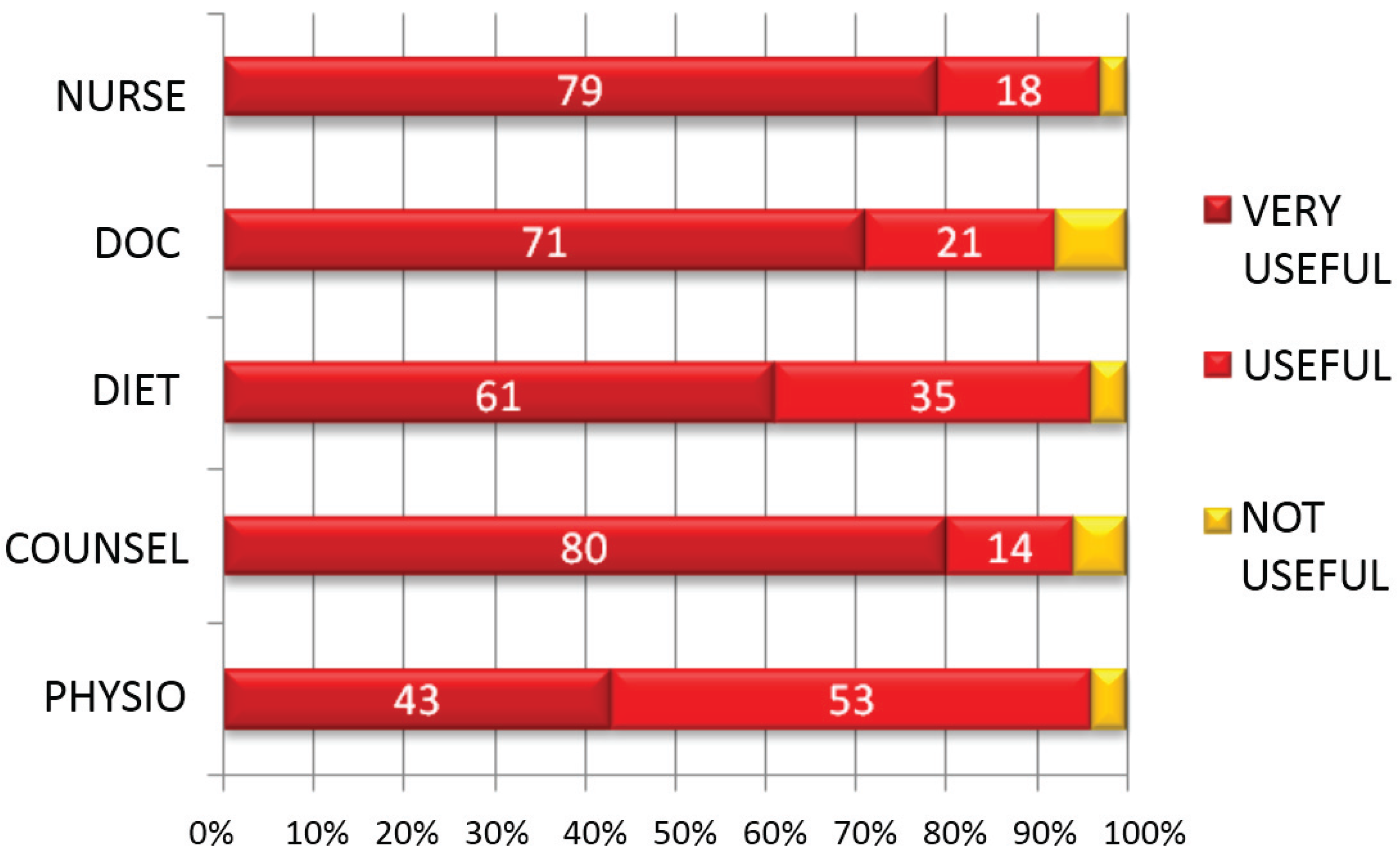
3.5. Efficacy of MDT Consultations
| Category | Agree (n) | Disagree (n) | Total (n) |
|---|---|---|---|
| Improved Diet | 161 | 19 | 180 |
| More Confident | 116 | 64 | 180 |
| More Active | 133 | 47 | 180 |
| No. of Patients Who Saw Team Member | Nurse | Doctor | Dietitan | Counsellor | Physiotherapist | Max |
|---|---|---|---|---|---|---|
| n | 180 | 180 | 110 | 106 | 23 | 180 |
| % | 100 | 100 | 61 | 59 | 13 | 100 |
| Category | Very Useful (%) | Useful (%) | Not Useful (%) |
|---|---|---|---|
| Nurse | 79 | 18 | 3 |
| Doctor | 71 | 21 | 8 |
| Dietitian | 61 | 35 | 4 |
| Counsellor | 80 | 14 | 6 |
| Physio | 43 | 53 | 4 |
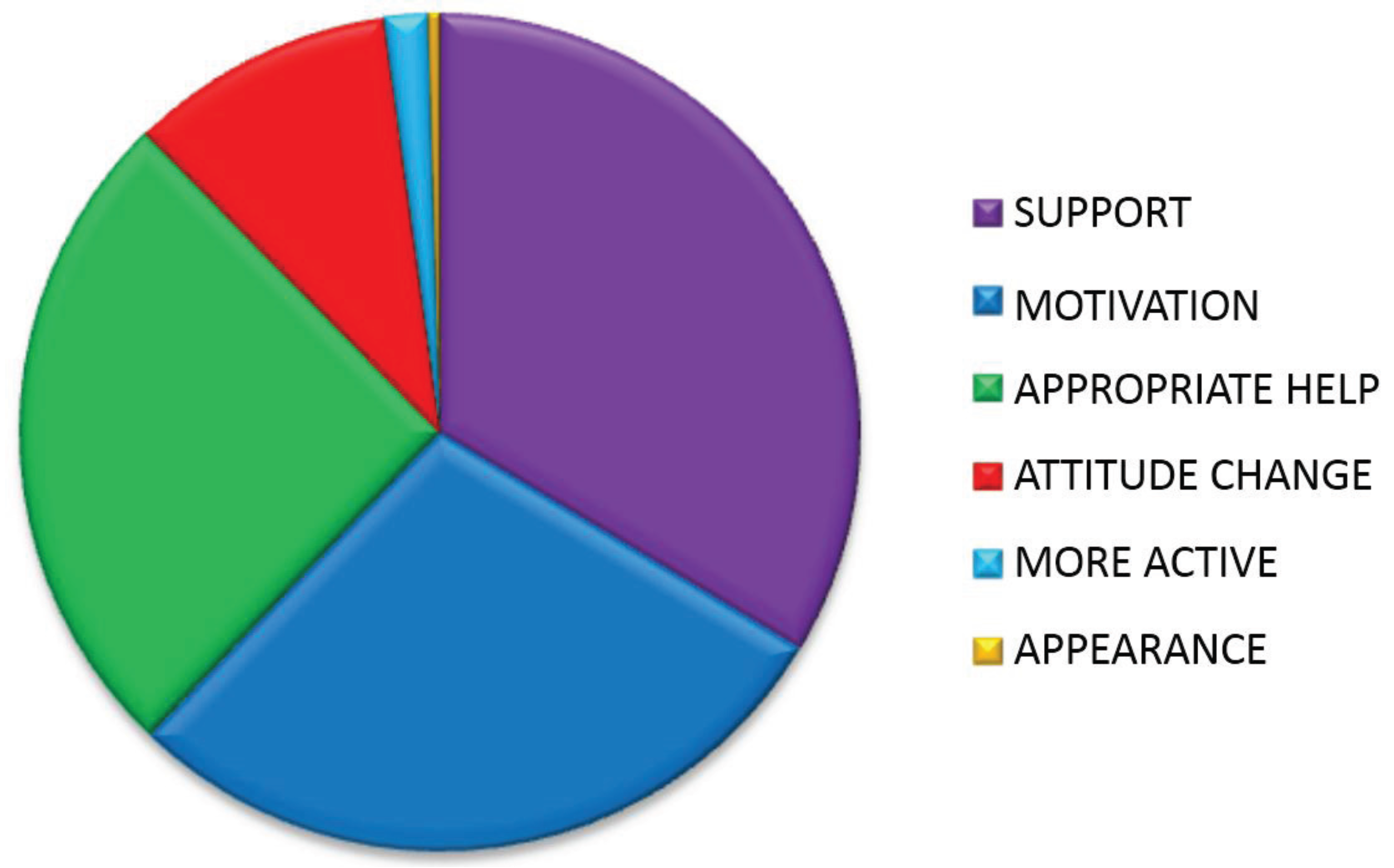
3.6. Since Attending the Clinic Have You Felt Encouraged to Lead a Healthier Lifestyle, Yes or No? Please Explain
| Reason | n | % |
|---|---|---|
| Support | 79 | 34 |
| Motivation | 67 | 29 |
| Appropriate help | 60 | 26 |
| Attitude change | 24 | 9 |
| More active | 4 | 1 |
| Appearance | 1 | 1 |
| Total | 235 | 100 |
| Category | Meaning | Patient Quotes |
|---|---|---|
| Support | Support given by team | “For the first time I feel I’m being listened to” |
| “The teams’ attitudes create a positive environment” | ||
