Combined Effects of Fe3O4 Nanoparticles and Chemotherapeutic Agents on Prostate Cancer Cells In Vitro
Abstract
:1. Introduction
2. Materials and Methods
2.1. NP Solution Preparation and Chemical Agents
2.2. Cell Lines
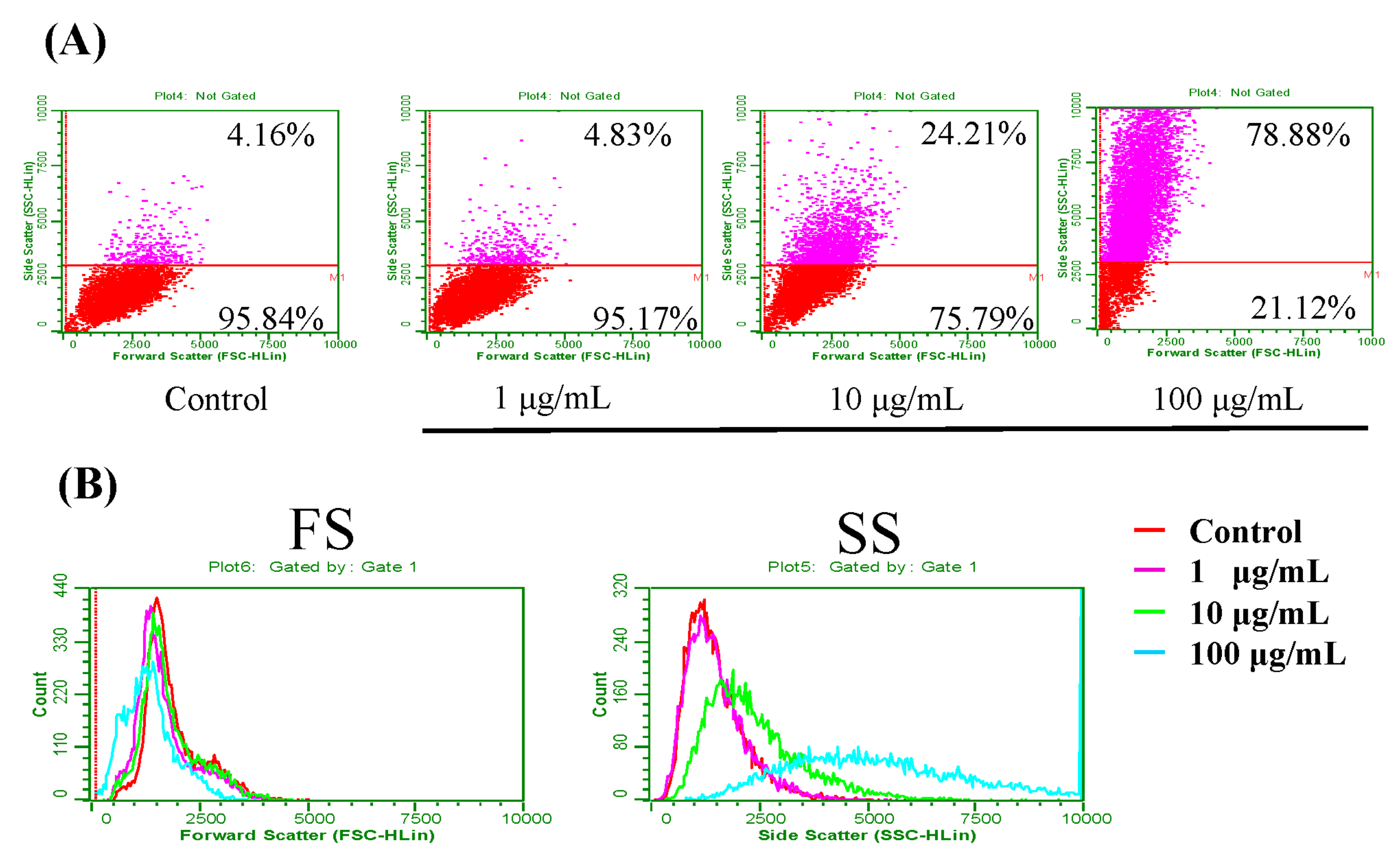
2.3. Flow Cytometry (FCM) Analysis for Fe3O4 NPs Uptake by Prostate Cancer Cells
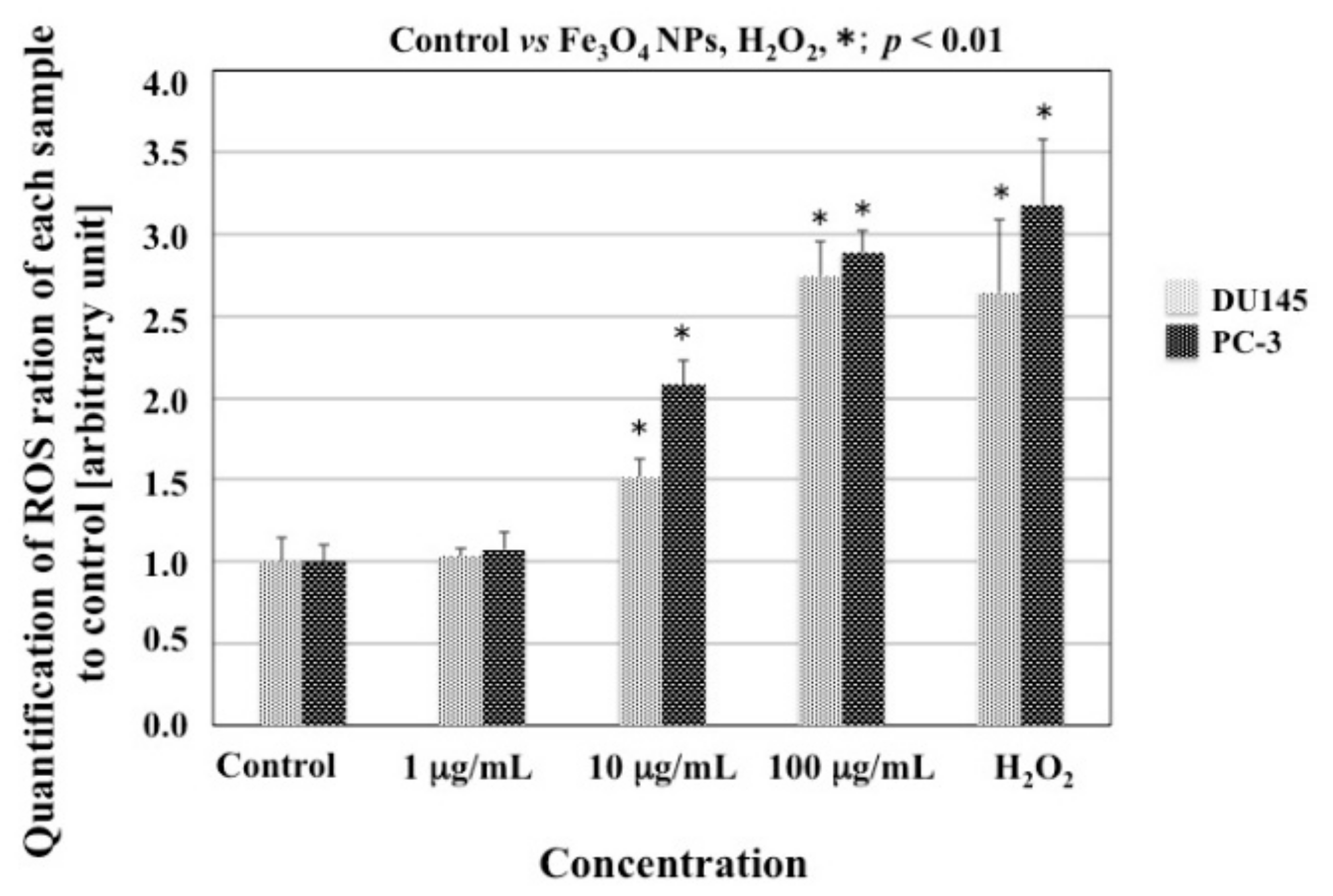
2.4. Measurement of Intracellular Reactive Oxygen Species (ROS)
2.5. FCM Analysis for the Cell Cycle
2.6. Alamar Blue Assay for Cell Viability
2.7. FCM Analysis for Cell Apoptosis
2.8. Real-Time Quantitative Polymerase Chain Reaction (RT-qPCR)
2.9. Western Blot Analysis
2.10. Statistical Analysis
3. Results
3.1. Fe3O4 NPs Uptake
3.2. Effects of Fe3O4 NPs on Cell Viability
3.3. ROS Production in Cells Treated with Fe3O4 NPs
3.4. Effects of Fe3O4 NPs on the Cell Cycle
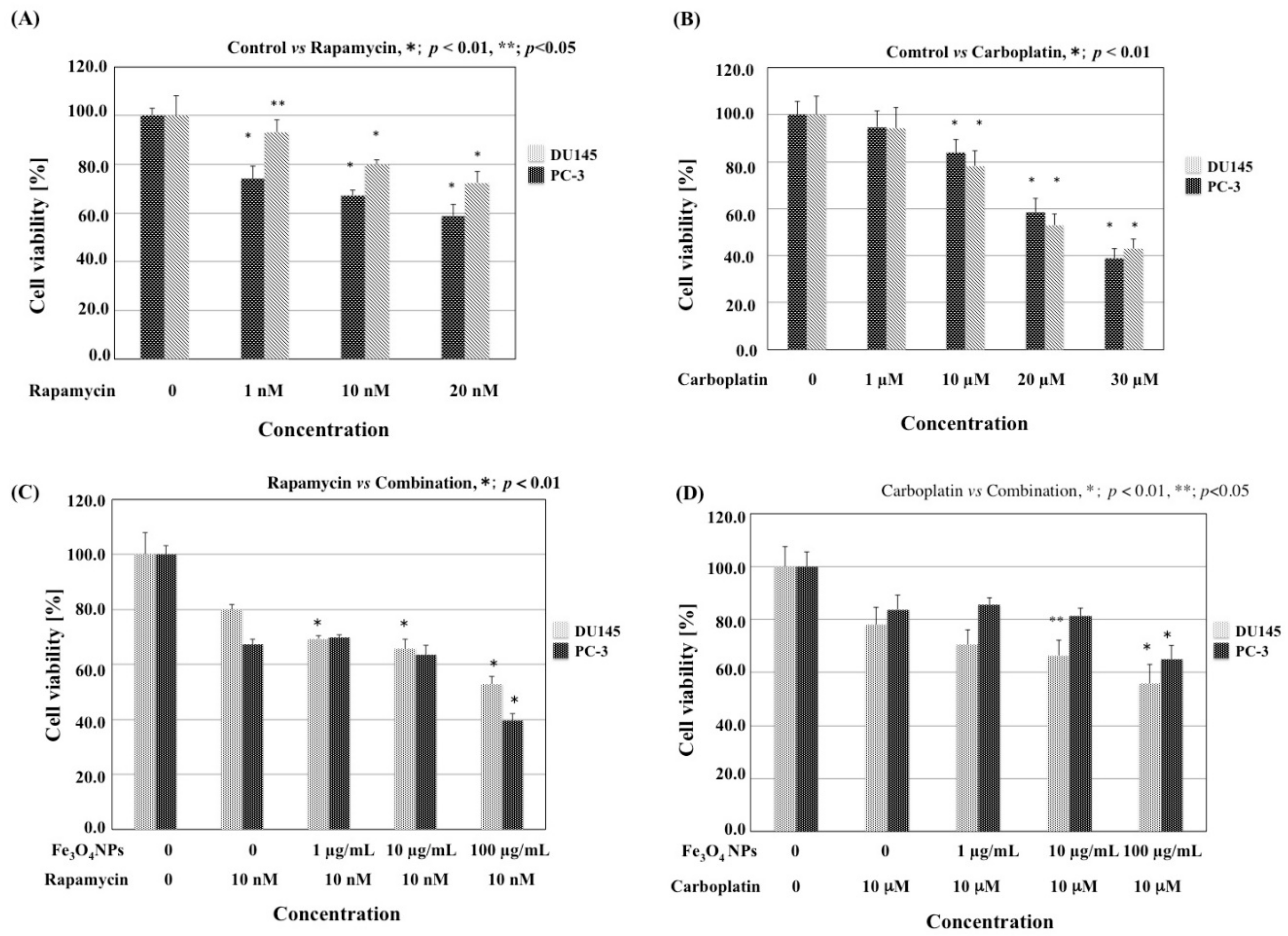
3.5. Combined Effects of Fe3O4 NPs and Chemotherapeutic Agents on Cell Viability
3.6. Combined Effects of Fe3O4 NPs and Chemotherapeutic Agents on Apoptosis
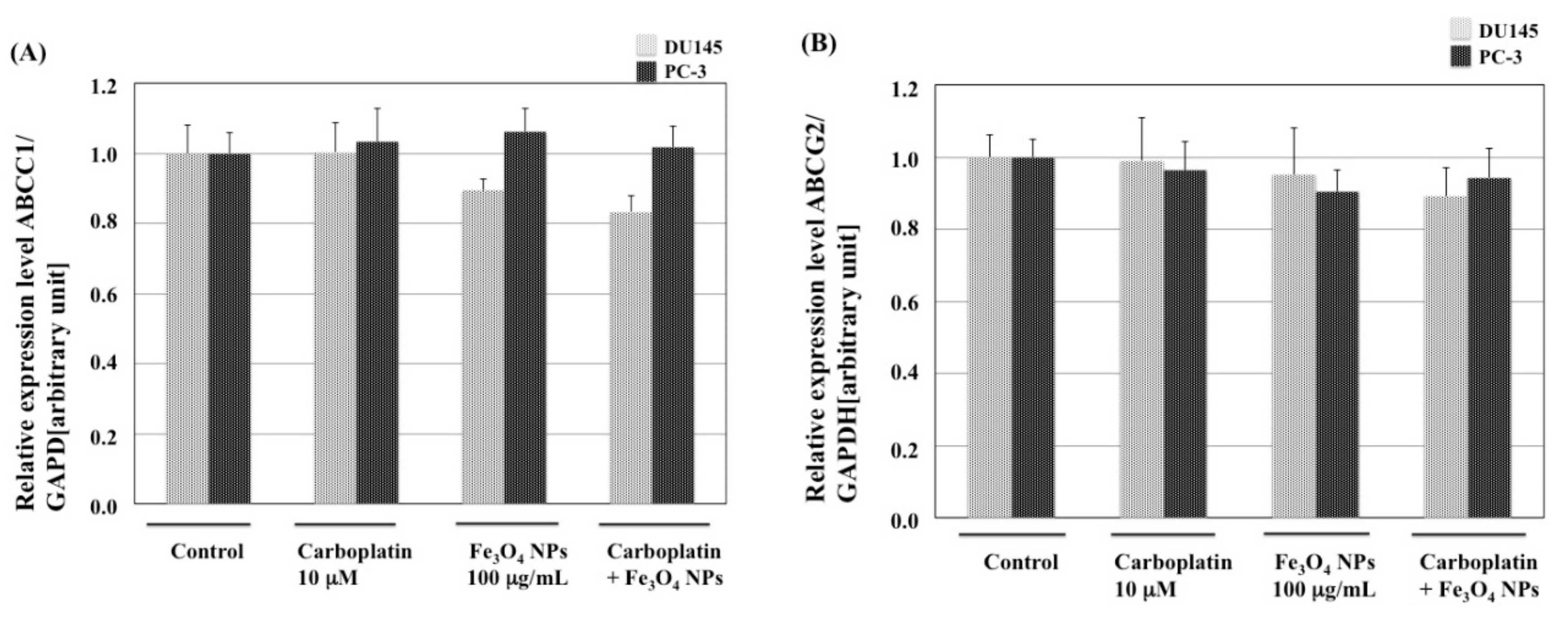
3.7. Effects of Fe3O4 NPs, Chemotherapeutic Agents, and Their Combinations on the Expression of MDR1, MRP1, and BCRP mRNA in Prostate Cancer Cells
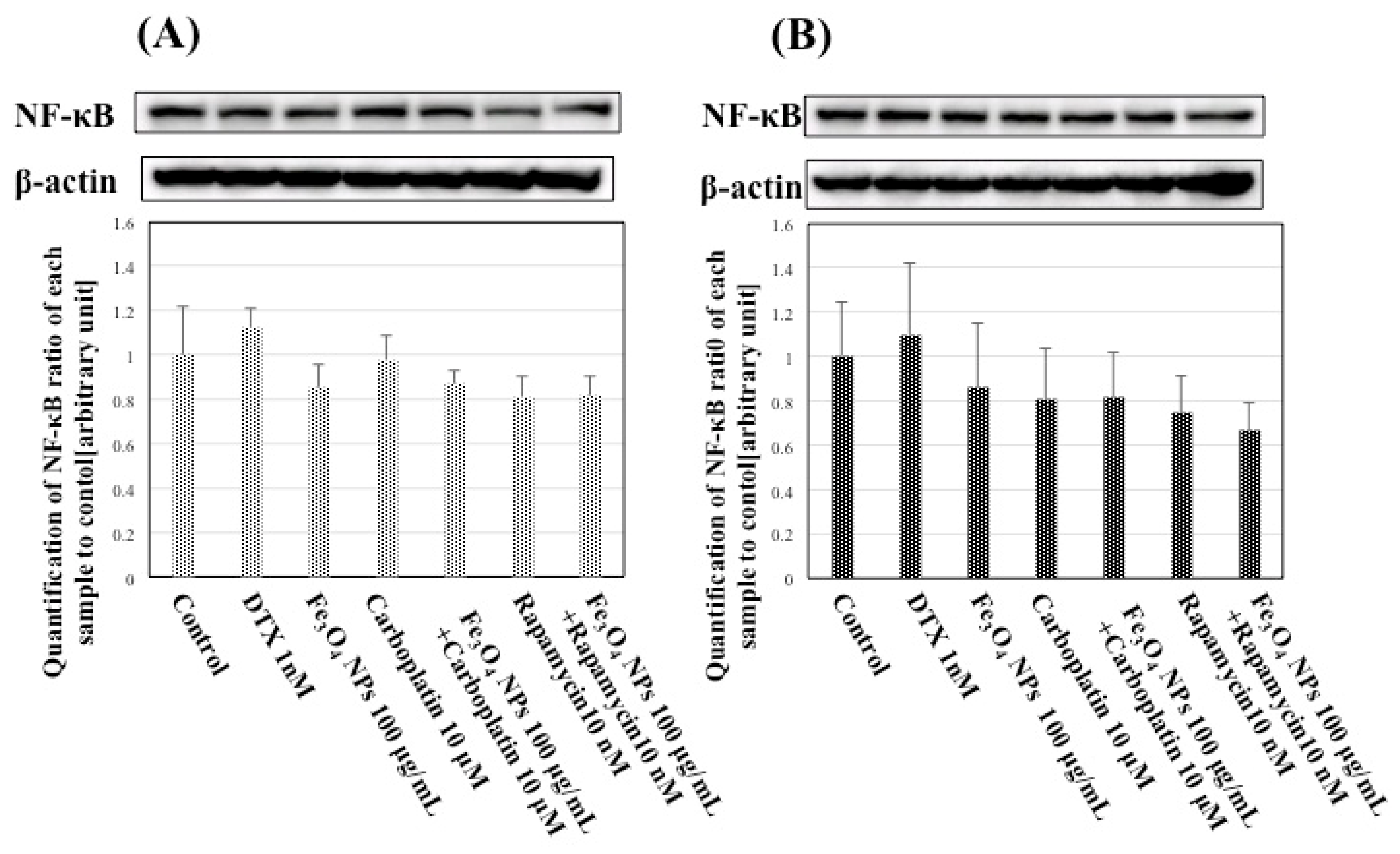
3.8. Effects of Fe3O4 NPs, Chemotherapeutic Agents, and Their Combinations on NF-κB Expression in Prostate Cancer Cells
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| ADT | Androgen-deprivation therapy |
| ABCC1 | ATP-binding cassette subfamily C member 1 |
| ABCG2 | ATP-binding cassette subfamily G member2 |
| BCRP | Breast Cancer Resistance Protein |
| CRPC | Castration-Resistant Prostate Cancer |
| CI | Cooperative Index |
