Association of Hypertension with All-Cause Mortality among Hospitalized Patients with COVID-19
Abstract
:1. Introduction
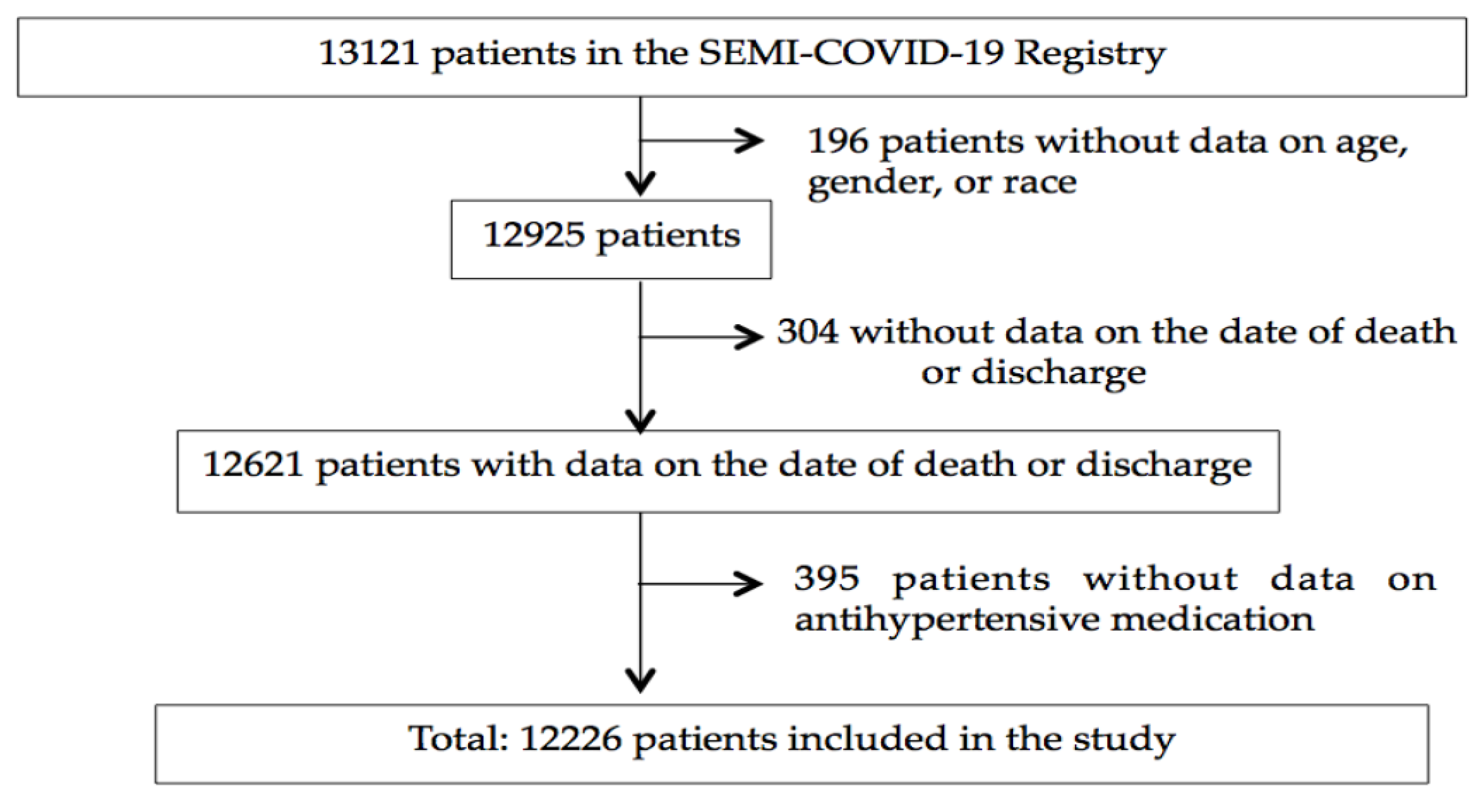
2. Subjects and Methods
3. Results
3.1. Demographic Characteristics of the Study Population
