Variation in Anticoagulant Recommendations by the Guidelines and Decision Tools among Patients with Atrial Fibrillation
Abstract
:1. Introduction
2. Methods
2.1. Study Design
2.2. Study Subjects
2.3. Exposure Definition
2.4. Stroke Risk and Bleeding Risk
2.5. Decision Aid Recommendations
2.6. Main Independent Variable
Concordance Status
2.7. Analyses
3. Results
| Characteristics | OAC Exposed | OAC Unexposed | Total | p Value |
|---|---|---|---|---|
| Number of patients (n %) | 7668 (50.68%) | 7461 (49.32%) | 15129 | |
| Mean age, y (SD) | 65.04 (11.82) | 62.54 (14.84) | 63.81 (13.45) | <0.001 |
| N (%) | N (%) | N (%) | ||
| Age Category, y | <0.001 | |||
| 18–30 | 29 (0.38%) | 146 (1.96%) | 175 (1.16%) | |
| 31–49 | 584 (7.62%) | 1156 (15.49%) | 1740 (11.50%) | |
| 50–64 | 3453 (45.03%) | 3092 (41.44%) | 6545 (43.26%) | |
| 65–74 | 1745 (22.76%) | 1240 (16.62%) | 2985 (19.73%) | |
| 75–84 | 1570 (20.47%) | 1429 (19.15%) | 2999 (19.82%) | |
| ≥85 | 287 (3.74%) | 398 (5.33%) | 685 (4.53%) | |
| Gender | <0.001 | |||
| Male | 4961 (53.16%) | 4372 (46.84%) | 9333 (61.69%) | |
| Female | 2707 (35.30%) | 3089 (41.40%) | 5796 (38.31%) | |
| Geographic Region | <0.001 | |||
| East | 1591 (20.75%) | 1474 (19.76%) | 3065 (20.26%) | |
| Midwest | 2656 (34.64%) | 2454 (32.89%) | 5110 (33.78%) | |
| South | 2301 (30.01%) | 2271 (30.44%) | 4572 (30.22%) | |
| West | 1120 (14.61%) | 1262 (16.91%) | 2382 (15.74%) | |
| Comorbidities | ||||
| Prior stroke or TIA | 551 (7.19%) | 476 (6.38%) | 1027 (6.79%) | 0.048 |
| Hypertension | 5177 (67.51%) | 4263 (57.14%) | 9440 (62.4%) | <0.001 |
| Diabetes | 1857 (24.22%) | 1265 (16.95%) | 3122 (20.64%) | <0.001 |
| Heart failure | 1506 (19.64%) | 884 (11.85%) | 2390 (15.8%) | <0.001 |
| Anemia | 731(9.53%) | 864 (11.58%) | 1595 (10.54%) | <0.001 |
| History of any bleed | 675 (8.80%) | 732 (9.81%) | 1407 (9.30%) | 0.032 |
| Renal impairment | 493 (6.43%) | 441 (5.91%) | 934 (6.17%) | 0.185 |
| Liver failure | 255 (3.33%) | 258 (3.46%) | 513 (3.39%) | 0.652 |
| Vascular disease | 2377 (31.00%) | 2202 (29.51%) | 4579 (30.27%) | 0.046 |
| Antiplatelet agents | 488 (6.36%) | 403 (5.40%) | 891 (5.89%) | 0.011 |
| NASIDs | 1443 (18.82%) | 1208 (16.19%) | 2651 (17.52%) | <0.001 |
| GI agents | 1532 (19.98%) | 1398 (18.74%) | 2930 (19.37%) | 0.053 |
| Antineoplastic agents | 178 (2.32%) | 135 (1.81%) | 313 (2.07%) | 0.027 |
| Systemic corticosteroids | 1136 (14.81%) | 939 (12.59%) | 2075 (13.72%) | <0.001 |
| Alcohol use | 124 (1.62%) | 119 (1.59%) | 243 (1.61%) | 0.913 |
| Stroke risk scores | ||||
