Photothermal Radiometry for Skin Research
Abstract
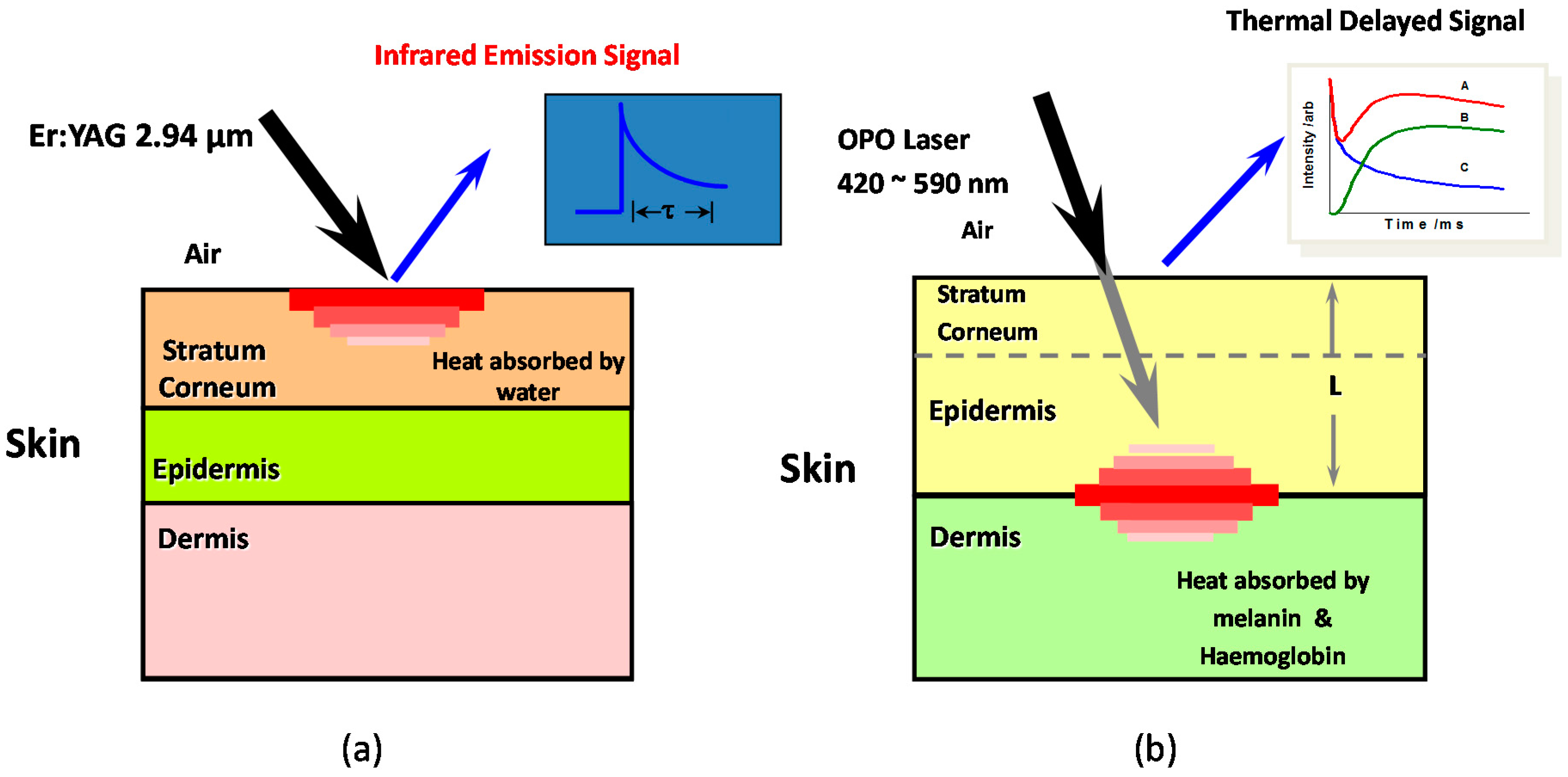
:1. Introduction
2. Theoretical Background
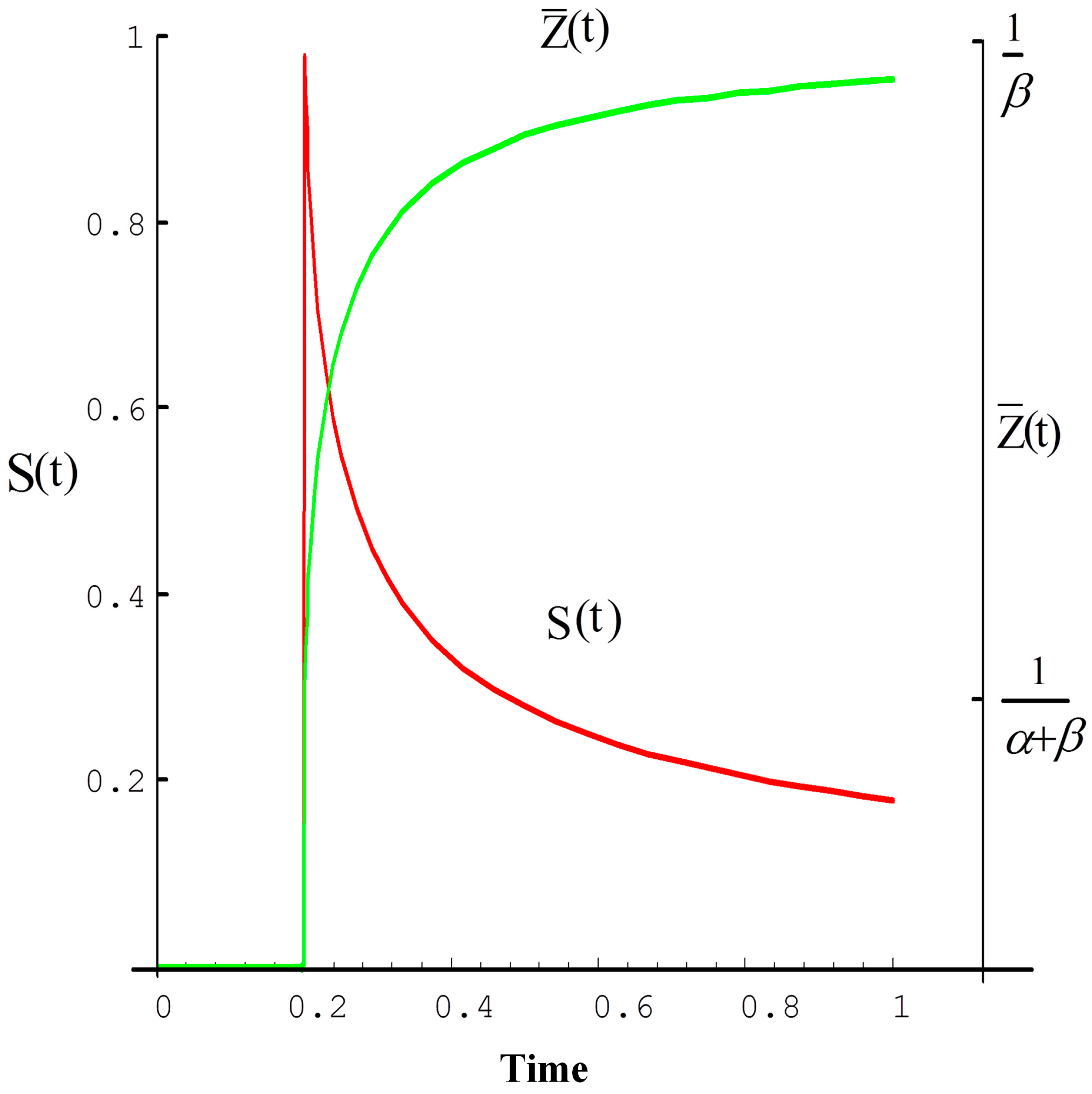
2.1. Homogeneous Model
2.2. Gradient Model
2.3. Non-Homogeneous Model
3. OTTER Applications
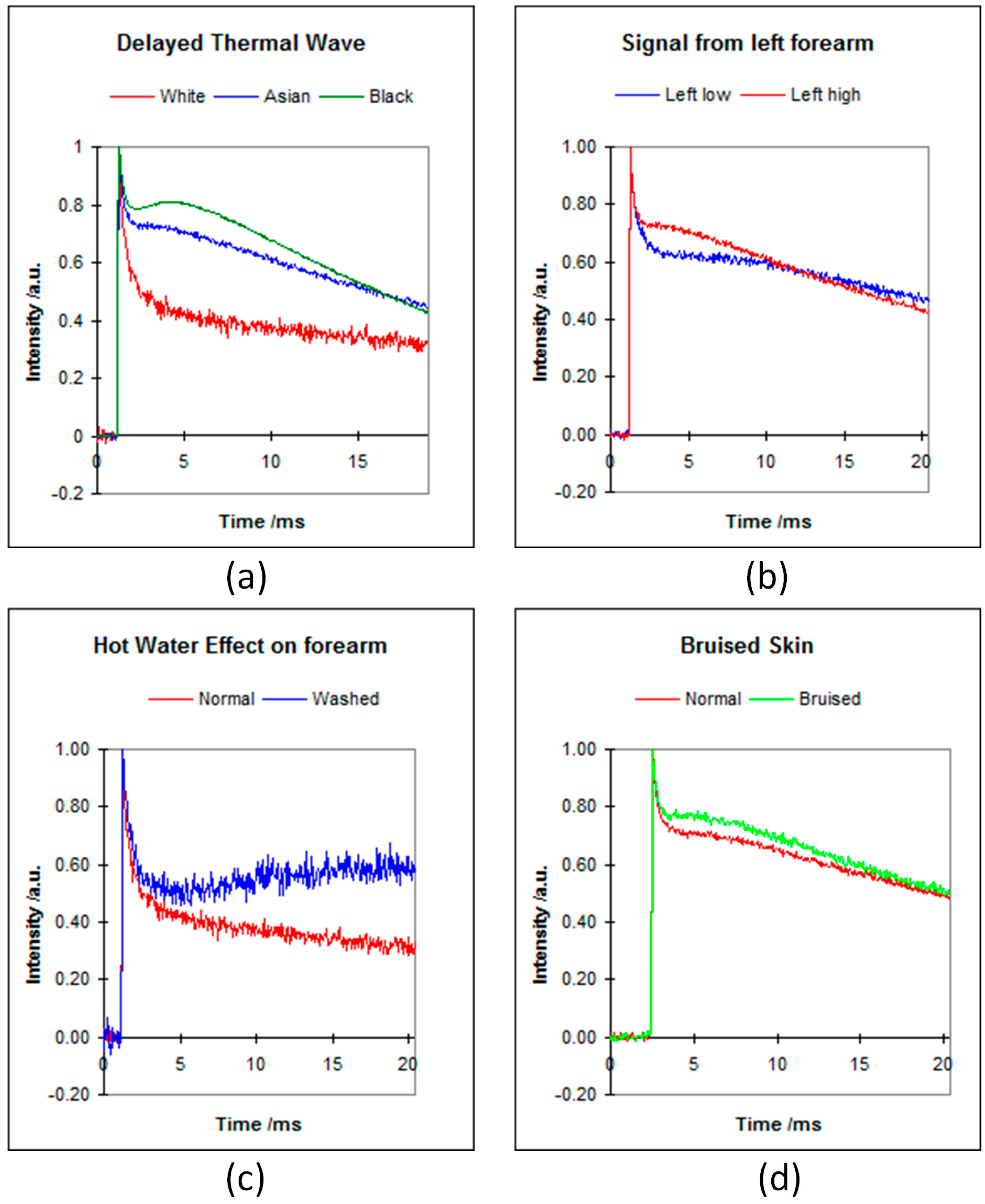
3.1. Skin Pigment Measurements
3.2. Skin Water Content Measurements
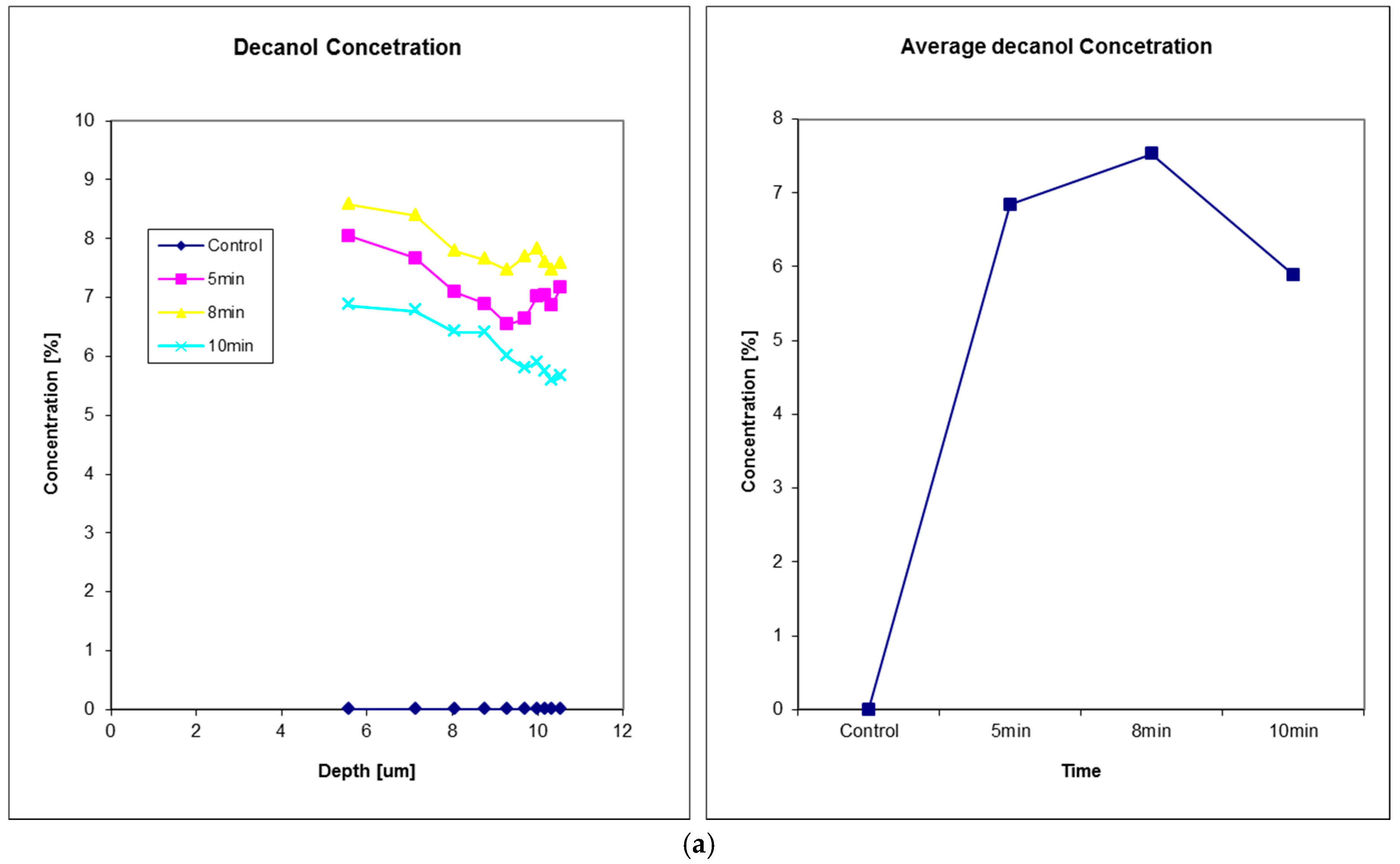
3.3. Solvent Penetration Measurements
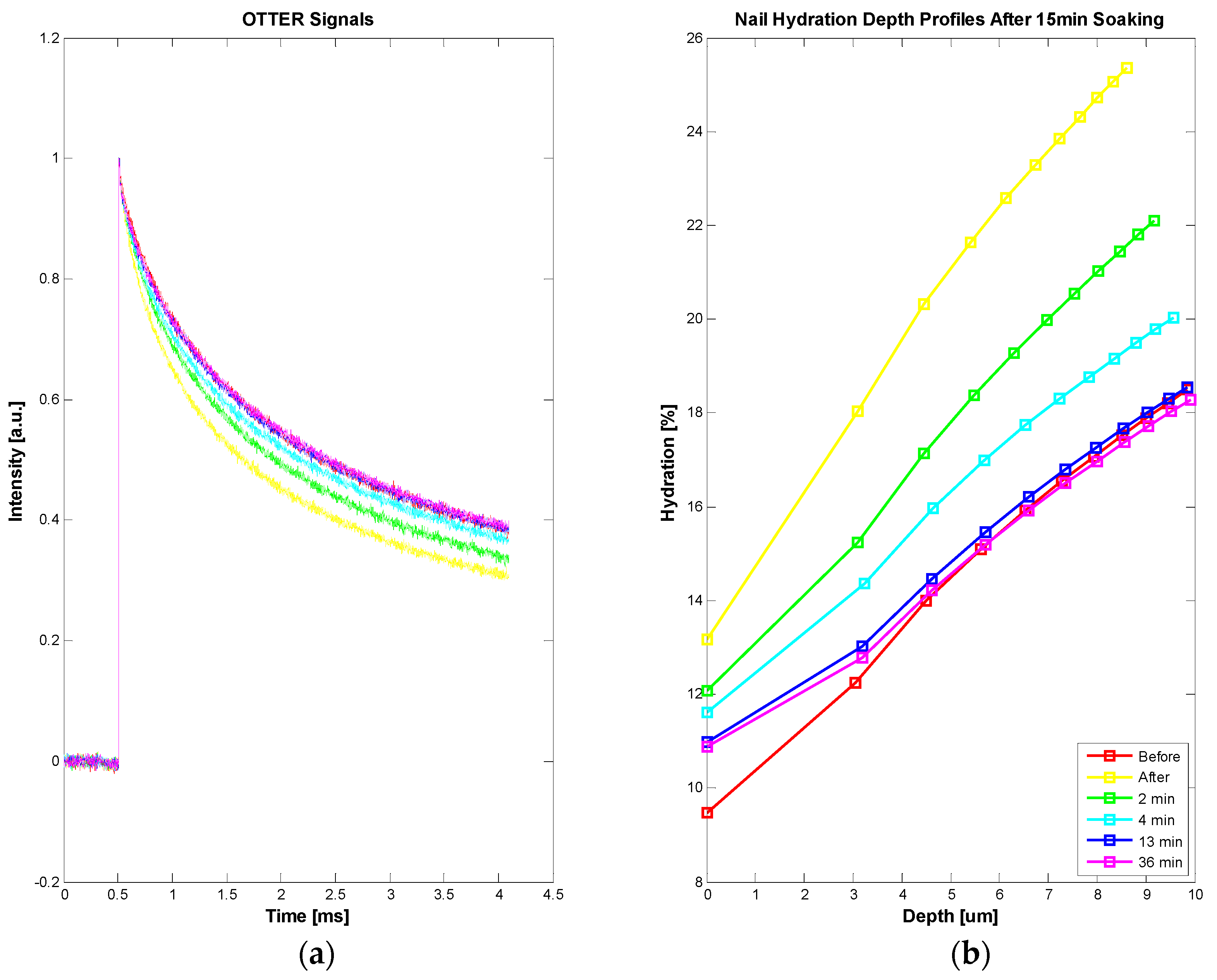
3.4. Nail Measurements
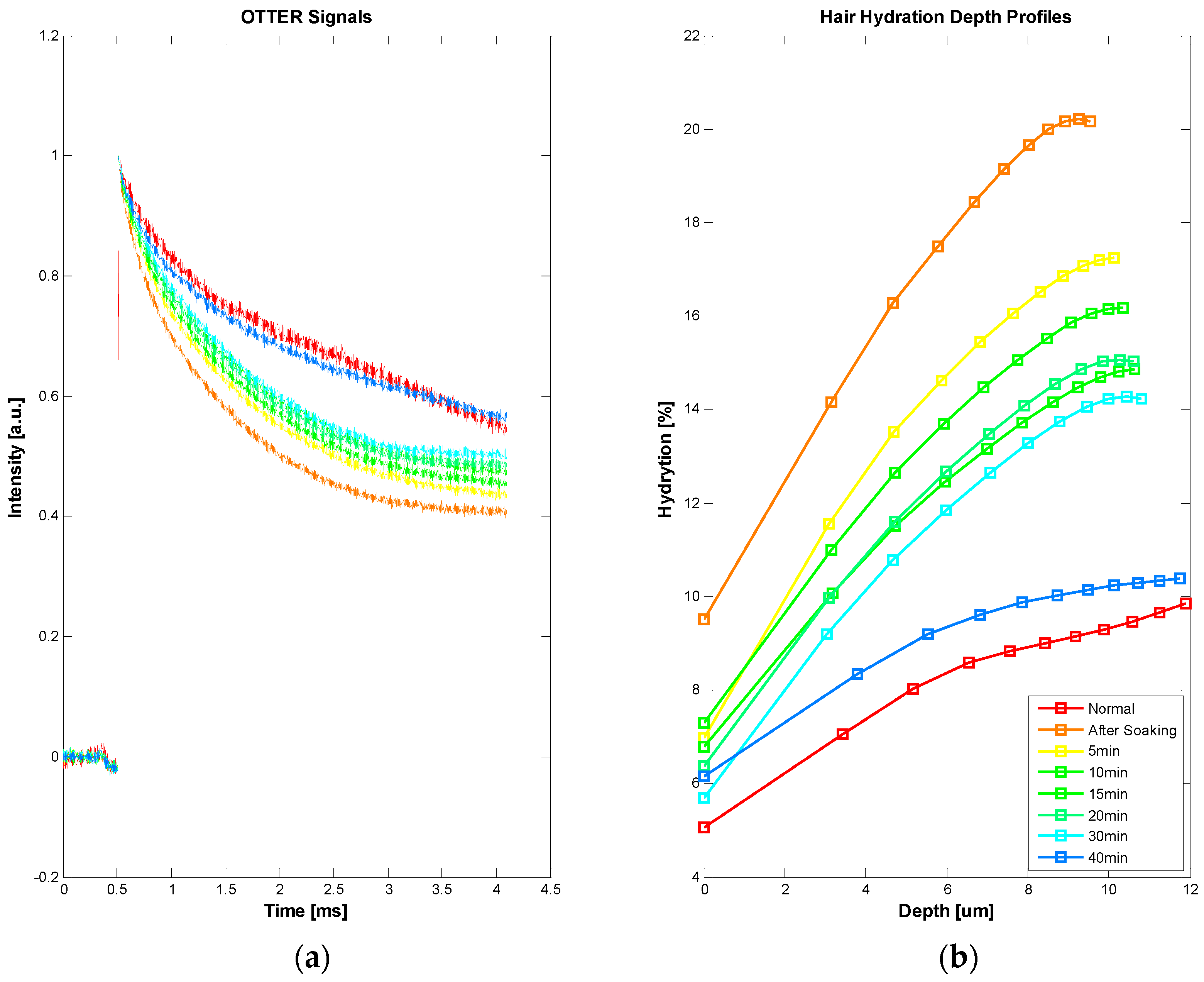
3.5. Hair Measurements
3.6. Future Developments
4. Conclusions and Future Works
Acknowledgments
Conflicts of Interest
References
- Tam, A.C.; Sullivan, B. Remote sensing applications of pulsed photothermal radiometry. Appl. Phys. Lett. 1983, 43, 333–335. [Google Scholar] [CrossRef]