| DMSO | Dimetyl sulfoxide |
| DTX | Docetaxel |
| DLS | Dynamic light scattering |
| FBS | Fetal bovine serum |
| Fe3O4 NPs | Fe3O4 nanoparticles |
| FCM | Flow cytometery |
| FITC | Fluorescein isothiocyanate |
| FS | Forward-scattered |
| GAPDH | Glyceraldehyde 3-phosphate dehydrogenase |
| MNPs | Magnetic nanoparticles |
| mTOR | mammalian target of rapamycin |
| mCRPC | metastatic castration-resistant prostate cancer |
| MRP1 | Multiple drug resistance 1 |
| NPs | Nanoparticles |
| NF-κB | Nuclear Factor-kappa B |
| PBS | phosphate-buffered saline |
| PDI | Polydispersity index |
| PI | Propidium Iodide |
| PSA | Prostate-Specific Antigen |
| ROS | Reactive Oxygen Species |
| RT-qPCR | Real-time quantitateive polymerase chain reaction |
| SS | Side-scattered |
| TEM | Transmission electron microscopy |
| XRD | X-ray powder diffraction |
References
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2016. CA Cancer J. Clin. 2016, 66, 7–30. [Google Scholar] [CrossRef] [PubMed]
- Seisen, T.; Rouprêt, M.; Gomez, F.; Malouf, G.G.; Shariat, S.F.; Peyronnet, B.; Spano, J.P.; Cancel-Tassin, G.; Cussenot, O. A comprehensive review of genomic landscape, biomarkers and treatment sequencing in castration-resistant prostate cancer. Cancer Treat. Rev. 2016, 48, 25–33. [Google Scholar] [CrossRef] [PubMed]
- Chandrasekar, T.; Yang, J.C.; Gao, A.C.; Evans, C.P. Mechanisms of the resistance in castration-resistance prostate cancer (CRPC). Transl. Androl. Urol. 2015, 4, 365–380. [Google Scholar] [PubMed]
- Chakraborty, M.; Jain, S.; Rani, V. Nanotechnology: Emerging tool for diagnostic and therapeutics. Appl. Biochem. Biotechnol. 2011, 165, 1178–1187. [Google Scholar] [CrossRef] [PubMed]