| CHADS2 score | <0.001 | |||
| Low (score = 0) | 1524 (19.87%) | 2426 (32.52%) | 3950 (26.11%) | |
| Medium (score = 1) | 2676 (34.90%) | 2510 (33.64%) | 5186 (34.28%) | |
| High (score ≥ 2) | 3468 (45.23%) | 2525 (33.84%) | 5993 (39.61%) | |
| CHA2DS2-VASc score | <0.001 | |||
| Low (score = 0) | 804 (10.49%) | 1269 (17.01%) | 2073 (13.70%) | |
| Medium (score = 1) | 1478 (19.27%) | 1719 (23.04%) | 3197 (21.13%) | |
| High (score ≥ 2) | 5386 (70.24%) | 4473 (59.95%) | 9859 (65.17%) | |
| Bleeding risk scores | ||||
| ATRIA score | 0.002 | |||
| Low (score ≤ 3) | 6590 (85.94%) | 6391 (85.66%) | 12981 (85.80%) | |
| Medium (score = 4) | 596 (6.29%) | 401 (5.37%) | 883 (5.84%) | |
| High (score ≥ 5) | 596 (7.77%) | 669 (8.97%) | 1265 (8.36%) | |
| HAS BLED score | <0.001 | |||
| Low (score = 0) | 1159 (15.11%) | 1731 (23.20%) | 2890 (19.10%) | |
| Medium (score = 1 or 2) | 4944 (64.48%) | 4418 (59.21%) | 9362 (61.88%) | |
| High (score ≥ 3) | 1564 (20.41%) | 1312 (17.58%) | 2877 (19.02%) | |
| Anticoagulant exposure after index date | ||||
| Warfarin | 5886 (76.76%) | - | 5886 (38.91%) | |
| Dabigatran | 756 (9.86%) | - | 756 (5.00%) | |
| Rivaroxaban | 178 (2.32%) | - | 178 (1.18%) | |
| Apixaban | 5 (0.07%) | - | 5 (0.03%) | |
| Antiplatelet agents | 365 (4.76%) | 434 (5.82%) | 799 (5.28%) | |
| Stroke Risk | Bleeding risk | AHA Aggressive | AHA Conservative | Casciano | CHEST | ESC | LaHaye |
|---|---|---|---|---|---|---|---|
| Low (CHA2DS2-VASc score = 0) | Low (HAS-BLED score = 0) | 0 | 0 | 0 | 0 | 0 | 0 |
| n (%) = 1628 (10.76%) | (0.00%) | (0.00%) | (0.00%) | (0.00%) | (0.00%) | (0.00%) | |
| Medium (HAS-BLED score = 1 or 2) | 0 | 0 | 0 | 0 | 0 | 0 | |
| n (%) = 439(2.90%) | (0.00%) | (0.00%) | (0.00%) | (0.00%) | (0.00%) | (0.00%) | |
| High (HAS-BLED score ≥ 3) | 0 | 0 | 0 | 0 | 0 | 0 | |
| n (%) = 6 (0.04%) | (0.00%) | (0.00%) | (0.00%) | (0.00%) | (0.00%) | (0.00%) | |
| Sub-total | 0 | 0 | 0 | 0 | 0 | 0 | |
| (0.00%) | (0.00%) | (0.00%) | (0.00%) | (0.00%) | (0.00%) | ||
| Medium (CHA2DS2-VASc score = 1) | Low (HAS-BLED score = 0) | 1043 | 0 | 193 | 196 | 1043 | 0 |
| n (%) = 1043(6.89%) | (100%) | (0.00%) | (18.50%) | (18.79%) | (100%) | (0.00%) | |
| Medium (HAS-BLED score = 1 or2) | 2093 | 0 | 1371 | 1505 | 2093 | 0 | |
| n (%) = 2093(13.83%) | (100%) | (0.00%) | (65.50%) | (71.91%) | (100%) | (0.00%) | |
| High (HAS-BLED score ≥ 3) | 61 | 0 | 19 | 57 | 0 | 0 | |
| n (%) = 61 (0.40%) | (100%) | (0.00%) | (31.15%) | (93.44%) | (0.00%) | (0.00%) | |
| Sub-total | 3197 | 0 | 1583 | 1758 | 3136 | 0 | |
