Brief Treatment of Symptoms of Post-Traumatic Stress Disorder (PTSD) by Use of Accelerated Resolution Therapy (ART®)
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participant Inclusion and Exclusion
2.2. Recruitment
2.3. Therapist Training
2.4. Participant Intake Assessment
2.5. ART Protocol
2.6. Individual ART Sessions
2.7. Data Collection
2.8. Statistical Methods
3. Results
3.1. Screening and Enrollment

3.2. Demographic and Presenting Characteristics
| Characteristic | All (n = 80) | Male (n = 18) | Female (n = 62) | |
|---|---|---|---|---|
| Age in years (mean ± SD) | 40.0 ± 10.2 | 41.9 ± 11.8 | 40.6 ± 9.8 | |
| Race (%) | ||||
| Black or African American | 7.5 | 0.0 | 9.7 | |
| White | 88.8 | 94.4 | 87.1 | |
| Asian | 1.3 | 0.0 | 1.6 | |
| Native Hawaiian/Pacific Islander | 0.0 | 0.0 | 0.0 | |
| American Indian/Alaskan Native | 1.3 | 0.0 | 1.6 | |
| Not reported | 1.2 | 5.6 | 0.0 | |
| Hispanic (%) | 28.6 | 5.6 | 35.6 | |
| Married (%) | 58.8 | 61.1 | 58.1 | |
| Employed – full or part time (%) | 59.8 | 72.2 | 55.9 | |
| PDSQ score (mean ± SD) (T-score) | 53.7 ± 8.6 | 54.6 ± 8.6 | 53.5 ± 8.6 | |
| Less than 40 (%) | 2.5 | 0.0 | 3.2 | |
| 40 to 60 (%) | 75.0 | 77.8 | 74.2 | |
| More than 60 (%) | 22.5 | 22.2 | 22.6 | |
| PCL-C score (mean ± SD) | 54.5 ± 13.0 | 57.3 ± 14.3 | 53.7 ± 12.6 | |
| Less than 40 (%) | 13.8 | 11.1 | 14.5 | |
| 40 to 60 (%) | 47.5 | 38.9 | 50.0 | |
| More than 60 (%) | 38.8 | 50.0 | 35.5 | |
| No. of traumatic memories still impacting life (%) | ||||
| 1 to 2 | 19.0 | 23.57 | 17.7 | |
| 3 to 4 | 31.6 | 35.3 | 30.6 | |
| 5 or more | 49.4 | 41.2 | 51.6 | |
| Previous treatment for PTSD/other MH condition (%) | 67.9 | 50.0 | 73.3 | |
| On disability for PTSD or other MH disorder (%) | 10.1 | 5.9 | 11.3 | |
| Guilt associated with traumatic memory(ies) (%) | 81.3 | 88.9 | 79.0 | |
| Time lived with traumatic memory(ies) (%) | ||||
| Less than 1 year | 6.3 | 5.6 | 6.5 | |
| 1 to 6 years | 13.8 | 22.2 | 11.3 | |