- Mahmoudi, M.; Sant, S.; Wang, B.; Laurent, S.; Sen, T. Superparamagnetic iron oxide nanoparticles (SPIONs): Development, surface modification and applications in chemotherapy. Adv. Drug Deliv. Rev. 2011, 63, 24–46. [Google Scholar] [CrossRef] [PubMed]
- Vinardell, M.P.; Mitjans, M. Antitumor activities of metal oxide nanoparticles. Nanomaterials 2015, 5, 1004–1021. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Calero, M.; Chiappi, M.; Lazaro-Carrillo, A.; Rodríguez, M.J.; Chichón, F.J.; Crosbie-Staunton, K.; Prina-Mello, A.; Volkov, Y.; Villanueva, A.; Carrascosa, J.L. Characterization of interaction of magnetic nanoparticles with breast cancer cells. J. Nanotechnol. 2015, 13, 16. [Google Scholar] [CrossRef] [PubMed]
- Chen, B.A.; Dai, Y.; Wang, X.M.; Zhang, R.Y.; Xu, W.L.; Shen, H.L.; Gao, F.; Sun, Q.; Deng, X.J.; Ding, J.H.; et al. Synergistic effect of the combination of nanoparticulate Fe3O4 and Au with daunomycin on K562/A02 cells. Int. J. Nanomed. 2008, 3, 343–350. [Google Scholar] [CrossRef]
- Chen, B.; Cheng, J.; Shen, M.; Gao, F.; Xu, W.; Shen, H.; Ding, J.; Gao, C.; Sun, Q.; Sun, X.; et al. Magnetic nanoparticle of Fe3O4 and 5-bromotetrandrin interact synergistically to induce apoptosis by daunorubicin in leukemia cells. Int. J. Nanomed. 2009, 4, 65–71. [Google Scholar]
- Jing, H.; Wang, J.; Yang, P.; Ke, X.; Xia, G.; Chen, B. Magnetic Fe3O4 nanoparticles and chemotherapy agents interact synergistically to induce apoptosis in lymphoma cells. Int. J. Nanomed. 2010, 5, 999–1004. [Google Scholar]
- Zhang, W.; Qiao, L.; Wang, X.; Senthilkumar, R.; Wang, F.; Chen, B. Inducing cell cycle arrest and apoptosis by dimercaptosuccinic acid modified Fe3O4 magnetic nanoparticles combined with nontoxic concentration of bortezomib and gambogic acid in RPMI-8226 cells. Int. J. Nanomed. 2015, 10, 3275–3289. [Google Scholar]