| (100%) | (0.00%) | (49.51%) | (54.98%) | (98.09%) | (0.00%) | ||
| High (CHA2DS2-VASc score ≥ 2) | Low (HAS-BLED score = 0) | 219 | 219 | 151 | 158 | 219 | 219 |
| n (%) = 219 (1.45%) | (100.00%) | (100.00%) | (68.95%) | (72.15%) | (100.00%) | (100.00%) | |
| Medium (HAS-BLED score = 1 or 2) | 6830 | 6830 | 5819 | 6468 | 6830 | 1102 | |
| n (%) = 6830 (45.15%) | (100.00%) | (100.00%) | (85.20%) | (94.70%) | (100.00%) | (16.13%) | |
| High (HAS-BLED score ≥ 3) | 2810 | 2810 | 2210 | 2795 | 2810 | 935 | |
| n (%) = 2810 (18.57%) | (100.00%) | (100.00%) | (78.65%) | (99.47%) | (100.00%) | (33.27%) | |
| Sub-total | 9859 | 9859 | 8180 | 9421 | 9859 | 2256 | |
| (100.00%) | (100.00%) | (82.96%) | (95.57%) | (100.00%) | (22.88%) | ||
| Overall | 15129 (100%) | 13056 | 9859 | 9763 | 11179 | 12995 | 2256 |
| (86.30%) | (65.17%) | (64.53%) | (73.89%) | (85.89%) | (14.91%) |
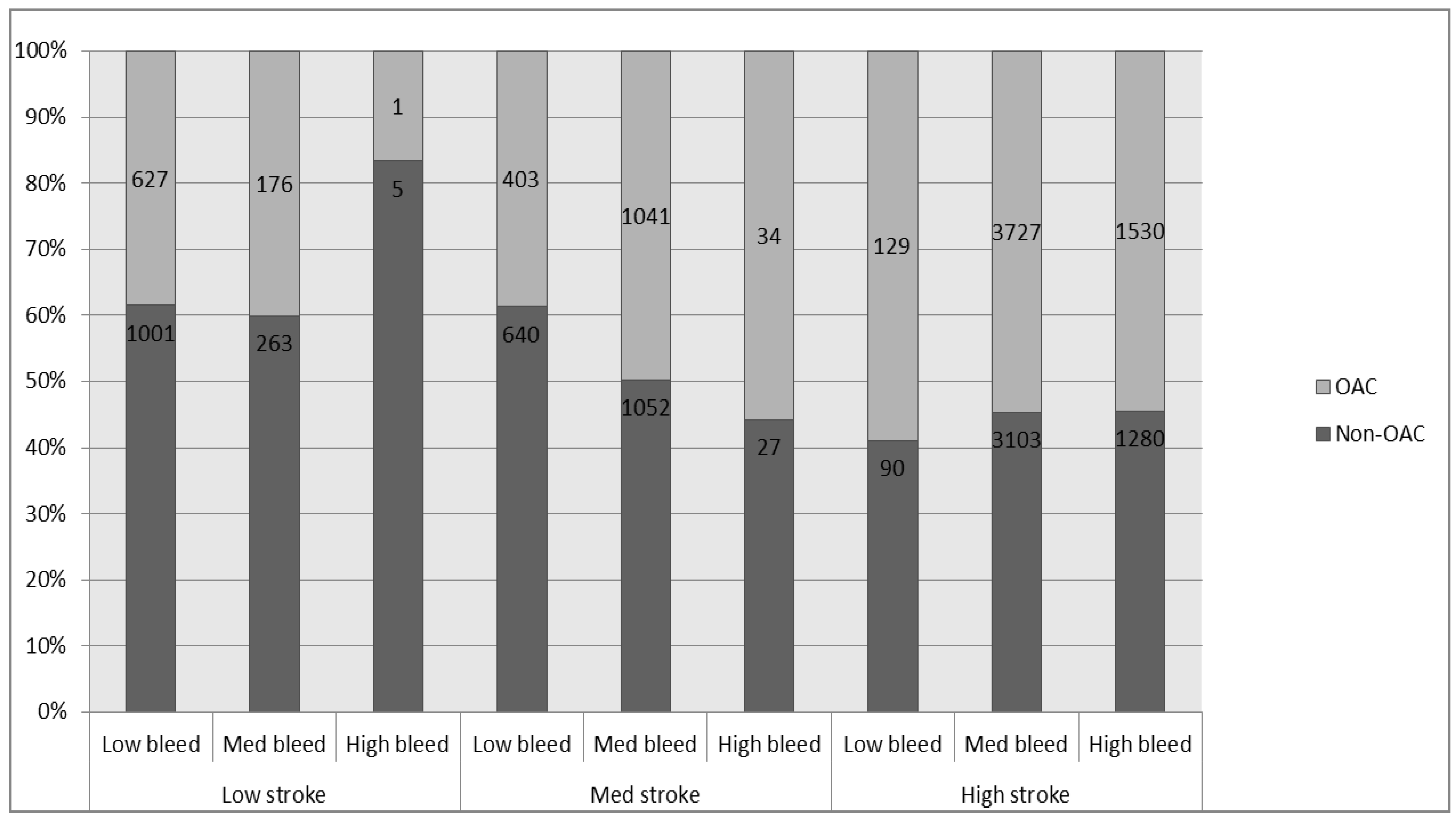
| Stroke Risk | Bleeding Risk | AHA Aggressive | AHA Conservative | Casciano | CHEST | ESC | LaHaye |
|---|---|---|---|---|---|---|---|
| Low (CHA2DS2-VASc score = 0)* | Sub-total | ARNO | ARNO | ARNO | ARNO | ARNO | ARNO |
| Medium (CHA2DS2-VASc score = 1) | Low (HAS-BLED score = 0) | 640 (61.36%) | ARNO | 52 (26.94%) | 54 (27.55%) | 640 (61.36%) | ARNO |
| Medium (HAS-BLED score = 1 or 2) | 1052 (50.26%) | ARNO | 661 (48.21%) | 728 (48.37%) | 1052 (50.26%) | ARNO | |
| High (HAS-BLED score ≥ 3) | 27 (44.26%) | ARNO | 8 (42.11%) | 27 (47.37%) | ARNO | ARNO | |
| Sub-total | 1719 (53.77%) | ARNO | 721 (45.55%) | 809 (46.02%) | 1692 (53.95%) | ARNO | |
| High (CHA2DS2-VAS score ≥ 2) | Low (HAS-BLED score = 0) | 90 (41.10%) | 90 (41.10%) | 47 (31.13%) | 48 (30.38%) | 90 (41.10%) | 90 (41.10%) |
| Medium (HAS-BLED score = 1 or 2) | 3103 (45.43%) | 3103 (45.43%) | 2578 (44.30%) | 2904 (44.90%) | 3103 (45.43%) | 542 (49.18%) | |
| High (HAS-BLED score ≥ 3) | 1280 (45.55%) | 1280 (45.55%) | 973 (44.03%) | 1274 (45.58%) | 1280 (45.55%) | 449 (48.02%) | |
| Sub-total | 4473 (45.37%) | 4473 (45.37%) | 3598 (43.98%) | 4226 (44.86%) | 4473 (45.37%) | 1081 (47.92%) | |
| Overall | Total | 6192 (47.42%) | 4473 (48.01%) | 4319 (44.23%) | 5035 (45.04%) | 6165 (47.44%) | 1081 (47.92%) |
| Stroke Risk | Bleeding Risk | AHA Aggressive | AHA Conservative | Casciano | CHEST | ESC | LaHaye |
|---|---|---|---|---|---|---|---|
| Low (CHA2DS2-VASc score = 0) | Low (HAS-BLED score = 0) | 627 (38.51%) | 627 (38.51%) | 627 (38.51%) | 627 (38.51%) | 627 (38.51%) | 627 (38.51%) |
| Medium (HAS-BLED score = 1 or 2) | 176 (40.09%) | 176 (40.09%) | 176 (40.09%) | 176 (40.09%) | 176 (40.09%) | 176 (40.09%) | |
