Deep Brain Stimulation of the Basolateral Amygdala: Targeting Technique and Electrodiagnostic Findings
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subject
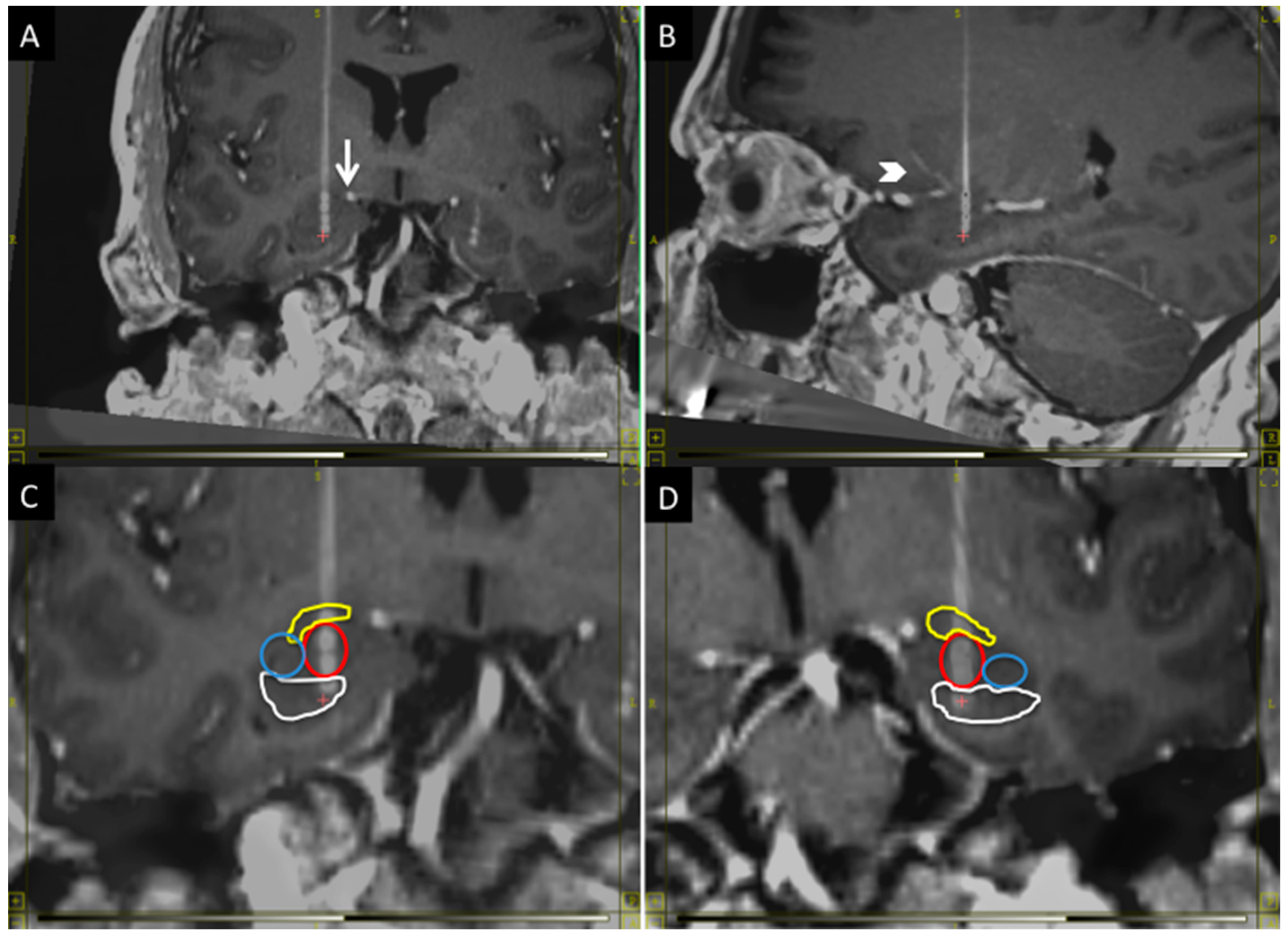
2.2. Targeting
2.3. Anesthesia and Microelectrode Recording
2.4. EEG Recording
2.5. Sleep and Nightmares Recording
3. Results
3.1. Microelectrode and DBS Lead Positions
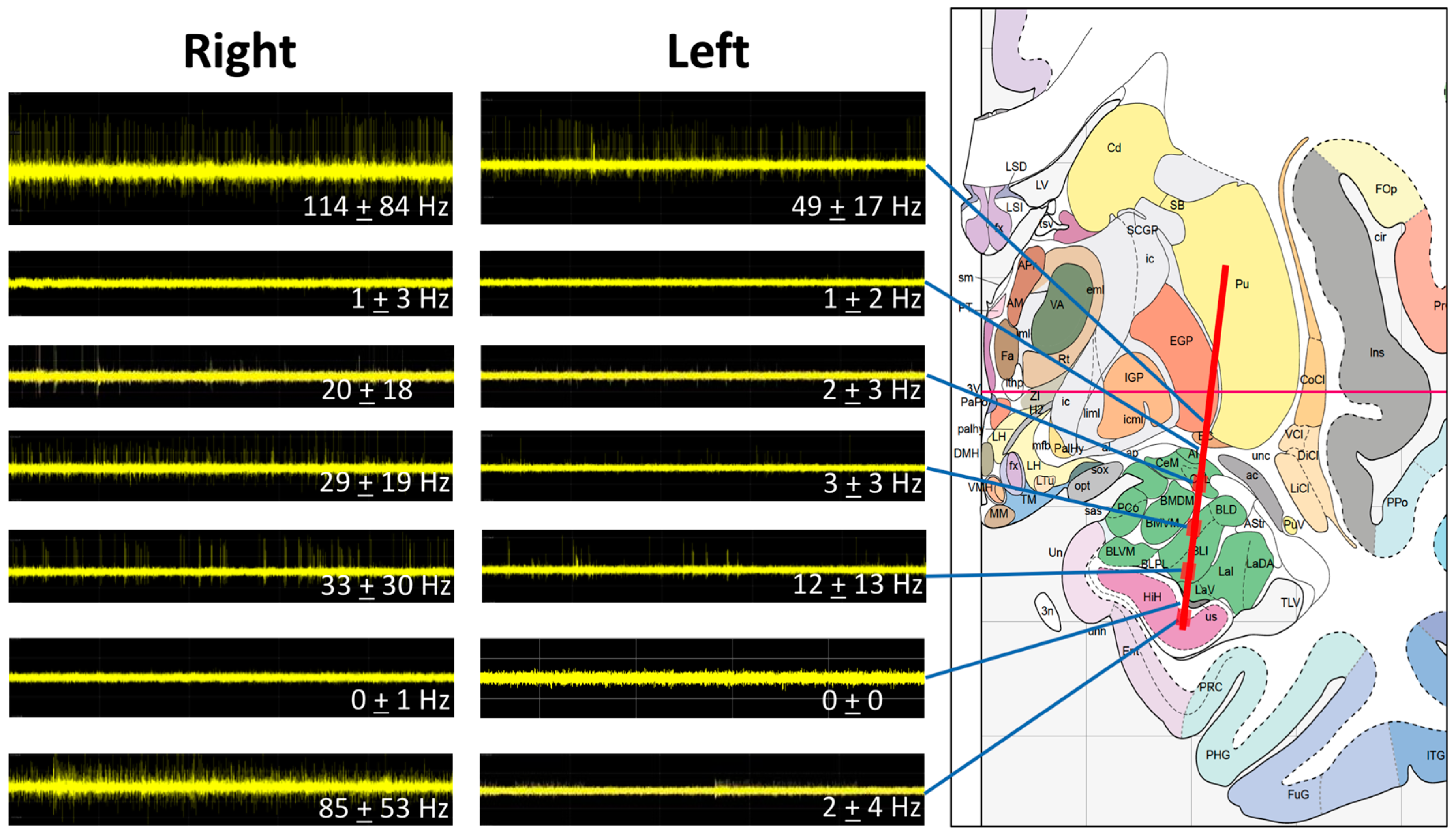
3.2. Microelectrode Recording
3.3. Intraoperative Neurostimulation
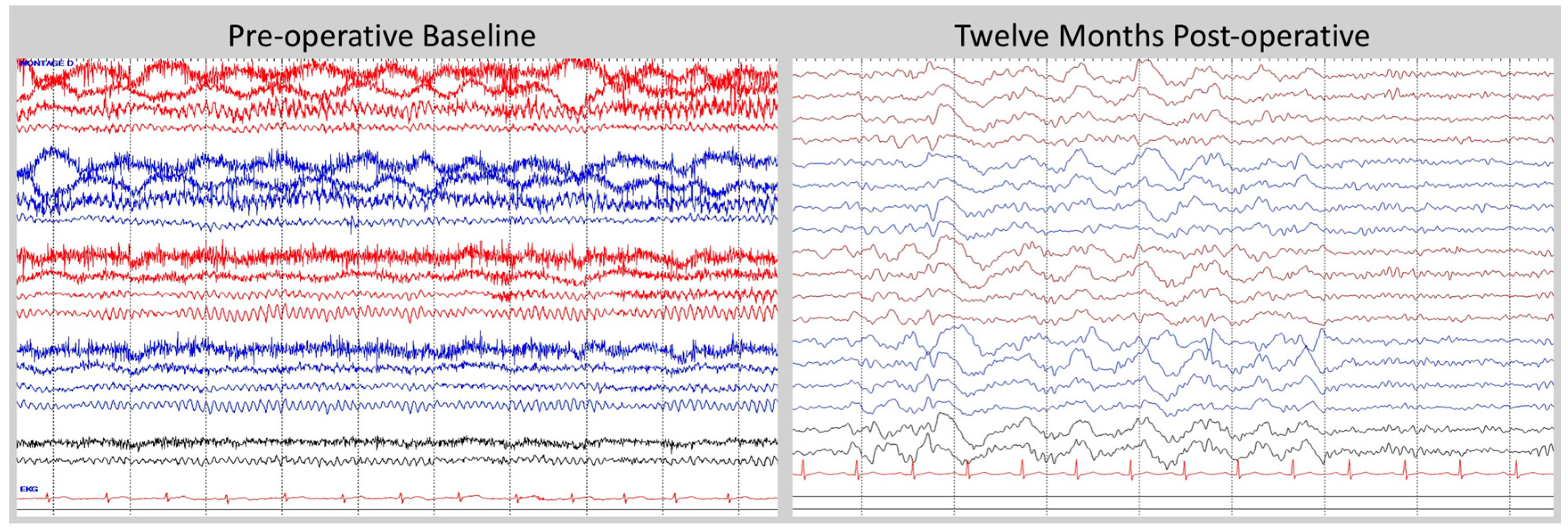
3.4. Post-Operative Electroencephalogram
4. Discussion
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Freese, J.L.; Amaral, D.G. Neuroanatomy of the primate amygdala. In The Human Amygdala; Whalen, P., Phelps, E.A., Eds.; The Guilford Press: New York, NY, USA, 2009; pp. 3–42. [Google Scholar]
- Marek, R.; Strobel, C.; Bredy, T.W.; Sah, P. The amygdala and medial prefrontal cortex: Partners in the fear circuit. J. Physiol. 2013, 591, 2381–2391. [Google Scholar] [CrossRef] [PubMed]
- Murray, E.A.; Izquierdo, A.; Malkova, L. Amygdala function in positive reinforcement. In The Human Amygdala; Whalen, P., Phelps, E.A., Eds.; The Guilford Press: New York, NY, USA, 2009; pp. 82–104. [Google Scholar]
- Luthi, A.; Luscher, C. Pathological circuit function underlying addiction and anxiety disorders. Nat. Neurosci. 2014, 17, 1635–1643. [Google Scholar] [CrossRef] [PubMed]
- Sotres-Bayon, F.; Sierra-Mercado, D.; Pardilla-Delgado, E.; Quirk, G. Gating of fear in prelimbic cortex by hippocampal and amygdala inputs. Neuron 2012, 76, 804–812. [Google Scholar] [CrossRef] [PubMed]