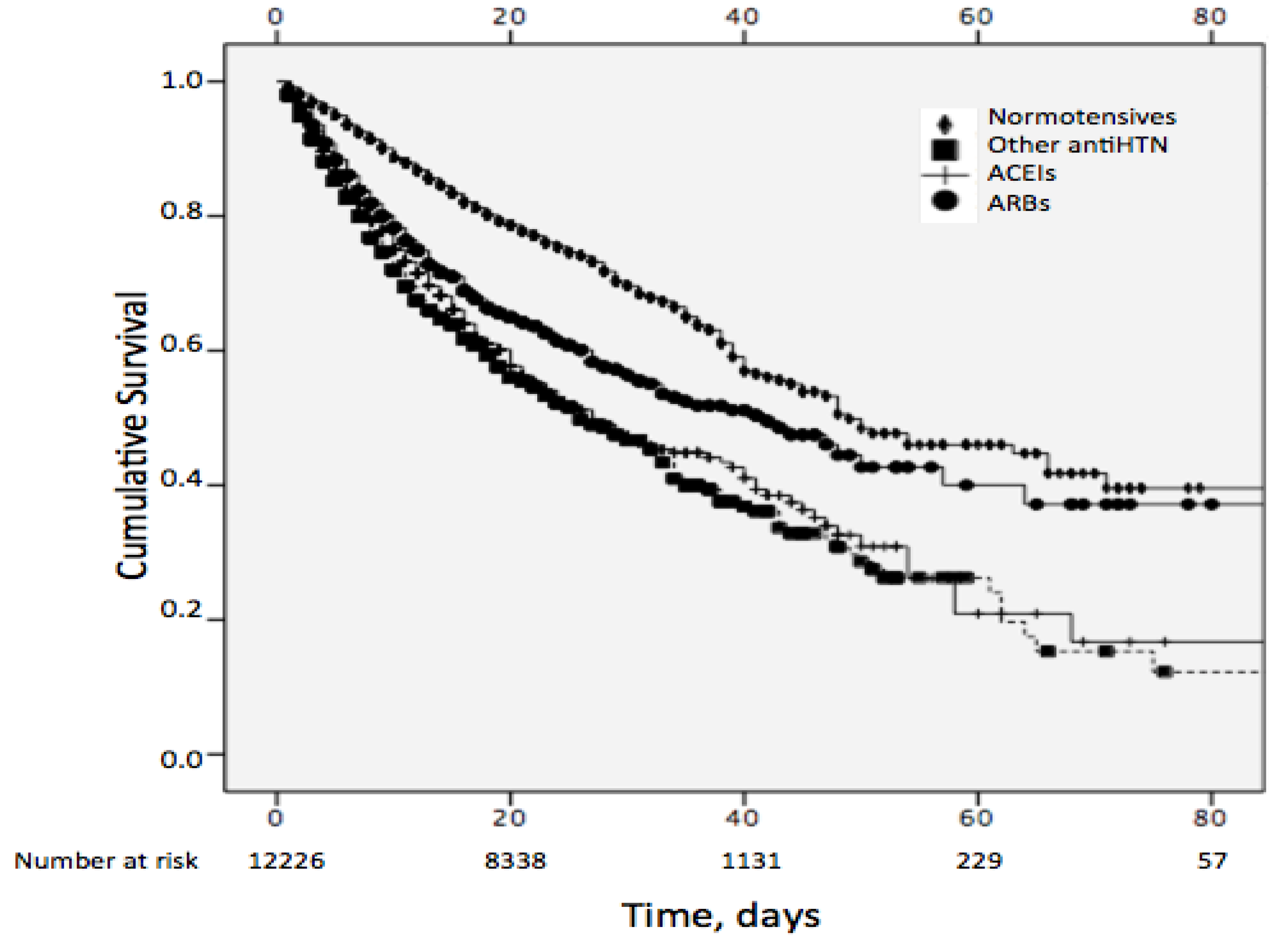
3.2. Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Johns Hopkins University Website. Available online: https://coronavirus.jhu.edu/map.html (accessed on 14 August 2020).
