Assistive Technology Needs and Measurement of the Psychosocial Impact of Assistive Technologies for Independent Living of Older Hispanics: Lessons Learned
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants’ Recruitment and Sampling
2.2. Data Collection Instruments
2.2.1. The Socio-Demographic Questionnaire
2.2.2. Assistive Technology Card Assessment (ATCA)
2.2.3. Puerto Rican Version of the Psychosocial Impact of Assistive Devices Scale (PIADS)
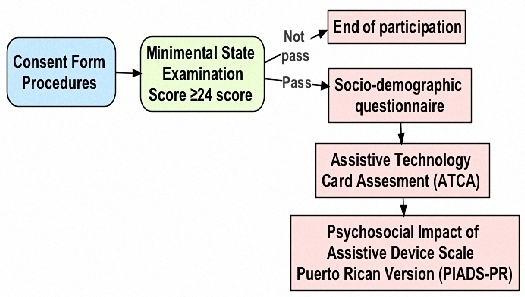
2.3. Procedures
2.4. Data Analysis
3. Results
3.1. Sample Characteristics
3.2. Assistive Technology Needs
3.3. Psychosocial Impact of AT
4. Discussion
4.1. Assistive Technology Needs
4.2. Psychosocial Impact of AT
4.3. Methodological Challenges and Lessons Learned
4.4. Limitations of the Study
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Ward, B.W.; Schiller, J.S.; Goodman, R.A. Multiple chronic conditions among US adults: A 2012 update. Prev. Chronic. Dis. 2014, 11. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Death and Mortality. NCHS FastStats Web Site. Available online: http://www.cdc.gov/nchs/fastats/deaths.htm (accessed on 20 December 2013).
- Hootman, J.M.; Brault, M.W.; Helmick, C.G.; Theis, K.A.; Armour, B.S. Prevalence and most common causes of disability among adults—United States, 2005. Morb. Mortal. Wkly. Rep. 2009, 58, 421–426. [Google Scholar]
- Centers for Disease Control and Prevention. The State of Aging and Health in America 2013. Available online: http://www.cdc.gov/features/agingandhealth/state_of_aging_and_health_in_america_2013.pdf (accessed on 11 June 2016).
- Erickson, W.; Lee, C.; von Schrader, S. Disability Statistics from the 2012 American Community Survey (ACS). Available online: http://www.disabilitystatistics.org (accessed on 20 May 2015).
- Freedman, V.A.; Agree, E.M.; Martin, L.G.; Cornman, J.C. Trends in the use of assistive technology and personal care for late-life disability, 1992–2001. Gerontologist 2005, 46, 124–127. [Google Scholar] [CrossRef]
- McCreadie, C.; Tinker, A. The acceptability of assistive technology to older people. Ageing Soc. 2005, 25, 91–110. [Google Scholar] [CrossRef]
- Tinker, A. Introducing assistive technologies (AT) into the homes of older people: the REKI (Reading/King’s) research project. Hous. Care Support. 2004, 7, 30–34. [Google Scholar] [CrossRef]
- Mann, W.C.; Ottenbacher, K.J.; Fraas, L.; Tomita, M.; Granger, C.V. Effectiveness of assistive technology and environmental interventions in maintaining independence and reducing home care costs for the frail elderly. Arch. Fam. Med. 1999, 8, 210–217. [Google Scholar] [CrossRef] [PubMed]
- Day, H.; Jutai, J.; Woolrich, W.; Strong, G. The stability of impact of assistive devices. Disabil. Rehabil. 2001, 23, 400–404. [Google Scholar] [PubMed]
- Lin, I.F.; Wu, H.S. Activity limitations, use of assistive devices or personal help, and well-being: Variation by education. J. Gerontol. Seri. B. Psychol. Sci. Soc. Sci. 2014, 69, S16–S25. [Google Scholar] [CrossRef] [PubMed]
- Wilson, D.J.; Mitchell, J.M.; Kemp, B.J.; Adkins, R.H.; Mann, W. Effects of assistive technology on functional decline in people aging with a disability. Assist. Technol. 2009, 21, 208–217. [Google Scholar] [CrossRef] [PubMed]
- Day, H.; Jutai, J.; Campbell, K.A. Development of a scale to measure the psychosocial impact of assistive devices: Lessons learned and the road ahead. Disabil. Rehabil. 2002, 24, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Cornman, J.C.; Freedman, V.A. Racial and ethnic disparities in mobility device use in late life. J. Gerontol. Seri. B Psychol. Sci. Soc. Sci. 2008, 6, S34–S41. [Google Scholar] [CrossRef]