- Mpakopoulou, M.; Gatos, H.; Brotis, A.; Paterakis, K.; Fountas, K. Stereotactic amygdalotomy in the management of severe aggressive behavioral disorders. Neurosurg. Focus 2008, 25. [Google Scholar] [CrossRef] [PubMed]
- Koek, R.J.; Schwartz, H.N.; Scully, S.; Langevin, J.P.; Spangler, S.; Korotinsky, A.; Jou, K.; Leuchter, A. Treatment-refractory posttraumatic stress disorder (TRPTSD): A review and framework for the future. Prog. Neuropsychopharmacol. Biol. Psychiatry 2016, 70, 170–218. [Google Scholar] [CrossRef] [PubMed]
- Langevin, J.P.; De Salles, A.A.F.; Kosoyan, H.; Krahl, S. Deep brain stimulation alleviates posttraumatic stress disorder in a rat model. J. Psychiatr Res. 2010, 44, 1241–1245. [Google Scholar] [CrossRef] [PubMed]
- Stidd, D.A.; Vogelsang, K.; Krahl, S.E.; Langevin, J.P.; Fellous, J.M. Amygdala deep brain stimulation is superior to paroxetine treatment in a rat model of posttraumatic stress disorder. Brain Stimul. 2013, 6, 837–844. [Google Scholar] [CrossRef] [PubMed]
- Koek, R.J.; Langevin, J.P.; Krahl, S.E.; Kosoyan, H.J.; Schwartz, H.N.; Chen, J.W.; Melrose, R.; Mandelkern, M.J.; Sultzer, D. Deep brain stimulation of the basolateral amygdala for treatment-refractory combat post-traumatic stress disorder (PTSD): Study protocol for a pilot randomized controlled trial with blinded, staggered onset of stimulation. Trials 2014, 15. [Google Scholar] [CrossRef] [PubMed]