- Guan, W.J.; Ni, Z.Y.; Hu, Y.; Liang, C.; Ou, J.; He, L.; Liu, H.; Shan, C.; Lei, D.S.C.; Hui, B.; et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef] [PubMed]
- Grasselli, G.; Zangrillo, A.; Zanella, A.; Massimo, A.; Luca, C.; Antonio, C.; Danilo, C.; Antonio, C.; Giuseppe, F.; Roberto, F.; et al. Baseline Characteristics and Outcomes of 1591 Patients Infected With SARS-CoV-2 Admitted to ICUs of the Lombardy Region. JAMA 2020, 323, 1574–1581. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Global Atlas on Cardiovascular Disease Prevention and Control; World Health Organization: Geneva, Switzerland, 2011; ISBN 978-92-4-156437-3.
- Liang, W.; Liang, H.; Ou, L.; Chen, B.; Chen, A.; Li, C.; Li, Y.; Guan, W.; Sang, L.; Lu, J.; et al. Development and Validation of a Clinical Risk Score to Predict the Occurrence of Critical Illness in Hospitalized Patients With COVID-19. JAMA Int. Med. 2020, e202033. [Google Scholar] [CrossRef] [PubMed]
- Drummond, G.R.; Vinh, A.; Guzik, T.J.; Sobey, C.G. Immune mechanisms of hypertension. Nat. Rev. Immunol. 2019, 19, 517–532. [Google Scholar] [CrossRef]
- Zhang, Y.; Murugesan, P.; Huang, K.; Cai, H. NADPH oxidases and oxidase crosstalk in cardiovascular diseases: Novel therapeutic targets. Nat. Rev. Cardiol. 2020, 17, 170–194. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, M.; Kleine-Weber, H.; Schroeder, S.; Krüger, N.; Herrler, T.; Erichsen, S.; Schiergens, T.S.; Herrler, G.; Wu, N.-H.; Nitsche, A.; et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell 2020, 181, 271–280.e8. [Google Scholar] [CrossRef] [PubMed]
- Turner, A.J.; Hiscox, J.A.; Hooper, N.M. ACE2: From vasopeptidase to SARS virus receptor. Trends Pharmacol. Sci. 2004, 25, 291–294. [Google Scholar] [CrossRef]
- Williams, B.; Mancia, G.; Spiering, W.; Rosei, E.A.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; De Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef]
- Furuhashi, M.; Moniwa, N.; Mita, T.; Fuseya, T.; Ishimura, S.; Ohno, K.; Shibata, S.; Tanaka, M.; Watanabe, Y.; Akasaka, H.; et al. Urinary angiotensin-converting enzyme 2 in hypertensive patients may be increased by olmesartan, an angiotensin II receptor blocker. Am. J. Hypertens. 2015, 28, 15–21. [Google Scholar] [CrossRef] [Green Version]
- Santos, R.A.S.; Sampaio, W.O.; Alzamora, A.C.; Motta-Santos, D.; Alenina, N.; Bader, M.; Campagnole-Santos, M. The ACE2/angiotensin-(1-7)/MAS axis of the renin-angiotensin system: Focus on angiotensin-(1-7). Physiol. Rev. 2018, 98, 505–553. [Google Scholar] [CrossRef] [Green Version]
- Fang, L.; Karakiulakis, G.; Roth, M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir. Med. 2020, 8, e21. [Google Scholar] [CrossRef]
- Mancia, G.; Rea, F.; Ludergnani, M.; Apolone, G.; Corrao, G. Renin-Angiotensin-Aldosterone System Blockers and the Risk of Covid-19. N. Engl. J. Med. 2020, 382, 2431–2440. [Google Scholar] [CrossRef] [PubMed]
