Thoracic, Lumbar, and Sacral Pedicle Screw Placement Using Stryker-Ziehm Virtual Screw Technology and Navigated Stryker Cordless Driver 3: Technical Note
Abstract
:1. Introduction
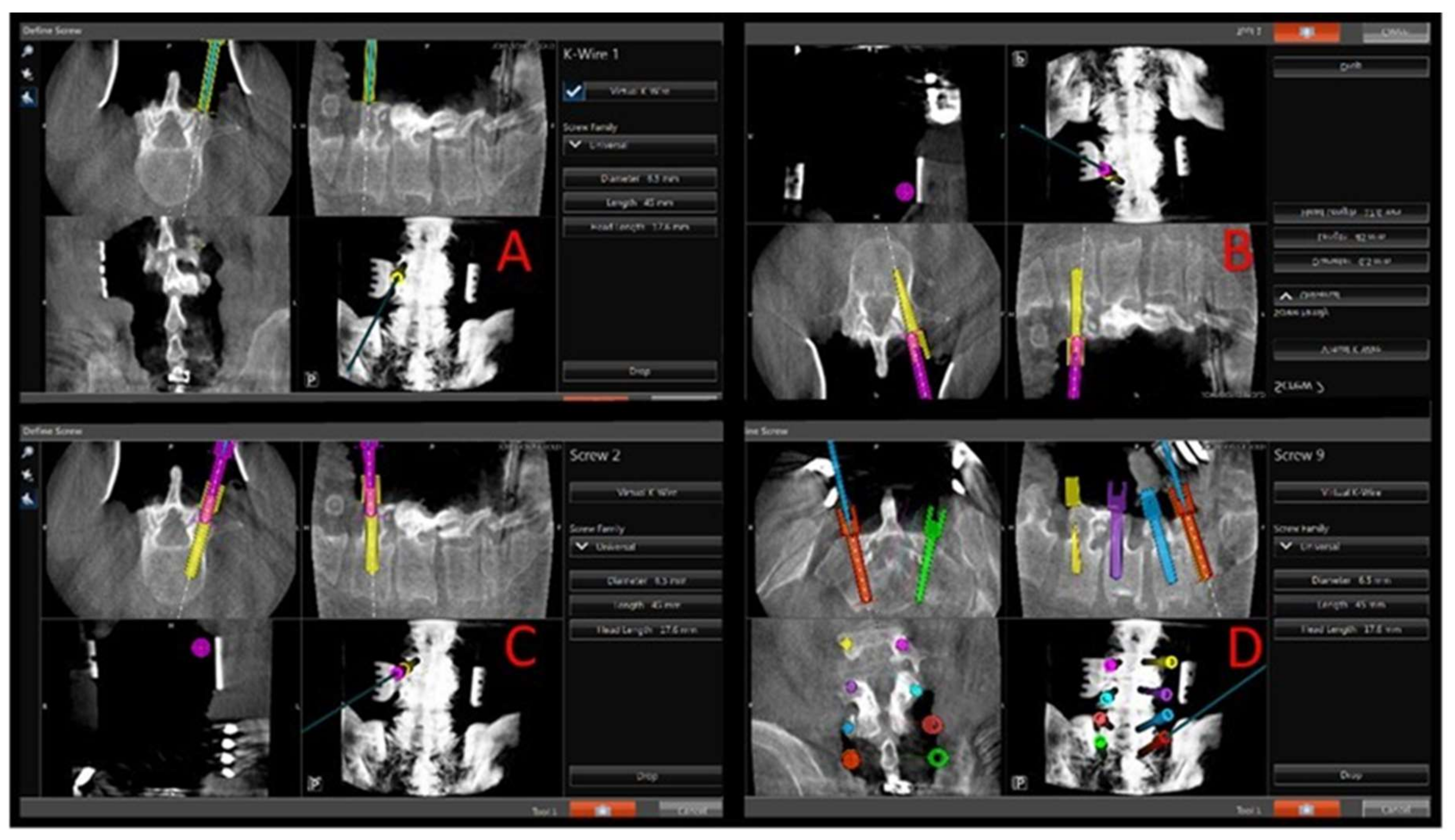
2. Methods
3. Results
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Kim, J.-S.; Härtl, R.; Mayer, H.M. Minimally invasive spinal surgery. In BioMed Research International; Hindawi Publishing Corporation: Cairo, Egypt, 2016; Available online: https://www.hindawi.com/journals/bmri/2016/5048659/ (accessed on 15 January 2018).