| Motivation | Motivated by team | “I feel motivated in the right way” |
| “Regular appointments keep motivation up” | ||
| Appropriate help | Receiving appropriate information | “Being told 1:1 by a clinician the consequences of not addressing my weight made me understand the seriousness of the issue” |
| “Seeing the dietitian to find out where I was going wrong” | ||
| Attitude change | A change of attitude has allowed behaviour change | “I feel more mentally strong” |
| “Sessions with the counsellor have helped me feel I can do it” | ||
| More active | Weight loss enabled more activity | “I’m able to move more because I’ve lost weight” |
| Appearance | Wanted to look different | “I wanted to change the way I looked” |
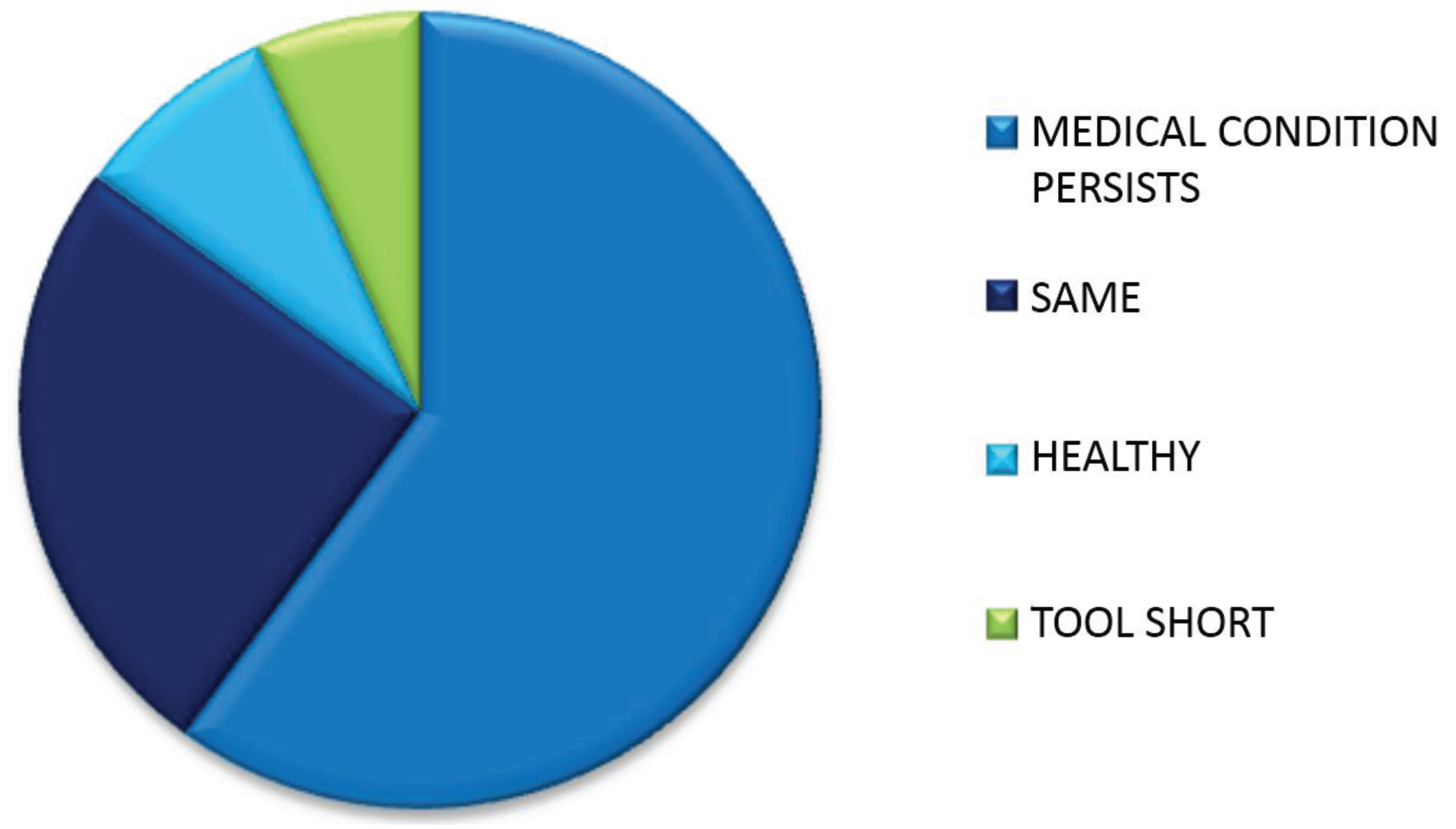
3.7. Since Attending the Clinic Have You Felt Your Health Has Improved Yes or No? Please Explain
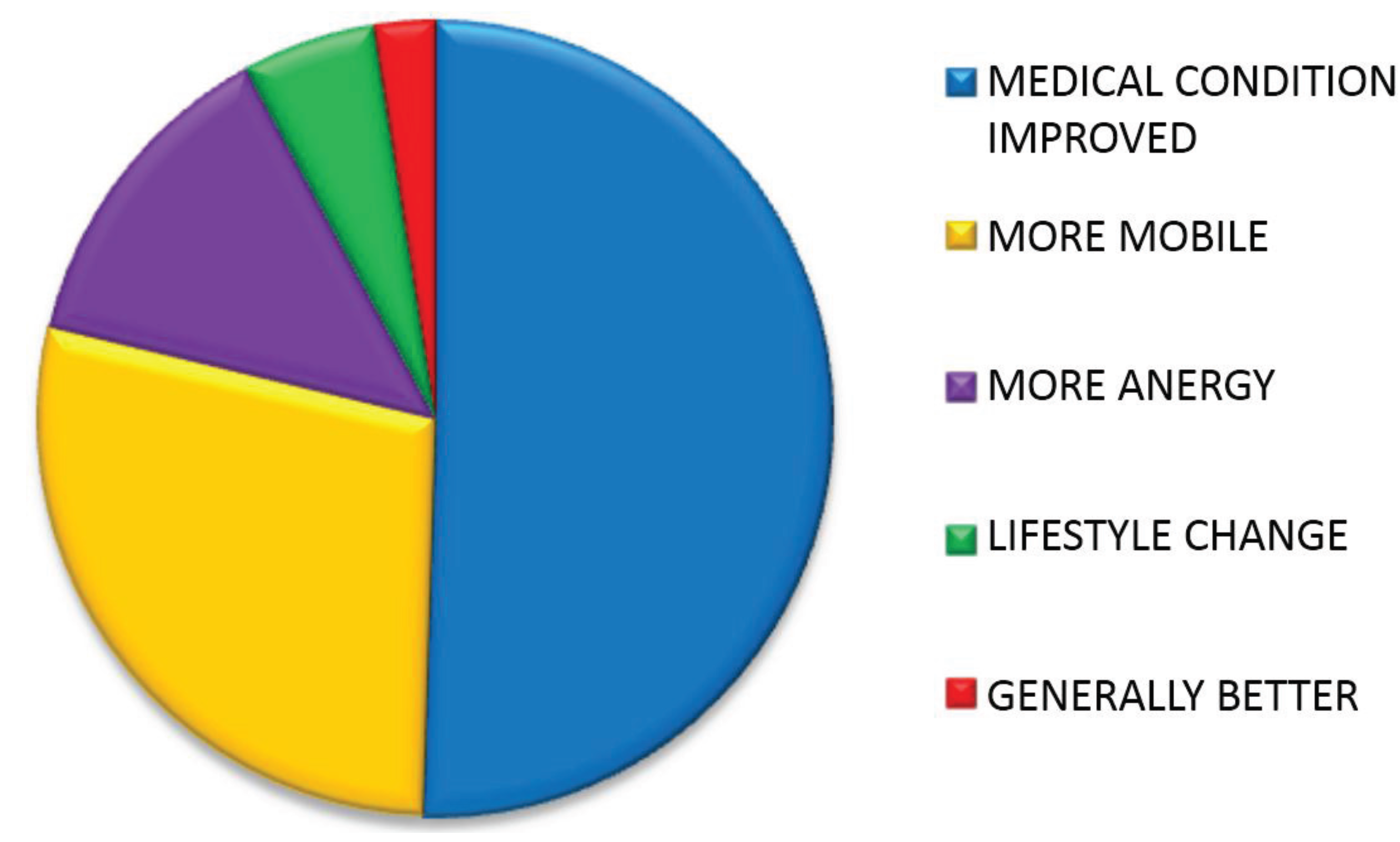
| Reason | n | % |
|---|---|---|
| Medical condition | 102 | 51 |
| More mobile | 57 | 28 |
| More energy | 27 | 13 |
| Lifestyle change | 11 | 5 |
| Generally better | 5 | 3 |
| TOTAL | 202 | 100 |
| Category | Meaning | Patient Quotes |
|---|---|---|