- Iaccarino, G.; Grassı, G.; Borghi, C.; Ferri, C.; Salvetti, M.; Volpe, M.; SARS-RAS Investigators; Cicero, A.F.; Minuz, P.; Muiesan, M.L.; et al. Age and Multimorbidity Predict Death Among COVID-19 Patients: Results of the SARS-RAS Study of the Italian Society of Hypertension. Hypertension 2020, 76, 366–372. [Google Scholar] [CrossRef] [PubMed]
- Chow, C.K.; Teo, K.K.; Rangarajan, S.; Islam, S.; Gupta, R.; Avezum, A.; Bahonar, A.; Chifamba, J.; Dagenais, G.; Diaz, R.; et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA 2013, 310, 959–968. [Google Scholar] [CrossRef] [Green Version]
- Lind, L.; Sundström, J.; Ärnlöv, J.; Lampa, E. Impact of aging on the strength of cardiovascular risk factors: A longitudinal study over 40 years. J. Am. Heart Assoc. 2018, 7, e007061. [Google Scholar] [CrossRef] [Green Version]
- Kuba, K.; Imai, Y.; Rao, S.; Gao, H.; Guo, F.; Guan, B.; Huan, Y.; Yang, P.; Zhang, Y.; Deng, W.; et al. A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus-induced lung injury. Nat. Med. 2005, 11, 875–879. [Google Scholar] [CrossRef]
- Saavedra, J.M. Angiotensin receptor blockers and COVID-19. Pharmacol. Res. 2020, 156, 104832. [Google Scholar] [CrossRef]
- American College of Cardiology. HFSA/ACC/AHA Statement Addresses Concerns re: Using RAAS Antagonists in COVID-19. 17 March 2020. Available online: https://www.acc.org/latestin-cardiology/articles/2020/03/17/08/59/hfsa-accahastatementaddresses-concernsreusingraasantagonists-incovid19 (accessed on 14 August 2020).
- European Society of Cardiology. Position Statement of theESC Council on Hypertension on ACE-Inhibitors and Angiotensin Receptor Blockers. 13 March 2020. Available online: https://www.escardio.org/Councils/Council-onHypertension-(CHT)/News/position-statement-of-the-esc-council-on-hypertension-on-ace-inhibitors-and-ang (accessed on 14 August 2020).
- Casas-Rojo, J.M.; Antón-Santos, J.M.; Millán-Núñez-Cortés, J.; Lumbreras-Bermejo, C.; Ramos-Rincón, J.M.; Roy-Vallejo, E.; Artero-Mora, A.; Arnalich-Fernández, F.; García-Bruñén, J.M.; Vargas-Núñez, J.A.; et al. Características clínicas de los pacientes hospitalizados con COVID-19 en España: Resultados del Registro SEMI-COVID-19. Rev. Clínica Española 2020. [Google Scholar] [CrossRef]
- WHO. Clinical Management of Severe Acute Respiratory Infection When Novel Coronavirus (NCOV) Infection Is Suspected: Interim Guidance. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance-publications (accessed on 10 July 2020).
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Análisis de los casos de COVID-19 notificados a la RENAVE hasta el 10 de mayo en España, Informe COVID-19 nº 33. 29 de mayo de 2020. Informe nº 33. Análisis de los casos de COVID-19 notificados a la RENAVE hasta el 10 de mayo en España a 29 de mayo de 2020. Equipo COVID-19. RENAVE. CNE. CNM (ISCIII). Available online: https://www.isciii.es/QueHacemos/Servicios/VigilanciaSaludPublicaRENAVE/EnfermedadesTransmisibles/Documents/INFORMES/Informes%20COVID-19/Informe%20n%C2%BA%2033.%20An%C3%A1lisis%20de%20los%20casos%20de%20COVID-19%20hasta%20el%2010%20de%20mayo%20en%20Espa%C3%B1a%20a%2029%20de%20mayo%20de%202020.pdf (accessed on 14 August 2020).