| High (HAS-BLED score ≥ 3) | 1 (16.67%) | 1 (16.67%) | 1 (16.67%) | 1 (16.67%) | 1 (16.67%) | 1 (16.67%) | |
| Sub-total | 804 (38.78%) | 804 (38.78%) | 804 (38.78%) | 804 (38.78%) | 804 (38.78%) | 804 (38.78%) | |
| Medium (CHA2DS2-VASc score = 1 | Low (HAS-BLED score = 0) | ARO | 403 (38.64%) | 262 (30.82%) | 261 (30.81%) | ARO | 403 (38.64%) |
| Medium (HAS-BLED score = 1 or 2) | ARO | 1041 (49.74%) | 331 (45.84%) | 264 (44.90%) | ARO | 1041 (49.74%) | |
| High (HAS-BLED score ≥ 3) | ARO | 34 (55.74%) | 23 (54.76%) | 4 (100.00%) | 34 (55.74%) | 34 (55.74%) | |
| Sub-total | ARO | 1478 (46.23%) | 616 (38.17%) | 529 (36.76%) | 34 (55.73%) | 1478 (46.23%) | |
| High (CHA2DS2-VASc score ≥ 2) | Low (HAS-BLED score = 0) | ARO | ARO | 25 (36.76%) | 19 (31.15%) | ARO | ARO |
| Medium (HAS-BLED score = 1 or 2) | ARO | ARO | 486 (48.07%) | 163 (45.03%) | ARO | 3167 (55.29%) | |
| High (HAS-BLED score ≥ 3) | ARO | ARO | 293 (48.83%) | 9 (60.00%) | ARO | 1044 (55.68%) | |
| Sub-total | ARO | ARO | 804 (47.88%) | 191 (43.61%) | ARO | 4211 (55.38%) | |
| Overall | Total | 804 (38.78%) | 2282 (43.30%) | 2224 (41.45%) | 1564 (39.59%) | 838 (39.27%) | 6493 (50.43%) |
4. Discussion
5. Limitations
6. Conclusions
Supplementary Files
Supplementary File 1Acknowledgments
Author Contributions
Conflicts of Interest
References
- Singer, D.E.; Albers, G.W.; Dalen, J.E.; Fang, M.C.; Go, A.S.; Halperin, J.L.; Lip, G.Y.; Manning, W.J. Antithrombotic therapy in atrial fibrillation: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 2008, 133, 546S–592S. [Google Scholar] [CrossRef] [PubMed]
- Garg, N.; Kumar, A.; Flaker, G.C. Antiplatelet therapy for stroke prevention in atrial fibrillation. Mo. Med. 2010, 107, 44–47. [Google Scholar] [PubMed]
- Ogilvie, I.M.; Newton, N.; Welner, S.A.; Cowell, W.; Lip, G.Y. Underuse of oral anticoagulants in atrial fibrillation: A systematic review. Am. J. Med. 2010, 123, 638–645. [Google Scholar] [CrossRef] [PubMed]
- Gage, B.F.; Boechler, M.; Doggette, A.L.; Fortune, G.; Flaker, G.C.; Rich, M.W.; Radford, M.J. Adverse outcomes and predictors of underuse of antithrombotic therapy in medicare beneficiaries with chronic atrial fibrillation. Stroke 2000, 31, 822–827. [Google Scholar] [CrossRef] [PubMed]
