One Medicine, One Acupuncture
Abstract
:Simple Summary
Abstract
1. Introduction
2. Opening Communication Channels
3. Promoting Safety with a “One Acupuncture” Framework
4. Science as the Foundation for One Acupuncture
5. How Does Needling Influence Nerves?
6. Acupuncture Effects and the Central Nervous System
7. Sources of Confusion in Traditional Chinese Veterinary Medical (TCVM) Point Locations


8. Additional Veterinary Acupuncture Points in Question
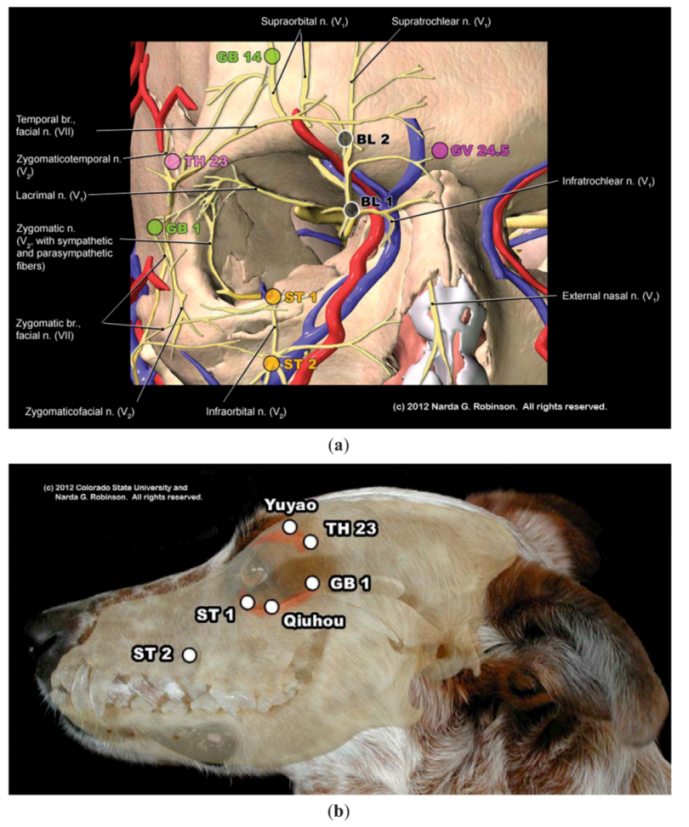
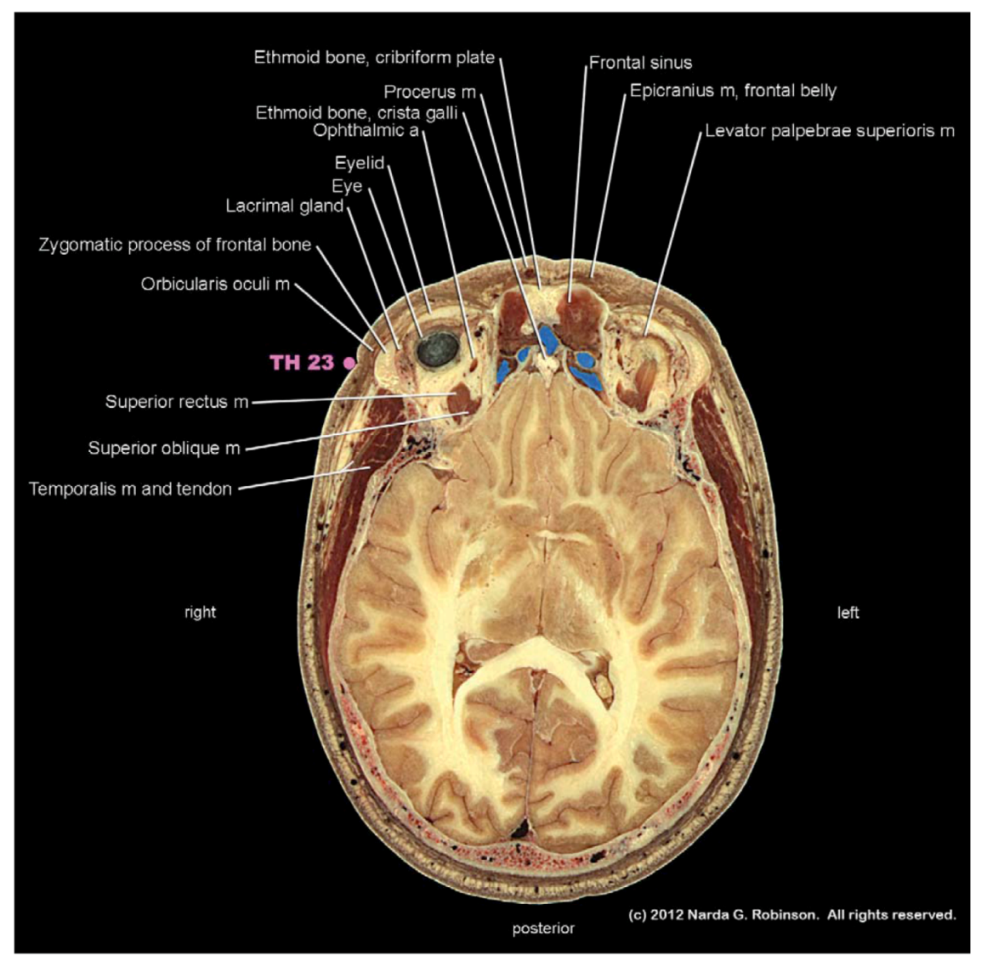
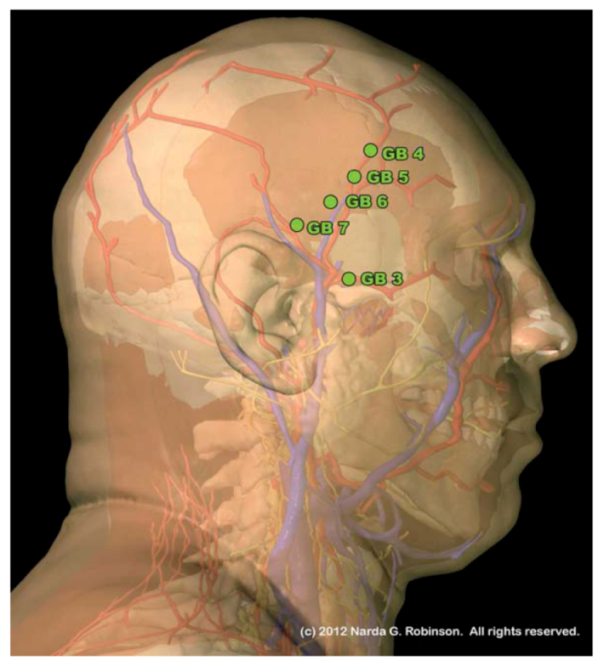
8.1. Head
8.1.1. Maxilla
8.1.2. Temporal Fossa
8.1.3. Ear
8.2. Axial Skeleton
8.2.1. Comparative Anatomy of the Spine
8.2.2. Neck
8.2.3. Back
8.2.4. Tail
8.2.5. Mammae
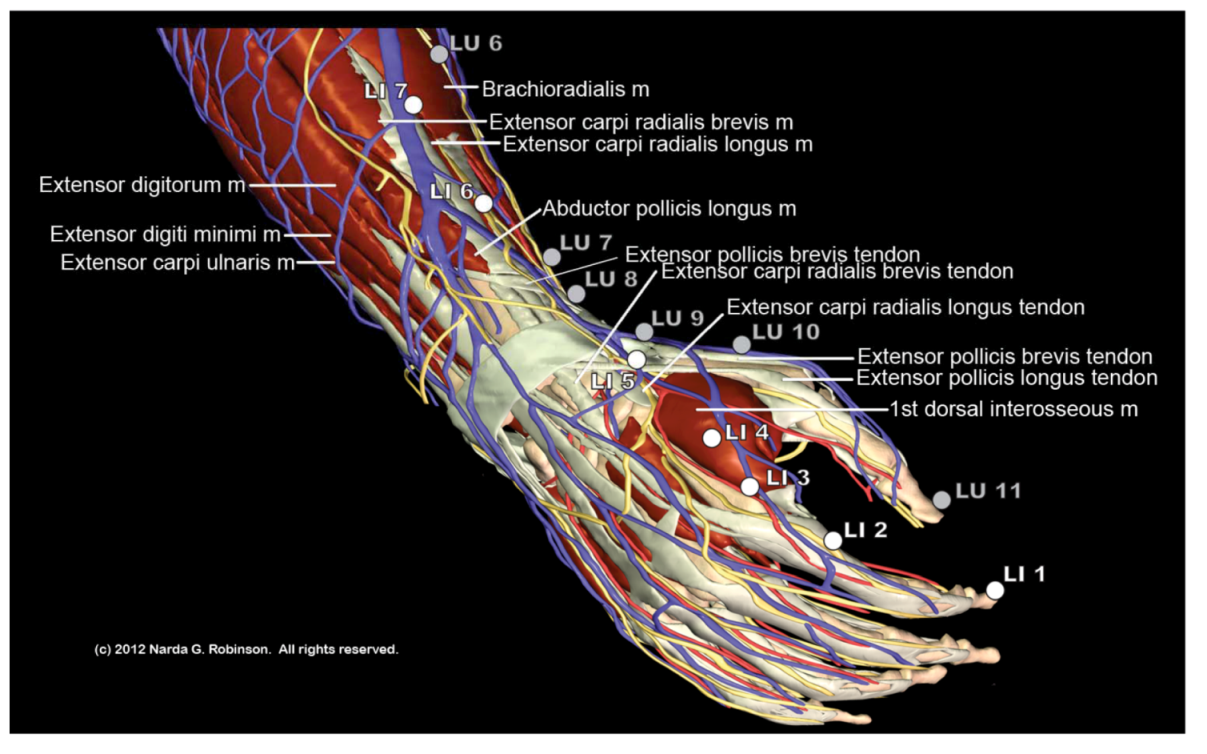
8.3. Appendicular Skeleton
8.3.1. Thoracic and Pelvic Limbs
8.4. Myofascial Trigger Points
9. Conclusions
Acknowledgments
Conflict of Interest
References
- Panzer, R.B. A comparison of the traditional Chinese versus transpositional Zangfu organ association acupoint locations in the horse. Am. J. Chin. Med. 1993, 21, 119–131. [Google Scholar] [CrossRef]
- Klauder, J.V. Interrelations of human and veterinary medicine. N. Engl. J. Med. 1958, 258, 170–177. [Google Scholar] [CrossRef]
- King, L.J.; Anderson, L.R.; Blackmore, C.G.; Blackwell, M.J.; Lautner, E.A.; Marcus, L.C.; Meyer, T.E.; Monath, T.P.; Nave, J.E.; Ohle, J.; Pappaioanou, M.; Sobota, J.; Stokes, W.S.; Davis, R.M.; Glaser, J.H.; and Mahr, R.K. Executive summary of the AVMA One Health Initiative Task Force report. J. Am. Vet. Med. Assoc. 2008, 233, 259–261. [Google Scholar] [CrossRef]