- Imhof, R.E.; Birch, D.J.S.; Thornley, F.R.; Gilchrist, J.R.; Strivens, T.A. Opto-thermal transient emission radiometry. J. Phys. E Sci. Instrum. 1984, 17, 521–525. [Google Scholar] [CrossRef]
- Long, F.H.; Anderson, R.R.; Deutsch, T.F. Pulsed photothermal radiometry for depth profiling of layered media. Appl. Phys. Lett. 1987, 51, 2076–2078. [Google Scholar] [CrossRef]
- Jacques, S.L.; Nelson, J.S.; Wright, W.H.; Milner, T.E. Pulsed photothermal radiometry of port-wine-stain lesions. Appl. Opt. 1993, 32, 2439–2446. [Google Scholar] [CrossRef] [PubMed]
- Vitkin, I.A.; Wilson, B.C.; Anderson, R.R.; Prahl, S.A. Pulsed photothermal radiometry in optically transparent media containing discrete optical absorbers. Phys. Med. Biol. 1994, 39, 1721–1744. [Google Scholar] [CrossRef] [PubMed]
- Almond, D.P.; Patel, P.M. Photothermal Science and Techniques; ASIN: B017PNMQS8; Chapman and Hall: London, UK, 1996. [Google Scholar]
- Vavilov, V.P.; Burleigh, D.D. Review of pulsed thermal NDT: Physical principles, theory and data processing. NDT & E Int. 2015, 73, 28–52. [Google Scholar]
- Imhof, R.E.; Zhang, B.; Birch, D.J.S. Photothermal Radiometry for NDE. In Progress in Photothermal and Photoacoustic Science and Technology; Mandelis, A., Ed.; PTR Prentice Hall: Englewood Cliffs, NJ, USA, 1994; Volume II, pp. 185–236. [Google Scholar]
- Imhof, R.E.; McKendrick, A.D.; Xiao, P. Thermal emission decay Fourier transform infrared spectroscopy. Rev. Sci. Instrum. 1995, 66, 5203–5213. [Google Scholar] [CrossRef]
- Xiao, P. Opto-Thermal Mathematical Modeling and Data Analysis in Skin Measurements. Ph.D. Thesis, London South Bank University, London, UK, 1997. [Google Scholar]