- Resnik, L.; Allen, S. Racial and ethnic differences in use of assistive devices for mobility: Effect modification by age. J. Aging Health 2006, 18, 106–124. [Google Scholar] [CrossRef] [PubMed]
- Kaye, H.S.; Yeager, P.; Reed, M. Disparities in usage of assistive technologies among people with disabilities. Assist. Technol. 2008, 24, 194–203. [Google Scholar] [CrossRef] [PubMed]
- Scherer, M.J. Outcomes of assistive technology use on quality of life. Disabil. Rehabil. 1996, 18, 439–448. [Google Scholar] [CrossRef] [PubMed]
- Devitt, R.; Chau, B.; Jutai, J.W. The Effect of Wheelchair Use on the Quality of Life of Persons with Multiple Sclerosis. Occup. Ther. Health Care. 2002, 17, 63–79. [Google Scholar] [CrossRef] [PubMed]
- Jutai, J.; Bayley, M.; Teasell, R.; Hartley, M. Psychosocial impact of assistive technology devices in stroke. In Assistive Technology-Shaping the Future; IOS Press: Amsterdam, The Netherlands, 2003; pp. 814–818. [Google Scholar]
- Ward, A.L.; Hammond, S.; Holsten, S.; Bravver, E.; Brooks, B.R. Power Wheelchair Use in Persons With Amyotrophic Lateral Sclerosis: Changes Over Time. Assist. Technol. 2015, 27, 238–245. [Google Scholar] [CrossRef] [PubMed]
- Jutai, J.W.; Hartley, M.; Gryfe, P.; Day, H. Assistive devices for elderly people who have amyotrophic lateral sclerosis. In Proceedings of International Conference on Technology and Aging, Toronto, ON, Canada, 12–14 September 2001.
- Louise-Bender, P.T.; Kim, J.; Weiner, B. The shaping of individual meanings assigned to assistive technology: A review of personal factors. Disabil. Rehabil. 2002, 15, 5–20. [Google Scholar]
- Salminen, A.L.; Brandt, A.; Samuelsson, K.; Töytäri, O.; Malmivaara, A. Mobility devices to promote activity and participation: a systematic review. J. Rehabil. Med. 2009, 41, 697–706. [Google Scholar] [CrossRef] [PubMed]
- DeRuyter, F. The importance of outcome measures for assistive technology service delivery systems. Technol. Disabil. 1997, 6, 89–100. [Google Scholar] [CrossRef]
- Orellano, E.M.; Jutai, J.W. Cross-cultural adaptation of the psychosocial impact of assistive device scale (PIADS) for Puerto Rican assistive technology users. Assist. Technol. 2013, 5, 194–203. [Google Scholar] [CrossRef] [PubMed]
- Portney, L.G.; Watkins, M.P. Foundations of Clinical Research: Applications to Practice, 3rd ed.; Pearson Prentice Hall: Upper Saddle River, NJ, USA, 2009. [Google Scholar]
- Crum, R.M.; Anthony, J.C.; Bassett, S.S.; Folstein, M.F. Population-based norms for the Mini-Mental State Examination by age and education level. J. Am. Med. Assoc. 1993, 269, 2386–2391. [Google Scholar] [CrossRef]
- Jutai, J.; Day, H. Psychosocial impact of assistive devices scale (PIADS). Technol. Disabil. 2002, 14, 107–111. [Google Scholar]
- Cheek, P.; Nikpour, L.; Nowlin, H.D. Aging well with smart technology. Nurs. Adm. Q. 2005, 29, 329–338. [Google Scholar] [CrossRef] [PubMed]
- Häggblom-Kronlöf, G.; Sonn, U. Use of assistive devices—A reality full of contradictions in elderly persons′ everyday life. Disabil. Rehabil. Assist. Technol. 2007, 2, 335–345. [Google Scholar] [CrossRef] [PubMed]
- Gitlow, L.; Eastman, E.; Gefell, A.; Morehouse, L.; O′Connor, C.; Spangenberg, C. Assessing Assistive Device Needs of Community Dwelling Older Adults in Tompkins County. Physi. Occup. Ther. Geriatr. 2012, 30, 368–382. [Google Scholar] [CrossRef]
- Chan, K.T.; Tran, T.; Berridge, C.; Shi, J.; Chun, S. Examining social determinants in use of assistive devices for Asian American elders with a disability. Gerontologist 2015, 55, 365–366. [Google Scholar]
- Pausada, T.; Pereira, J.; Nieto, L.; Groba, B.; Diez, E. Evaluating the Psychosocial Impact of Wheelchair in People with Neuromuscular Disorders. Available online: https://www.resna.org/sites/default/files/conference/2014/Outcomes/Pousada.html (accessed on 12 September 2015).
