Assessing Patient bypass Behavior Using Taxi Trip Origin–Destination (OD) Data
Abstract
:1. Introduction
2. Methods
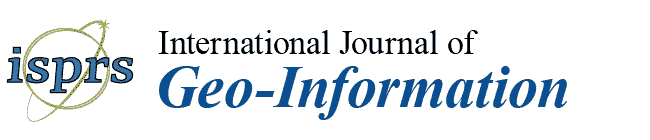
2.1. Datasets and Study Area
- PointID: record identification;
- TaxiID: sampled taxi identification;
- Longitude: longitude information for a taxi during the recording period;
- Latitude: latitude information for a taxi during the recording period;
- Time: the recording time; and
- State: whether a taxi is with (1) or without (0) passengers.
2.2. Bypass Behavior Assessment Indices
Bypass Behavior Index
Index 1: Hospital bypass trip distance ranking
Index 3: Hospital bypass proportion
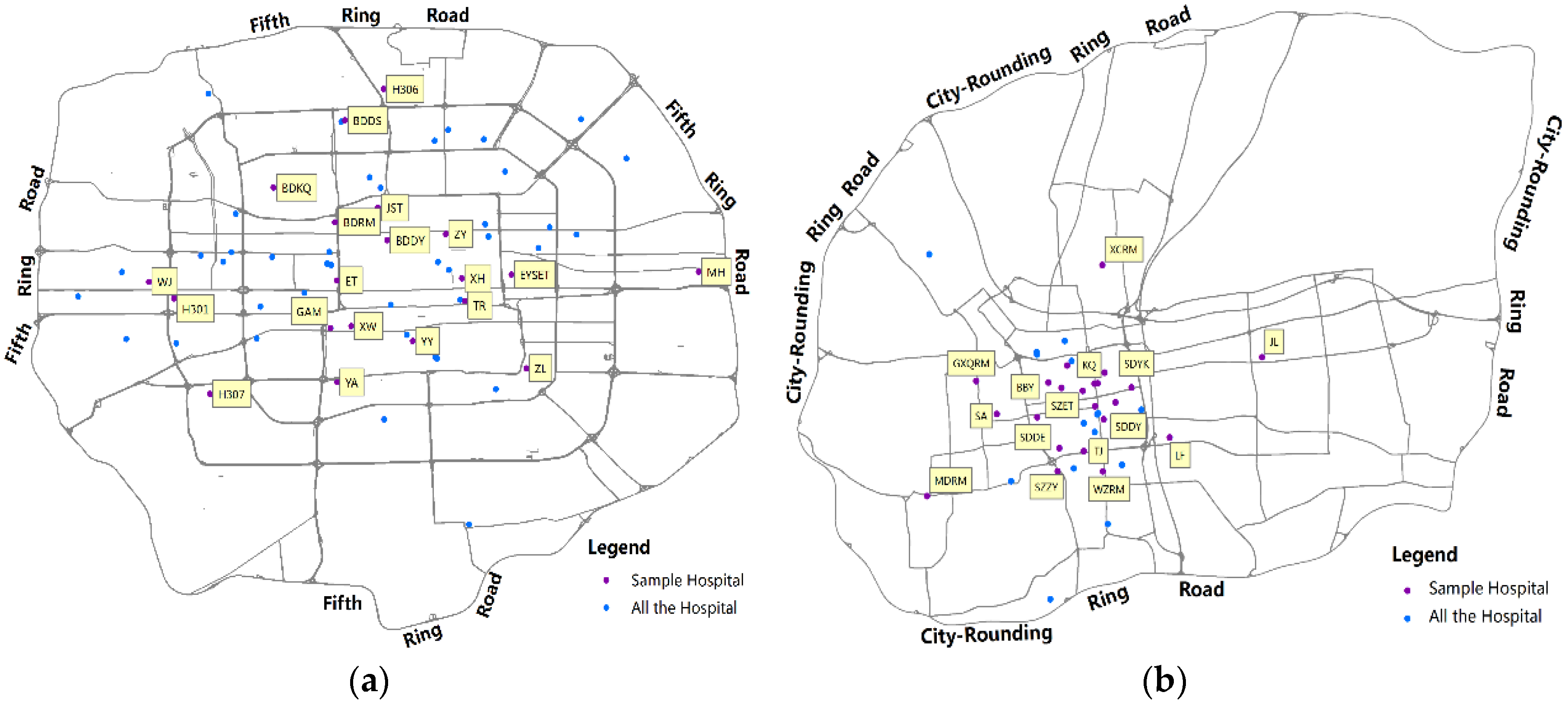
2.3. Source Point Recognition
- Step 1
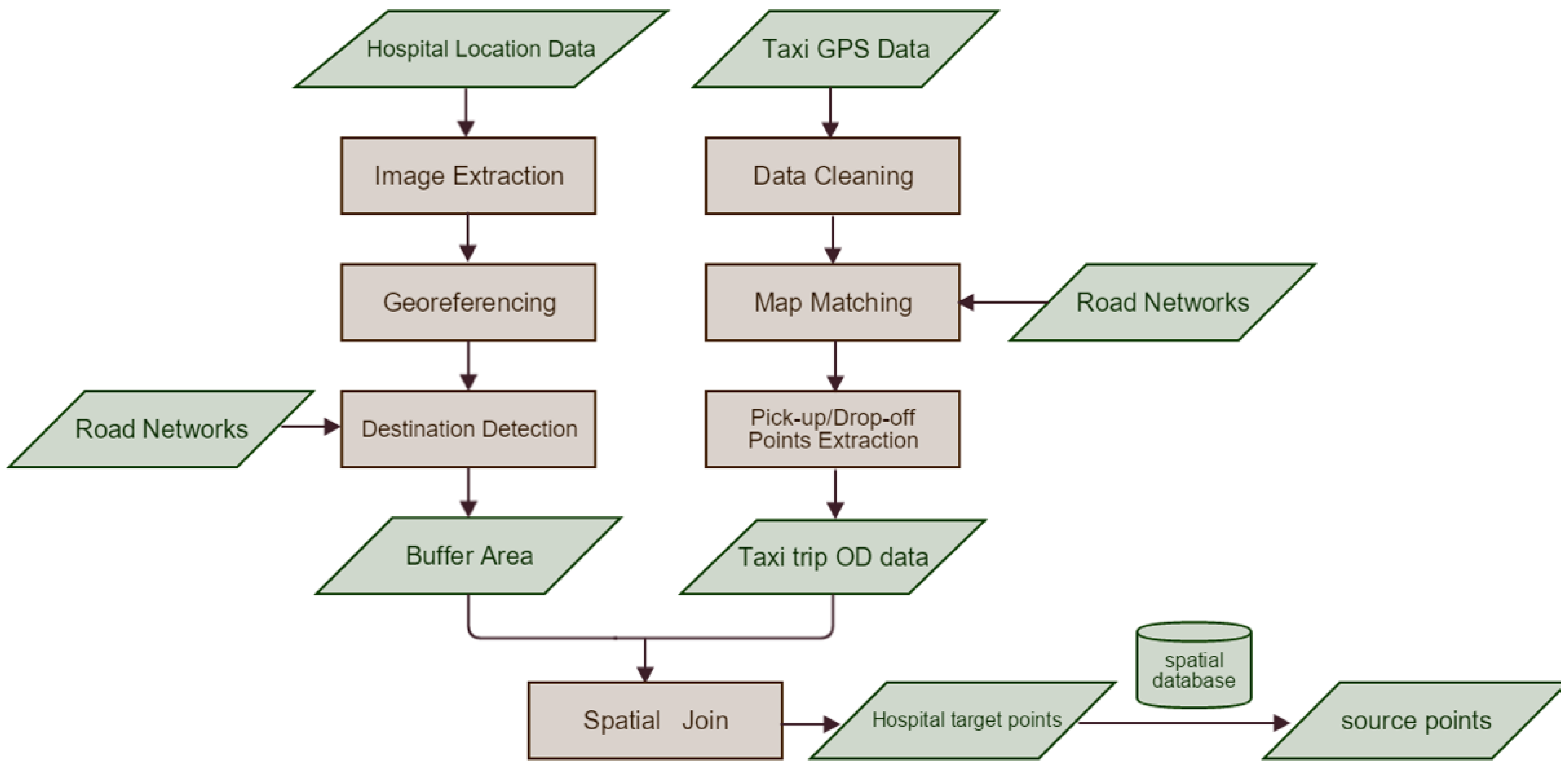
- Extract the image with the area surrounding ZL according to Google Earth, and then georeference the image to the map coordinate system of the existing road network in ArcGIS 10.1 as shown in Figure 3a (the red line indicates the road network).