- Xiao, P.; Imhof, R.E. Inverse Method Analysis in Opto-Thermal Skin Measurements. SPIE Proc. 1999, 3601, 340–347. [Google Scholar]
- Xiao, P.; Gull, S.F.; Imhof, R.E. Opto-Thermal Inverse Modelling Using a Maximum Entropy Approach. Anal. Sci. 2001, 17, s394–s397. [Google Scholar]
- Xiao, P.; Guo, X.; Notingher, I.; Cowen, J.A.; O’Driscoll, D.; Imhof, R.E. Optothermal Skin Pigment Spectral Depth Profiling using an OPO Laser. SPIE Proc. 1999, 3601, 348–354. [Google Scholar]
- Xiao, P.; Cowen, J.A.; Guo, X.; O’Driscoll, D.; Imhof, R.E. Photothermal In-vivo Characterization of Human Skin using Tuneable OPO laser Excitation. In Photoacoustic and Photothermal Phenomena: 10th International Conference, Rome, Italy, 23–27 August 1998; Scudieri, F., Bertolotti, M., Eds.; American Institute of Physics: College Park, MD, USA, 1999; pp. 621–623. [Google Scholar]
- Xiao, P.; Imhof, R.E. Opto-thermal measurement of water distribution within the stratum corneum. In Skin Bioengineering Techniques and Applications in Dermatology and Cosmetology; Karger: Basel, Switzerland, 1998; Volume 26, pp. 48–60. [Google Scholar]
- Xiao, P.; Cowen, J.A.; Imhof, R.E. In-Vivo Transdermal Drug Diffusion Depth Profiling—A New Approach to Opto-Thermal Signal Analysis. Anal. Sci. 2001, 17, s349–s352. [Google Scholar]
- Xiao, P.; Ou, X.; Ciortea, L.I.; Berg, E.P.; Imhof, R.E. In Vivo Skin Solvent Penetration Measurements Using Opto-thermal Radiometry and Fingerprint Sensor. Int. J. Thermophys. 2012, 33, 1787–1794. [Google Scholar] [CrossRef]
