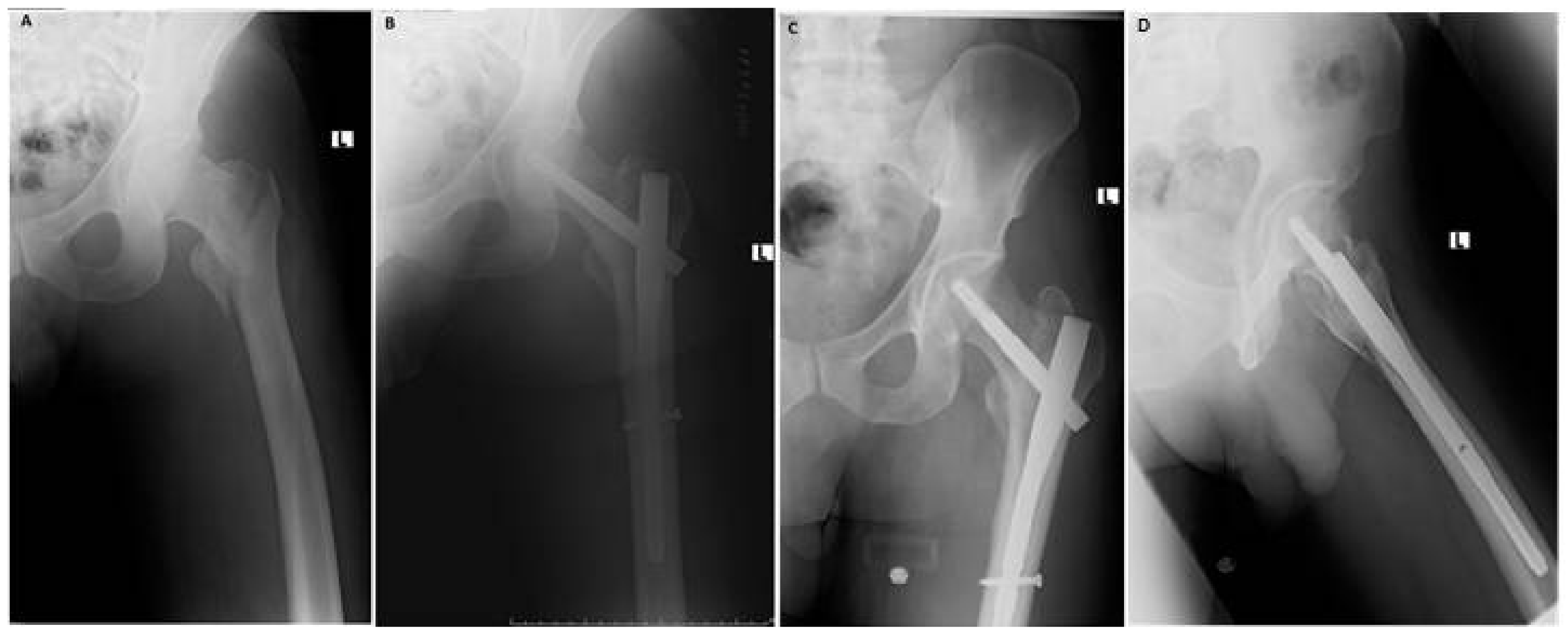
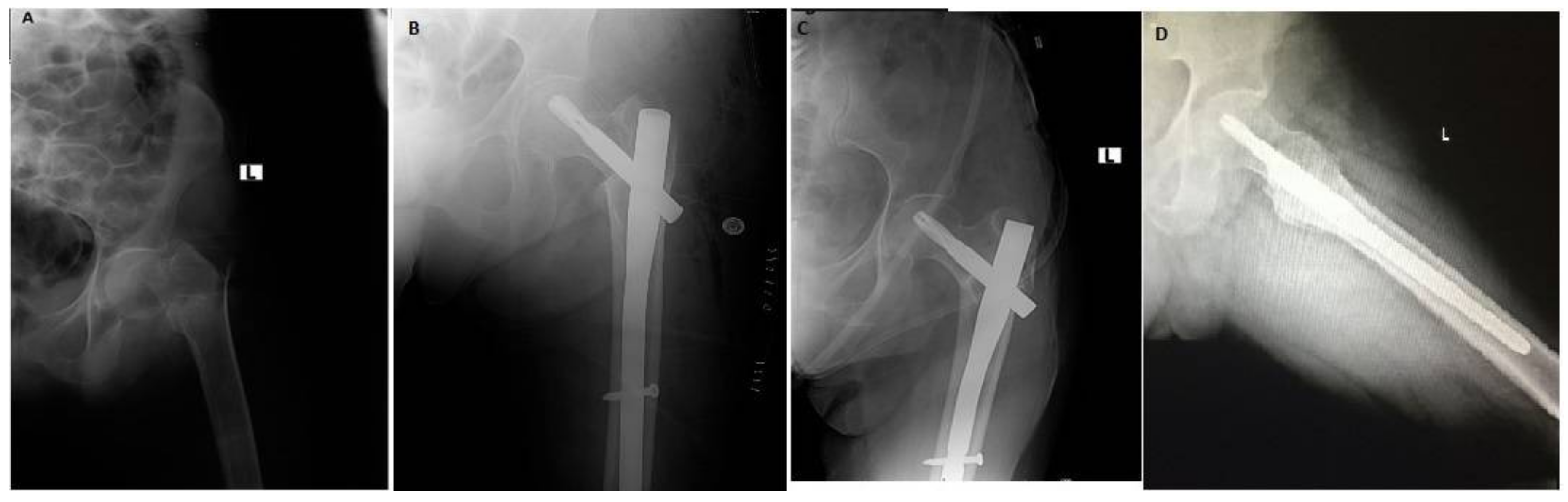
Functional and Radiological Results of Proximal Femoral Nail Antirotation (PFNA) Osteosynthesis in the Treatment of Unstable Pertrochanteric Fractures
Abstract
:1. Introduction
2. Experimental Section
3. Results
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Xu, Y.Z.; Geng, D.C.; Mao, H.Q.; Zhu, X.S.; Yang, H.L. A comparison of the proximal femoral nail antirotation device and dynamic hip screw in the treatment of unstable pertrochanteric fracture. J. Int. Med. Res. 2010, 38, 1266–1275. [Google Scholar] [CrossRef] [PubMed]
- Handoll, H.H.; Parker, M.J. Conservative versus operative treatment for hip fractures in adult. Cochrane Database Syst. Rev. 2008, 16, CD000337. [Google Scholar] [CrossRef] [PubMed]
- Pu, J.S.; Liu, L.; Wang, G.L.; Fang, Y.; Yang, T.F. Results of the proximal femoral nail anti-rotation (PFNA) in elderly Chinese patients. Int. Orthop. 2009, 33, 1441–1444. [Google Scholar] [CrossRef] [PubMed]
- Jones, H.W.; Johnston, P.; Parker, M. Are short femoral nails superior to the sltiding hip screw? A meta-analysis of 24 studies involving 3279 fractures. Int. Orthop. 2006, 30, 69–78. [Google Scholar] [CrossRef] [PubMed]
- Zeng, C.; Wang, Y.R.; Wei, J.; Gao, S.G.; Zhang, F.J.; Sun, Z.Q.; Lei, G.H. Treatment of trochanteric fractures with proximal femoral nail antirotation or dynamic hip screw systems: A meta-analysis. J. Int. Med. Res. 2012, 40, 839–851. [Google Scholar] [CrossRef] [PubMed]
- Barquet, A.; Francescoli, L.; Rienzi, D.; Lopez, L. Intertrochanteric-subtrochanteric fractures: Treatment with the long Gamma nail. J. Orthop. Trauma 2000, 14, 324–328. [Google Scholar] [CrossRef] [PubMed]
- Haidukewych, G.; Israel, A.; Berry, D. Reverse obliquity fractures of the intertrochanteric region of the femur. J. Bone Jt. Surg. Am. 2001, 38, 643–650. [Google Scholar] [CrossRef]
- Carulli, C.; Piacentini, F.; Paoli, T.; Civinini, R.; Innocenti, M. A comparison of two fixation methods for femoral trochanteric fractures: A new generation intramedullary system vs. sliding hip screw. Clin. Cases Miner. Bone Metab. 2017, 14, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Curtis, M.J.; Jinnah, R.H.; Wilson, V.; Cunningham, B.W. Proximal femoral fractures: A biomechanical study to compare intramedullary and extramedullary fixation. Injury 1994, 25, 99–104. [Google Scholar] [CrossRef]
