Emotion Regulation in Adolescent Males with Attention-Deficit Hyperactivity Disorder: Testing the Effects of Comorbid Conduct Disorder
Abstract
:1. Introduction
2. Experimental Section
2.1. Sample
2.2. Clinical Measures
2.3. The Ultimatum Game
2.4. Data Analyses
3. Results
| NC (N = 47) | ADHD (N = 90) | ADHD + LA/CD (N = 64) | ADHD + HA/CD (N = 30) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Sig | Post Hoc | |
| Age | 15.19 | 1.33 | 13.70 | 1.89 | 14.28 | 1.80 | 13.47 | 1.55 | p < 0.001 | NC > ADHD and ADHD + LA/CD and ADHD + HA/CD |
| IQ | 88.00 | 9.46 | 93.41 | 10.33 | 88.92 | 9.18 | 86.57 | 8.70 | p < 0.05 | ADHD > ADHD + LA/CD and ADHD + HA/CD |
| ADHD score | N/A | N/A | 11.78 | 4.95 | 13.03 | 4.29 | 13.50 | 4.02 | ns | |
| Total CD score | N/A | N/A | 0.98 | 0.14 | 4.45 | 0.16 | 8.00 | 0.24 | p < 0.001 | ADHD < ADHD + LA/CD < ADHD+HA/CD |
| Aggressive CD score | N/A | N/A | 0.20 | 0.43 | 1.19 | 0.79 | 3.50 | 0.63 | p < 0.001 | ADHD < ADHD + LA/CD < ADHD + HA/CD |
| Non-Aggressive CD score | N/A | N/A | 0.78 | 0.73 | 3.27 | 1.36 | 4.50 | 1.93 | p < 0.001 | ADHD < ADHD + LA/CD < ADHD+HA/CD |
| CU traits | N/A | N/A | 16.56 | 6.15 | 19.28 | 7.19 | 22.28 | 5.32 | p < 0.001 | ADHD < ADHD + LA/CD and ADHD + HA/CD |
| ODD score | N/A | N/A | 2.91 | 2.46 | 4.41 | 2.72 | 5.37 | 2.53 | p < 0.001 | ADHD < ADHD + LA/CD and ADHD + HA/CD |
| Emotional symptoms | N/A | N/A | 4.78 | 2.75 | 4.88 | 2.47 | 5.43 | 3.12 | ns | |
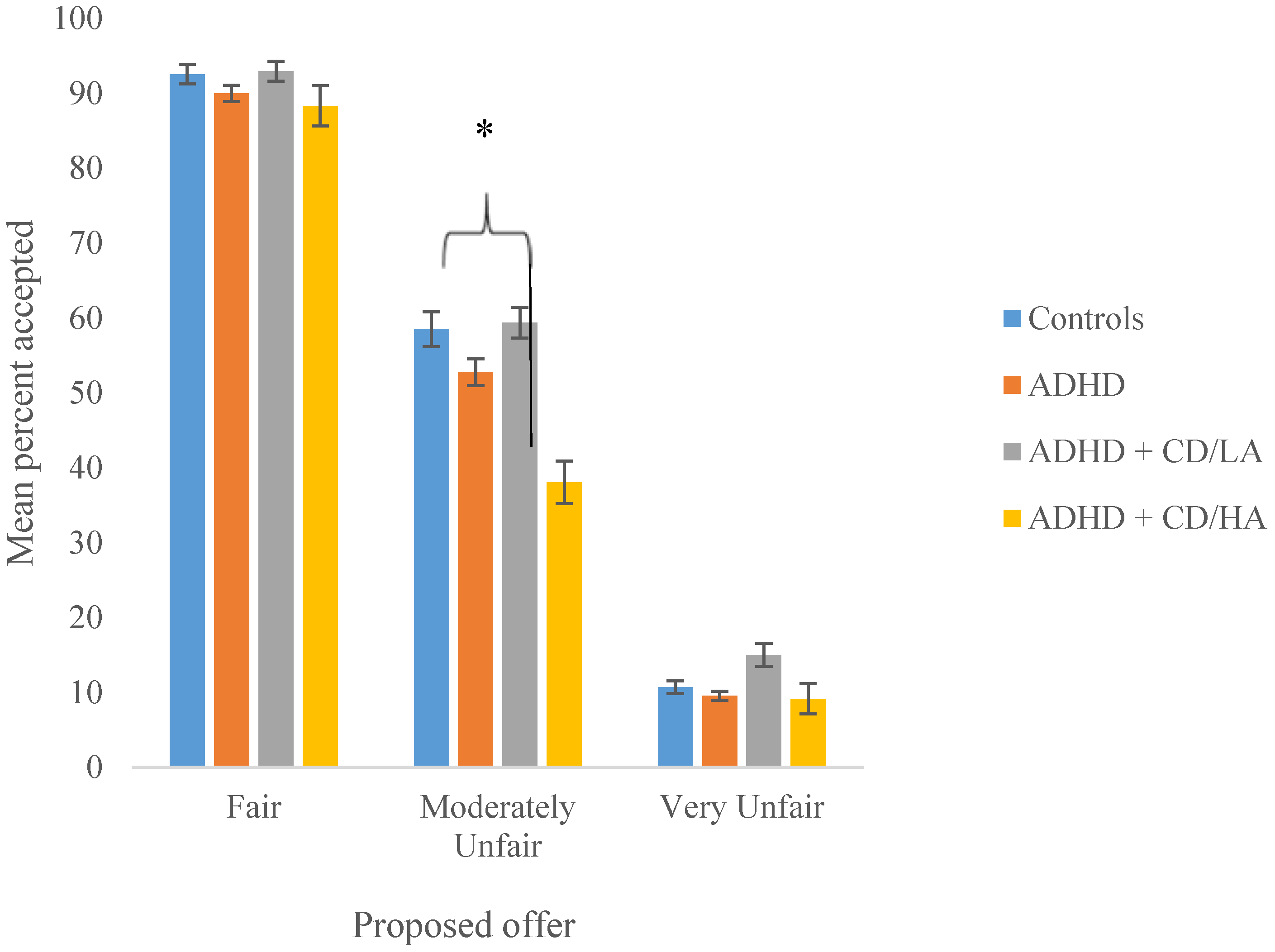
The Ultimatum Game
| NC (N = 47) | ADHD (N = 90) | ADHD + CD/LA (N = 64) | ADHD + CD/HA (N = 30) | |||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Proposed Offer | 1.77 | 1.13 | 1.97 | 1.41 | 2.30 | 1.63 | 2.34 | 1.78 |
| Age | IQ | ADHD | CD | Aggressive CD | CU Traits | ODD | Emotional Symptoms | Mod unfair | |
|---|---|---|---|---|---|---|---|---|---|
| Age | - | - | - | - | - | - | - | - | - |
| IQ | 0.02 | - | - | - | - | - | - | - | - |
| ADHD | −0.21 * | 0.24 * | - | - | - | - | - | - | - |
| CD | −0.14 | −0.08 | 0.18 | - | - | - | - | - | - |
| Aggressive CD | −0.32 ** | −0.17 | 0.10 | 0.66 ** | - | - | - | - | - |
| CU traits | −0.02 | −0.05 | 0.12 | 0.21 * | 0.16 | - | - | - | - |
| ODD | −0.09 | 0.05 | 0.45 ** | 0.27 * | 0.33 ** | 0.15 | - | - | - |
| Emotional symptoms | −0.22 * | 0.07 | 0.18 | 0.15 | 0.11 | −0.11 | 0.16 | - | - |
| Mod unfair | 0.19 | −0.05 | −0.18 | −0.21* | −0.25* | −0.11 | −0.06 | 0.02 | - |
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Jensen, S.A.; Rosen, L.A. Emotional reactivity in children with attention-deficit/hyperactivity disorder. J. Atten. Disord. 2004, 8, 53–61. [Google Scholar] [CrossRef] [PubMed]
- Braaten, E.B.; Rosen, L.A. Self-regulation of affect in attention deficit-hyperactivity disorder (ADHD) and non ADHD boys: Differences in empathic responding. J. Consult. Clin. Psychol. 2000, 68, 313–321. [Google Scholar] [CrossRef] [PubMed]