| 7 years or more | 80.0 | 72.2 | 82.3 | |
3.3. Examination of Treatment Efficacy
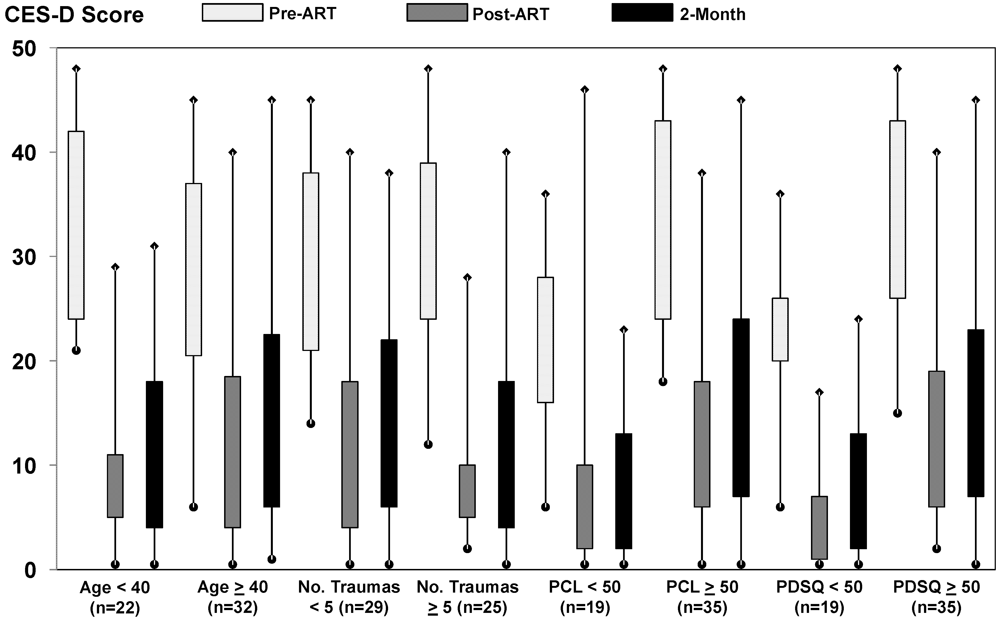
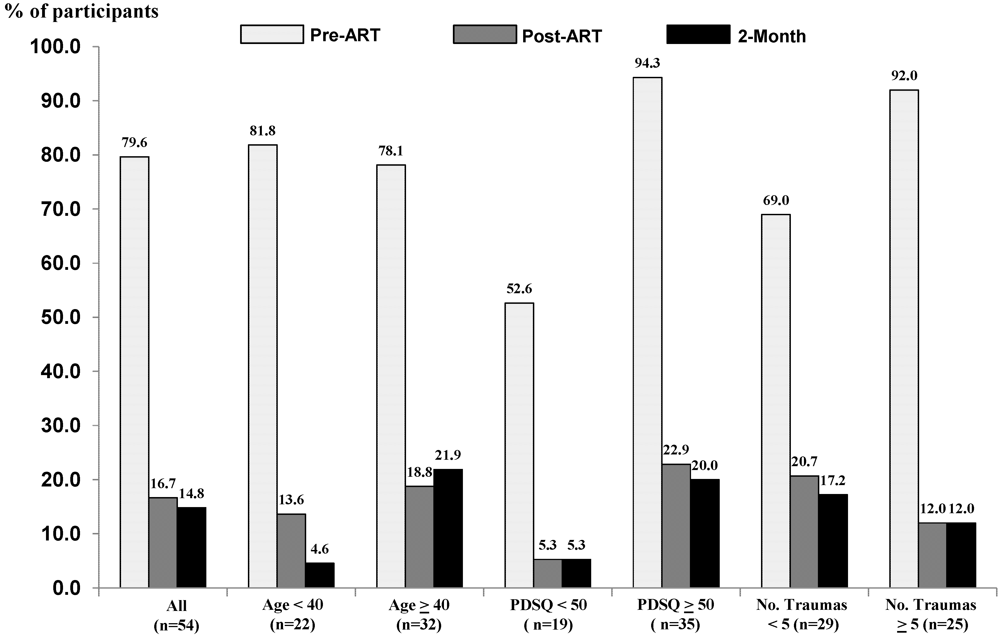
3.4. Subgroup Analyses
| Symptom Measure | Pre- Versus Post-Treatment | Pre-Treatment Versus 2-Month Follow-Up | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Pre a | Post a | Diff ab | ES | P | N | Pre a | 2-Mo. a | Diff ab | ES | P | |
| PTSD Checklist (PCL-C) | 54 | 54.5 (12.2) | 31.2 (11.4) | 22.8 (13.5) | 1.72 | <0.0001 | 54 | 54.5 (12.2) | 30.0 (12.4) | 24.5 (12.4) | 1.98 | <0.0001 |
| Brief Symptom Inventory | 52 | 30.8 (14.6) | 10.1 (10.8) | 20.8 (11.9) | 1.74 | <0.0001 | 54 | 30.7 (14.3) | 10.1 (12.1) | 20.7 (13.1) | 1.57 | <0.0001 |
| CES-D (Depression) | 54 | 29.5 (10.9) | 11.8 (11.1) | 17.7 (12.5) | 1.41 | <0.0001 | 54 | 29.5 (10.9) | 13.5 (12.1) | 16.0 (11.0) | 1.46 | <0.0001 |
| STICSA (Somatic) | 54 | 20.6 (6.9) | 13.8 (3.5) | 6.9 (6.2) | 1.11 | <0.0001 | 54 | 20.6 (6.9) | 14.9 (5.0) | 5.7 (5.2) | 1.10 | <0.0001 |
| STICSA (Cognitive) | 54 | 25.2 (6.6) | 15.5 (5.0) | 9.7 (6.0) | 1.62 | <0.0001 | 54 | 25.2 (6.6) | 17.5 (6.8) | 7.7 (6.8) | 1.14 | <0.0001 |
| Pittsburgh Sleep Quality | 46 | 9.2 (4.5) | 6.4 (4.4) | 2.4 (3.1) | 0.87 | <0.0001 | 45 | 9.3 (4.6) | 7.0 (4.6) | 2.4 (3.7) | 0.70 | <0.0001 |
| Trauma Related Growth | ||||||||||||
| Global Guilt | 54 | 4.7 (2.4) | 1.6 (1.9) | 3.1 (2.4) | 1.28 | <0.0001 | 54 | 4.7 (2.4) | 1.9 (2.0) | 2.8 (2.8) | 1.02 | <0.0001 |
| Distress | 54 | 18.9 (4.1) | 7.4 (5.9) | 11.2 (6.0) | 1.88 | <0.0001 | 54 | 18.9 (4.1) | 8.2 (5.9) | 10.7 (5.7) | 1.88 | <0.0001 |
| Guilt Cognition | 54 | 44.7 (18.6) | 24.1 (13.2) | 20.1 (17.1) | 1.17 | <0.0001 | 54 | 44.7 (18.6) | 24.5 (15.2) | 19.7 (19.0) | 1.04 | <0.0001 |
| Post-Traumatic Growth | ||||||||||||
| I:Relation to Others | 52 | 12.3 (6.9) | 17.0 (6.6) | 4.8 (4.4) | 0.89 | <0.0001 | 52 | 12.3 (6.9) | 15.3 (6.8) | 3.0 (4.9) | 0.66 | <0.0001 |