- Step 2
- Create an outline of ZL through image interpretation and find its west and south gate as shown in Figure 3b (the translucent blue polygon indicates the spatial environment of ZL).
- Step 3
- Focus on the two gates. Draw the potential target point area (roughly 50 m along the road) separately. When GPS positioning error issues are encountered, the potential area can be covered. The yellow polygon in Figure 3c shows the potential ZL area; therefore, origin and destination points in the yellow polygon serve as the target points of ZL.
- Step 4
- Identify each target point’s corresponding source point in the database (points that belong to the same trip). Figure 3d presents some of the ZL source points on a map.
3. Results
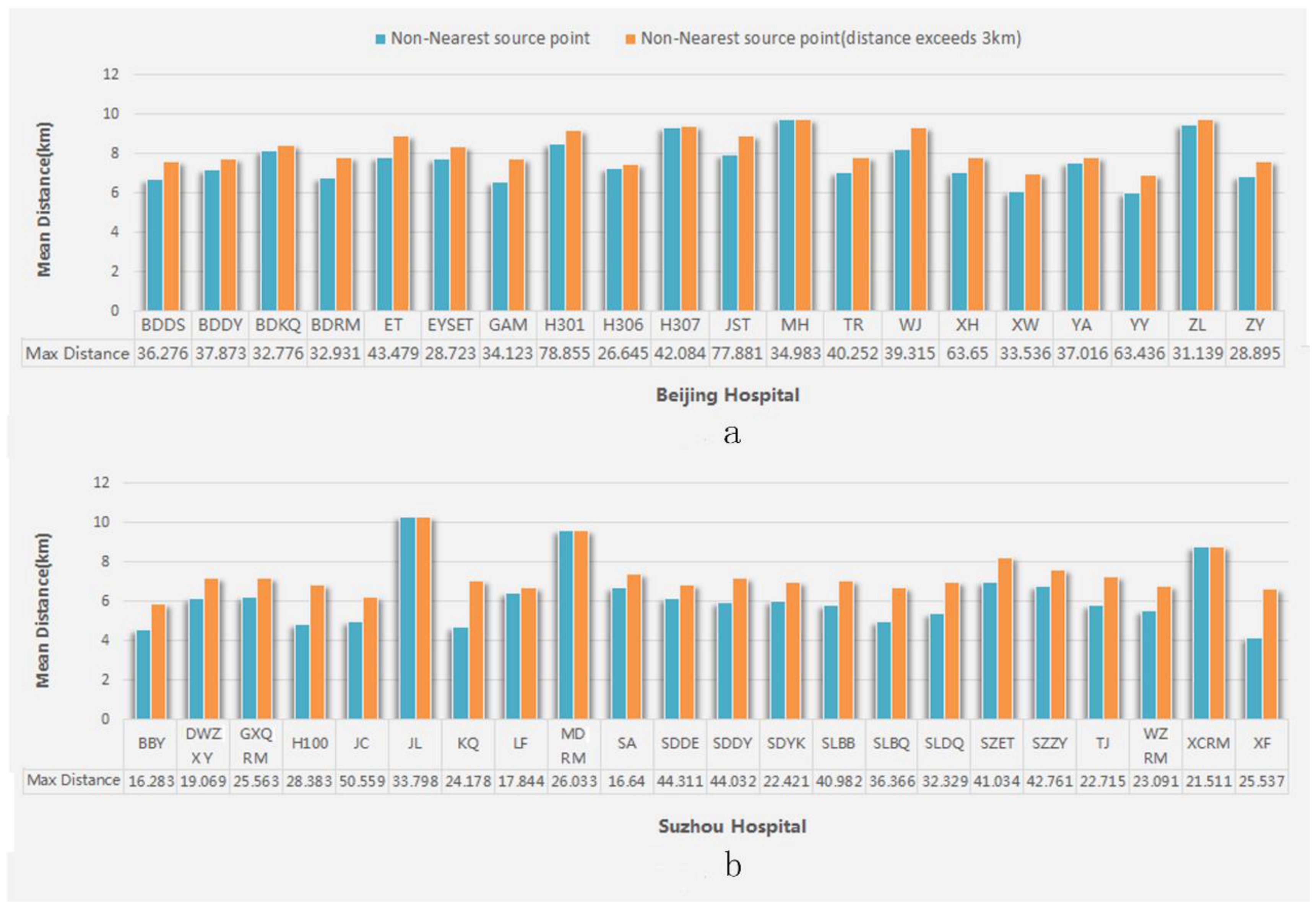
3.1. Statistical Characteristics of Hospital Bypass Distance
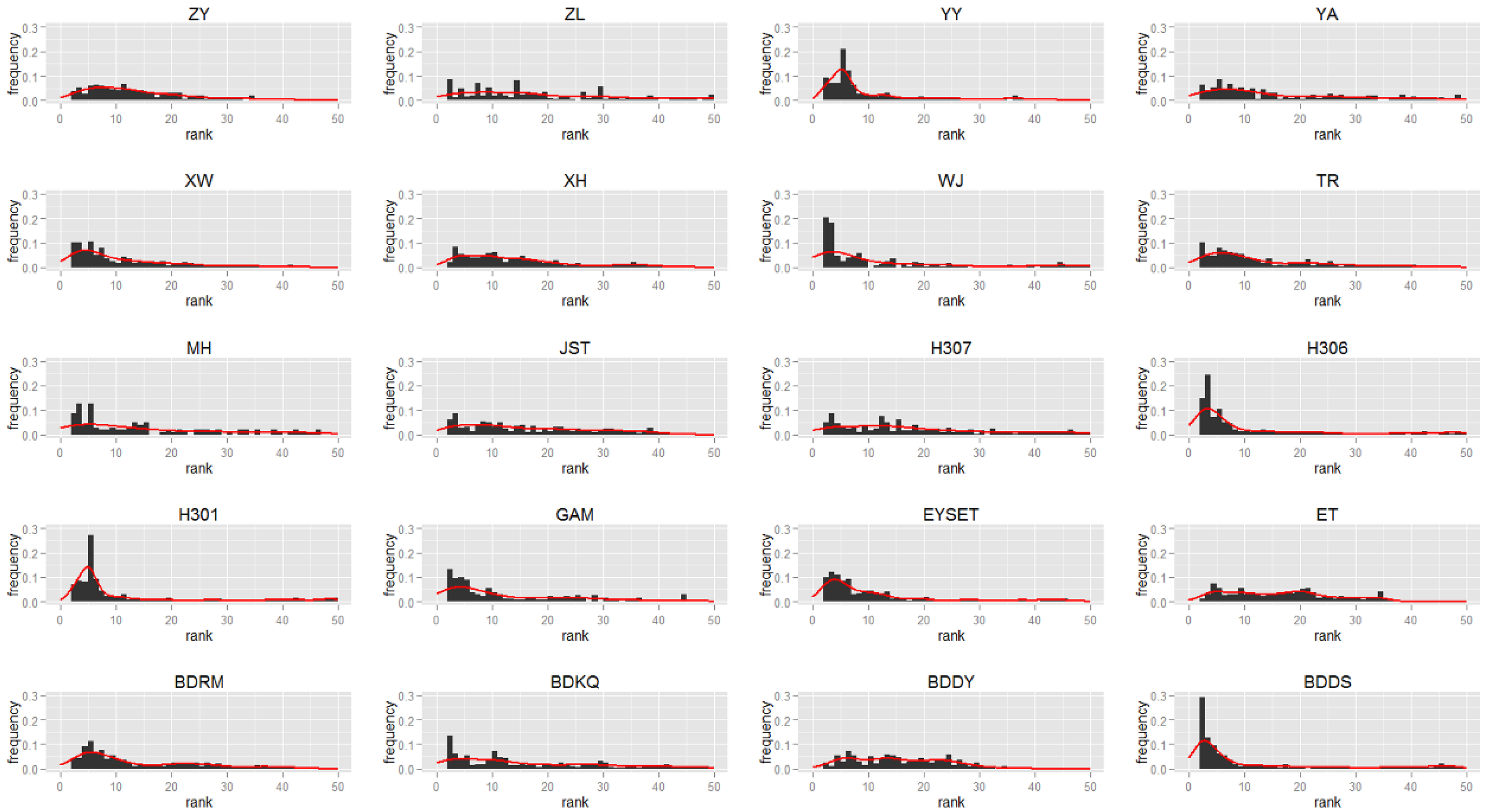
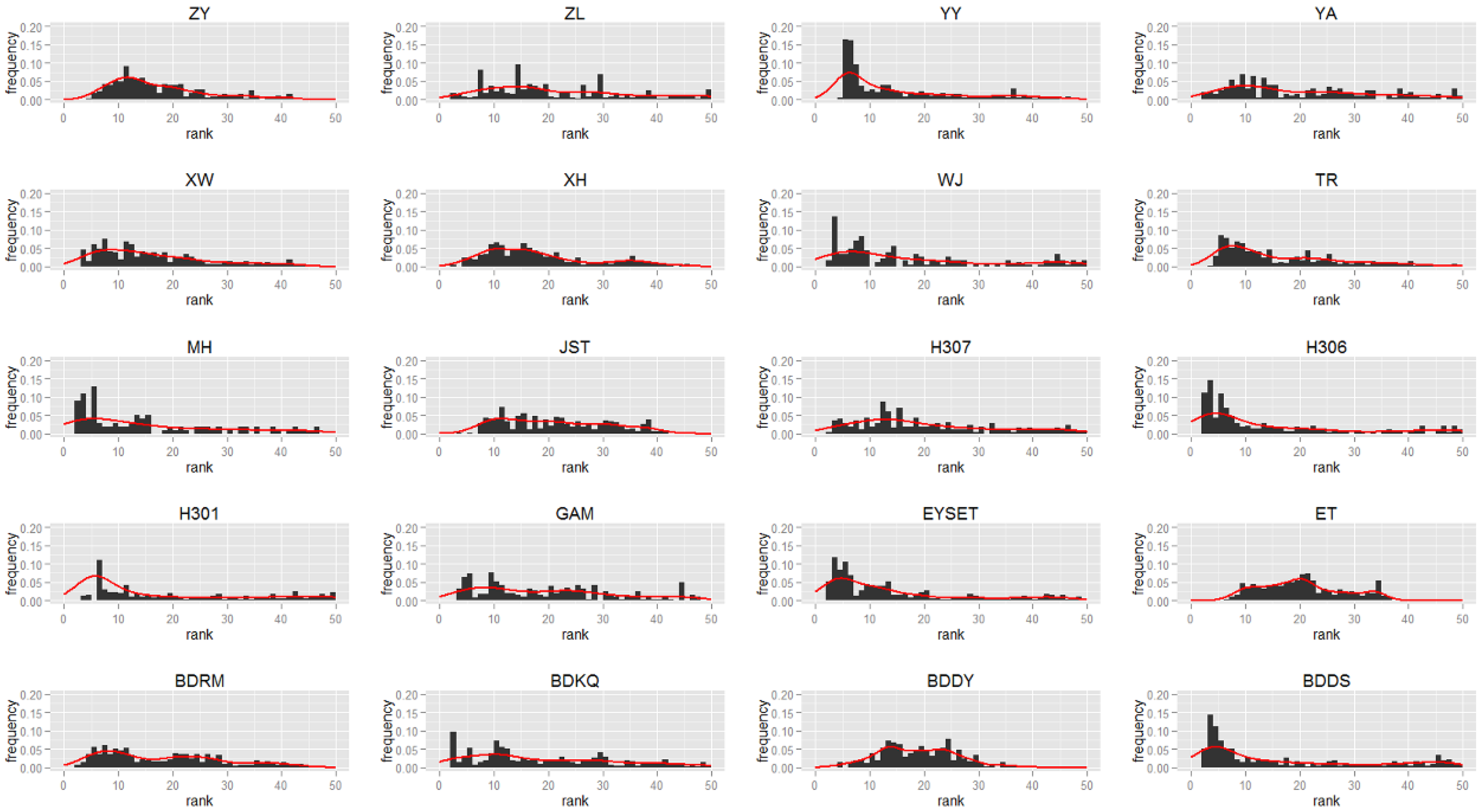
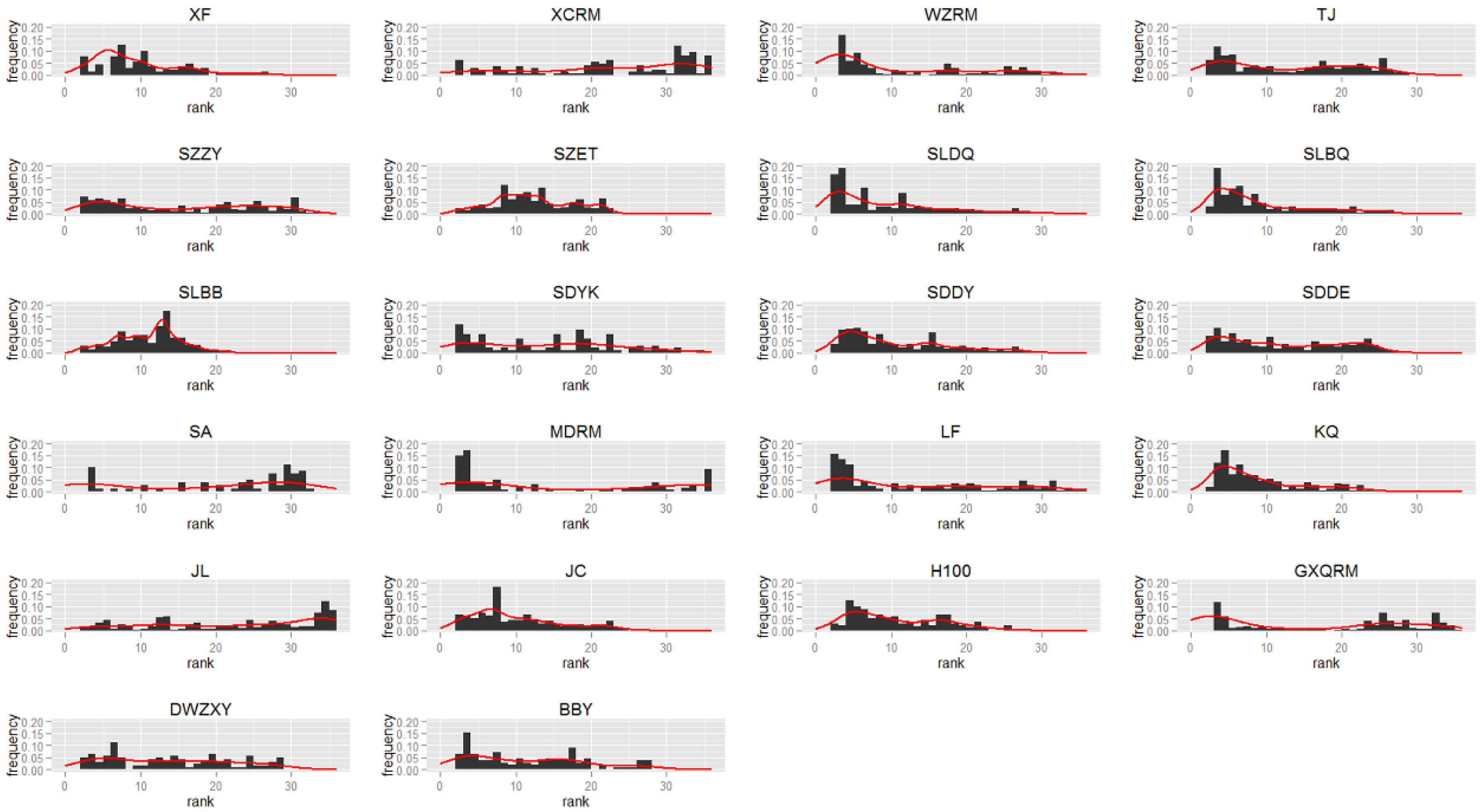
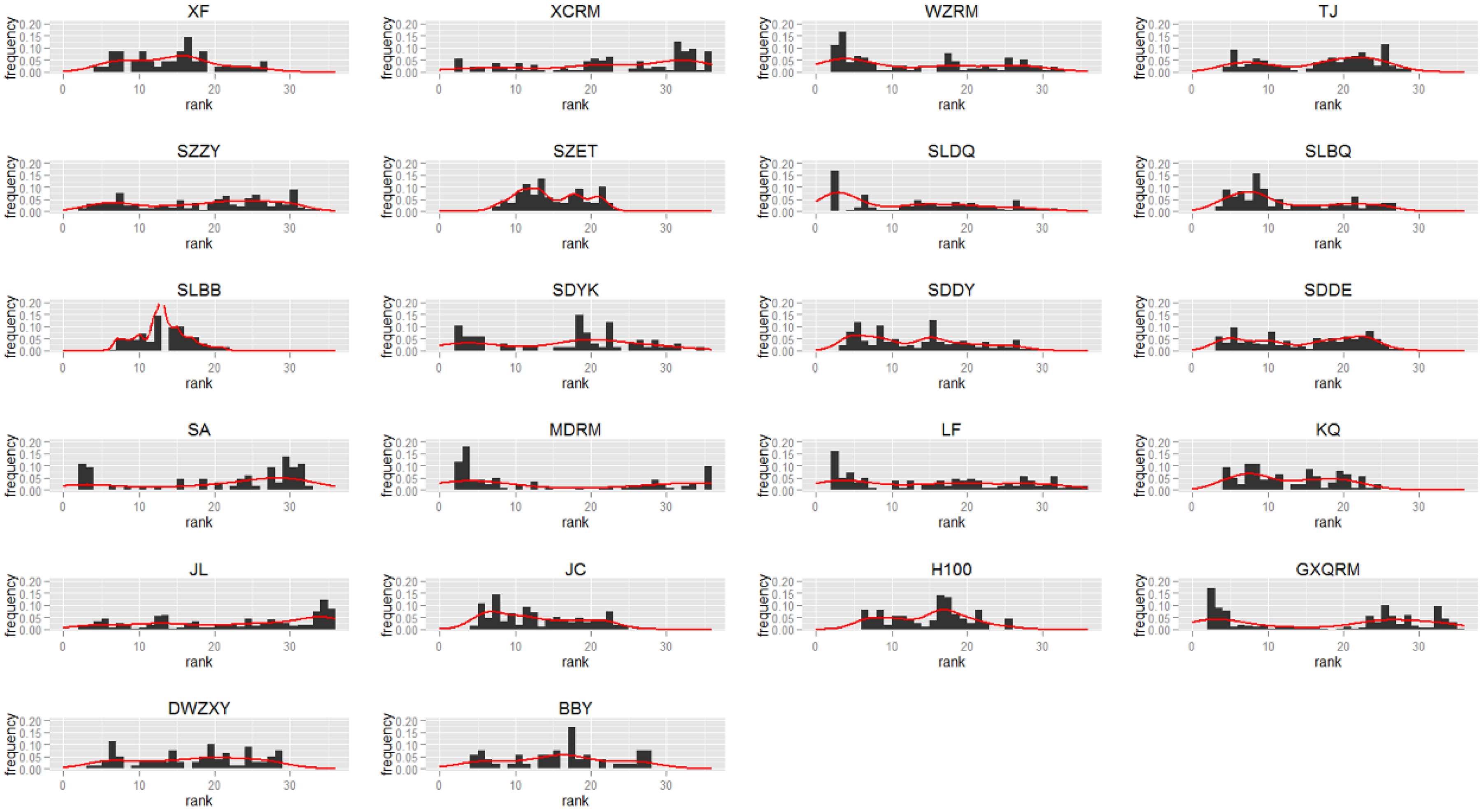
3.2. Distance Ranking Characteristics
- Hospital bypass source points are mainly found between the sections ranked 2 and 10, which include YY, XW, EYSET, BDDS, GAM, H306, WJ, and H301;
- Hospital bypass source point distributions are relatively uniform between the sections ranked 2 and 30, which include BDRM, TR, ZY, XH, BDDY, ET, and JST;