- Atlas, R.M. One health: Its origins and future. Curr. Top. Microbiol. Immunol. 2012. [Google Scholar] [CrossRef]
- Leung, Z.; Middleton, D.; Morrison, K. One Health and EcoHealth in Ontario: A qualitative study exploring how holistic and integrative approaches are shaping public health practice in Ontario. BMC Publ. Health 2012, 12. [Google Scholar]
- One Health: A New Professional Imperative. 15 July 2008. Available online: http://www.avma.org/onehealth/onehealth_final.pdf (accessed on 16 June 2012).
- Hayashi, A.; Matera, J.M.; Fonseca Pinto, A.C. Evaluation of electroacupuncture treatment for thoracolumbar intervertebral disk disease in dogs. J. Am. Vet. Med. Assoc. 2007, 231, 913–918. [Google Scholar] [CrossRef]
- Laim, A.; Jaggy, A.; Forterre, F.; Doherr, M.G.; Aeschbacher, G.; Glardon, O. Effects of adjunct electroacupuncture on severity of postoperative pain in dogs undergoing hemilaminectomy because of acute thoracolumbar intervertebral disk disease. J. Am. Vet. Med. Assoc. 2009, 234, 1141–1146. [Google Scholar] [CrossRef]
- Joaquim, J.G.; Luna, S.P.; Brondani, J.T.; Torelli, S.R.; Rahal, S.C.; de Paula Freitas, F. Comparison of decompressive surgery, electroacupuncture, and decompressive surgery followed by electroacupuncture for the treatment of dogs with intervertebral disk disease with long-standing severe neurologic deficits. J. Am. Vet. Med. Assoc. 2010, 236, 1225–1229. [Google Scholar] [CrossRef]
- Mayo, E. Acupuncture and wound healing. AJTCVM 2012, 7, 45–51. [Google Scholar]
