1. Introduction
Self-medication is a human trait in which an individual (or a member of the individuals’ family) selects and uses medicines or any other substances for the treatment of self-recognized or self-diagnosed physical or psychological ailments [
1]. Conventionally it has been described as the intake of drugs, herbs or other home remedies on an individual’s own persuasion or taking the advice of another person without consulting a physician [
2,
3]. Thus it forms an integral part of patients’ self-care which in fact is the first choice and is one of the most crucial tools when an individual encounters common health problems that do not require a doctor’s visit [
4,
5]. Due to insufficient medical facilities, the free accessibility of over-the-counter (OTC) drugs in the local market and the impoverished national drug regulatory policy, it is now becoming a very common occurrence in numerous countries of the world. Other reasons for self-medication are the shortage of time to visit a physician, inability to get a quick appointment, mild illness, long distance of hospitals and clinics from home, and finally unaffordable doctor’s fees. Moreover, extraction of much information from online sources, magazines or periodicals makes people courageous about treating their own illness [
6]. However, people are endangering their lives by practicing self-medication as it can lead to habituation, lethal allergic reactions, under dosage of medication which may not alleviate the symptom, and also over dosage that can cause collateral injury to different organs [
7].
The substances which are most extensively self-medicated are OTC drugs and dietary supplements. Besides analgesics, antimalarials, antibiotics, and cold syrups are intermittently used for self-administration [
8]. Sometimes some psychoactive drugs like recreational drugs, alcohol, and comfort foods are self-medicated to alleviate the symptoms of mental distress, stress, and anxiety [
9]. The practice of self-medication has become very familiar throughout the world [
10,
11,
12,
13] with a high prevalence rate in developing countries [
14,
15]. Some studies have found that the amplitude of self-prescribing rate with antibiotics in Asia is 4–7.5% which is higher that of 3% in northern Europe [
16]. Although self-medication, when practiced precisely can save time and is also cost effective to the patients where professional care is relatively expensive and not readily available, there are several critical health hazard issues that should be considered before endorsing the potential benefits of self-medication [
7,
17,
18]. Sometimes it may lead to wastage of resources, boost up resistance to pathogens, and cause severe health problems, including adverse drug reaction, addiction, and ultimately death [
7].
There are no examples of data relating health hazards and health care utilization including the practice of self-medication among young adults, but it is expected that they are highly motivated towards self-administration of drugs by the internet and media [
19]. A study carried out by the university students of Karachi, Pakistan demonstrated that the propensity of self-prescribing of medications among medical students was 77.7%, and was 83.3% for non-medical students [
20]. So the study on self-practice of medications among university pharmacy undergraduates is imperative as they are that segment of the population who are well educated and have access to all the information regarding their health. Moreover study on the tendency of self-medication practice among pharmacy undergraduates is essential as they are the oncoming drug prescribers and health educationalist [
5].
Over-the-counter (OTC) drugs are the only drugs which can be self-prescribed and sold in convenience stores, grocery stores, and health shops without prescription as they are less hazardous [
21]. In Bangladesh paracetamol, ORS saline, metronidazole, ranitidine, omeprazole, aspirin, and diaclofenac sodium etc. are accepted to be sold as OTC drugs. However, due to immoral drug sellers and improper regulation, 90% of stocked drugs are sold without any prescription and therefore the phenomenon of self-medication is a common topic in our country [
21]. Besides there have been very confined researches conducted regarding the impact of self-medication practice among university pharmacy undergraduates [
15].
Considering all this evidence, this research work focuses on assessing the perceptions about self-medication practice among the pharmacy students of Bangladesh. The study also compares the attitudes toward and the extent of practicing self-care between male and female students, as well as the year in pharmacy school.
2. Methods
2.1. Study Design
This population-based cross-sectional study was carried out to investigate the knowledge, attitudes and practice of self-medication among the undergraduate pharmacy students of Bangladesh from January to June, 2016. The study was conducted by using both qualitative and quantitative data.