- Hospital bypass source points show clear distribution patterns in the sections ranked 30–50, which include ZL, H307, MH, YA, and BDKQ.
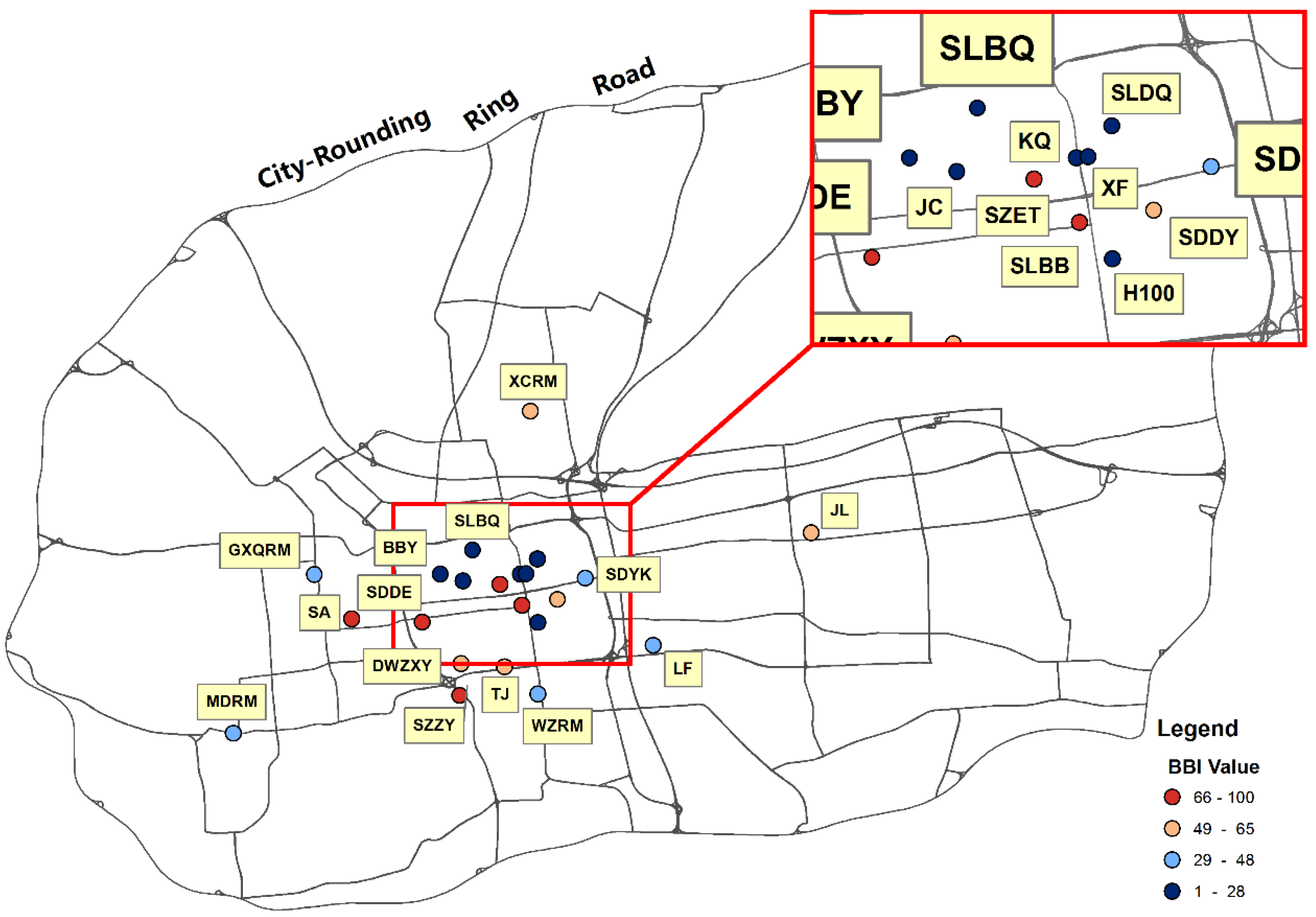
- Hospital bypass source points are mainly found between the sections ranked 2 and 15, which include XF, WZRM, TJ, SZET, SLDQ, SLBQ, SLBB, SDDY, LF, KQ, JC, H100, and BBY;
- Hospital bypass source point distributions are relatively uniform from the sections ranked 2 to 30, which include SZZY, SDYK, SDDE, and DWZXY;
- Hospital bypass source points show a clear distribution pattern from the section ranked 30 to the end, which account for XCRM, SA, MDRM, GXQRM, and JL.