- AO/ASIF. PFNA Leading the Way to Optimal Stability: Synthes; Original Instruments and Implants of the Association for the Study of Internal Fixation; STRATEC Medical: Oberdorf, Switzerland, 2004; pp. 1–44. [Google Scholar]
- Mereddy, P.; Kamath, S.; Ramakrishnan, M.; Malik, H.; Donnachie, N. The AO/ASIF proximal femoral nail antirotation (PFNA): A new design for the treatment of unstable proximal femoral fractures. Injury 2009, 40, 428–432. [Google Scholar] [CrossRef] [PubMed]
- Harris, W.H. Traumatic arthritis of the hip after dislocation and acetabular fractures: Treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J. Bone Jt. Surg. Am. 1969, 51, 737–755. [Google Scholar] [CrossRef]
- Zhang, H.; Zhu, X.; Pei, G.; Zeng, X.; Zhang, N.; Xu, P.; Chen, D.; Yu, W.; Zhang, X. A retrospective analysis of the InerTan nail and proximal femoral nail anti-rotationin in the treatment of intertrochanteric fractures in elderly patients with osteoporosis: A minimum follow-up of 3 years. J. Orthop. Surg. Res. 2017, 12, 147. [Google Scholar] [CrossRef] [PubMed]
- Sommers, M.B.; Roth, C.; Hall, H.; Kam, B.C.; Ehmake, L.W.; Krieq, J.C.; Madey, S.M.; Bottlang, M. A laboratory model to evaluate cut out resistance of implants for pertrochanteric fracture fixation. J. Orthop. Trauma 2004, 18, 361–368. [Google Scholar] [CrossRef] [PubMed]
- Hwang, J.H.; Oh, J.K.; Oh, C.W.; Lee, S.J.; Myung-Rae, C.; Kim, H.; Kim, M.K. A biomechanical evaluation of proximal femoral nail antirotation with respect to helical blade position in femoral head: A cadaveric study. Indian J. Orthop. 2012, 46, 627–632. [Google Scholar] [PubMed]
- Banan, H.; Al-Sabti, A.; Jimulia, T.; Hart, A.J. The treatment of unstable, extracapsular hip fractures with the AO/ASIF proximal femoral nail (PFN)—Our first 60 cases. Injury 2002, 33, 401–405. [Google Scholar] [CrossRef]
- Simmermacher, R.K.; Bosch, A.M.; Van der Werken, C. The AO/ASIF-proximal femoral nail (PFN): A new device for the treatment of unstable proximal femoral fractures. Injury 1999, 30, 327–332. [Google Scholar] [CrossRef]