- Factor, P.I.; Rosen, P.J.; Reyes, R.A. The relation of poor emotional awareness and externalizing behavior among children with ADHD. J. Atten. Disord. 2013. [Google Scholar] [CrossRef] [PubMed]
- Thompson, R.A. Emotion regulation: A theme in search of definition. Monogr. Soc. Res. Child Dev. 1994, 59, 25–52. [Google Scholar] [CrossRef] [PubMed]
- Shaw, P.; Stringaris, A.; Nigg, J.; Leibenluft, E. Emotion dysregulation in attention deficit hyperactivity disorder. Am. J. Psychiatry 2014, 171, 276–293. [Google Scholar] [CrossRef] [PubMed]
- Stringaris, A.; Goodman, R. Three dimensions of oppositionality in youth. J. Child Psychol. Psychiatry 2009, 50, 216–223. [Google Scholar] [CrossRef] [PubMed]
- Clements, S.D. Minimal Brain Dysfunction in Children: Terminology and Identification: Phase One of a Three-Phase Project; Department of Health Education and Welfare: Washington, DC, USA, 1996. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 3rd ed.; American Psychiatric Press: Washington, DC, USA, 1980. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Press: Alrington, VA, USA, 2013. [Google Scholar]
- Gross, J.J. Emotion regulation: Affective, cognitive, and social consequences. Psychophysiology 2002, 39, 281–291. [Google Scholar] [CrossRef] [PubMed]
- Abelson, J.J.; Liberzon, I.; Young, E.A.; Khan, S. Cognitive modulation of the endocrine stress response to a pharmacological challenge in normal and panic disorder subjects. Arch. Gen. Psychiatry 2005, 62, 668–675. [Google Scholar] [CrossRef] [PubMed]
- Barkley, R.A. Why emotional impulsiveness should be a central feature of ADHD. ADHD Rep. 2010, 18, 1–5. [Google Scholar]
- Achenbach, T.; Rescorla, L. The Manual for the ASEBA School-Age Forms & Profiles; University of Vermont, Research Centre for Children, Youth, and Families: Burlington, VT, USA, 2001. [Google Scholar]
- Factor, P.I.; Reyes, R.A.; Rosen, P.J. Emotional Impulsivity in Children with ADHD Associated with Comorbid—Not ADHD—Symptomatology. J. Child Psychol. Psychiatry 2014, 36, 530–541. [Google Scholar] [CrossRef]
- Biederman, J.; Newcorn, J.; Sprich, S. Comorbidity of attention deficit hyperactivity disorder. Am. J. Psychiatry 1991, 148, 564–567. [Google Scholar] [PubMed]
- Thapar, A.; Langley, K.; Owen, M.J.; O’Donovan, M.C. Advances in genetic findings on attention deficit hyperactivity disorder. Psychol. Med. 2007, 37, 1681–1692. [Google Scholar] [CrossRef] [PubMed]
- Faraone, S.V.; Biederman, J.; Monuteaux, M.C. Toward guidelines for pedigree selection in genetic studies of attention deficit hyperactivity disorder. Genet. Epidemiol. 2000, 18, 1–16. [Google Scholar] [CrossRef]
- Thapar, A.; Harrington, R.; McGuffin, P. Examining the comorbidity of ADHD-related behaviours and conduct problems using a twin study design. Br. J. Psychiatry 2001, 179, 224–229. [Google Scholar] [CrossRef] [PubMed]