- Sato, A.; Itcho, N.; Ishiguro, H.; Okamoto, D.; Kobayashi, N.; Kawai, K.; Kasai, H.; Kurioka, D.; Uemura, H.; Kubota, Y.; et al. Magnetic nanoparticles of Fe3O4 enhance docetaxel-induced prostate cancer cell death. Int. J. Nanomed. 2013, 8, 3151–3160. [Google Scholar]
- Suzuki, H.; Toyooka, T.; Ibuki, Y. Simple and easy method to evaluate uptake potential of nanoparticles in mammalian cells using a flow cytometric light scatter analysis. Environ. Sci. Technol. 2007, 41, 3018–3024. [Google Scholar] [CrossRef] [PubMed]
- Zucker, R.M.; Massaro, E.J.; Sanders, K.M.; Degn, L.L.; Boyes, W.K. Detection of TiO2 nanoparticles in cells by flow cytometry. Cytom. Part A 2010, 77, 677–685. [Google Scholar] [CrossRef] [PubMed]
- Foucquier, J.; Guedj, M. Analysis of drug combinations: Current methodical landscape. Pharmacol. Res. Perspect. 2015, 3, e00149. [Google Scholar] [CrossRef] [PubMed]
- Codony-Servat, J.; Marin-Aguilera, M.; Visa, L.; García-Albéniz, X.; Pineda, E.; Fernández, P.L.; Filella, X.; Gascón, P.; Mellado, B. Nuclear factor-kappa B and interleukin-6 related docetaxel resistance in castration-resistant prostate cancer. Prostate 2013, 73, 512–521. [Google Scholar] [CrossRef] [PubMed]
- Gao, F.; Yuan, Q.; Gao, L.; Cai, P.; Zhu, H.; Liu, R.; Wang, Y.; Wei, Y.; Huang, G.; Liang, J.; et al. Cytotoxicity and therapeutic effect of irinotecan combined with selenium nanoparticles. Biomaterials 2014, 35, 8854–8866. [Google Scholar] [CrossRef] [PubMed]
- Xiong, X.; Arvizo, R.A.; Saha, S.; Robertson, D.J.; McMeekin, S.; Bhattachrya, R.; Mukherjee, P. Sensitization of ovarian cancer cells to cisplatin by gold nanoparticles. Oncotarget 2014, 5, 6453–6465. [Google Scholar] [CrossRef] [PubMed]