2.2. Study Area
To conduct the study, the pharmacy department of five public universities of Bangladesh namely Dhaka University, Jahangirnagar University, Chittagong University, Comilla University, and Noakhali Science and Technology University were chosen as the study area. The above mentioned universities were chosen by the field investigators based on the availability and accessibility of the participants. Time and distance were also the key factors for the selection of the study areas.
2.3. Study Participants
The study included 250 undergraduate students (131 male and 119 female) enrolled in a Bachelor of Pharmacy program who understood English, aged between 18–25 years and were permanent residents of Bangladesh, with different socioeconomic backgrounds from five different public universities. Both residential and nonresidential students were selected randomly, i.e., we did not consider whether the students were resident or non-resident in different halls of the university. Before data collection each and every participant was clearly informed about the purpose of the study and a written consent was taken from each of the respondents.
2.4. Participants and Eligibility Criteria
This study included only those respondents who were easily available for data collection and interested to provide information willingly. Those who did not feel comfortable to give information were excluded from the study.
2.5. Sampling and Sample Size
A simple random sampling technique was used for the selection of study participants. The sample size was calculated assuming that 50% of the undergraduate pharmacy students had a tendency of self-medication practice with 5% margin of error and 95% confidence interval. The sample size was calculated to be 232. However, to ensure more representative data, we selected a larger sample size of 250 for this study.
2.6. Data Collection
The procedure of data collection was segmented into three steps. The first step was to fill out the questionnaire including socio-demographic information by the study subjects. The second step was to discuss the study protocol, and the final step was to cross-check the questionnaires filled by the respondents. The questionnaire was adopted from a formerly published study which was developed, standardized, and previously used by Kumar et al. [
4] for undergraduate pharmacy students. The questionnaire was divided into four segments and consisted of 16 close-ended and 11 open-ended questions.
Section 1 contained questions related to socio-demographic information of the respondents.
Section 2 included questions about the practice of self-medication by the respondents.
Section 3 was concerned with the knowledge and awareness related questions of the respondents while
Section 4 was on questions related to the perception of the respondents regarding self-medication practice.
The questionnaire was distributed to the selected student together with a written consent form that explained the purpose of the research and assured them of their confidentiality. The interviews lasted for 15 min and included a range of questions about self-medication along with an explanation about self-medication, its main principles, as well as evidence based and practical demonstration. The questionnaire was constructed in English and translated to Bengali by the interviewers to make the questions easily understandable to the participants during the interview. They were asked to complete the questionnaire immediately. The authors were present on hand to answer questions or clarify any doubts that they might have.
2.7. Statistical Analysis
Data analyses were conducted using SPSS software version 20.0 (SPSS Inc., Chicago, IL, USA). Descriptive statistics was used for the calculation of proportions. The Chi-square test was performed to measure the association between the demographic characteristics and responses to understanding, perceptions and self-use of medication. The p values were calculated by the Chi-square test. An alpha level of 0.05 or less was considered significant. The Microsoft excel program was used for data analysis and for chart, graph, and diagram preparation.
4. Discussion
People have always been very cautious about their personal health status and for this they have used self-medication, a feature of healthcare, from ancient times. Although self-medication has many pros and cons it depends on who uses it and how it is used for self-treatment [
4]. We focused on pharmacy students because they have adequate knowledge of medicine in theory and are more cautious about the safety of drugs which is lacking in other student groups or in the general population. Thus a pharmacy student’s view on the self-medication practice can be considered as a major factor to judge the characteristics of their future prescription pattern.