- Cohen, N.; Almoznino-Sarafian, D.; Alon, I.; Gorelik, O.; Koopfer, M.; Chachashvily, S.; Shteinshnaider, M.; Litvinjuk, V.; Modai, D. Warfarin for stroke prevention still underused in atrial fibrillation: Patterns of omission. Stroke 2000, 31, 1217–1222. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.J.; Bell, J.R.; Deroo, D.B.; Kirk, J.W.; Wasson, J.H. Physician variation in anticoagulating patients with atrial fibrillation. Dartmouth Primary Care COOP Project. Arch. Inter. Med. 1990, 150, 83–86. [Google Scholar] [CrossRef]
- Beyth, R.J.; Antani, M.R.; Covinsky, K.E.; Miller, D.G.; Chren, M.M.; Quinn, L.M.; Landefeld, C.S. Why isn’t warfarin prescribed to patients with nonrheumatic atrial fibrillation? J. Gen. Inter. Med. 1996, 11, 721–728. [Google Scholar] [CrossRef]
- Akao, M.; Chun, Y.H.; Esato, M.; Abe, M.; Tsuji, H.; Wada, H.; Hasegawa, K.; Fushimi AF Registry Investigators. Inappropriate use of oral anticoagulants for patients with atrial fibrillation. Circ. J. 2014, 78, 2166–2172. [Google Scholar] [CrossRef] [PubMed]
- Lahaye, S.A.; Gibbens, S.L.; Ball, D.G.; Day, A.G.; Olesen, J.B.; Skanes, A.C. A clinical decision aid for the selection of antithrombotic therapy for the prevention of stroke due to atrial fibrillation. Eur. Heart J. 2012, 33, 2163–2171. [Google Scholar] [CrossRef] [PubMed]
- January, C.T.; Wann, L.S.; Alpert, J.S.; Calkins, H.; Cleveland, J.C., Jr.; Cigarroa, J.E.; Conti, J.B.; Ellinor, P.T.; Ezekowitz, M.D.; Field, M.E.; et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J. Am. Coll. Cardiol. 2014, 64, e1–e76. [Google Scholar] [CrossRef] [PubMed]
- Casciano, J.P.; Singer, D.E.; Kwong, W.J.; Fox, E.S.; Martin, B.C. Anticoagulation therapy for patients with non-valvular atrial fibrillation: comparison of decision analytic model recommendations and real-world warfarin prescription use. Am. J. Cardiovasc. Drugs 2012, 12, 313–323. [Google Scholar] [CrossRef] [PubMed]
- You, J.J.; Singer, D.E.; Howard, P.A.; Lane, D.A.; Eckman, M.H.; Fang, M.C.; Hylek, E.M.; Schulman, S.; Go, A.S.; Hughes, M.; et al. Antithrombotic therapy for atrial fibrillation: antithrombotic therapy and prevention of thrombosis: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012, 141, e531S–e575S. [Google Scholar] [CrossRef] [PubMed]
- Camm, A.J.; Lip, G.Y.; de Caterina, R.; Savelieva, I.; Atar, D.; Hohnloser, S.H.; Hindricks, G.; Kirchhof, P.; ESC Committee for Practice Guidelines (CPG); Bax, J.J.; et al. 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: An update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur. Heart J. 2012, 33, 2719–2747. [Google Scholar] [CrossRef] [PubMed]
- Wess, M.L.; Schauer, D.P.; Johnston, J.A.; Moomaw, C.J.; Brewer, D.E.; Cook, E.F.; Eckman, M.H. Application of a decision support tool for anticoagulation in patients with non-valvular atrial fibrillation. J. Gen. Inter. Med. 2008, 23, 411–417. [Google Scholar] [CrossRef]