- Quillo-Olvera, J.; Lin, G.-X.; Suen, T.-K.; Jo, H.-J.; Kim, J.-S. Anterior transcorporeal tunnel approach for cervical myelopathy guided by CT-based intraoperative spinal navigation: Technical note. J. Clin. Neurosci. 2018, 48, 218–223. [Google Scholar] [CrossRef]
- Kim, Y.J.; Lenke, L.G.; Bridwell, K.H.; Cho, Y.S.; Riew, K.D. Free hand pedicle screw placement in the thoracic spine: Is it safe? Spine 2004, 29, 333–342. [Google Scholar] [CrossRef] [PubMed]
- Tjardes, T.; Shafizadeh, S.; Rixen, D.; Paffrath, T.; Bouillon, B.; Steinhausen, E.S. Image-guided spine surgery: State of the art and future directions. Eur. Spine J. 2010, 19, 25–45. [Google Scholar] [CrossRef]
- Gelalis, I.D.; Paschos, N.K.; Pakos, E.E.; Politis, A.N.; Arnaoutoglou, C.M.; Karageorgos, A.C. Accuracy of pedicle screw placement: A systematic review of prospective in vivo studies comparing free hand, fluoroscopy guidance and navigation techniques. Eur. Spine J. 2012, 21, 247–255. [Google Scholar] [CrossRef] [PubMed]
- Gonzalvo, A.; Fitt, G.; Liew, S. The learning curve of pedicle screw placement: How many screws are enough? Spine 2009, 34, 761–765. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Zhao, J.; Xie, Y.; Mi, J. The utility of a digital virtual template for junior surgeons in pedicle screw placement in the lumbar spine. BioMed Res. Int. 2016, 2016, 3076025. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.H.; Lin, M.H.; Weng, H.H.; Cheng, W.C.; Tsai, Y.H.; Wang, T.C.; Yang, J.T. Feasibility of intra-operative computed tomography navigation system for pedicle screw insertion of the thoraco-lumbar spine. J. Spinal Disord. Tech. 2013, 26, E183–E187. [Google Scholar] [CrossRef] [PubMed]
- Puvanesarajah, V.; Liauw, J.A.; Lo, S.-F.; Lina, I.A.; Witham, T.F. Techniques and accuracy of thoracolumbar pedicle screw placement. World J. Orthop. 2014, 5, 112–123. [Google Scholar] [CrossRef] [PubMed]
- Boucher, H.H. A method of spinal fusion. J. Bone Joint Surg. Br. 1959, 41, 248–259. [Google Scholar] [CrossRef]
- Kabins, M.B.; Weinstein, J.N. The history of vertebral screw and pedicle screw fixation. Iowa Orthop. J. 1991, 11, 127–136. [Google Scholar]
- Gaines, R.W. The use of pedicle-screw internal fixation for the operative treatment of spinal disorders. J. Bone Joint Surg. Am. 2000, 82, 1458–1476. [Google Scholar] [CrossRef]
- Hartl, R.; Theodore, N.; Dickman, C.A.; Sonntag, V.K.H. Technique of thoracic pedicle screw fixation for trauma. Oper. Tech. Neurosurg. 2004, 7, 22–30. [Google Scholar] [CrossRef]
- Suk, S.I.; Kim, W.J.; Lee, S.M.; Kim, J.H.; Chung, E.R. Thoracic pedicle screw fixation in spinal deformities: Are they really safe? Spine 2001, 26, 2049–2057. [Google Scholar] [CrossRef] [PubMed]
- Youkilis, A.S.; Quint, D.J.; McGillicuddy, J.E.; Papadopoulos, S.M. Stereotactic navigation for placement of pedicle screws in the thoracic spine. Neurosurgery 2001, 48, 771–778. [Google Scholar] [PubMed]
- Avila, M.J.; Baaj, A.A. Freehand thoracic pedicle screw placement: Review of existing strategies and a step-by-step guide using uniform landmarks for all levels. Cureus 2016, 8, E501. [Google Scholar] [CrossRef] [PubMed]
- Gertzbein, S.D.; Robbins, S.E. Accuracy of pedicular screw placement in vivo. Spine 1990, 15, 11–14. [Google Scholar] [CrossRef] [PubMed]
- Karapinar, L.; Erel, N.; Ozturk, H.; Altay, T.; Kaya, A. Pedicle screw placement with a free hand technique in thoracolumbar spine: Is it safe? J. Spinal Disord. Tech. 2008, 21, 63–67. [Google Scholar] [CrossRef] [PubMed]