| II: New Possibilities | 52 | 12.7 (6.5) | 16.9 (6.6) | 4.4 (6.0) | 0.72 | <0.0001 | 52 | 12.7 (6.5) | 15.5 (7.2) | 2.8 (5.5) | 0.53 | 0.0009 |
| III: Personal Strength | 52 | 8.5 (5.4) | 11.8 (6.2) | 3.6 (5.5) | 0.63 | <0.0001 | 52 | 8.5 (5.4) | 11.6 (5.6) | 3.1 (4.6) | 0.69 | <0.0001 |
| IV: Spiritual Change | 52 | 5.3 (2.9) | 7.2 (2.6) | 2.0 (2.7) | 0.73 | <0.0001 | 52 | 5.3 (2.9) | 6.4 (3.0) | 1.1 (3.1) | 0.36 | 0.008 |
| V: Appreciation-Life | 52 | 7.8 (4.0) | 9.6 (4.2) | 2.8 (4.3) | 0.44 | 0.001 | 52 | 7.8 (4.0) | 9.3 (3.9) | 1.5 (4.0) | 0.39 | 0.009 |
| Self-Compassion Scale | 54 | 66.8 (16.8) | 84.4 (21.4) | 16.4 (19.9) | 0.82 | <0.0001 | 54 | 66.8 (16.8) | 81.7 (21.8) | 14.9 (17.8) | 0.84 | <0.0001 |
| Aggression Questionnaire | 54 | 77.2 (20.2) | 63.9 (20.1) | 13.2 (13.5) | 0.98 | <0.0001 | 54 | 77.2 (20.2) | 64.5 (21.0) | 12.7 (15.0) | 0.85 | <0.0001 |
| Alcohol Use (AUDIT) | 52 | 3.0 (3.3) | 2.5 (3.0) | 0.6 (1.8) | 0.26 | 0.03 | 54 | 2.9 (3.3) | 1.8 (2.1) | 1.1 (2.3) | 0.48 | 0.0008 |

3.5. Clinical Interpretation of Treatment Effects
3.6. Medications
3.7. Adverse Events
3.8. Sensitivity Analyses
4. Discussion
4.1. Summary of Findings
4.2. Possible Therapeutic Mechanism
4.3. Systemic Treatment Effects
4.4. Current Treatment Modalities
4.5. Strengths and Limitations
5. Conclusions
Acknowledgements
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed.; American Psychiatric Association: Washington, DC, USA, 2000. [Google Scholar]
- Kessler, R.C.; Sonnega, A.; Bromet, E.; Hughes, M.; Nelson, C.B. Posttraumatic stress disorder in the national comorbidity survey. Arch. Gen. Psychiatry 1995, 52, 1048–1060. [Google Scholar] [CrossRef]
- National Comorbidity Survey. NCS-R appendix tables: Table 1. Lifetime prevalence of DSM-IV/WMH-CIDI disorders by sex and cohort. Table 2. Twelve-month prevalence of DSM-IV/WMH-CIDI disorders by sex and cohort. Available online: http://www.hcp.med.harvard.edu/ncs/publications.php (accessed on June 15 2011).