- Hamshere, M.L.; Langley, K.; Martin, J.; Agha, S.S.; Stergiakouli, E.; Anney, R.J.; Buitelaar, J.; Faraone, S.V.; Lesch, K.P.; Neale, B.M.; et al. High loading of polygenic risk for ADHD in children with comorbid aggression. Am. J. Psychiatry 2013, 170, 909–916. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Norvilitis, J.M.; Casey, R.J.; Brooklier, K.M.; Bonello, P.J. Emotion appraisal in children with attention-deficit/hyperactivity disorder and their parents. J. Atten. Disord. 2000, 4, 15–26. [Google Scholar]
- Scime, M.; Norvilitis, J.M. Task performance and response to frustration in children with attention deficit hyperactivity disorder. Psychol. Sch. 2006, 43, 377–386. [Google Scholar] [CrossRef]
- Singh, S.D.; Ellis, C.R.; Winton, A.S.; Singh, N.N.; Leung, J.P.; Oswald, D.P. Recognition of facial expressions of emotion by children with attention-deficit hyperactivity disorder. Behav. Modif. 1998, 22, 128–142. [Google Scholar]
- Melnick, S.M.; Hinshaw, S.P. Emotion regulation and parenting in AD/HD and comparison boys: Linkages with social behaviors and peer preference. J. Abnorm. Child Psychol. 2000, 28, 73–86. [Google Scholar] [CrossRef] [PubMed]
- Walcott, C.M.; Landau, S. The relation between disinhibition and emotion regulation in boys with attention deficit hyperactivity disorder. J. Clin. Child Adolesc. Psychol. 2004, 33, 772–782. [Google Scholar] [CrossRef] [PubMed]
- Guth, W.; Schmittenberger, R.; Schwarze, B. An experimental analysis of ultimatum bargaining. J. Econ. Behav. Organ. 1982, 3, 376–388. [Google Scholar] [CrossRef]
- Koenigs, M.; Tranel, D. Irrational economic decision-making after ventromedial prefrontal damage: Evidence from the ultimatum game. J. Neurosci. 2007, 27, 951–956. [Google Scholar] [CrossRef] [PubMed]
- Crockett, M.J.; Clark, L.; Tabibnia, G.; Lieberman, M.D.; Robbins, T.W. Serotonin modulates behavioural reactions to unfairness. Science 2008, 320, 1739. [Google Scholar] [CrossRef] [PubMed]
- Koenigs, M.; Kruepke, M.; Newman, J.P. Economic decision-making in psychopathy: A comparison with ventromedial prefrontal lesion patients. Neuropsychologia 2010, 48, 2198–2204. [Google Scholar] [CrossRef] [PubMed]
- Fishburn, P.C. Utility Theory for Decision Making; Wiley: New York, NY, USA, 1970. [Google Scholar]
- Bolton, G.E.; Zwick, R. Anonymity versus punishment in ultimatum bargaining. Game Econ. Behav. 1995, 10, 95–121. [Google Scholar] [CrossRef]
- Van’t Wout, M.; Kahn, R.S.; Sanfey, A.G.; Aleman, A. Affective state and decision-making in the Ultimatum Game. Exp. Brain Res. 2006, 169, 564–568. [Google Scholar] [CrossRef] [PubMed]
- Pillutla, M.M.; Murnighan, J.K. Unfairness, anger, and spite: Emotional rejections of ultimatum offers. Organ. Behav. Hum. Dec. 1996, 68, 208–224. [Google Scholar] [CrossRef]
- Fehr, E.; Gachter, S. Altruistic punishment in humans. Nature 2002, 415, 137–140. [Google Scholar] [CrossRef] [PubMed]
- Harle, K.M.; Sanfey, A.G. Incidental sadness biases social economic decisions in the Ultimatum Game. Emotion 2007, 7, 876–881. [Google Scholar] [CrossRef] [PubMed]