- Modi, H.; Suh, S.W.; Song, H.-R.; Yang, J.-H. Accuracy of thoracic pedicle screw placement in scoliosis using the ideal pedicle entry point during the freehand technique. Int. Orthop. 2009, 33, 469–475. [Google Scholar] [CrossRef] [PubMed]
- Parker, S.L.; McGirt, M.J.; Farber, S.H.; Amin, A.G.; Rick, A.-M.; Suk, I. Accuracy of free-hand pedicle screws in the thoracic and lumbar spine: Analysis of 6816 consecutive screws. Neurosurgery 2011, 68, 170–178. [Google Scholar] [CrossRef] [PubMed]
- Schizas, C.; Theumann, N.; Kosmopoulos, V. Inserting pedicle screws in the upper thoracic spine without the use of fluoroscopy or image guidance. Is it safe? Eur. Spine J. 2007, 16, 625–629. [Google Scholar] [CrossRef] [PubMed]
- Dinesh, S.K.; Tiruchelvarayan, R.; Ng, I.A. prospective study on the use of intraoperative computed tomography (iCT) for image-guided placement of thoracic pedicle screws. Br. J. Neurosurg. 2012, 26, 838–844. [Google Scholar] [CrossRef] [PubMed]
- Idler, C.; Rolfe, K.W.; Gorek, J.E. Accuracy of percutaneous lumbar pedicle screw placement using the oblique or “owl’s-eye” view and novel guidance technology. J. Neurosurg. Spine 2010, 13, 509–515. [Google Scholar] [CrossRef] [PubMed]
- Ling, J.M.; Dinesh, S.K.; Pang, B.C.; Chen, M.W.; Lim, H.L.; Louange, D.T. Routine spinal navigation for thoraco-lumbar pedicle screw insertion using the O-arm three-dimensional imaging system improves placement accuracy. J. Clin. Neurosci. 2014, 21, 493–498. [Google Scholar] [CrossRef] [PubMed]
- Nottmeier, E.W.; Seemer, W.; Young, P.M. Placement of thoracolumbar pedicle screws using three-dimensional image guidance: Experience in a large patient cohort. J. Neurosurg. Spine 2008, 10, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Oertel, M.F.; Hobart, J.; Stein, M.; Schreiber, V.; Scharbrodt, W. Clinical and methodological precision of spinal navigation assisted by 3D intraoperative O-arm radiographic imaging. J. Neurosurg. Spine 2011, 14, 532–536. [Google Scholar] [CrossRef] [PubMed]
- Scheufler, K.-M.; Franke, J.; Eckardt, A.; Dohmen, H. Accuracy of image-guided pedicle screw placement using intraoperative computed tomography-based navigation with automated referencing. Part II: Thoracolumbar spine. Neurosurgery 2011, 69, 1307–1316. [Google Scholar] [CrossRef] [PubMed]

| Number of Patients | 23 |
| Patient age range | 19–65 |
| Pathology treated | |
| Degenerative | 15 |
| Trauma | 7 |
| Neoplasm | 1 |
| Number of screws placed with virtual technique | |
| Thoracic | 38 |
| Lumbar | 90 |
| Sacral | 16 |
| Number of screws needing revision after Instrumentation, Intraoperative CT | 1 (0.69%) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Satarasinghe, P.; Hamilton, K.D.; Tarver, M.J.; Buchanan, R.J.; Koltz, M.T. Thoracic, Lumbar, and Sacral Pedicle Screw Placement Using Stryker-Ziehm Virtual Screw Technology and Navigated Stryker Cordless Driver 3: Technical Note. J. Clin. Med. 2018, 7, 84. https://doi.org/10.3390/jcm7040084
Satarasinghe P, Hamilton KD, Tarver MJ, Buchanan RJ, Koltz MT. Thoracic, Lumbar, and Sacral Pedicle Screw Placement Using Stryker-Ziehm Virtual Screw Technology and Navigated Stryker Cordless Driver 3: Technical Note. Journal of Clinical Medicine. 2018; 7(4):84. https://doi.org/10.3390/jcm7040084
Chicago/Turabian StyleSatarasinghe, Praveen, Kojo D. Hamilton, Michael J. Tarver, Robert J. Buchanan, and Michael T. Koltz. 2018. "Thoracic, Lumbar, and Sacral Pedicle Screw Placement Using Stryker-Ziehm Virtual Screw Technology and Navigated Stryker Cordless Driver 3: Technical Note" Journal of Clinical Medicine 7, no. 4: 84. https://doi.org/10.3390/jcm7040084