- Tanielian, T.; Jaycox, L. Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery; RAND Corporation: Santa Monica, CA, USA, 2008. [Google Scholar]
- Kang, H.K.; Natelson, B.H.; Mahan, C.M.; Lee, K.Y.; Murphy, F.M. Post-traumatic stress disorder and chronic fatigue syndrome-like illness among Gulf War veterans: A population-based survey of 30,000 veterans. Am. J. Epidemiol. 2003, 157, 141–148. [Google Scholar] [CrossRef]
- Kulka, R.A.; Schlenger, W.A.; Fairbanks, J.A.; Hough, R.L.; Jordan, B.K.; Marmar, C.R.; Cranston, A.S. Trauma and the Vietnam War Generation: Report of Findings from the National Vietnam Veterans Readjustment Study; Brunner Mazel Publishers: New York, NY, USA, 1990. [Google Scholar]
- Bisson, J.I. Post-traumatic stress disorder. BMJ 2007, 334, 789–793. [Google Scholar] [CrossRef]
- Davidson, J.R.T.; Foa, E.B. Posttraumatic Stress Disorder: DSM-IV and Beyond; American Psychiatric Press: Washington, DC, USA, 1993. [Google Scholar]
- Hoge, C.W.; Terhakopian, A.; Castro, C.A.; Messer, S.C.; Engel, C.C. Association of posttraumatic stress disorder with somatic symptoms, health care visits, and absenteeism among Iraq war veterans. Am. J. Psychiatry 2007, 164, 150–153. [Google Scholar]
- VA National Center for PTSD. Relationships and PTSD. Available online: http://www.ptsd.va.gov/public/pages/ptsd-and-relationships.asp (accessed on June 15 2011).
- Oquendo, M.A.; Friend, J.M.; Halberstam, B.; Brodsky, B.S.; Burke, A.K.; Grunebaum, M.F.; Malone, K.M.; Mann, J.J. Association of comorbid posttraumatic stress disorder and major depression with greater risk for suicidal behavior. Am. J. Psychiatry 2003, 160, 580–582. [Google Scholar] [CrossRef]
- Foa, E.B.; Keane, T.M.; Friedman, M.J. Effective Treatments for PTSD: Practice Guidelines from the International Society for Traumatic Stress Studies; Guilford: New York, NY, USA, 2009. [Google Scholar]
- Institute of Medicine. Treatment of Posttraumatic Stress Disorder: An Assessment of the Evidence; Institute of Medicine: Washington, DC, USA, 2008. [Google Scholar]
- Ursano, R.J.; Bell, C.; Eth, S.; Friedman, M.J.; Norwood, A.E.; Pfefferbaum, B. Practice guideline for the treatment of patients with acute stress disorder and posttraumatic stress disorder. Am. J. Psychiatry 2004, 161, 3–31. [Google Scholar]
- Resick, P.A.; Schnicke, M.K. Cognitive Processing Therapy for Rape Victims: A Treatment Manual; Sage Publications: Newbury Park, CA, USA, 1996. [Google Scholar]
- Foa, E.B.; Rothbaum, B.O. Treating the Trauma of Rape: Cognitive Behavioral Therapy for PTSD; Guilford: New York, NY, USA, 1998. [Google Scholar]
- Chemtob, C.M.; Tolin, D.F.; van der Kolk, B.; Pitman, R.K. Eye Movement Desensitization and Reprocessing; Guilford: New York, NY, USA, 2000. [Google Scholar]
- Shapiro, F. Eye Movement Desensitization and Reprocessing: Basic Principles, Protocols and Procedures, 2nd ed.; Guilford: New York, NY, USA, 2001. [Google Scholar]
- Brady, K.; Pearlstein, T.; Asnis, G.M.; Baker, D.; Rothbaum, B.; Sikes, C.R.; Farfel, G.M. Efficacy and safety of sertraline treatment of posttraumatic stress disorder: A randomized controlled trial. J. Am. Med. Assoc. 2000, 283, 1837–1844. [Google Scholar]
- VA National Center for PTSD. Clinicians Guide to Medications for PTSD. Available online: http://www.ptsd.va.gov/professional/pages/clinicians-guide-to-medications-for-ptsd.asp (accessed on January 18 2012).