- Devitt, R.; Chau, B.; Jutai, J. The effect of wheelchair use on the quality of life of persons with multiple sclerosis. Occup. Ther. Health Care. 2003, 17, 63–79. [Google Scholar] [CrossRef] [PubMed]
- Demmers, L.; Monette, M.; Lapierre, Y.; Arnold, D.L.; Wolfson, C. Reliability, validity, and applicability of the Quebec User Evaluation of Satisfaction with Assistive Technology (QUEST 2.0) for adults with multiple sclerosis. Disabil. Rehabil. 2002, 24, 21–30. [Google Scholar] [CrossRef]
- Gryfe, P.; Jutai, J. Assistive technologies: Clients' perceptions of impact on quality of life. Rehab Community Care Manag. 1998, 7, 26–30. [Google Scholar]
- Gitlin, L.N.; Luborsky, M.R.; Schemm, R.L. Emerging concerns of older stroke patients about assistive device use. Gerontologist 1998, 38, 169–180. [Google Scholar] [CrossRef] [PubMed]
- Skymne, C.; Dahlin-Ivanoff, S.; Claesson, L.; Eklund, K. Getting used to assistive devices: Ambivalent experiences by frail elderly persons. Scand. J. Occup. Ther. 2012, 19, 194–203. [Google Scholar] [CrossRef] [PubMed]
- Orellano-Colón, E.; Mann, C.M.; Rivero, M.; Torres, M.; Jiati, J.; Santiago, A.; Varas, N. Hispanic older adult’s perceptions of personal, contextual and technology-related barriers for using assistive technology devices. J. Racia.l Ethn. Health Dispar. 2015. [Google Scholar] [CrossRef] [PubMed]
- Resnick, L.; Allen, S.; Lezonni, L. Perspectives on use of mobility aids in a diverse population of seniors: Implication for intervention. Disabil. Health J. 2009, 2, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Peek, S.T.; Wouter, E.J.; van Hoof, J.; Luijkx, K.G.; Boeije, H.R.; Vrjhoef, H.J. Factors influencing acceptance of technology for aging in place: A systematic review. Int. J. Med. Inform. 2014, 83, 235–248. [Google Scholar] [CrossRef] [PubMed]
- Dayer-Berenson, L. Cultural Competence of Nurses: Impact on Health and Illness; Jones & Bartlett Learning Publishers, LLC: Sudburry, MA, USA, 2011. [Google Scholar]
- D’Alonzo, K.T. Evaluation and revision of questionnaires for use among low-literacy immigrant Latinos. Rev. Latino Am. Enfermagem. 2011, 19, 1255–1264. [Google Scholar] [CrossRef]
- Marín, G.; Gamba, R.J.; Marín, B.V. Extreme response style and acquiescence among Hispanics: The role of acculturation and education. J. Cross Cult. Psychol. 1992, 23, 498–509. [Google Scholar] [CrossRef]
| Socio-Demographic Characteristics | Total n = 60 |
|---|---|
| Age Range (Min, max) | 70–97 |
| Mean (SD) | 77 (6.27) |
| Sex, n (%) | |
| Female | 40 (66.7) |
| Male | 20 (33.3) |
| Educational Level, n (%) | |
| High school or less | 48 (80) |
| Some college education | 12 (20) |
| Monthly Income, n (%) | |
| Low(<$1000) | 50 (83) |
| Medium ($1000–$2000) | 8 (13) |
| High (>$2000) | 2 (3) |
| Health Conditions, n (%) | |
| Hypertension | 35 (58) |
| Musculoskeletal | 33 (55) |
| Diabetes | 32 (53) |
| Visual | 15 (25) |
| Respiratory | 13 (23) |
| Cardiac | 12 (20) |
| Overweight | 12 (20) |
| Assistive Technology | Number and Percentages of Responses That Reported “I Would Use This but Do Not Have It” n (%) |
|---|---|
| Jar Openers | 35.0 (58.3) |
| Seat Lift | 34.0 (56.7) |
| Laundry Basket with Wheels | 30.0 (50.0) |
| Nonslip Rubber Mat | 29.0 (48.3) |
| Shopping Cart on Wheels | 29.0 (48.3) |
| Reacher | 28.0 (46.7) |
| Adhesive Tape to Stabilize Rugs | 27.0 (45.0) |
| Long- Handle Cleaning Brush | 26.0 (43.3) |
| Emergency Alert System | 26.0 (43.3) |
| Medications Reminder | 25.0 (41.7) |