- Grecucci, A.; Giorgetta, C.; van’t Wout, M.; Bonini, N.; Sanfey, A.G. Reappraising the ultimatum: An fMRI study of emotion regulation and decision making. Cereb. Cortex 2013, 23, 399–410. [Google Scholar] [CrossRef] [PubMed]
- Van’t Wout, M.; Chang, L.J.; Sanfey, A.G. The influence of emotion regulation on social interactive decision-making. Emotion 2010, 10, 815–821. [Google Scholar] [CrossRef] [PubMed]
- Kirk, D.; Gollwitzer, P.M.; Carnevale, P.J. Self-regulation in ultimatum bargaining: Goals and plans help accepting unfair but profitable offers. Soc. Cogn. 2011, 29, 528–546. [Google Scholar] [CrossRef]
- Gospic, K.; Mohlin, E.; Fransson, P.; Petrovic, P.; Johannesson, M.; Ingvar, M. Limbic justice: Amygdala involvement in immediate rejection in the ultimatum game. PLoS Biol. 2011, 9. [Google Scholar] [CrossRef] [PubMed]
- Sanfey, A.G.; Rilling, J.K.; Aronson, J.A.; Nystrom, L.E.; Cohen, J.D. The neural basis of economic decision-making in the ultimatum game. Science 2008, 300, 1755–1758. [Google Scholar] [CrossRef] [PubMed]
- Anderson, S.W.; Barrash, J.; Bechara, A.; Tranel, D. Impairments of emotion and real-world complex behavior following childhood- or adult-onset damage to ventromedial prefrontal cortex. J. Int. Neuropsychol. Soc. 2006, 12, 224–235. [Google Scholar] [CrossRef] [PubMed]
- Barrash, J.; Tranel, D.; Anderson, S.W. Acquired personality disturbances associated with bilateral damage to the ventromedial prefrontal region. Dev. Neuropsychol. 2000, 18, 355–381. [Google Scholar] [CrossRef] [PubMed]
- Berlin, H.A.; Rolls, E.T.; Kischka, U. Impulsivity, time perception, emotion, and reinforcement sensitivity in patients with orbitofrontal cortex lesions. Brain 2004, 127, 1108–1126. [Google Scholar] [CrossRef] [PubMed]
- Grafman, J.; Schwab, K.; Warden, D.; Pridgen, A.; Brown, H.R.; Salazar, A.M. Frontal lobe injuries, violence, and aggression: A report of the Vietnam head injury study. Neurology 1996, 46, 1231–1238. [Google Scholar] [CrossRef] [PubMed]
- Blumer, D.; Benson, D.F. Personality Changes with Frontal and Temporal Lobe Lesions. In Psychiatric Aspects of Neurological Disease; Benson, D.F., Blumer, D., Eds.; Grune and Stratton: New York, NY, USA, 1975; pp. 151–170. [Google Scholar]
- Damasio, A.R.; Tranel, D.; Damasio, H. Individuals with sociopathic behavior caused by frontal damage fail to respond autonomically to social stimuli. Behav. Brain Res. 1990, 41, 81–94. [Google Scholar] [CrossRef]
- Eslinger, P.J.; Damasio, A.R. Severe disturbance of higher cognition after bilateral frontal lobe ablation: Patient EVR. Neurology 1985, 35, 1731–1741. [Google Scholar] [CrossRef] [PubMed]
- Vieira, J.B.; Almeida, P.R.; Ferreira-Santos, F.; Barbosa, F.; Marques-Teixeira, J.; Marsh, A.A. Distinct neural activation patterns underlie economic decisions in high and low psychopathy scorers. Soc. Cogn. Affect. Neurosci. 2014, 9, 1099–1107. [Google Scholar] [CrossRef] [PubMed]
- Murnighan, J.K.; Saxon, M.S. Ultimatum bargaining by children and adults. J. Econ. Psychol. 1998, 19, 415–445. [Google Scholar] [CrossRef]