- Blanchard, E.B.; Jones-Alexander, J.; Buckley, T.C.; Forneris, C.A. Psychometric properties of the PTSD checklist (PCL). Behav. Res. Ther. 1996, 34, 669–673. [Google Scholar] [CrossRef]
- Weathers, F.; Litz, B.; Herman, D.; Huska, J.; Keane, T. The PTSD Checklist (PCL): Reliability, Validity, and Diagnostic Utility. In Paper presented at the Annual Convention of the International Society for Traumatic Stress Studies, San Antonio, TX, USA, 24–27 October 1993.
- Zimmerman, M.; Chelminski, I. A scale to screen for DSM-IV Axis I disorders in psychiatric out-patients: Performance of the Psychiatric Diagnostic Screening Questionnaire. Psychol. Med. 2006, 36, 1601–1611. [Google Scholar] [CrossRef]
- Zimmerman, M.; Mattia, J.I. A self-report scale to help make psychiatric diagnoses: The Psychiatric Diagnostic Screening Questionnaire. Arch. Gen. Psychiatry 2001, 58, 787–794. [Google Scholar] [CrossRef]
- Stickgold, R.A. EMDR: A putative neurobiological mechanism of action. J. Clin. Psychol. 2002, 58, 61–75. [Google Scholar] [CrossRef]
- Holmes, E.A.; Arntz, A.; Smucker, M.R. Imagery rescripting in cognitive behaviour therapy: Images, treatment techniques and outcomes. J. Behav. Ther. Exp. Psychiatry 2007, 38, 297–305. [Google Scholar] [CrossRef]
- Grunert, B.K.; Weis, J.M.; Smucker, M.R.; Christianson, H. Imagery rescripting and reprocessing therapy after failed prolonged imaginal exposure for posttraumatic stress disorder following industrial injury. J. Behav. Ther. Exp. Psychiatry 2007, 38, 317–328. [Google Scholar]
- Derogatis, L.R. Brief Symptom Inventory (BSI)-18. Administration, scoring and procedures manual. NCS Pearson Inc.: Minneapolis, MN, 2001. Available online: http://psychcorp.pearsonassessments.com/HAIWEB/Cultures/enus/Productdetail.htm?Pid=PAg110&Mode=summary (accessed on June 13,2012).