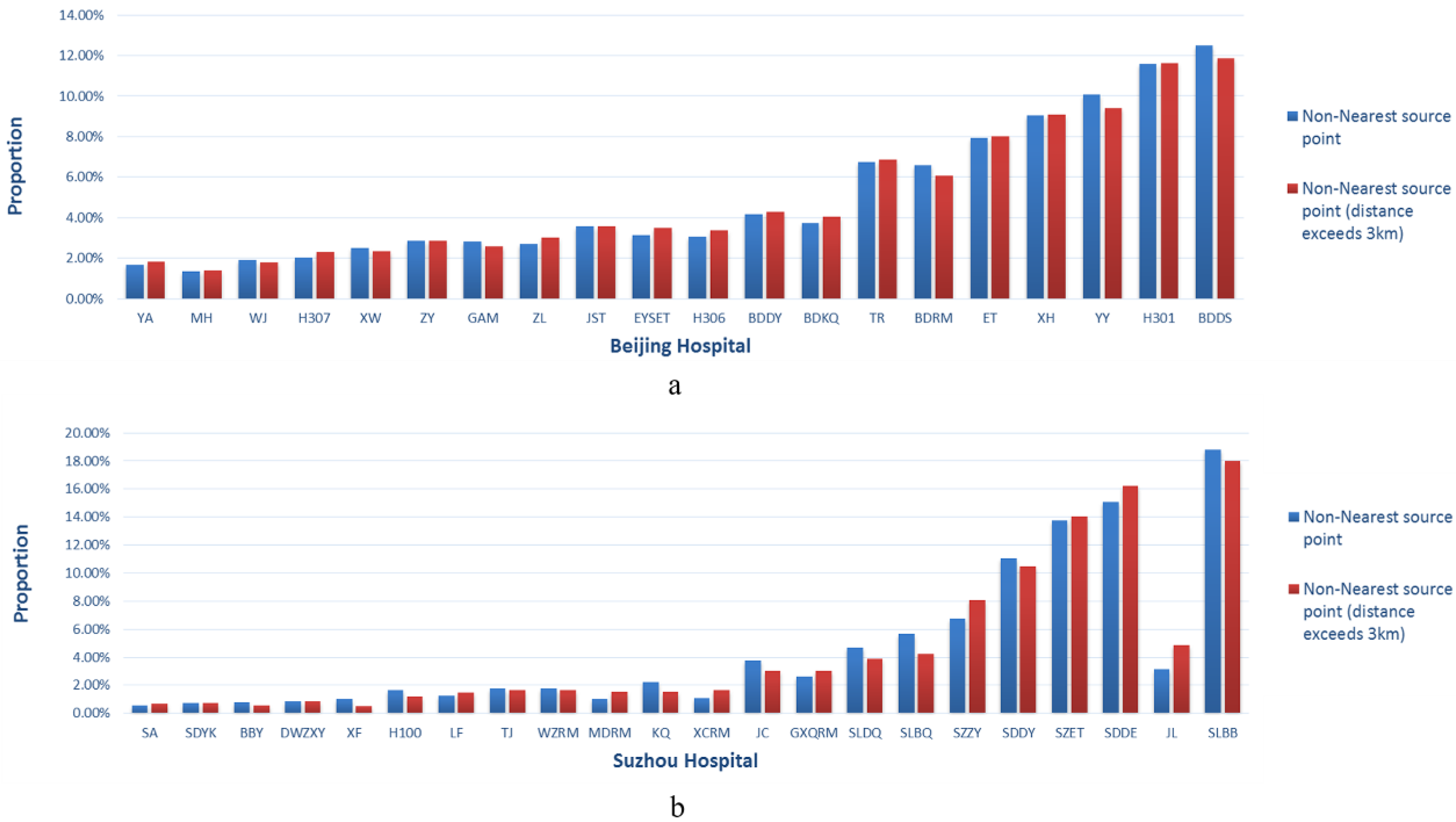
3.3. Hospital Bypass Share
3.4. Hospital Bypass Proportion
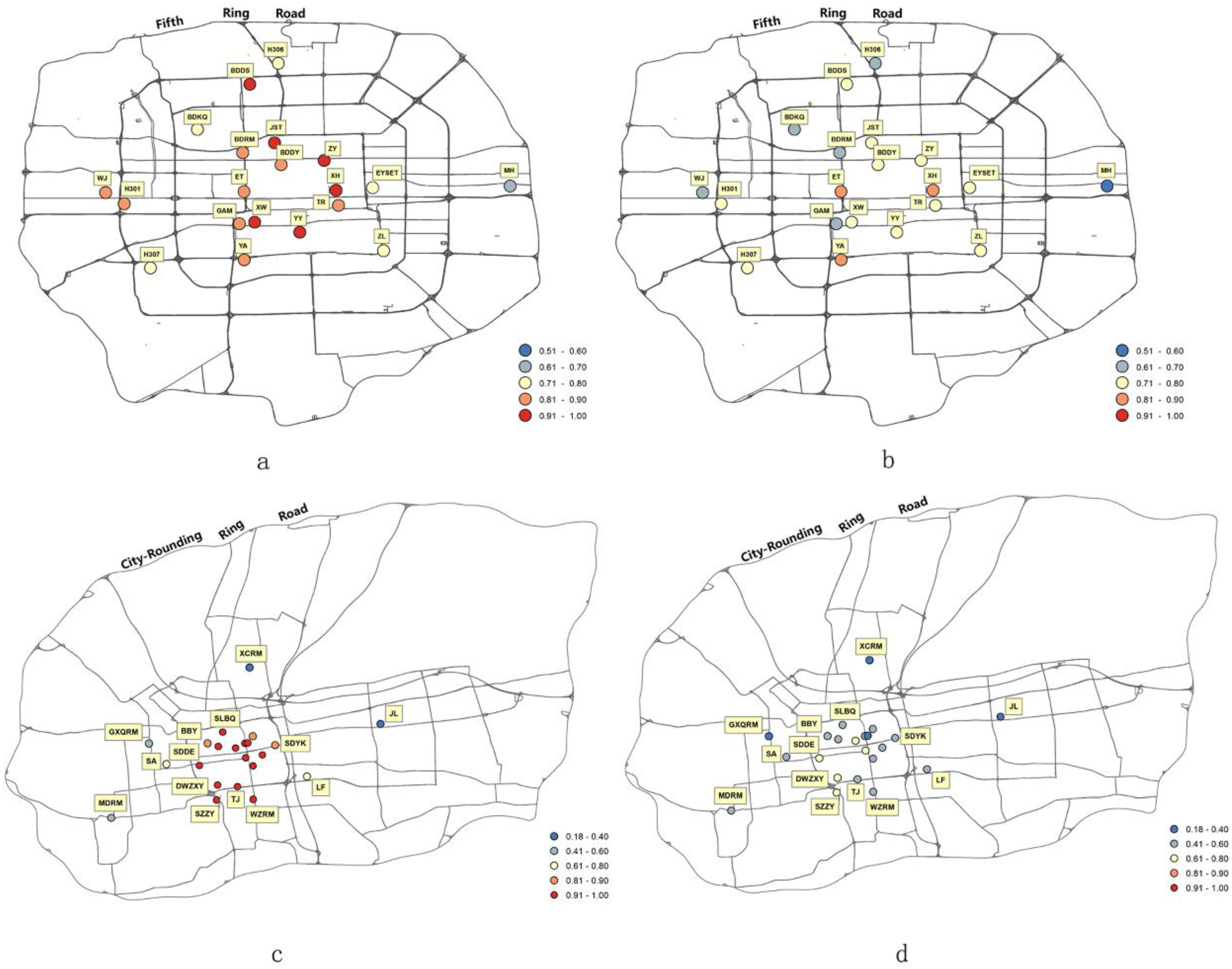
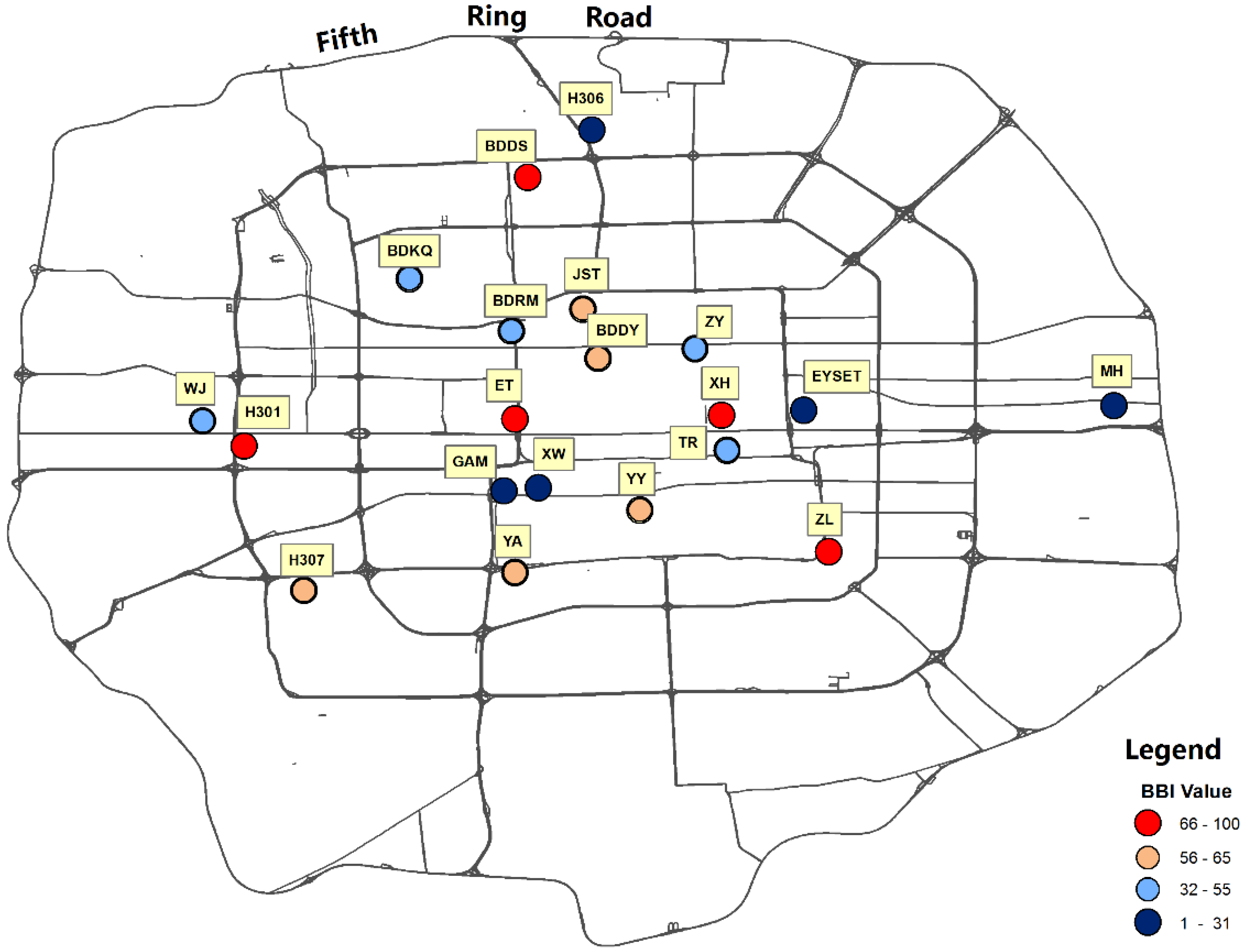
3.5. Bypass Behavior Assessment
4. Discussion
4.1. Bypass Behavior Analysis
4.2. Comparisons between the Two Study Areas
5. Conclusions
- For the Beijing hospitals examined, H301, ET, XH, BDDS, and ZL occupy the top five BBI rank positions; for the Suzhou hospitals examined, SDDE, SZZY, SLBB, ET, and SA occupy the top five BBI rank positions.
- Hospital reputation, transport considerations, and spatial distributions may influence BBI variations. The presence of specialty departments, convenient transportation access, and prime location features increase a hospital’s bypass level.
- Generally speaking, patient hospital bypass phenomena are likely to be more pronounced in Beijing. Differences in the bypass trip distances between hospitals are more significant in Suzhou. These results are likely attributable to differences in hospital distribution patterns and quality levels between the two cities.
Acknowledgments
Author Contributions
Conflicts of Interest
Appendix A
| Location | Full Name of Hospital | Abbreviation |
|---|---|---|
| Beijing | Peking University Third Hospital | BDDS |
| Beijing | Peking University First Hospital | BDDY |
| Beijing | Peking University School of Stomatology | BDKQ |
| Beijing | Peking University People’s Hospital | BDRM |
| Beijing | Beijing Children’s Hospital affiliated to Capital Medical University | ET |
| Beijing | Children’s Hospital affiliated to The Capital Institute of Pediatrics | EYSET |
| Beijing | Guang’anmen Hospital affiliated to China Academy of Chinese Medical Sciences | GAM |
| Beijing | 301 Hospital | H301 |
| Beijing | 306 Hospital | H306 |
| Beijing | 307 Hospital | H307 |
| Beijing | Beijing Jishuitan Hospital | JST |
| Beijing | Civil Aviation General Hospital | MH |
| Beijing | Beijing Tongren Hospital affiliated to Capital Medical University | TR |
| Beijing | The Armed Police General Hospital | WJ |
| Beijing | Peking Union Medical College Hospital | XH |
| Beijing | Xuan Wu Hospital affiliated to Capital Medical University | XW |
| Beijing | Beijing You’an Hospital affiliated to Capital Medical University | YA |
| Beijing | Beijing Friendship Hospital affiliated to Capital Medical University | YY |
| Beijing | Cancer Hospital affiliated to Chinese Academy of Medical Sciences | ZL |
| Beijing | Beijing Hospital of Traditional Chinese Medicine | ZY |
| Suzhou | Suzhou Beibingying Hospital | BBY |
| Suzhou | Suzhou Dongwu Hospital integrating Traditional Chinese & Western Medicine | DWZXY |
| Suzhou | Suzhou Gaoxinqu People’s Hospital | GXQRM |
| Suzhou | 100 Hospital | H100 |
| Suzhou | Suzhou Jinchang Medical Beauty | JC |
| Suzhou | Suzhou Kowloon Hospital affiliated to Shanghai Jiaotong University Medical School | JL |
| Suzhou | Suzhou Stomatological Hospital | KQ |
| Suzhou | Suzhou Gongyeyuanqu Loufeng Hospital | LF |
| Suzhou | Suzhou Mudu People’s Hospital | MDRM |
| Suzhou | Suzhou SaintLove Plastic Beauty | SA |
| Suzhou | The Second Affiliated Hospital of Soochow University | SDDE |
| Suzhou | The First Affiliated Hospital of Soochow University | SDDY |
| Suzhou | Lixiang Eye Hospital of Soochow University | SDYK |
| Suzhou | Suzhou Municipal Hospital, Headquarters | SLBB |
| Suzhou | Suzhou Municipal Hospital, North District | SLBQ |
| Suzhou | Suzhou Municipal Hospital, East District | SLDQ |
| Suzhou | Children’s Hospital of Soochow University | SZET |
| Suzhou | Suzhou Hospital of Traditional Chinese Medicine | SZZY |
| Suzhou | Suzhou Tongji Medical Cosmetology | TJ |
| Suzhou | Suzhou Wuzhong People’s Hospital | WZRM |
| Suzhou | Suzhou Xiangcheng People’s Hospital | XCRM |
| Suzhou | The Fire Hospital of Suzhou | XF |
Appendix B
| Hospital | Non-Neighboring Hospital Bypass Distances (km) | Non-Neighboring Hospital Bypass Distances (Exceeding 3 km) | ||||||
|---|---|---|---|---|---|---|---|---|