Students of Bangladesh frequently use self-medication and gender difference has not been shown to have any influence on the practice of self-medication. The reason behind insignificant gender differences in the overall exercise of self-medication may be the study format that allowed the respondents to select drugs by themselves [
5]. In our study we found that about 88.0% of the students self-practice different types of medication. A similar type of study was conducted by Kumar et al. [
4] in coastal south India and signified that the amplitude of self-medication practice was 78.90% among medical students. Other similar studies also demonstrated the prevalence rate of self-medication ranged between 57.1% and 92% among the medicals students in India [
22]. Several research works carried out in other developing countries revealed that the prevalence of self-medication was 38.5% and 43.2% among medical, pharmacy, and health science students in Ethiopia [
22,
23], 51% among citizens in Slovenia [
24], 55.3% and 55% among medical students in Pakistan [
25] and Egypt [
26] respectively, 56.9% among medical undergraduate students in Nigeria [
27], and 80.9% among female university students in Malaysia [
28]. The major influential reason behind the higher propensity of self-medication might be the unregulated easy availability of all categories of medicine without prescription.
Similar to some previously published articles [
22,
29,
30,
31], headache, common cold, fever, pain, and vomiting were the most common symptoms for self-administration of medications mentioned by the respondents. It was quoted in our research report that the most common cause for self-treatment with drugs was the insignificance of the illness which did not require a doctor’s visit. Similar outcomes were reported by the study conducted in India [
7,
32]. This type of attitude of the respondents may be attributed to a disregard and absence of consciousness about the advancement of diseases. Sometimes the people who practice medication for self-treatment may suffer from a serious illness as the symptoms of many diseases are primarily mild but wrong diagnosis and treatment may promote serious health hazards. However, in agreement with other studies, easy availability of medicines [
4,
6], quick relief [
16], and time saving [
33] were found to be the other causatives for preferring self-medication practice.
As stated earlier, antipyretics, analgesics, antacids, and antidiarrheal drugs were the most common classes of drugs self-prescribed for treatment by almost all of the respondents in our study. Almost identical observations were found in the studies conducted in India [