- Xiao, P.; Imhof, R.E. Data Analysis Technique for Pulsed Opto-Thermal Measurements. UK Patent Application 0004374.5, 25 February 2000. [Google Scholar]
- Xiao, P.; Imhof, R.E. Apparatus for in vivo Skin Characterization. UK Patent Application GB1014212.3, 26 August 2010. [Google Scholar]
- Scheuplein, R.J. A survey of some fundamental aspects of the absorption and reflection of light by tissue. J. Soc. Cosmet. Chem. 1964, 15, 111–122. [Google Scholar]
- Jacques, S.L. Laser Tissue Interactions. Las. Gener. Surg. 1992, 72, 531–557. [Google Scholar]
- Yoon, G.; Welch, A.J.; Motamedi, M.; van Gement, M.C.J. Development and application of Three-Dimentional Light Distribution Model for Laser Irradiated Tissue. IEEE J. Quan. Elec. 1987, 23, 1721–1733. [Google Scholar] [CrossRef]
- Cowen, J.A. In-vivo Opto-thermal Transdermal Diffusion Measurement. Ph.D. Thesis, London South Bank University, London, UK, 1999. [Google Scholar]
- Xiao, P.; Zheng, X.; Imhof, R.E.; Hirata, K.; McAuley, W.J.; Mateus, R.; Hadgraft, J.; Lane, M.E. Opto-Thermal Transient Emission Radiometry (OTTER) to image diffusion in nails in vivo. Int. J. Pharm. 2011, 406, 111–113. [Google Scholar] [CrossRef] [PubMed]
- Xiao, P.; Ciortea, L.I.; Singh, H.; Berg, E.P.; Imhof, R.E. Opto-thermal Radiometry for In-Vivo Nail Measurements. J. Phys. Conf. Ser. 2009, 214, 012008. [Google Scholar] [CrossRef]
- Notingher, I.; Imhof, R.E.; Xiao, P.; Pascut, F.C. Spectral Depth Profiling of Arbitrary Surfaces by Thermal Emission Decay-Fourier Transform Infrared Spectroscopy. Appl. Spectrosc. 2003, 57, 1494–1501. [Google Scholar] [CrossRef] [PubMed]
- Notingher, I.; Imhof, R.E.; Xiao, P.; Pascut, F.C. Near-surface depth-resolved midinfrared emission spectroscopy. Rev. Sci. Instrum. 2003, 74, 346–348. [Google Scholar] [CrossRef]
- Pascut, F.C. Fiber-Optic Optothermal Emission Radiometry for In-vivo Skin Measurements. Ph.D. Thesis, London South Bank University, London, UK, 2004. [Google Scholar]




© 2016 by the author; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons by Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xiao, P. Photothermal Radiometry for Skin Research. Cosmetics 2016, 3, 10. https://doi.org/10.3390/cosmetics3010010
Xiao P. Photothermal Radiometry for Skin Research. Cosmetics. 2016; 3(1):10. https://doi.org/10.3390/cosmetics3010010
Chicago/Turabian StyleXiao, Perry. 2016. "Photothermal Radiometry for Skin Research" Cosmetics 3, no. 1: 10. https://doi.org/10.3390/cosmetics3010010