- Gobbo, O.L.; Sjaastad, K.; Radomski, M.W.; Volkov, Y.; Prina-Mello, A. Magnetic nanoparticles in cancer theranostics. Theranostics 2015, 5, 1249–1263. [Google Scholar] [CrossRef] [PubMed]
- Kovács, D.; Szőke, K.; Igaz, N.; Spengler, G.; Molnár, J.; Tóth, T.; Madarász, D.; Rázga, Z.; Kónya, Z.; Boros, I.M.; et al. Silver nanoparticles modulate ABC transporter activity and enhance chemotherapy in multidrug resistant cancer. Nanomedicine 2016, 12, 601–610. [Google Scholar] [CrossRef] [PubMed]
- Petrushev, B.; Boca, S.; Simon, T.; Berce, C.; Frinc, I.; Dima, D.; Selicean, S.; Gafencu, G.A.; Tanase, A.; Zdrenghea, M.; et al. Gold nanoparticles enhance the effect of tyrosine kinase inhibitors in acute myeloid leukemia therapy. Int. J. Nanomed. 2016, 11, 641–660. [Google Scholar]
- Wang, J.; Yi, J. Cancer cell killing via ROS: To increase or decrease, that is the question. Cancer Biol. Ther. 2008, 7, 1875–1884. [Google Scholar] [CrossRef] [PubMed]
- Shang, L.; Nienhaus, K.; Nienhaus, G.U. Engineered nanoparticles interacting with cells: Size matters. J. Nanobiotechnol. 2014, 12, 5. [Google Scholar] [CrossRef] [PubMed]
- Wiogo, H.T.R.; Lim, M.; Bulmus, V.; Yun, J.; Aml, R. Stabilization of magnetic iron oxide nanoparticles in biological media by fetal bovine serum (FBS). Langmuir 2011, 27, 843–850. [Google Scholar] [CrossRef] [PubMed]
- Sabuncu, A.C.; Grubbs, J.; Qian, S.; Abdel-Fattah, T.M.; Stacey, M.W.; Beskok, A. Probing nanoparticle interactions in cell culture media. Colloids Surf. B Biointerfaces 2012, 95, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Moore, T.L.; Rodriguez-Lorenzo, L.; Hirsch, V.; Balog, S.; Urban, D.; Jud, C.; Rothen-Rutishauser, N.; Lattuada, M.; Petri-Fink, A. Nanoparticl coolidal stability in cell culture media and impact on cellular interactions. Chem. Soc. Rev. 2015, 44, 6287–6305. [Google Scholar]