4,
34], Pakistan [
32], Iran [
35], and Ethiopia [
8] where these common classes of drugs were frequently used by medical students. Meanwhile, the use of antibiotics was different to that of analgesics and antipyretics. This tendency is because of the knowledge of pharmacy graduates on the resistance and side effects of antibiotics. It is well known that proper medicinal knowledge can promote a good prescribing pattern of pharmacists. However, at the same time inappropriate or irrational use of these drugs can lead to various hazardous effects including the reduction in the capability of microbial flora to resist detrimental microorganisms, the development of multidrug resistance, addiction, toxicity, and other related syndromes [
32]. Therefore, such kind of practice should be discouraged.
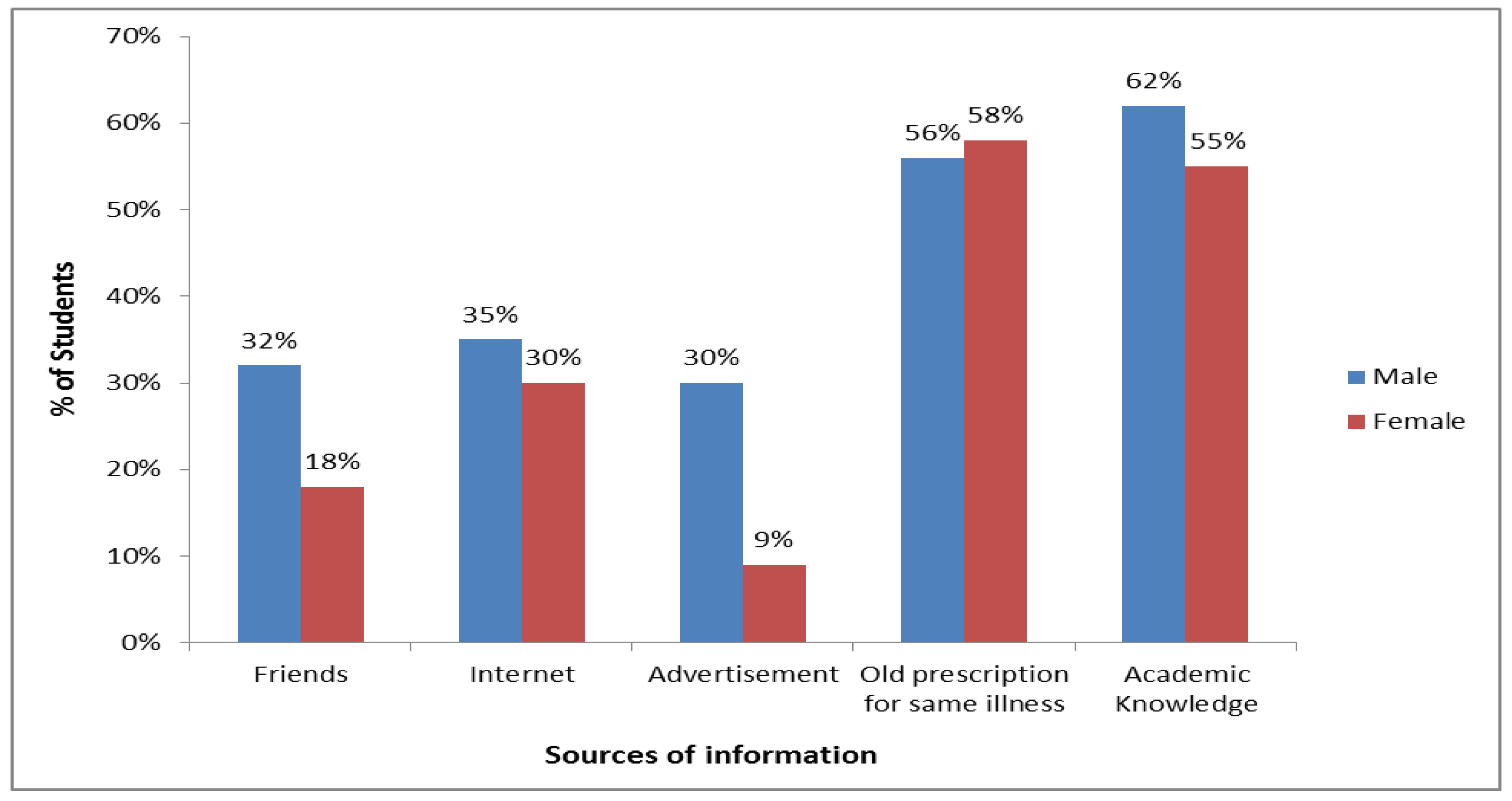
Our study found that the key factor for self-medication practice by the participants was their adequate pharmacological knowledge which they had gathered from their academic courses. These findings are similar to those from studies conducted in Nepal [
7], India [
4,
33], Malaysia [
36], Ethiopia [
8], and Pakistan [
32]. The second major source of information on self-prescribed drugs was from previous prescriptions for the same illness and this result was analogous to the findings of the study conducted in India [
4,
33]. Further, other researches conveyed in India [
34] and Ethiopia [
8] reported the internet as another common source of knowledge on self-prescribed medicines which was the third common source of information in our study results.
The fact that majority (52.80%) of the respondents gathered information about self-medication from the previously prescribed medicines of physicians was consistent with the research work conducted earlier [
37]. However as the respondents were younger, they were also influenced by other sources like previous illness experiences, opinions of family members, friends and local people, and advertisement. This result resembles formerly conducted research findings [
23,
37]. All the students irrespective of the year of the study reported that they were completely aware of the treatment procedure using self-medication. They were also cautious about completing the dose of the medicine, checking the instructions given on the insert before using and also looking for the expiry date of the drug before using it. Less awareness was noted among 1st year students which was similar to the findings of Kalyan et al. [
38] and Sontakke et al. [
34] Non-inclusion of pharmacology as a subject in the 1st year curriculum could be the reason.