- Takigami, I.; Matsumoto, K.; Ohara, A.; Yamanaka, K.; Naqanawa, T.; Ohashi, M.; Date, K.; Shimizu, K. Treatment of trochanteric fractures with the PFNA (proximal femoral nail antirotation) Nail system–report of early results. Bull. NYU Hosp. Jt. Dis. 2008, 66, 276–279. [Google Scholar] [PubMed]
- Al-yassari, G.; Langstaff, R.J.; Jones, J.W.M.; Al-Lami, M. The AO/ASIF proximal femoral nail (PFN) for the treatment of unstable trochanteric femoral fracture. Injury 2002, 33, 395–399. [Google Scholar] [CrossRef]
- Herrera, A.; Domingo, L.J.; Calvo, A.; Martinez, A. A comparative study of trochanteric fractures treated with Gamma nail or the proximal femoral nail. Int. Orthop. 2002, 26, 365–369. [Google Scholar] [PubMed]
- Albareda, J.; Laderiga, A.; Palanca, D.; Paniaqua, L.; Seral, F. Complications and technical problems with gamma nail. Int. Orthop. 1996, 20, 4750. [Google Scholar] [CrossRef]
- Aguado-Maestro, I.; Escudero-Marcos, R.; Garcia-Garcia, J.M.; Alonso-Garcia, N.; Perez-Bermejo, D.D.; Aguado-Hernandez, H.J.; Nistal-Rodriquez, J.; Garcia-Alonso, M. Results and complications of pertrochanteric hip fractures using an intramedullary nail with a helical blade (proximal femoral nail antirotation) in 200 patients. Rev. Esp. Cir. Ortop. Traumatol. 2013, 57, 201–207. [Google Scholar] [CrossRef] [PubMed]
- Şahin, E.K.; İmerci, A.; Kınık, H.; Karapınar, L.; Canbek, U.; Savran, A. Comparison of proximal femoral nail antirotation (PFNA) with AO dynamic condylar screws (DCS) for the treatment for unstable peritrochanteric femoral fracture. Eur. J. Orthop. Surg. Traumatol. 2014, 24, 347–352. [Google Scholar] [CrossRef] [PubMed]
- Karapınar, L.; Kumbaracı, M.; Kaya, A.; Imerci, A.; Incesu, M. Proximal femoral nail anti-rotation (PFNA) to treat peritrochanterics in elderly patients. Eur. J. Orthop. Surg. Traumatol. 2011, 5, 1–7. [Google Scholar] [CrossRef]
- Simmermacher, R.K.; Ljungqvist, J.; Bail, H.; Hochertz, T.; Vochteloo, A.J.; Werken, C.; On Behalf of the AO—PFNA Studygroup. The new proximal femoral nail antirotation (PFNA) in daily practice: Results of a multicentre clinical study. Injury 2008, 39, 932–939. [Google Scholar] [CrossRef] [PubMed]