| Medical condition | Improvement in medical condition | “Resolves sleep apnoea” “I no longer need insulin” |
| More mobile | More mobile | “I can get about more ” “I am more active” |
| More energy | More energy | “I am less tired” “I have more energy” |
| Lifestyle change | A non-medical improvement to life | “I am less stressed” “I have lost weight” |
| Generally better | Sense of feeling “better” | “I just generally feel better” |
| Reason | n | % |
|---|---|---|
| Medical condition | 36 | 60 |
| Health same | 15 | 25 |
| Already healthy | 5 | 8 |
| Attendance too short | 4 | 7 |
| Total | 60 | 100 |
| Category | Meaning | Patient Quotes |
|---|---|---|
| Medical condition | No improvement in medical condition | “My blood pressure is still high” “My joints are still ainful” |
| Health same | Feels health is the same | “I don’t feel any more healthy” “My health is the same” |
| Already healthy | Health was good before | “I wasn’t unhealthy before” |
| Attendance too short | Time attending clinic is too short to feel benefits | “It’s too early to feel healthier yet” |
| Medical Condition | Yes (n) | % of All Reasons Given for Indicating Improved Health |
|---|---|---|
| Less Short Of Breath | 41 | 20.5 |
| Better Sleep | 13 | 6.5 |
| Better Controlled Blood Pressure | 12 | 6 |
| Less Joint Pain | 11 | 5.5 |
| Better Mental Health | 6 | 3 |
| Fewer Symptoms of Diabetes | 5 | 2.5 |
| Other | 14 | 7 |
| Totals | 102 | 51 |
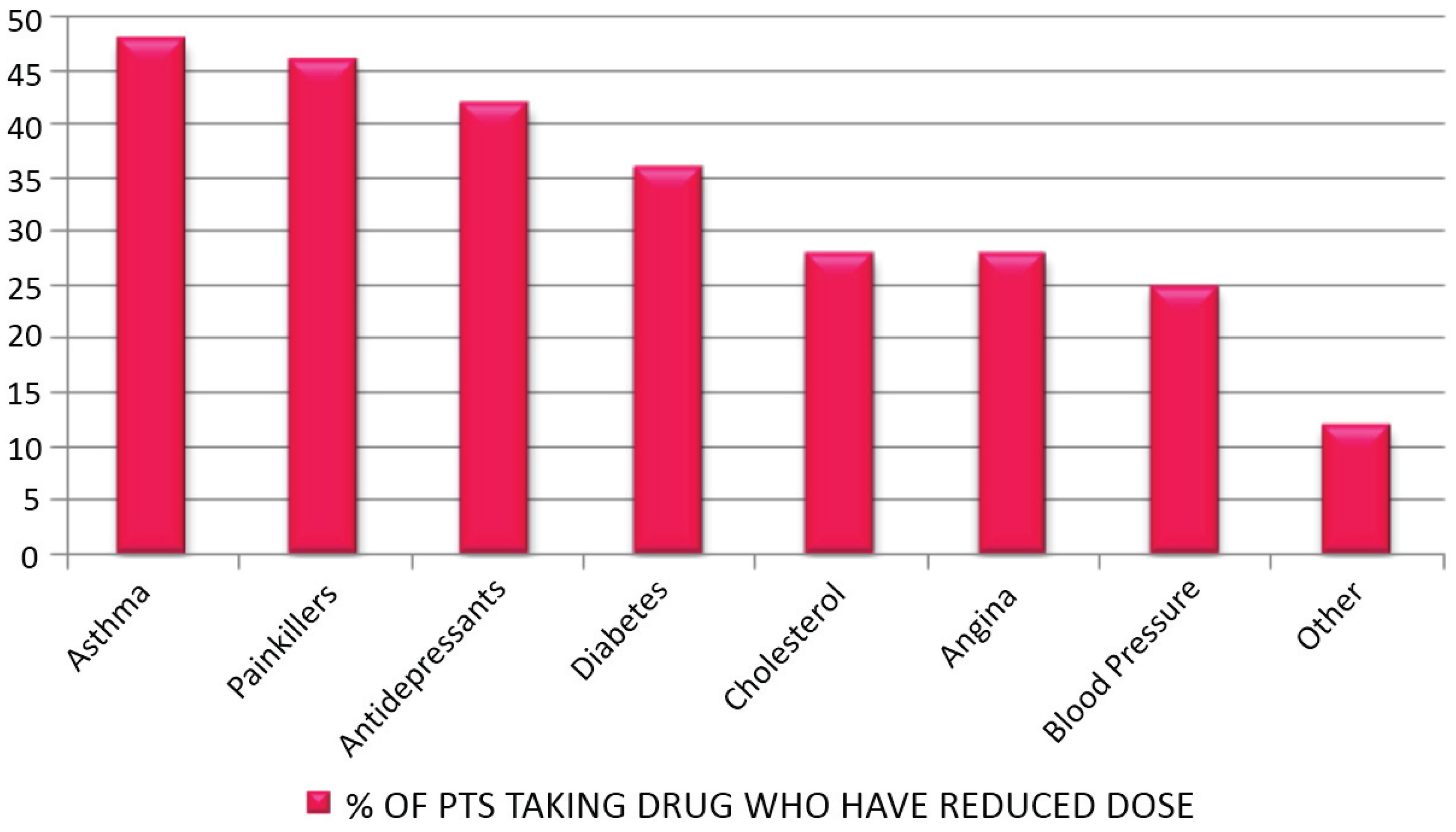
3.8. If You Were Taking Medication for the Following Medical Conditions—Have They Been Decreased since Attending the Clinic?
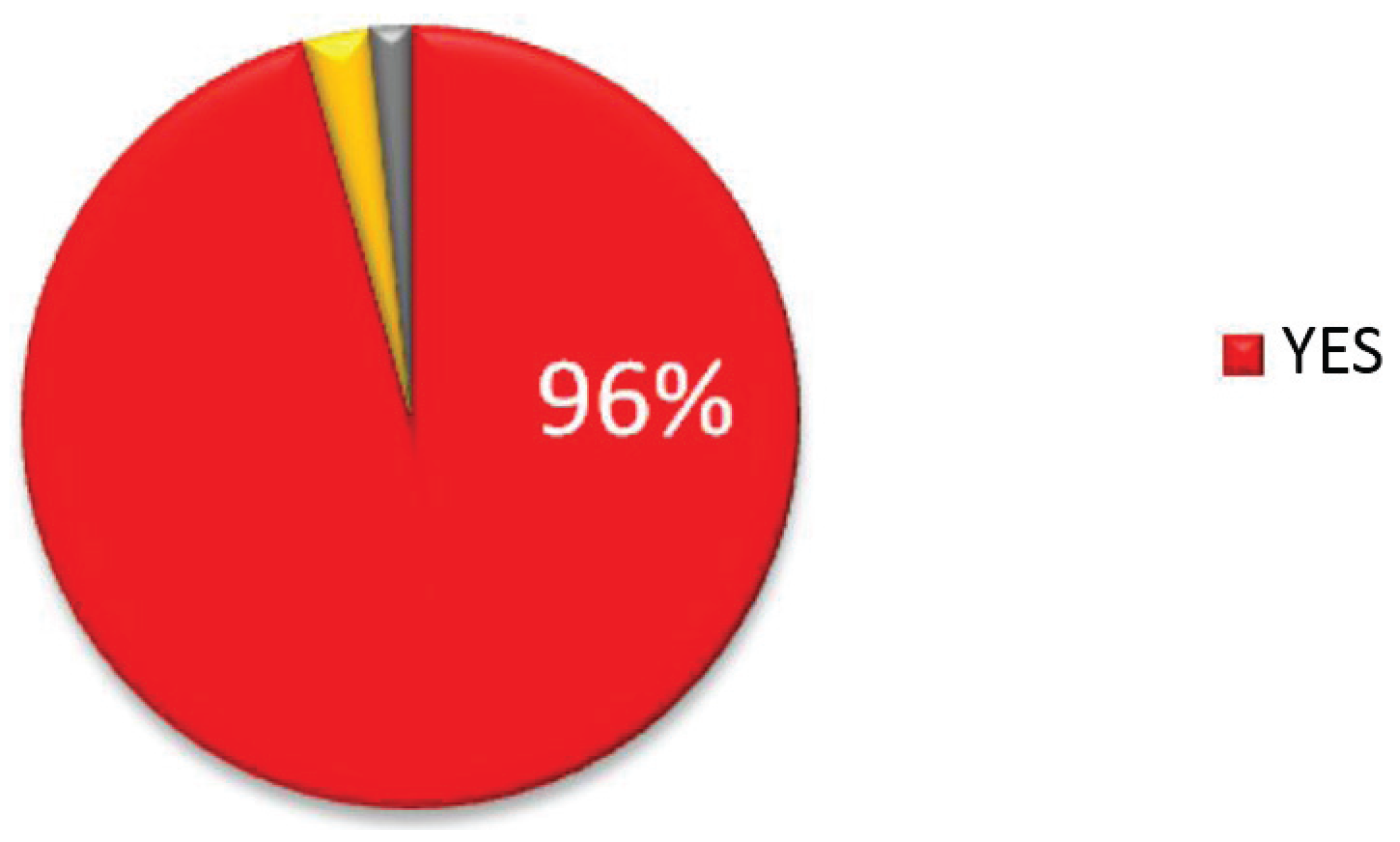
3.9. Would You Recommend the Clinic to Others?
| Medication Decrease | n | Total n | % |
|---|---|---|---|
| Asthma | 23 | 48 | 48 |
| Painkillers | 53 | 116 | 46 |
| Antidepressants | 27 | 65 | 42 |
| Diabetes | 14 | 39 | 36 |
| Cholesterol | 16 | 57 | 28 |
| Angina | 5 | 18 | 28 |
| Blood Pressure | 22 | 88 | 25 |
| Other | 3 | 25 | 12 |
3.10. Are You Employed? If Yes Are You Taking Less Time Off Because of Ill Health Since Attending the Clinic? Yes/No
3.11. Improvements
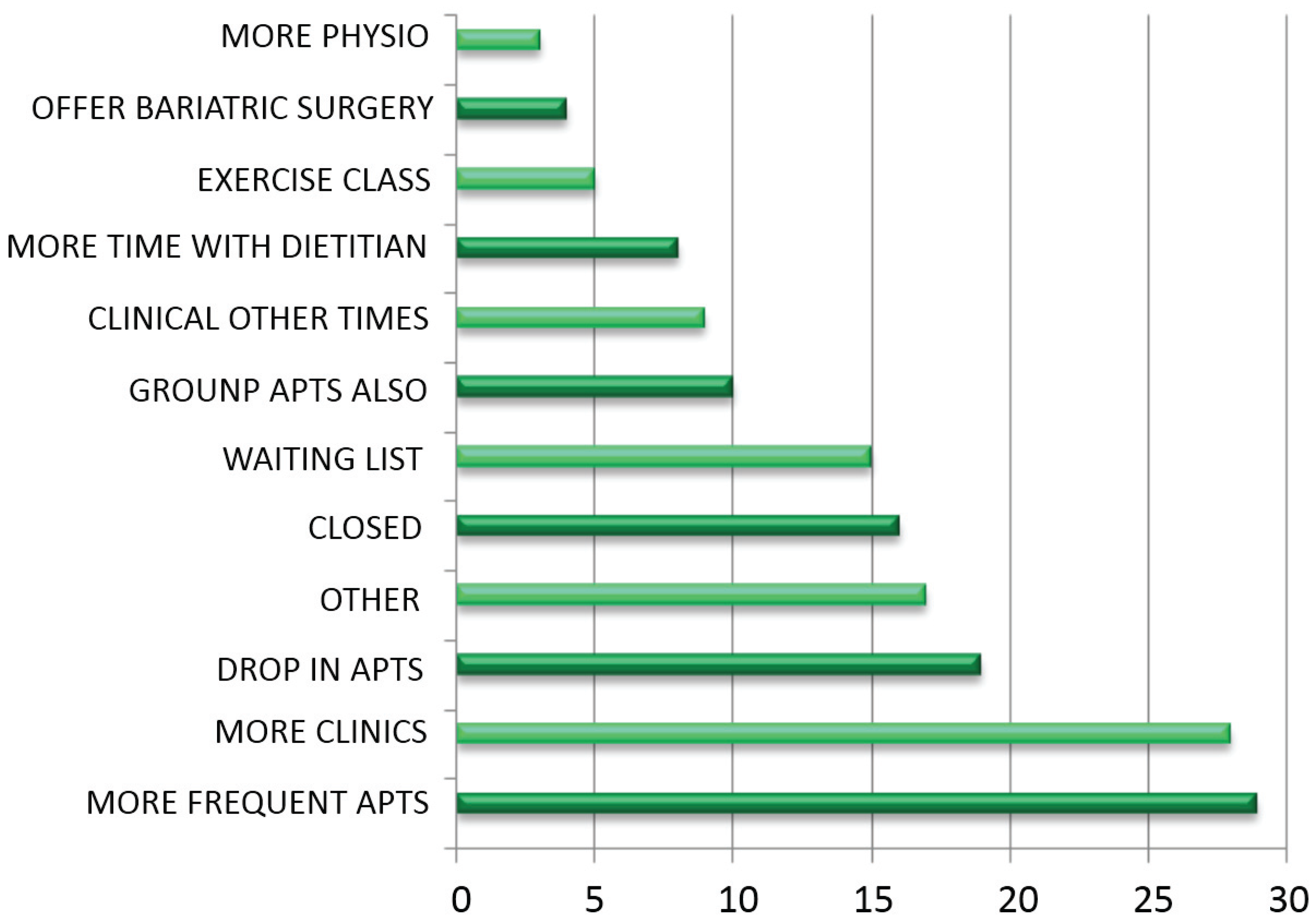
| Improvement | n |
|---|---|
| More physio | 3 |
| Surgery | 4 |
| Exercise class | 5 |
| Dietitian | 8 |
| Other times | 9 |
| Groups also | 10 |
| Waiting List | 15 |
| Closer | 16 |
| Other | 17 |
| Drop In apts. | 19 |
| More clinics | 28 |
| More frequent apts. | 29 |