- DAWN AC Anticoagulation Software—4S Dawn Clinical Software. RefGrab-It. Available online: http://www.4s-dawn.com/products/anticoagulation/dawnac/ (accessed on 7 February 2014).
- Medical Disclaimer—AFib.ca. RefGrab-It. Available online: http://www.afib.ca/Disclaimer (accessed on 7 February 2014).
- Gage, B.F.; Waterman, A.D.; Shannon, W.; Boechler, M.; Rich, M.W.; Radford, M.J. Validation of clinical classification schemes for predicting stroke: Results from the National Registry of Atrial Fibrillation. JAMA 2001, 285, 2864–2870. [Google Scholar] [CrossRef] [PubMed]
- Lip, G.Y.; Nieuwlaat, R.; Pisters, R.; Lane, D.A.; Crijns, H.J. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: The euro heart survey on atrial fibrillation. Chest 2010, 137, 263–272. [Google Scholar] [CrossRef] [PubMed]
- Fang, M.C.; Go, A.S.; Chang, Y.; Borowsky, L.H.; Pomernacki, N.K.; Udaltsova, N.; Singer, D.E. A new risk scheme to predict warfarin-associated hemorrhage: The ATRIA (Anticoagulation and Risk Factors in Atrial Fibrillation) Study. J. Am. Coll. Cardiol. 2011, 58, 395–401. [Google Scholar] [CrossRef] [PubMed]
- Lip, G.Y.; Frison, L.; Halperin, J.L.; Lane, D.A. Comparative validation of a novel risk score for predicting bleeding risk in anticoagulated patients with atrial fibrillation: the HAS-BLED (Hypertension, Abnormal Renal/Liver Function, Stroke, Bleeding History or Predisposition, Labile INR, Elderly, Drugs/Alcohol Concomitantly) score. J. Am. Coll. Cardiol. 2011, 57, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Singer, D.E.; Chang, Y.; Fang, M.C.; Borowsky, L.H.; Pomernacki, N.K.; Udaltsova, N.; Go, A.S. The net clinical benefit of warfarin anticoagulation in atrial fibrillation. Ann. Inter. Med. 2009, 151, 297–305. [Google Scholar] [CrossRef]
- Go, A.S.; Hylek, E.M.; Chang, Y.; Phillips, K.A.; Henault, L.E.; Capra, A.M.; Jensvold, N.G.; Selby, J.V.; Singer, D.E. Anticoagulation therapy for stroke prevention in atrial fibrillation: How well do randomized trials translate into clinical practice? JAMA 2003, 290, 2685–2692. [Google Scholar] [CrossRef] [PubMed]
- Go, A.S.; Hylek, E.M.; Borowsky, L.H.; Phillips, K.A.; Selby, J.V.; Singer, D.E. Warfarin use among ambulatory patients with nonvalvular atrial fibrillation: the anticoagulation and risk factors in atrial fibrillation (ATRIA) study. Ann. Inter. Med. 1999, 131, 927–934. [Google Scholar] [CrossRef]