| Mean | Max | STDEV | Var | Mean | Max | STDEV | Var | |
| BDDS | 6.706 | 36.276 | 4.626 | 21.400 | 7.577 | 36.276 | 4.556 | 20.756 |
| BDDY | 7.199 | 37.873 | 4.624 | 21.379 | 7.732 | 37.873 | 4.573 | 20.914 |
| BDKQ | 8.129 | 32.776 | 4.909 | 24.101 | 8.397 | 32.776 | 4.869 | 23.706 |
| BDRM | 6.795 | 32.931 | 4.966 | 24.661 | 7.842 | 32.931 | 4.991 | 24.915 |
| ET | 7.838 | 43.479 | 5.520 | 30.466 | 8.887 | 43.479 | 5.360 | 28.733 |
| EYSET | 7.766 | 28.723 | 4.541 | 20.625 | 8.374 | 28.723 | 4.386 | 19.234 |
| GAM | 6.549 | 34.123 | 4.345 | 18.883 | 7.758 | 34.123 | 4.187 | 17.529 |
| H301 | 8.524 | 78.855 | 6.706 | 44.975 | 9.206 | 78.855 | 6.733 | 45.337 |
| H306 | 7.264 | 26.645 | 4.625 | 21.389 | 7.477 | 26.645 | 4.616 | 21.308 |
| H307 | 9.332 | 42.084 | 5.455 | 29.756 | 9.429 | 42.084 | 5.437 | 29.564 |
| JST | 7.931 | 77.881 | 6.130 | 37.574 | 8.921 | 77.881 | 6.116 | 37.411 |
| MH | 9.754 | 34.983 | 5.323 | 28.336 | 9.754 | 34.983 | 5.323 | 28.336 |
| TR | 7.077 | 40.252 | 4.559 | 20.781 | 7.806 | 40.252 | 4.398 | 19.340 |
| WJ | 8.224 | 39.315 | 6.060 | 36.719 | 9.337 | 39.315 | 5.964 | 35.565 |
| XH | 7.080 | 63.650 | 4.716 | 22.242 | 7.802 | 63.650 | 4.631 | 21.449 |
| XW | 6.138 | 33.536 | 4.172 | 17.407 | 7.011 | 33.536 | 4.149 | 17.214 |
| YA | 7.545 | 37.016 | 4.744 | 22.504 | 7.796 | 37.016 | 4.739 | 22.461 |
| YY | 5.988 | 63.436 | 4.369 | 19.086 | 6.881 | 63.436 | 4.377 | 19.155 |
| ZL | 9.497 | 31.139 | 5.301 | 28.100 | 9.753 | 31.139 | 5.223 | 27.276 |
| ZY | 6.858 | 28.895 | 4.618 | 21.329 | 7.601 | 28.895 | 4.566 | 20.847 |
| Hospital | Non-Neighboring Hospital Bypass Distances (km) | Non-Neighboring Hospital Bypass Distances (Exceeding 3 km) | ||||||
|---|---|---|---|---|---|---|---|---|
| Mean | Max | STDEV | Var | Mean | Max | STDEV | Var | |
| BBY | 4.559 | 16.283 | 3.209 | 10.299 | 5.906 | 16.283 | 3.156 | 9.960 |
| DWZXY | 6.159 | 19.069 | 4.221 | 17.820 | 7.207 | 19.069 | 4.153 | 17.248 |
| GXQRM | 6.238 | 25.563 | 3.811 | 14.527 | 7.166 | 25.563 | 3.616 | 13.074 |
| H100 | 4.874 | 28.383 | 4.126 | 17.023 | 6.858 | 28.383 | 4.378 | 19.164 |
| JC | 5.010 | 50.559 | 3.849 | 14.815 | 6.217 | 50.559 | 4.013 | 16.100 |
| JL | 10.283 | 33.798 | 4.002 | 16.014 | 10.283 | 33.798 | 4.002 | 16.014 |
| KQ | 4.728 | 24.178 | 4.027 | 16.217 | 7.018 | 24.178 | 4.355 | 18.963 |
| LF | 6.400 | 17.844 | 3.171 | 10.058 | 6.727 | 17.844 | 3.085 | 9.519 |
| MDRM | 9.584 | 26.033 | 4.882 | 23.836 | 9.634 | 26.033 | 4.865 | 23.672 |
| SA | 6.715 | 16.640 | 3.466 | 12.015 | 7.427 | 16.640 | 3.192 | 10.189 |
| SDDE | 6.146 | 44.311 | 4.163 | 17.328 | 6.833 | 44.311 | 4.180 | 17.476 |
| SDDY | 5.973 | 44.032 | 4.752 | 22.582 | 7.212 | 44.032 | 4.835 | 23.378 |
| SDYK | 5.995 | 22.421 | 3.792 | 14.378 | 6.948 | 22.421 | 3.621 | 13.108 |
| SLBB | 5.806 | 40.982 | 4.482 | 20.088 | 7.062 | 40.982 | 4.510 | 20.342 |
| SLBQ | 5.002 | 36.366 | 3.824 | 14.621 | 6.679 | 36.366 | 3.865 | 14.937 |
| SLDQ | 5.408 | 32.329 | 4.135 | 17.098 | 6.972 | 32.329 | 4.235 | 17.932 |
| SZET | 6.956 | 41.034 | 5.401 | 29.170 | 8.211 | 41.034 | 5.361 | 28.745 |
| SZZY | 6.747 | 42.761 | 4.753 | 22.590 | 7.613 | 42.761 | 4.681 | 21.914 |
| TJ | 5.786 | 22.715 | 4.009 | 16.075 | 7.236 | 22.715 | 3.919 | 15.362 |
| WZRM | 5.566 | 23.091 | 3.730 | 13.916 | 6.747 | 23.091 | 3.675 | 13.507 |
| XCRM | 8.806 | 21.511 | 3.460 | 11.970 | 8.806 | 21.511 | 3.460 | 11.970 |
| XF | 4.168 | 25.537 | 3.677 | 13.524 | 6.659 | 25.537 | 4.394 | 19.308 |
References
- Zhang, Y.; Wang, X.; Qi, W.; Wang, J. Literature review on domestic difficulties of medical treatment. China Mod. Med. 2013, 20, 14–16. [Google Scholar]
- Bai, X.; Shi, P.; Liu, Y. Society: Realizing China’s urban dream. Nature 2014, 509, 158–160. [Google Scholar] [CrossRef] [PubMed]
- Meng, H. Study on the Current Situation, Problems and Countermeasures of Medical Function Dispersal in Beijing Central District; Capital University of Economics and Business: Beijing, China, 2014. [Google Scholar]