3.12. Comments
| Category | Meaning | Patient quotes |
|---|---|---|
| More physio | More time with physiotherapist | “I’d like more demonstrations from the physiotherapist” |
| Surgery | Offer bariatric surgery | “Include bariatric surgery at the clinic” |
| Exercise class | Offer an exercise class | “The clinic could so with an exercise class liked to it” “Include referral to GP exercise scheme” |
| Dietitian | More time with dietitian | “I’d like more time with the dietitian” “Provide more dietitians” |
| Other times | Run clinic at other times | “Offer clinics in the evenings” “Offer appointments at more flexible times” |
| Groups also | Offer group appointments also | “Run group sessions also to motivate in-between appointments” “Offer group sessions for more frequent monitoring” |
| Waiting List | Reduce waiting list | “Reduce time required to wait on the list for referral to the clinic” |
| Closer | Run clinics close to patients’ homes | “It would be easier if I didn’t have to travel so far” |
| Other | Other suggestions | “Reduce walking distance from car-ark to clinic” |
| Drop In apts. | Offer drop in appointments | “Offer drop in appointments for weigh-ins” |
| More clinics | Run more clinics | “Provide more clinics” |

| Comment | n |
|---|---|
| CBT crucial | 3 |
| Negative | 7 |
| Team attitude | 82 |
| Clinic comforts | 10 |
| Nurses | 11 |
| Team | 16 |
| Other | 28 |
| Happy with clinic | 32 |
| Very happy with clinic | 62 |
| Category | Meaning | Patient Quotes |
|---|---|---|
| CBT crucial | Counsellor session is crucial | “The sessions provided by the counsellor are crucial” |
| Negative | Negative responses | “I’m really unhappy with everything” |
| Team attitude | Attitude of team members is significant | “The team are very welcoming” “The team’s attitude is great” |
| Clinic comforts | Clinic provides a comforting environment | “The clinic is a comfort zone” “The clinic is a lifeline” |
| Nurses | Specific mention of the nurses | “The nurses are great” “I have a great rapport with the nurses” |
| Team | Specific mention of the team members as a whole | “The staff are great. I really look forward to going to clinic” “The team are great” |
| Other | Other comments | “The clinic runs smoothly ” |
| Happy with clinic | Happy with clinic | “I am happy with everything” |
| Very happy with clinic | Very happy with clinic | “I am very happy with the clinic—I would be bedridden without it” |
4. Discussion
4.1. Summary of Main Findings and Comparisons with Literature
4.2. Strengths and Limitations of the Study
4.3. Suggestions for Future Work
5. Conclusions
Acknowledgements
Author Contributions
Conflicts of Interest
Appendix A

Appendix B. Questionnaire for Patient Interviews. Aneurin Bevan Specialist Weight Management Clinic
- (1)
- How long have you been attending the clinic? <3 months/3–6 months/6–12 months/>12 months
- (2)
- Have you lost weight since attending the clinic? Yes/NoIf yes how much weight have you lost?
- (3)
- If you were offered, on referral to the clinic, a choice of appointments type which would you choose?(Please circle) Individual appointment OR GroupPlease include comments
- (4a)
- (4b)
- (5)
- Have you felt encouraged to lead a healthier lifestyle?—Yes/NoPlease explain
- (6)
- Since attending the clinic have you felt your health has improved?—Yes/NoPlease explain
- (7)
- (8)
- Would you recommend the clinic to others?—Yes/No
- (9)
- Are you employed? Yes/NoIf yes are you taking less time off because of ill health since attending the clinic? Yes/No
- (10)
- If you could make any improvements to the clinic, what would they be?