- Yu, W.; Zhang, X.; Zhu, X.; Hu, J.; Liu, Y. A retrospective analysis of the InterTan nail and proximal femoral nail anti-rotation-Asia in the treatment of unstable intertrochanteric femur fractures in the elderly. J. Orthop. Surg. Res. 2016, 11, 10. [Google Scholar] [CrossRef] [PubMed]
- Macheras, G.A.; Galanakos, S.P.; Koutsostathis, S.; Kateros, K.; Karras, A.; Papadakis, S.A. Unstable pertrochanteric Fractures. A comparison of preliminary results using three different methods of fixation. EEXOT 2013, 64, 25–33. [Google Scholar]
| Variable | Value |
|---|---|
| Patients No. | 50 |
| Age: mean (range) | 72.8 (20–94) |
| Gender: male/female | 28/22 |
| Type of fracture | |
| A2 | 37 |
| A3 | 13 |
| Mechanism of injury | |
| Simple fall at home | 46 |
| Traffic Accident | 4 |
| Mean blood loss (mL) ± SD | 80 ± 54.92 |
| Mean operative time (min) ± SD | 73.60 ± 31.28 |
| Mean hospital Stay (days) ± SD | 6.86 ± 3.39 |
| Number | Mean Harris Hip Score ± SD | Mean Neck-Shaft Angle ± SD | |
|---|---|---|---|
| Fracture type | |||
| 31A2 | 37 | 77.92 ± 9.27 | 127.59 ± 5.14 |
| 31A3 | 13 | 83.38 ± 7.48 p-value 0.27 | 126.08 ± 4.91 p-value 0.88 |
| Fixation device | |||
| Long PFN | 9 | 84.33 ± 8.96 | 126.22 ± 5.85 |
| Short PFN | 41 | 78.24 ± 8.86 p-value 0.94 | 127.41 ± 4.94 p-value 0.56 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Radaideh, A.M.; Qudah, H.A.; Audat, Z.A.; Jahmani, R.A.; Yousef, I.R.; Saleh, A.A.A. Functional and Radiological Results of Proximal Femoral Nail Antirotation (PFNA) Osteosynthesis in the Treatment of Unstable Pertrochanteric Fractures. J. Clin. Med. 2018, 7, 78. https://doi.org/10.3390/jcm7040078
Radaideh AM, Qudah HA, Audat ZA, Jahmani RA, Yousef IR, Saleh AAA. Functional and Radiological Results of Proximal Femoral Nail Antirotation (PFNA) Osteosynthesis in the Treatment of Unstable Pertrochanteric Fractures. Journal of Clinical Medicine. 2018; 7(4):78. https://doi.org/10.3390/jcm7040078
Chicago/Turabian StyleRadaideh, Ahmad M., Hashem A. Qudah, Ziad A. Audat, Rami A. Jahmani, Ibraheem R. Yousef, and Abed Allah A. Saleh. 2018. "Functional and Radiological Results of Proximal Femoral Nail Antirotation (PFNA) Osteosynthesis in the Treatment of Unstable Pertrochanteric Fractures" Journal of Clinical Medicine 7, no. 4: 78. https://doi.org/10.3390/jcm7040078