- Singh, N.; Jenkins, G.J.S.; Asadi, R.; Doak, S.H. Potential toxicity of superparamagnetic iron oxide nanoparticles (SPION). Nano Rev. 2010, 1, 10. [Google Scholar] [CrossRef] [PubMed]
- Khandrika, L.; Kumar, B.; Koul, S.; Maroni, P.; Koul, H.K. Oxidative stress in prostate cancer. Cancer Lett. 2009, 282, 125–136. [Google Scholar] [CrossRef] [PubMed]
- Shiota, M.; Yokomizo, A.; Naito, S. Oxidative stress and androgen receptor signaling in the development and progression of castration-resistant prostate cancer. Free Radic. Biol. Med. 2011, 51, 1320–1328. [Google Scholar] [CrossRef] [PubMed]
- Chaiswing, L.; Zhong, W.; Oberley, T.D. Distinct redox profiles of selected human prostate carcinoma cell lines: Implications of radiational design of redox therapy. Cancers 2011, 3, 3557–3584. [Google Scholar] [CrossRef] [PubMed]
- Mahon, K.L.; Henshall, S.M.; Sutherland, R.L.; Horvath, L.G. Pathways of chemotherapy resistance in castration-resistant prostate cancer. Endocr. Relat. Cancer 2011, 18, R103–R123. [Google Scholar] [CrossRef] [PubMed]
- Wartenberg, M.; Hoffmann, E.; Schwaindt, H.; Grünheck, F.; Petros, J.; Arnold, J.R.; Hescheler, J.; Sauer, H. Reactive oxygen species-linked regulation of the multidrug resistance transporter P-glycoprotein in Nox-1 overexpressing prostate tumor spheroids. FEBS Lett. 2005, 579, 4541–4549. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Ding, Z.; Peng, Y.; Pan, F.; Li, J.; Zou, L.; Zhang, Y.; Liang, H. HIF-1α inhibition reverses multidrug resistance in colon cancer cells via downregulation of MDR1/P-glycoprotein. PLoS ONE 2014, 9, e98882. [Google Scholar] [CrossRef] [PubMed]