- Harbaugh, W.T.; Krause, K.; Liday, S.G. Bargaining by children. Soc. Sci. Res. Netw. 2003, 2002–2040. [Google Scholar] [CrossRef]
- Hoffman, R.; Tee, J. Adolescent-adult interactions and culture in the ultimatum game. J. Econ. Psychol. 2006, 27, 98–116. [Google Scholar] [CrossRef]
- Brenhouse, H.C.; Andersen, S.L. Developmental trajectories during adolescence in males and females: A cross-species understanding of underlying brain changes. Neurosci. Biobehav. Rev. 2011, 35, 1697–1703. [Google Scholar] [CrossRef] [PubMed]
- Frick, P.J.; Morris, A.S. Temperament and developmental pathways to conduct problems. J. Clin. Child Adolesc. Psychol. 2004, 33, 54–68. [Google Scholar] [CrossRef] [PubMed]
- Burt, S.A.; Donnellan, M.B. Personality correlates of aggressive and non-aggressive antisocial behavior. Personal. Individ. Differ. 2008, 44, 53–63. [Google Scholar] [CrossRef]
- Lahey, B.B.; Waldman, I.D. Annual research review: Phenotypic and causal structure of conduct disorder in the broader context of prevalent forms of psychopathology. J. Child Psychol. Psychiatry 2012, 53, 536–557. [Google Scholar] [CrossRef] [PubMed]
- Hawes, D.J.; Price, M.J.; Dadds, M.R. Callous-unemotional traits and the treatment of conduct problems in childhood and adolescence: A comprehensive review. Clin. Child Fam. Psychol. Rev. 2014, 17, 248–267. [Google Scholar] [CrossRef] [PubMed]
- Frick, P.J.; Ray, J.V.; Thornton, L.C.; Kahn, R.E. Can callous-unemotional traits enhance the understanding, diagnosis, and treatment of serious conduct problems in children and adolescents? A comprehensive review. Psychol. Bull. 2014, 140, 1–57. [Google Scholar] [CrossRef] [PubMed]
- Osumi, T.; Ohira, H. The positive side of psychopathy: Emotional detachment in psychopathy and rational decision-making in the ultimatum game. Personal. Individ. Differ. 2010, 49, 451–456. [Google Scholar] [CrossRef]
- White, S.F.; Brislin, S.J.; Meffert, H.; Sinclair, S.; Blair, R.J.R. Callous-unemotional traits modulate the neural response associated with punishing another individual during social exchange: A preliminary investigation. Personal. Disord. 2013, 27, 99–112. [Google Scholar] [CrossRef] [PubMed]
- Radke, S.; Brazil, I.A.; Scheper, I.; Bulten, B.H.; De Bruijn, E.R. Unfair offers, unfair offenders? Fairness considerations in incarcerated individuals with and without psychopathy. Front. Hum. Neurosci. 2013, 7, 406. [Google Scholar] [CrossRef] [PubMed]
- Achenbach, T.M. Manual for the YSR and 1991 Profile; University of Vermont: Burlington, VT, USA, 1991. [Google Scholar]
- Wechsler, D. Wechsler Abbreviated Scale of Intelligence (WASI); Harcourt: San Antonio, TX, USA, 1999. [Google Scholar]
- Goodman, R.; Ford, T.; Richards, H.; Gatward, R.; Meltzer, H. The development well-being assessment: Description and initial validation of an integrated assessment of child and adolescent psychopathology. J. Child Psychol. Psychiatry 2000, 41, 645–655. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed.; American Psychiatric Press: Washington, DC, USA, 2000. [Google Scholar]