- Chen, J. Solution of the problems of “proper health care is difficult to get” by mobile medical service. Guangzhou Med. J. 2015, 46, 93–95. [Google Scholar]
- Li, D.; Ma, Y.; He, Q.; Yang, X.; Qi, Y. The effect of new medical reform policy on medical service accessibility. J. Bengbu Med. Coll. 2015, 40, 305–308. [Google Scholar]
- Liu, J.J.; Bellamy, G.; Barnet, B.; Weng, S. Bypass of local primary care in rural counties: Effect of patient and community characteristics. Ann. Fam. Med. 2008, 6, 124–130. [Google Scholar] [CrossRef] [PubMed]
- Sanders, S.R.; Erickson, L.D.; Call, V.R.; Mcknight, M.L. Middle-aged and older adult health care selection: Health care bypass behavior in rural communities in Montana. J. Appl. Gerontol. 2015. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Bellamy, G.R.; McCormick, M. Patient bypass behavior and critical access hospitals: Implications for patient retention. J. Rural Health 2007, 23, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Gauthier, B.; Wane, W. Bypassing health providers: The quest for better price and quality of health care in Chad. Soc. Sci. Med. 2011, 73, 540–549. [Google Scholar] [CrossRef] [PubMed]
- Sanders, S.R.; Erickson, L.D.; Call, V.R.; McKnight, M.L.; Hedges, D.W. Rural health care bypass behavior: How community and spatial characteristics affect primary health care selection. J. Rural Health 2014, 31, 146–156. [Google Scholar] [CrossRef] [PubMed]
- Roh, C.Y.; Lee, K.H.; Fottler, M.D. Determinants of hospital choice of rural hospital patients: The impact of networks, service scopes, and market competition. J. Med. Syst. 2008, 32, 343–353. [Google Scholar] [CrossRef] [PubMed]
- Karkee, R.; Lee, A.H.; Binns, C.W. Bypassing birth centres for childbirth: An analysis of data from a community-based prospective cohort study in Nepal. Health Policy Plan. 2015, 30, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Kruk, M.E.; Mbaruku, G.; Mccord, C.W.; Moran, M.; Rockers, P.C.; Galea, S. Bypassing primary care facilities for childbirth: A population-based study in rural Tanzania. Health Policy Plan. 2009, 24, 279–288. [Google Scholar] [CrossRef] [PubMed]
- Victoor, A.; Delnoij, D.M.; Friele, R.D.; Rademakers, J.J. Determinants of patient choice of healthcare providers: A scoping review. BMC Health Serv. Res. 2012, 12, 272. [Google Scholar] [CrossRef] [PubMed]
- Drph, R.L.G.; Falcone, D.J.; Broyles, R.W.; Goldsteen, K.; Reilly, B.J. Local factors affecting the tendency to bypass local hospitals for inpatient mental health care: An exploratory analysis. J. Rural Health 1994, 10, 89–97. [Google Scholar]
- He, X. Factors Affecting Rural Kentucky Patients Hospital Choice and Bypass Behavior. Master’s Thesis, University of Kentucky, Lexington, KY, USA, 2011. [Google Scholar]
- Varkevisser, M.; Geest, S.A.V.D. Why do patients bypass the nearest hospital? An empirical analysis for orthopaedic care and neurosurgery in the Netherlands. Eur. J. Health Econ. 2006, 8, 287–295. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.; Capra, L.; Wolfson, O.; Yang, H. Urban computing: Concepts, methodologies, and applications. ACM Trans. Intell. Syst. Technol. 2014, 5, 222–235. [Google Scholar] [CrossRef]
- Castro, P.S.; Zhang, D.; Chen, C.; Li, S.; Pan, G. From taxi GPS traces to social and community dynamics: A survey. ACM Comput. Surv. 2013, 46, 1167–1182. [Google Scholar] [CrossRef]
- Veloso, M.; Phithakkitnukoon, S.; Bento, C. Sensing urban mobility with taxi flow. In Proceedings of the 3rd ACM SIGSPATIAL International Workshop on Location-Based Social Networks, Chicago, IL, USA, 1–4 November 2011; pp. 41–44.
- Jiang, B.; Yin, J.; Chen, Z.; Zhao, S. Characterizing the human mobility pattern in a large street network. Phys. Rev. E 2009, 80, 1711–1715. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Li, S.; Pan, G. Mining the Semantics of Origin-Destination Flows Using Taxi Traces; UbiComp: Pittsburgh, PA, USA, 2012. [Google Scholar]