- Wartenberg, M.; Richter, M.; Datchev, A.; Grünther, S.; Milosevic, N.; Bekhite, M.M.; Figulla, H.R.; Aran, J.M.; Pétriz, J.; Sauer, H. Glycolytic pyruvate regulates P-Glycoprotein expression in multicellular tumor spheroids via modulation of the intracellular redox state. J. Cell. Biochem. 2010, 109, 434–446. [Google Scholar] [CrossRef] [PubMed]
- Bitting, R.L.; Armstrong, A.J. Targeting the PI3K/Akt/mTOR pathway in castration-resistant prostate cancer. Endocr. Relat. Cancer 2013, 20, R83–R99. [Google Scholar] [CrossRef] [PubMed]
- Wu, L.; Birle, D.C.; Tannock, I.F. Effects of the mammalian target of rapamycin inhibitor CCI-779 used alone or with chemotherapy on human prostate cancer cells and xenografts. Cancer Res. 2005, 65, 2825–2831. [Google Scholar] [CrossRef] [PubMed]
- Hambright, H.G.; Meng, P.; Kumar, A.P.; Ghosh, R. Inhibition of PI3K/AKT/mTOR axis disrupts oxidative stress mediated survival of melanoma cells. Oncotarget 2015, 6, 7195–7208. [Google Scholar] [CrossRef] [PubMed]
- Hager, S.; Ackermann, C.J.; Joerger, M.; Gillessen, S.; Omlin, A. Anti-tumor activity of platinum compounds in advanced prostate cancer-a systematic literature review. Ann. Oncol. 2016, 27, 975–984. [Google Scholar] [CrossRef] [PubMed]
- Marullo, R.; Werner, E.; Degtyareva, N.; Moore, B.; Altavilla, G.; Ramalingam, S.S.; Doetsch, P.W. Cisplatin induces a mitochondrial-ROS response that contributes to cytotoxicity depending on mitochondrial redox status and bioenergetic functions. PLoS ONE 2013, 8, e81162. [Google Scholar] [CrossRef] [PubMed]