- Sturm, V.; Fricke, O.; Buhrle, C.P.; Lenartz, D.; Maarouf, M.; Treuer, H.; Mai, J.K.; Lehmkuhl, G. DBS in the basolateral amygdala improves symptoms of autism and related self-injurious behavior: A case report and hypothesis on the pathogenesis of the disorder. Front. Hum. Neurosci. 2013, 6, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Blake, D.D.; Weathers, F.W.; Nagy, L.M.; Kaloupek, D.G.; Gusman, F.D.; Charney, D.S.; Keane, T.M. The development of a clinician-administered PTSD Scale. J. Trauma Stress 1995, 8, 75–90. [Google Scholar] [CrossRef] [PubMed]
- Schaltenbrand, G.; Wahren, W. Atlas for Stereotaxy of the Human Brain, 3rd ed.; Thieme: New York, NY, USA, 2005. [Google Scholar]
- Mai, J.; Paxinos, G.; Voss, T. Atlas of the Human Brain, 3rd ed.; Elsevier: New York, NY, USA, 2008. [Google Scholar]
- Bancaud, J.; Brunet-Bourgin, F.; Chauvel, P.; Halgren, E. Anatomical origin of déjà vu and vivid “memories” in human temporal lobe epilepsy. Brain 1994, 117, 71–90. [Google Scholar] [CrossRef] [PubMed]
- Langevin, J.P.; Koek, R.J.; Schwartz, H.N.; Chen, J.W.; Sultzer, D.L.; Mandelkern, M.A.; Kulick, A.D.; Krahl, S.E. Deep brain stimulation of the basolateral amygdala for treatment-refractory posttraumatic stress disorder. Biol. Psychiatry 2015, 79, 82–84. [Google Scholar] [CrossRef] [PubMed]
- Engdahl, B.; Leuthold, A.C.; Tan, H.R.M.; Lewis, S.M.; Winskowski, A.M.; Dikel, T.N.; Georgopoulos, A.P. Post-traumatic stress disorder: A right temporal lobe syndrome? J. Neural. Eng. 2010, 7. [Google Scholar] [CrossRef] [PubMed]