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wu- han, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Guan, W.-J.; Liang, W.-H.; Zhao, Y.; Liang, H.-R.; Chen, Z.-S.; Li, Y.-M.; Liu, X.-Q.; Chen, R.-C.; Tang, C.-L.; Wang, T.; et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: A nationwide analysis. Eur. Respir. J. 2020, 55, 2000547. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leiva Sisnieguez, C.E.; Espeche, W.G.; Salazar, M.R. Arterial hypertension and the risk of severity and mortality of COVID-19. Eur. Respir. J. 2020, 55, 2001148. [Google Scholar] [CrossRef]
- Fosbøl, E.L.; Butt, J.H.; Østergaard, L.; Andersson, C.; Selmer, C.; Kragholm, K.; Schou, M.; Phelps, M.; Gislason, G.H.; Gerds, T.A.; et al. Association of Angiotensin-Converting Enzyme Inhibitor or Angiotensin Receptor Blocker Use With COVID-19 Diagnosis and Mortality. JAMA 2020, 324, 168–177. [Google Scholar] [CrossRef] [PubMed]
- Mehta, P.; McAuley, D.F.; Brown, M.; Sanchez, E.; Tattersall, R.S.; Manson, J.J. HLH Across Speciality Collaboration, UK. COVID-19: Consider cytokine storm syndromes and immunosuppression. Lancet 2020, 395, 1033–1034. [Google Scholar] [CrossRef]
- Rao, C. Medical certification of cause of death for COVID 19. Bull. World Health Organ. 2020, 98, 298-A. [Google Scholar] [CrossRef]
| Variable | Total Study Population (n = 12226) | Non-Survivors (n = 2630) | Survivors (n = 9596) | p Value |
|---|---|---|---|---|
| Age, years | 67.5 ± 16.1 | 79.6 ± 10.5 | 64.1 ± 15.7 | 0.0001 |
| Women, % | 42.6 | 38.1 | 43.8 | 0.0001 |
| Hypertension, % | 50.9 | 70.6 | 45.5 | 0.0001 |
| Diabetes mellitus, % | 19.1 | 28.2 | 16.6 | 0.0001 |
| COPD, % | 7.0 | 12.5 | 5.5 | 0.0001 |
| CKD, % | 6.0 | 12.5 | 4.3 | 0.0001 |
| Coronary heart disease, % | 8.0 | 14.1 | 6.3 | 0.0001 |
| Heart failure, % | 7.1 | 15.4 | 4.9 | 0.0001 |
| Stroke, % | 7.7 | 14.2 | 6.0 | 0.0001 |