- Radloff, L.S. The CES-D scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Ree, M.J.; French, D.; MacLeod, C.; Locke, V. Distinguishing cognitive and somatic dimensions of state and trait anxiety: Development and validation of the state-trait inventory for cognitive and somatic anxiety (STICSA). Behav. Cogn. Psychother. 2008, 36, 313–332. [Google Scholar]
- Neff, K.D. The development and validation of a scale to measure self-compassion. Self Identity 2003, 2, 223–250. [Google Scholar] [CrossRef]
- Buss, A.H.; Perry, M. The aggression questionnaire. J. Pers. Soc. Psychol. 1992, 63, 452–459. [Google Scholar] [CrossRef]
- Saunders, J.B.; Aasland, O.G.; Babor, T.F.; de la Fuente, J.R.; Grant, M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption–II. Addiction 1993, 88, 791–804. [Google Scholar] [CrossRef]
- Kubany, E.S. Development and validation of the Trauma-Related Guilt Inventory (TRGI). Psychol. Assess. 1996, 8, 428–444. [Google Scholar] [CrossRef]
- Tedeschi, R.G.; Calhoun, L.G. The posttraumatic growth inventory: Measuring the positive legacy of trauma. J. Trauma. Stress 1996, 9, 455–471. [Google Scholar] [CrossRef]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatr. Resid. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Morris, S.B.; DeShon, R.P. Combining effect size estimates in meta-analysis with repeated measures and independent-groups designs. Psychol. Methods 2002, 7, 105–125. [Google Scholar] [CrossRef]
- Grubaugh, A.L.; Elhai, J.D.; Cusack, K.J.; Wells, C.; Frueh, B.C. Screening for PTSD in public-sector mental health settings: The diagnostic utility of the PTSD checklist. Depress. Anxiety 2007, 24, 124–129. [Google Scholar] [CrossRef]
- McDowell, I.; Newell, C. Measuring Health, a Guide to Rating Scales and Questionnaires, 2nd ed.; Oxford University Press: New York, NY, USA, 1996. [Google Scholar]
- Monson, C.M.; Gradus, J.L.; Young-Xu, Y.; Schnurr, P.P.; Price, J.L.; Schumm, J.A. Change in posttraumatic stress disorder symptoms: Do clinicians and patients agree? Psychol. Assess. 2008, 20, 131–138. [Google Scholar] [CrossRef]
- Andrade, J.; Kavanagh, D.; Baddeley, A. Eye movements and visual imagery: A working memory approach to the treatment of post-traumatic stress disorder. Br. J. Clin. Psychol. 1997, 36, 209–233. [Google Scholar] [CrossRef]
- van den Hout, M.; Muris, P.; Salemink, E.; Kindt, M. Autobiographical memories become less vivid and emotional after eye movements. Br. J. Clin. Psychol. 2001, 40, 121–130. [Google Scholar] [CrossRef]
- Lee, C.W.; Taylor, G.; Drummond, P.D. The active ingredient in EMDR: Is it traditional exposure or dual focus of attention? Clin. Psychol. Psychother. 2006, 13, 97–107. [Google Scholar] [CrossRef]
- Christman, S.D.; Garvey, K.J.; Proper, R.E.; Phaneuf, K.A. Bilateral eye movements enhance the retrieval of episodic memories. Neuropsychology 2003, 17, 221–229. [Google Scholar] [CrossRef]
- Sacka, M.; Lempa, W.; Steinmetz, A.; Lamprecht, F.; Hofmann, A. Alterations in autonomic tone during trauma exposure using eye movement desensitization and reprocessing (EMDR)–Results of a preliminary investigation. J. Anxiety Disord. 2008, 22, 1264–1271. [Google Scholar] [CrossRef]
- MacCulloch, M.J.; Feldman, P. Eye movement desensitization treatment utilizes the positive visceral element of the investigatory reflex to inhibit the memories of post-traumatic stress disorder: A theoretical analysis. Br. J. Psychiatry 1996, 169, 571–579. [Google Scholar] [CrossRef]
- Foa, E.B.; Kozak, M.J. Emotional processing of fear: Exposure to corrective information. Psychol. Bull. 1986, 99, 20–35. [Google Scholar] [CrossRef]
- Paller, K.A.; Voss, J.L. Memory reactivation and consolidation during sleep. Learn. Mem. 2004, 11, 664–670. [Google Scholar] [CrossRef]