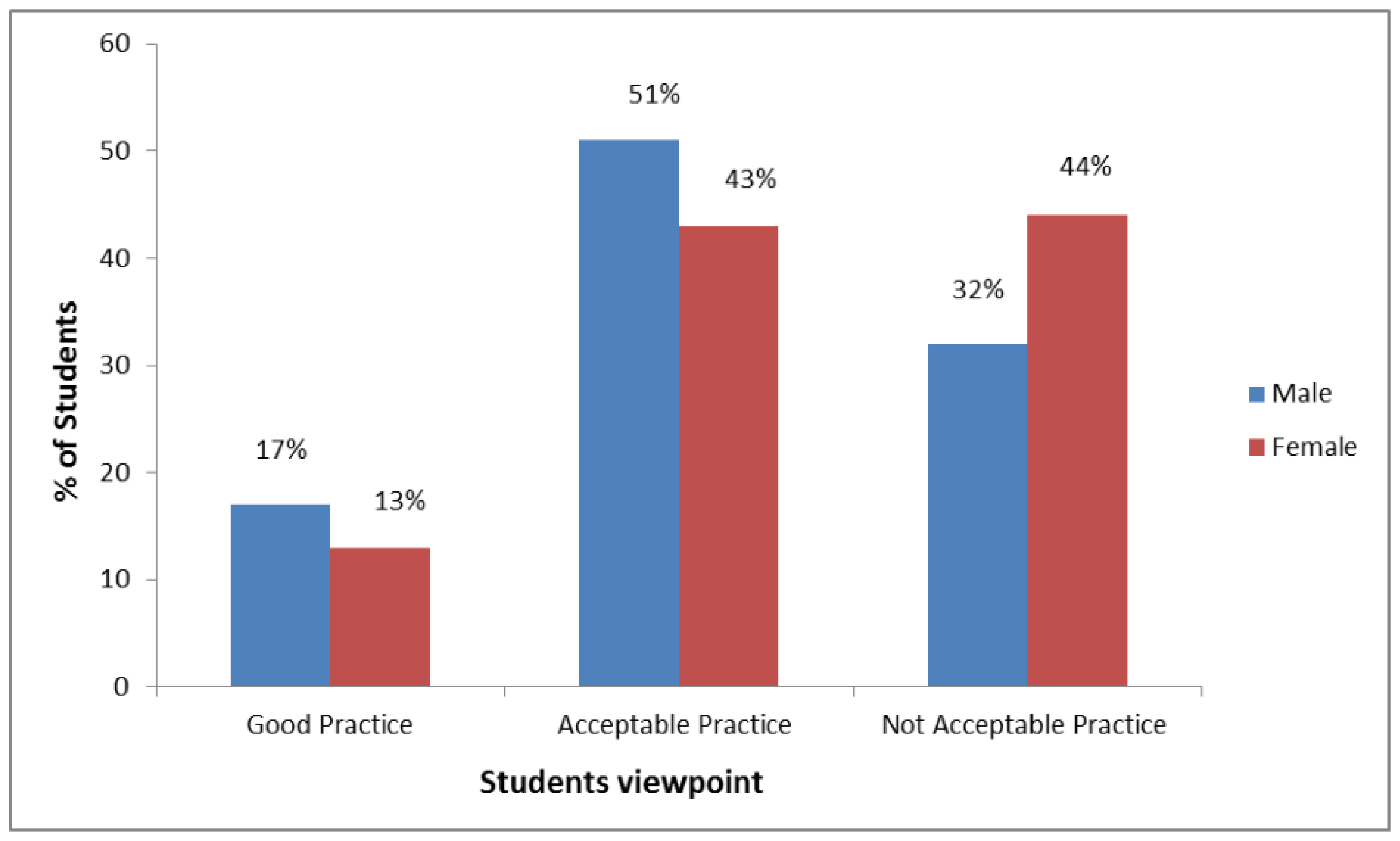
In this research work, about 73.2% of the respondents believed the practice of self-medication to be part of their own health-care and the proportion was higher than the reports from India [
34], Ethiopia [
22], and Pakistan [
25]. Self-medication can only be considered a part of self-care if legitimate use of medicaments can be ensured. It may lead to accidental drug toxicity as there is always a risk of using expired drugs and also sharing with friends or taking medicines that have been actually prescribed for other problems [
4,
29,
32,
39].