| Atrial fibrillation, % | 11.2 | 21.7 | 8.3 | 0.0001 |
| Peripheral vascular disease, % | 4.7 | 9.0 | 3.5 | 0.0001 |
| Charlson Comorbidity Index score | 3.6 ± 2.7 | 5.7 ± 2.4 | 3.1 ± 2.5 | 0.0001 |
| Variable | Normotensive Subjects (n = 6001) | Hypertensive Subjects | p Value | ||
|---|---|---|---|---|---|
| Non-ACEI/ARB (n = 1987) | ACEI (n = 1983) | ARB (n = 2255) | |||
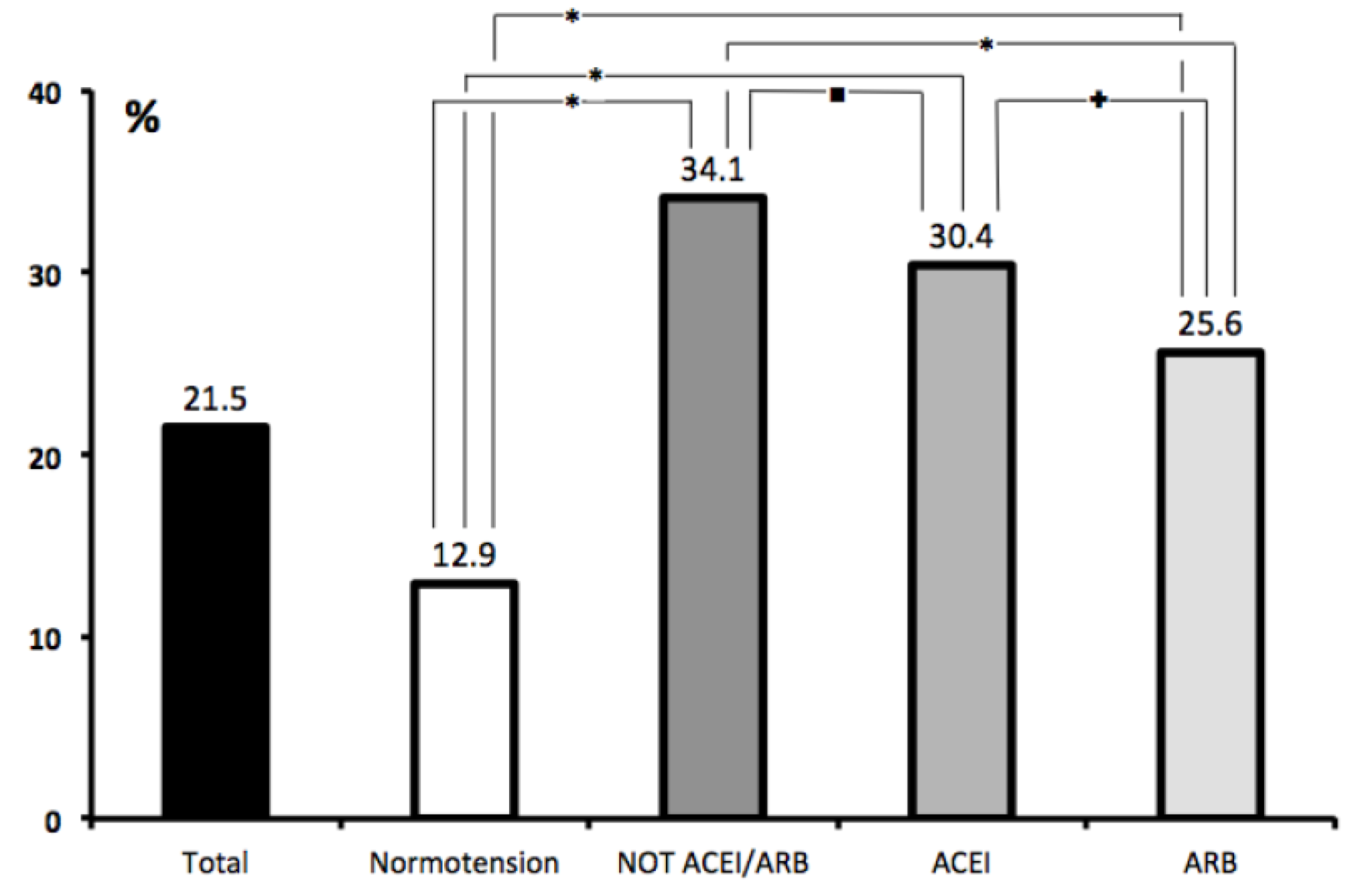
| Death, % | 12.9 | 34.1 | 30.4 | 25.6 | 0.0001 |
| Age, years | 60.1 ± 16.1 | 76.4 ± 12.7 | 73.5 ± 12.6 | 73.9 ± 11.8 | 0.0001 |
| Women, % | 41.8 | 48.5 | 39.1 | 42.4 | 0.0001 |
| Hypertension, % | 0 | 100 | 100 | 100 | 0.0001 |
| Diabetes mellitus, % | 9.3 | 25.5 | 29.3 | 30.4 | 0.0001 |
| COPD, % | 4.6 | 10.0 | 9.2 | 9.0 | 0.0001 |
| CKD, % | 1.8 | 12.5 | 7.3 | 10.5 | 0.0001 |
| Coronary heart disease, % | 3.1 | 13.0 | 12.9 | 12.1 | 0.0001 |
| Heart failure, % | 2.6 | 14.7 | 10.6 | 9.4 | 0.0001 |
| Stroke, % | 3.9 | 12.6 | 11.2 | 10.8 | 0.0001 |
| Atrial fibrillation, % | 4.9 | 21.4 | 15.1 | 15.3 | 0.0001 |
| Peripheral vascular disease, % | 2.2 | 7.1 | 6.5 | 7.5 | 0.0001 |
| Charlson Comorbidity Index score | 2.5 ± 2.3 | 5.1 ± 2.6 | 4.5 ± 2.5 | 4.6 ± 2.5 | 0.0001 |
| Variable. | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|
| OR (CI 95%) | p Value | OR (CI 95%) | p Value | |
| Age, tertiles | ||||
| <60.9 | 1 | 1 | ||
| ≥60.9 and <76.3 | 5.3 (4.38–6.30) | 0.0001 | 2.0 (1.56–2.43) | 0.0001 |
| ≥76.3 | 20.3 (17.08–24.16) | 0.0001 | 4.7 (3.75–5.92) | 0.0001 |
| Blood pressure | ||||
| Normotension | 1 | 1 | ||
| Non-ACEIs/ARBs | 3.5 (3.11–3.95) | 0.0001 | 1.3 (1.08–1.43) | 0.002 |
| ACEIs | 3.0 (2.61–3.34) | 0.0001 | 1.6 (1.35–1.85) | 0.001 |
| ARBs | 2.3 (2.07–2.64) | 0.0001 | 1.2 (1.01–1.38) | 0.035 |
| Charlson Comorbidity Index, tertiles | ||||
| <2 | 1 | 1 | ||
| ≥2 and <5 | 11.2 (9.34–13.45) | 0.0001 | 4.7 (3.73–5.86) | 0.0001 |