- Wagner, U.; Gais, S.; Born, J. Emotional memory formation is enhanced across sleep intervals with high amounts of rapid eye movement sleep. Learn. Mem. 2001, 8, 112–119. [Google Scholar]
- Datta, S. Avoidance task training potentiates phasic pontine-wave density in the rat: A mechanism for sleep-dependent plasticity. J. Neurosci. 2000, 20, 8607–8613. [Google Scholar]
- Walker, M.P.; Stickgold, R. Sleep, memory and plasticity. Annu. Rev. Psychol. 2006, 57, 139–166. [Google Scholar] [CrossRef]
- Seidler, G.H.; Wagner, F.E. Comparing the efficacy of EMDR and trauma-focused cognitive-behavioral therapy in the treatment of PTSD: A meta-analytic study. Psychol. Med. 2006, 36, 1515–1522. [Google Scholar] [CrossRef]
- Bryant, R.A.; Moulds, M.L.; Guthrie, R.M.; Dang, S.T.; Nixon, R.D.V. Imaginal exposure alone and imaginal exposure with cognitive restructuring in treatment of posttraumatic stress disorder. J. Consult. Clin. Psychol. 2003, 71, 706–712. [Google Scholar] [CrossRef]
- Foa, E.B.; Dancu, C.V.; Hembree, E.A.; Jaycox, L.H.; Meadows, E.A.; Street, G.P. A comparison of exposure therapy, stress inoculation training, and their combination for reducing posttraumatic stress disorder in female assault victims. J. Consult. Clin. Psychol. 1999, 67, 194–200. [Google Scholar] [CrossRef]
- Marks, I.; Lovell, K.; Noshirvani, H.; Livanou, M.; Thrasher, S. Treatment of posttraumatic stress disorder by exposure and/or cognitive restructuring. Arch. Gen. Psychiatry 1998, 55, 317–324. [Google Scholar] [CrossRef]
- Resick, P.A.; Nishith, P.; Weaver, T.L.; Astin, M.C.; Feuer, C.A. A comparison of cognitive-processing therapy with prolonged exposure and a waiting condition for the treatment of chronic posttraumatic stress disorder in female rape victims. J. Consult. Clin. Psychology 2002, 70, 867–879. [Google Scholar] [CrossRef]
- Rothbaum, B.O.; Astin, M.C.; Marsteller, F. Prolonged exposure versus eye movement desensitization and reprocessing (EMDR) for PTSD rape victims. J. Trauma. Stress 2005, 18, 607–616. [Google Scholar] [CrossRef]
- Taylor, S.; Thordarson, D.S.; Maxfield, L.; Fedoroff, I.C.; Lovell, K.; Ogrodniczuk, J.S. Comparative efficacy, speed, and adverse effects of three PTSD treatments: Exposure therapy, EMDR, and relaxation training. J. Consult. Clin. Psychol. 2003, 71, 330–338. [Google Scholar] [CrossRef]
- Schnurr, P.P.; Friedman, M.J.; Engel, C.C.; Foa, E.B.; Shea, M.T.; Chow, B.K.; Resick, P.A.; Thurston, V.; Orsillo, S.M.; Haug, R.; et al. Cognitive behavioral therapy for posttraumatic stress disorder in women. A randomized controlled trial. J. Am. Med. Assoc. 2007, 297, 820–830. [Google Scholar]
© 2012 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Kip, K.E.; Elk, C.A.; Sullivan, K.L.; Kadel, R.; Lengacher, C.A.; Long, C.J.; Rosenzweig, L.; Shuman, A.; Hernandez, D.F.; Street, J.D.; et al. Brief Treatment of Symptoms of Post-Traumatic Stress Disorder (PTSD) by Use of Accelerated Resolution Therapy (ART®). Behav. Sci. 2012, 2, 115-134. https://doi.org/10.3390/bs2020115
Kip KE, Elk CA, Sullivan KL, Kadel R, Lengacher CA, Long CJ, Rosenzweig L, Shuman A, Hernandez DF, Street JD, et al. Brief Treatment of Symptoms of Post-Traumatic Stress Disorder (PTSD) by Use of Accelerated Resolution Therapy (ART®). Behavioral Sciences. 2012; 2(2):115-134. https://doi.org/10.3390/bs2020115
Chicago/Turabian StyleKip, Kevin E., Carrie A. Elk, Kelly L. Sullivan, Rajendra Kadel, Cecile A. Lengacher, Christopher J. Long, Laney Rosenzweig, Amy Shuman, Diego F. Hernandez, Jennifer D. Street, and et al. 2012. "Brief Treatment of Symptoms of Post-Traumatic Stress Disorder (PTSD) by Use of Accelerated Resolution Therapy (ART®)" Behavioral Sciences 2, no. 2: 115-134. https://doi.org/10.3390/bs2020115