- Hervault, A.; Thanh, N.T. Magnetic nanoparticle-based therapeutic agents for thermo-chemotherapy treatment of cancer. Nanoscale 2014, 6, 11553–11573. [Google Scholar] [CrossRef] [PubMed]




| PC-3 | Sub-G1 | G0/G1 | S | G2 |
|---|---|---|---|---|
| Control | 3.3 ± 0.1 | 66.1 ± 0.3 | 8.0 ± 0.2 | 22.7 ± 0.3 |
| Fe3O4 NPs (1 g/mL) | 4.5 ± 0.2 | 68.2 ± 0.5 | 8.3 ± 0.1 | 19.0 ± 0.7 |
| Fe3O4 NPs (10 g/mL) | 5.1 ± 0.2 | 67.9 ± 0.5 | 8.4 ± 0.1 | 18.5 ± 0.6 |
| Fe3O4 NPs (100 g/mL) | 5.5 ± 0.1 | 68.7 ± 0.3 | 8.9 ± 0.2 | 16.9 ± 0.3 |
| DU145 | Sub-G1 | G0/G1 | S | G2 |
| Control | 0.5 ± 0.1 | 53.7 ± 0.3 | 5.1 ± 0.1 | 40.8 ± 0.4 |
| Fe3O4 NPs (1 g/mL) | 0.5 ± 0.1 | 52.3 ± 0.4 | 5.7 ± 0.1 | 41.4 ± 0.4 |
| Fe3O4 NPs (10 g/mL) | 0.5 ± 0.1 | 53.0 ± 0.2 | 5.8 ± 0.1 | 40.8 ± 0.3 |
| Fe3O4 NPs (100 g/mL) | 0.6 ± 0.1 | 50.9 ± 0.7 | 8.5 ± 0.4 | 40.0 ± 1.1 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kojima, K.; Takahashi, S.; Saito, S.; Endo, Y.; Nittami, T.; Nozaki, T.; Sobti, R.C.; Watanabe, M. Combined Effects of Fe3O4 Nanoparticles and Chemotherapeutic Agents on Prostate Cancer Cells In Vitro. Appl. Sci. 2018, 8, 134. https://doi.org/10.3390/app8010134
Kojima K, Takahashi S, Saito S, Endo Y, Nittami T, Nozaki T, Sobti RC, Watanabe M. Combined Effects of Fe3O4 Nanoparticles and Chemotherapeutic Agents on Prostate Cancer Cells In Vitro. Applied Sciences. 2018; 8(1):134. https://doi.org/10.3390/app8010134
Chicago/Turabian StyleKojima, Kanako, Sanai Takahashi, Shungo Saito, Yoshihiro Endo, Tadashi Nittami, Tadashige Nozaki, Ranbir Chander Sobti, and Masatoshi Watanabe. 2018. "Combined Effects of Fe3O4 Nanoparticles and Chemotherapeutic Agents on Prostate Cancer Cells In Vitro" Applied Sciences 8, no. 1: 134. https://doi.org/10.3390/app8010134