- Si, Y.; Weng, J.; Chen, Z.; Wang, Y. Taxi Travel Purpose Estimation and Characteristic Analysis Based on Multi-Source Data and Semantic Reasoning—A Case Study of Beijing; Springer: Berlin, Germany, 2014. [Google Scholar]
- Peng, C.; Jin, X.; Wong, K.C.; Shi, M.; Liò, P. Collective human mobility pattern from taxi trips in urban area. PLoS ONE 2012, 7, e34487. [Google Scholar] [CrossRef]
- Nyberg, G.; Caidahl, K.; Kharitonova, N.; Petersson, A. U 2 Sod-db: A Database System to Manage Large-Scale Ubiquitous Urban Sensing Origin-Destination Data; ACM SIGKDD International Workshop on Urban Computing: Beijing, China, 2012. [Google Scholar]
- Zhang, F.; Wilkie, D.; Zheng, Y.; Xie, X. Sensing the pulse of urban refueling behavior. Acm Trans. Intell. Syst. Technol. 2013, 6, 13–22. [Google Scholar]
- Yue, Y.; Wang, H.; Hu, B.; Li, Q.; Li, Y.; Yeh, A. Exploratory calibration of a spatial interaction model using taxi GPS trajectories. Comput. Environ. Urban Syst. 2012, 36, 140–153. [Google Scholar] [CrossRef]
- Ebeijing, the Official Website of the Beijing Government. Available online: http://www.ebeijing.gov.cn/ (accessed on 1 December 2015).
- Bejing Unified Platform for Appointment Registration. Available online: http://www.bjguahao.gov.cn/index.htm (accessed on 2 December 2015).
- Suzhou, China. Available online: http://www.suzhou.gov.cn/zgszeng/ (accessed on 5 December 2015).
- Suzhou Statistic Bureau. Suzhou Statistical Yearbook; China Statistics Press: Beijing, China, 2014.
- 12320 Suzhou Health Hotline. Available online: http://www.szws.net/index.asp (accessed on 5 December 2015).
- The Latest Road Network in Beijing. Available online: http://www.datatang.com/data/43855 (accessed on 15 August 2015).
- Cavusgil, S.T. Measuring the potential of emerging markets: An indexing approach. Bus. Horiz. 1997, 40, 87–91. [Google Scholar] [CrossRef]
- Cavusgil, S.T.; Kiyak, T.; Yeniyurt, S. Complementary approaches to preliminary foreign market opportunity assessment: Country clustering and country ranking. Ind. Mark. Manag. 2004, 33, 607–617. [Google Scholar] [CrossRef]
- Rossi, E.; Kuitunen, M. Ranking of habitats for the assessment of ecological impact in land use planning. Biol. Conserv. 1996, 77, 227–234. [Google Scholar] [CrossRef]
- Mohamadabadi, H.S.; Tichkowsky, G.; Kumar, A. Development of a multi-criteria assessment model for ranking of renewable and non-renewable transportation fuel vehicles. Energy 2009, 34, 112–125. [Google Scholar] [CrossRef]
- Tokunaga, M.; Sannomiya, K.; Watanabe, S.; Nakanishi, R.; Yamanaga, H.; Yonemitsu, H.; Terasaki, T.; Mita, S.; Kawano, S.; Hirata, Y. Relationship between hospital ranking based on functional independence measure (FIM) efficiency and factors related to rehabilitation system for stroke patients—A study of three hospitals participating in Kumamoto stroke liaison critical pathway. Jpn. J. Compr. Rehabil. Sci. 2012, 3, 51–58. [Google Scholar]
- Xu, X.; Li, B.; Sun, X.; Li, L.; Ren, R.; Gao, F.; Jonas, J.B. Eyelid neoplasms in the Beijing Tongren eye centre between 1997 and 2006. Ophthalmic Surg. Lasers Imaging Retina 2008, 39, 367–372. [Google Scholar] [CrossRef]
- Bejing 19 A-Class Designated Medical Organizations in 2011. Available online: http://www.gov.cn/gzdt/2011-10/29/content_1981168.htm (accessed on 1 February 2016).
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, G.; Song, C.; Shu, H.; Zhang, J.; Pei, T.; Zhou, C. Assessing Patient bypass Behavior Using Taxi Trip Origin–Destination (OD) Data. ISPRS Int. J. Geo-Inf. 2016, 5, 157. https://doi.org/10.3390/ijgi5090157
Yang G, Song C, Shu H, Zhang J, Pei T, Zhou C. Assessing Patient bypass Behavior Using Taxi Trip Origin–Destination (OD) Data. ISPRS International Journal of Geo-Information. 2016; 5(9):157. https://doi.org/10.3390/ijgi5090157
Chicago/Turabian StyleYang, Gege, Ci Song, Hua Shu, Jia Zhang, Tao Pei, and Chenghu Zhou. 2016. "Assessing Patient bypass Behavior Using Taxi Trip Origin–Destination (OD) Data" ISPRS International Journal of Geo-Information 5, no. 9: 157. https://doi.org/10.3390/ijgi5090157