| Text Enlarger | 24.0 (40.0) |
| Magnifier that I do Not Have to Hold | 22.0 (36.7) |
| Bed Or Chair Lifts | 22.0 (36.7) |
| Long-Handle Shoe Horn | 22.0 (36.7) |
| Sock Aid | 22.0 (36.7) |
| Long-Handle Sponge | 21.0 (35.5) |
| Electric Can Opener | 21.0 (35.5) |
| Rails Around Toilet | 19.0 (31.7) |
| Locator Keys | 18.0 (30.0) |
| Nail Clipper with Magnifier | 17.0 (28.3) |
| Nonslip Mat | 17.0 (28.3) |
| Dressing Stick | 17.0 (28.3) |
| Long-Handle Dustpan | 17.0 (28.3) |
| Remote Controls for Electrical Equipment | 16.0 (26.7) |
| Tub Bench | 15.0 (25.0) |
| Button Hook | 15.0 (25.0) |
| Handle for Carry Bags | 15.0 (25.0) |
| Hand Shower | 13.0 (21.7) |
| Raised Toilet Base | 13.0 (21.7) |
| Text Enlarger for PC, Tablet or Cellular | 11.0 (18.3) |
| Rail for Bed | 11.0 (18.3) |
| Simple Cellular | 11.0 (18.3) |
| Simple TV Remote Control with Large Buttons | 11.0 (18.3) |
| High Stool with Long Handle | 11.0 (18.3) |
| Long-Handle Duster | 10.0 (16.7) |
| Scooter | 9.0 (15.0) |
| Three-in-one Commode | 9.0 (15.0) |
| Lever Knobs | 9.0 (15.0) |
| Walker | 8.0 (13.3) |
| Amplified Phone | 8.0 (13.3) |
| Grab Bars | 7.0 (11.7) |
| Raised Toilet Seat | 6.0 (10.0) |
| Hand Held Magnifier | 5.0 (8.3) |
| Night Light | 5.0 (8.3) |
| Wheelchair | 3.0 (5.5) |
| Phone with Amplified Keys | 3.0 (5.5) |
| Glasses | 2.0 (3.3) |
| Cane | 1.0 (1.7) |
| Pill Organizers | 1.0 (1.7) |
| Categories | Percentage of Total Responses (%) Categories on “ I Would Use This but Do Not Have It” |
|---|---|
| Home Tasks | 37.3 |
| Home Safety | 32.2 |
| Dressing | 31.7 |
| Home Accessibility | 25.7 |
| Personal Hygiene | 25.0 |
| Medication | 21.7 |
| Reading | 21.3 |
| Mobility | 20.9 |
| Toileting | 19.6 |
| Communication | 12.2 |
| Category | Assistive Technology Reported “I Would Use This but Don’t Have It” | Number and Percentages of Responses that Reported “I Would Use This but Don’t Have It” n (%) |
|---|---|---|
| Cooking | Jar Openers | 35 (58.3) |
| Nonslip Rubber | 29 (48.3) | |
| Built-up Handles for Utensils | 27 (45.0) | |
| Home Tasks | Laundry Basket on Wheels | 30 (50.0) |
| Shopping Cart on Wheels | 29 (48.3) | |
| Long-handle Cleaning Brush | 26 (43.3) | |
| Home Safety | Adhesive tape to stabilize rug | 27 (45.0) |
| Emergency Alert System | 26 (43.3) | |
| Night Light | 5 (8.3) |
| PR-PIADS Scale (n = 60) | Study Mean | SD |
|---|---|---|
| Competence | 2.77 | 0.45 |
| Adaptability | 2.51 | 0.61 |
| Self-esteem | 1.98 | 0.49 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Orellano-Colón, E.M.; Jutai, J.; Santiago, A.; Torres, V.; Benítez, K.; Torres, M. Assistive Technology Needs and Measurement of the Psychosocial Impact of Assistive Technologies for Independent Living of Older Hispanics: Lessons Learned. Technologies 2016, 4, 21. https://doi.org/10.3390/technologies4030021
Orellano-Colón EM, Jutai J, Santiago A, Torres V, Benítez K, Torres M. Assistive Technology Needs and Measurement of the Psychosocial Impact of Assistive Technologies for Independent Living of Older Hispanics: Lessons Learned. Technologies. 2016; 4(3):21. https://doi.org/10.3390/technologies4030021
Chicago/Turabian StyleOrellano-Colón, Elsa M., Jeffrey Jutai, Angélica Santiago, Víctor Torres, Keyla Benítez, and Mayra Torres. 2016. "Assistive Technology Needs and Measurement of the Psychosocial Impact of Assistive Technologies for Independent Living of Older Hispanics: Lessons Learned" Technologies 4, no. 3: 21. https://doi.org/10.3390/technologies4030021