- World Health Organisation (WHO). Classification of Mental and Behavioural Disorders: Research Diagnostic Criteria, 10th ed.; World Health Organization: Genva, Switzerland, 1992. [Google Scholar]
- Loeber, R.; Burke, J.; Pardini, D.A. Perspectives on oppositional defiant disorder, conduct disorder, and psychopathic features. J. Child Psychol. Psychiatry 2009, 50, 133–142. [Google Scholar] [CrossRef] [PubMed]
- Andershed, H.; Kerr, M.; Stattin, H.; Levander, S. Psychopathic Traits in Nonreferred Youths: A New Assessment Tool. In Psychopaths: Current International Perspectives; Blaauw, E., Sheridan, L., Eds.; Elsevier: The Hague, Netherlands, 2002; pp. 131–158. [Google Scholar]
- Andershed, H.; Hodgins, S.; Tengstrom, A. Convergent validity of the Youth Psychopathic Traits Inventory (YPI): Association with the Psychopathy Checklist: Youth Version (PCL-YV). Assessment 2007, 14, 144–154. [Google Scholar] [CrossRef] [PubMed]
- Skeem, J.L.; Cauffman, E. Views of the downward extension: Comparing the youth version of the Psychopathy Checklist with the Youth Psychopathic Traits Inventory. Behav. Sci. Law 2003, 21, 737–770. [Google Scholar] [CrossRef] [PubMed]
- Goodman, A.; Goodman, R. Strengths and difficulties questionnaire as a dimensional measure of child mental health. J. Am. Acad. Child Adolesc. Psychiatry 2009, 48, 400–403. [Google Scholar] [CrossRef] [PubMed]
- Van der Schalk, J.; Hawk, S.T.; Fischer, A.H.; Doosje, B. Moving faces, looking places: Validation of the Amsterdam Dynamic Facial Expression Set (ADFES). Emotion 2011, 11, 907–920. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Erlbaum: Hillsdale, MG, USA, 1988. [Google Scholar]
- Frick, P.J. Developmental pathways to conduct disorder: Implications for future directions in research, assessment, and treatment. J. Clin. Child Adolesc. Psychol. 2012, 41, 378–389. [Google Scholar] [CrossRef] [PubMed]
- Fehr, E.; Fischbacher, U. The nature of human altruism. Nature 2003, 425, 785–791. [Google Scholar] [CrossRef] [PubMed]
- Knoch, D.; Pascual-Leone, A.; Meyer, K.; Treyer, V.; Fehr, E. Diminishing reciprocal fairness by disrupting the right prefrontal cortex. Science 2006, 314, 829–832. [Google Scholar] [CrossRef] [PubMed]
- Civai, C.; Corradi-Dell’Acqua, C.; Gamer, M.; Rumiati, R.I. Are irrational reactions to unfairness truly emotionally-driven? Dissociated behavioural and emotional responses in the Ultimatum Game task. Cognition 2010, 114, 89–95. [Google Scholar] [CrossRef] [PubMed]
- Van den Bos, W.; Vahl, P.; Güroğlu, B.; van Nunspeet, F.; Colins, O.; Markus, M.; Rombouts, S.A.R.B.; van der Wee, N.; Vermeiren, R.; Crone, E.A. Neural correlates of social decision-making in severely antisocial adolescents. Soc. Cogn. Affect. Neurosci. 2014, 9, 2059–2066. [Google Scholar] [CrossRef] [PubMed]
- Sterzer, P.; Stadler, C. Neuroimaging of aggressive and violent behaviour in children and adolescents. Front. Behav. Neurosci. 2009, 3, 35. [Google Scholar] [CrossRef] [PubMed]