- Pagani, M.; Hogberg, G.; Salmaso, D.; Tarnell, B.; Sanchez-Crespo, A.; Soares, J.; Aberg-Wistedt, A.; Jacobsson, H.; Hallstrom, T.; Larsson, S.A.; et al. Regional cerebral blood flow during auditory recall in 47 subjects exposed to assaultive and non-assaultive trauma and developing or not posttraumatic stress disorder. Eur. Arch. Psychiatry Clin. Neurosci. 2005, 255, 359–365. [Google Scholar] [CrossRef] [PubMed]
- Brazier, M.A.B.; Finesinger, J.E.; Coob, S. A contrast between the electroencephalograms of 100 psychoneurotic patients and those of 500 normal adults. Am. J. Psychiatry 1945, 101, 443–448. [Google Scholar] [CrossRef]
- Lader, M.H.; Wing, L. Physiological Measures, Sedative Drugs and Morbid Anxiety; Oxford University Press: London, UK, 1966. [Google Scholar]

© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Langevin, J.-P.; Chen, J.W.Y.; Koek, R.J.; Sultzer, D.L.; Mandelkern, M.A.; Schwartz, H.N.; Krahl, S.E. Deep Brain Stimulation of the Basolateral Amygdala: Targeting Technique and Electrodiagnostic Findings. Brain Sci. 2016, 6, 28. https://doi.org/10.3390/brainsci6030028
Langevin J-P, Chen JWY, Koek RJ, Sultzer DL, Mandelkern MA, Schwartz HN, Krahl SE. Deep Brain Stimulation of the Basolateral Amygdala: Targeting Technique and Electrodiagnostic Findings. Brain Sciences. 2016; 6(3):28. https://doi.org/10.3390/brainsci6030028
Chicago/Turabian StyleLangevin, Jean-Philippe, James W. Y. Chen, Ralph J. Koek, David L. Sultzer, Mark A. Mandelkern, Holly N. Schwartz, and Scott E. Krahl. 2016. "Deep Brain Stimulation of the Basolateral Amygdala: Targeting Technique and Electrodiagnostic Findings" Brain Sciences 6, no. 3: 28. https://doi.org/10.3390/brainsci6030028