- Kate, F.; Jonah, B.; Bruce, P.; Kosuke, I.; Winghan Jacqueline, K. Utilization of anticoagulation therapy in medicare patients with nonvalvular atrial fibrillation. 2012, 5, 157–168. [Google Scholar]
- Hylek, E.M.; Go, A.S.; Chang, Y.; Jensvold, N.G.; Henault, L.E.; Selby, J.V.; Singer, D.E. Effect of intensity of oral anticoagulation on stroke severity and mortality in atrial fibrillation. New Engl. J. Med. 2003, 349, 1019–1026. [Google Scholar] [CrossRef] [PubMed]
- Lip, G.; Bassand, J.; Fitzmaurice, D.; Goldhaber, S.; Goto, S.; Verheugt, F.; Turpie, A.; Mueller, I.; Rushton-Smith, S.; Kakkar, A. Inappropriate utilization of anticoagulation in patients with atrial fibrillation: The global anticoagulant registry in the field (GARFIELD) registry. J. Am. Coll. Cardiol. 2012, 59, E670. [Google Scholar] [CrossRef]
- Steinberg, B.A.; Kim, S.; Thomas, L.; Fonarow, G.C.; Hylek, E.; Ansell, J.; Go, A.S.; Chang, P.; Kowey, P.; Gersh, B.J.; et al. Lack of concordance between empirical scores and physician assessments of stroke and bleeding risk in atrial fibrillation: Results from the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT-AF) registry. Circulation 2014, 129, 2005–2012. [Google Scholar] [CrossRef] [PubMed]
- Singer, D.E.; Chang, Y.; Borowsky, L.H.; Fang, M.C.; Pomernacki, N.K.; Udaltsova, N.; Reynolds, K.; Go, A.S. A new risk scheme to predict ischemic stroke and other thromboembolism in atrial fibrillation: the ATRIA study stroke risk score. J. Am. Heart Assoc. 2013, 2, e000250. [Google Scholar] [PubMed]
- Mercaldi, C.J.; Siu, K.; Sander, S.D.; Walker, D.R.; Wu, Y.; Li, Q.; Wu, N. Long-term costs of ischemic stroke and major bleeding events among medicare patients with nonvalvular atrial fibrillation. Cardiol. Res. Pract. 2012. [CrossRef]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shewale, A.; Johnson, J.; Li, C.; Nelsen, D.; Martin, B. Variation in Anticoagulant Recommendations by the Guidelines and Decision Tools among Patients with Atrial Fibrillation. Healthcare 2015, 3, 130-145. https://doi.org/10.3390/healthcare3010130
Shewale A, Johnson J, Li C, Nelsen D, Martin B. Variation in Anticoagulant Recommendations by the Guidelines and Decision Tools among Patients with Atrial Fibrillation. Healthcare. 2015; 3(1):130-145. https://doi.org/10.3390/healthcare3010130
Chicago/Turabian StyleShewale, Anand, Jill Johnson, Chenghui Li, David Nelsen, and Bradley Martin. 2015. "Variation in Anticoagulant Recommendations by the Guidelines and Decision Tools among Patients with Atrial Fibrillation" Healthcare 3, no. 1: 130-145. https://doi.org/10.3390/healthcare3010130