- Fairchild, G.; VanGoozen, S.; Stollery, S.; Aitken, M.; Savage, J.; Moore, S.; Goodyer, I. Decision making and executive function in male adolescents with early-onset or adolescence-onset conduct disorder and control subjects. Biol. Psychiatry 2009, 66, 162–168. [Google Scholar] [CrossRef] [PubMed]
- Hampshire, A.; Chamberlain, S.R.; Monti, M.M.; Duncan, J.; Owen, A.M. The role of the right inferior frontal gyrus: Inhibition and attentional control. NeuroImage 2010, 50, 1313–1319. [Google Scholar] [CrossRef] [PubMed]
- Aron, A.R.; Behrens, T.E.; Smith, S.; Frank, M.J.; Poldrack, R.A. Triangulating a cognitive control network using diffusion-weighted magnetic resonance imaging (MRI) and functional MRI. J. Neurosci. 2007, 27, 3743–3752. [Google Scholar] [CrossRef] [PubMed]
- Van Goozen, S.H.; Fairchild, G.; Snoek, H.; Harold, G.T. The evidence for a neurobiological model of childhood antisocial behavior. Psychol. Bull. 2007, 133, 149–182. [Google Scholar] [CrossRef] [PubMed]
- Fairchild, G.; Van Goozen, S.H.; Stollery, S.J.; Goodyer, I.M. Fear Conditioning and Affective Modulation of the Startle Reflex in Male Adolescents with Early-Onset or Adolescence-Onset Conduct Disorder and Healthy Control Subjects. Biol. Psychiatry 2008, 63, 279–285. [Google Scholar] [CrossRef] [PubMed]
- Suveg, C.; Kendall, P.C.; Comer, J.S.; Robin, J. Emotion-focused cognitive-behavioral therapy for anxious youth: A multiple-baseline evaluation. J. Contemp. Psychother. 2006, 36, 77–85. [Google Scholar]
- Kovacs, M.; Sherrill, J.; George, C.J.; Pollock, M.; Tumuluru, R.V.; Ho, V. Contextual emotion-regulation therapy for childhood depression: Description and pilot testing of a new intervention. J. Am. Acad. Child Adolesc. Psychiatry 2006, 45, 892–903. [Google Scholar] [CrossRef] [PubMed]
- Kazdin, A.E.; Siegel, T.C.; Bass, D. Cognitive problem-solving skills training and parent management training in the treatment of antisocial behavior in children. J. Consult. Clin. Psychol. 1992, 60, 733–747. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Northover, C.; Thapar, A.; Langley, K.; Van Goozen, S. Emotion Regulation in Adolescent Males with Attention-Deficit Hyperactivity Disorder: Testing the Effects of Comorbid Conduct Disorder. Brain Sci. 2015, 5, 369-386. https://doi.org/10.3390/brainsci5030369
Northover C, Thapar A, Langley K, Van Goozen S. Emotion Regulation in Adolescent Males with Attention-Deficit Hyperactivity Disorder: Testing the Effects of Comorbid Conduct Disorder. Brain Sciences. 2015; 5(3):369-386. https://doi.org/10.3390/brainsci5030369
Chicago/Turabian StyleNorthover, Clare, Anita Thapar, Kate Langley, and Stephanie Van Goozen. 2015. "Emotion Regulation in Adolescent Males with Attention-Deficit Hyperactivity Disorder: Testing the Effects of Comorbid Conduct Disorder" Brain Sciences 5, no. 3: 369-386. https://doi.org/10.3390/brainsci5030369