References
- Welsh Assembly Government. All Wales Obesity Pathway. Available online: http://wales.gov.uk/topics/health/improvement/index/pathway/?lang=en/ (accessed on 10 May 2015).
- World Health Organization. Fact Sheet 311: Obesity and Overweight. Available online: http://www.who.int/mediacentre/factsheets/fs311/en/ (accessed on 10 May 2015).
- McPherson, K.; Marsh, T.; Brown, M. Foresight. In Tackling Obesities: Future Choices—Modelling Future Trends in Obesity and the Impact on Health, 2nd ed.; The Foresight Programme: London, UK, 2007. [Google Scholar]
- World Health Organization. Obesity: Preventing and Managing the Global Epidemic. Available online: http://www.who.int/nutrition/publications/obesity/WHO_TRS_894/en/ (accessed on 10 May 2015).
- Loveman, E.; Frampton, G.K.; Shepherd, J.; Picot, J.; Cooper, K.; Bryant, J.; Welch, K.; Clegg, A. The clinical effectiveness and cost-effectiveness of long-term weight management schemes for adults: A systematic review. Health Technol. Assess. 2011, 15, 1–182. [Google Scholar] [CrossRef] [PubMed]
- Welsh Assembly Government (WAG). Key Statistics for Wales. 2012. Available online: http://wales.gov.uk/docs/statistics/2012/120927keyhealth12en.pdf (accessed on 10 May 2015). [Google Scholar]
- Hale, J.; Phillips, C.; Jewell, T. Assessing the Costs to the NHS Associated with Alcohol and Obesity in Wales; Welsh Assembly Government: Swansea, UK, 2011.
- BBC Economy Tracker. Available online: http://www.bbc.co.uk/news/10604117 (accessed on 20 December 2012).
- Dr Foster Research. Weighing up the Burden of Obesity: A Review by Dr Foster Research; Dr Foster Research: London, UK, 2008. [Google Scholar]
- Centre for Public Health Excellence at NICE; National Collaborating Centre for Primary Care. Obesity: The prevention, identification, assessment and management of overweight and obesity in adults and children. Available online: http://www.ncbi.nlm.nih.gov/pubmed/22497033 (accessed on 10 May 2015).
- Welsh Assembly Government (WAG). W090 Tackling Obesity in Blaenau Gwent. Available online: http://wales.gov.uk/topics/health/improvement/communities/fund/inequalitiessouth1/obesity/?lang=en (accessed on 10 May 2015).
- Haboubi, N.Y.; Dix, H.M.; Jones, S.; Gray, J.; Golding, G.; Weaver, A.; Reynolds, J. Effectiveness of multi-disciplinary weight management clinics. Obes. Rev. 2010, 11, 1–472. [Google Scholar]
- Thompson, A.; Haboubi, N.; Jones, S.; Gray, G.; Weaver, A.; Reynolds, J. Does weight loss influence co-morbidities associated with adult obesity? Obes. Rev. 2011, 12, 63–279. [Google Scholar]
- Greenlagh, T. How to Read a Paper, 3rd ed.; Blackwell: London, UK, 2006. [Google Scholar]
- Woolford, S.J.; Sallinen, B.J.; Schaffer, S.; Clark, S.J. Eat, play, love: Adolescent and parent perceptions of the components of a multidisciplinary weight management program. Cin. Pediatr. 2012, 51, 678–684. [Google Scholar] [CrossRef] [PubMed]
- Royal College of Physicians. Action on Obesity: Comprehensive Care for All. Available online: http://www.rcplondon.ac.uk/resources/action-obesity-comprehensive-care-all (accessed on 10 May 2015).
- Göhner, W.; Schlatter, M.; Seelig, H.; Frey, I.; Berg, A.; Fuchs, R. Two-Year Follow-up of an Interdisciplinary Cognitive-Behavioral Intervention Program for Obese Adults. J. Psychol. 2012, 146, 371–391. [Google Scholar] [CrossRef] [PubMed]
- National Audit Office HC 220. Tackling Obesity in England. Available online: http://www.nao.org.uk/publications/0001/tackling_obesity_in_england.aspx (accessed on 10 May 2015).
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Turner, D.; Haboubi, N. Qualitative and Quantitative Outcomes of a 1:1 Multidisciplinary Weight Management Clinic. Healthcare 2015, 3, 429-451. https://doi.org/10.3390/healthcare3020429
Turner D, Haboubi N. Qualitative and Quantitative Outcomes of a 1:1 Multidisciplinary Weight Management Clinic. Healthcare. 2015; 3(2):429-451. https://doi.org/10.3390/healthcare3020429
Chicago/Turabian StyleTurner, Desley, and Nadim Haboubi. 2015. "Qualitative and Quantitative Outcomes of a 1:1 Multidisciplinary Weight Management Clinic" Healthcare 3, no. 2: 429-451. https://doi.org/10.3390/healthcare3020429