| ≥5 | 28.2 (23.47–33.97) | 0.0001 | 8.1 (6.37–10,36) | 0.0001 |
| Gender | ||||
| Female | 1 | 1 | ||
| Male | 1.3 (1.16–1.38) | 0.0001 | 1.5 (1.39–1.71) | 0.0001 |
| ACEIs (in-hospital) | ||||
| no | 1 | 1 | ||
| yes | 1.1 (0.93–1.24) | 0.357 | 0.6 (0.45–0.66) | 0.0001 |
| ARBs (in-hospital) | ||||
| no | 1 | 1 | ||
| yes | 0.86 (0.74–0.99) | 0.046 | 0.5 (0.45–0.65) | 0.0001 |
| HF | ||||
| no | 1 | 1 | ||
| yes | 3.6 (3.08–4.09) | 0.0001 | 1.2 (1.01–1.41) | 0.037 |
| Atrial fibrillation | ||||
| no | 1 | 1 | ||
| yes | 1.3 (1.16–1.38) | 0.0001 | 1.2 (1.01–1.33) | 0.034 |
| CKD | ||||
| no | 1 | 1 | ||
| yes | 3.2 (2.75–3.73) | 0.0001 | 1.2 (0.99–1.41) | 0.068 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodilla, E.; Saura, A.; Jiménez, I.; Mendizábal, A.; Pineda-Cantero, A.; Lorenzo-Hernández, E.; Fidalgo-Montero, M.d.P.; López-Cuervo, J.F.; Gil-Sánchez, R.; Rabadán-Pejenaute, E.; et al. Association of Hypertension with All-Cause Mortality among Hospitalized Patients with COVID-19. J. Clin. Med. 2020, 9, 3136. https://doi.org/10.3390/jcm9103136
Rodilla E, Saura A, Jiménez I, Mendizábal A, Pineda-Cantero A, Lorenzo-Hernández E, Fidalgo-Montero MdP, López-Cuervo JF, Gil-Sánchez R, Rabadán-Pejenaute E, et al. Association of Hypertension with All-Cause Mortality among Hospitalized Patients with COVID-19. Journal of Clinical Medicine. 2020; 9(10):3136. https://doi.org/10.3390/jcm9103136
Chicago/Turabian StyleRodilla, Enrique, Alberto Saura, Iratxe Jiménez, Andrea Mendizábal, Araceli Pineda-Cantero, Elizabeth Lorenzo-Hernández, Maria del Pilar Fidalgo-Montero, Joaquín Fernandez López-Cuervo, Ricardo Gil-Sánchez, Elisa Rabadán-Pejenaute, and et al. 2020. "Association of Hypertension with All-Cause Mortality among Hospitalized Patients with COVID-19" Journal of Clinical Medicine 9, no. 10: 3136. https://doi.org/10.3390/jcm9103136