- Gerard, P.S. Images in clinical medicine: Acupuncture-like fragments. NEJM 1995, 332, 1792–1794. [Google Scholar] [CrossRef]
- Imray, T.J.; Hiramatsu, Y. Radiographic manifestations of Japanese acupuncture. Radiology 1975, 115, 625–626. [Google Scholar]
- Robinson, N.G. Gold bead implants—Medicine or Malpractice? Available online: http://csuvets.colostate.edu/pain/Articlespdf/GoldBeadImplants.pdf (accessed on 11 August 2012).
- MacPherson, H. Fatal and adverse events from acupuncture: Allegation, evidence, and the implications. J. Altern. Complement. Med. 1999, 5, 47–56. [Google Scholar] [CrossRef]
- Von Riedenauer, W.B.; Baker, M.K.; Brewer, R.J. Video-assisted thorascopic removal of migratory acupuncture needle causing pneumothorax. Chest 2007, 131, 899–901. [Google Scholar] [CrossRef]
- Yokogushi, K. Embedded needles in acupuncture: Case report and review of the literature. Available online: http://www.medicalacupuncture.org/aama_marf/journal/vol15_3/case4.html (accessed on 29 July 2007).
- Robinson, N.G. Interactive Medical Acupuncture Anatomy; Teton NewMedia: Jackson, WY, USA, to be published in 2013.
- Wang, S.-M.; Kain, Z.N.; White, P.F. Acupuncture analgesia: II. Clinical considerations. Acupunct. Analg. 2008, 106, 611–621. [Google Scholar]
- Takahashi, T. Mechanism of acupuncture on neuromodulation in the gut—A review. Neuromodulation 2011, 14, 8–12. [Google Scholar] [CrossRef]
- White, A. Editorial board of acupuncture in medicine. Western medical acupuncture: A definition. Acupunct. Med. 2009, 27, 33–35. [Google Scholar] [CrossRef]
- Lindley, S.; Cummings, T.M. Chapter 3. Acupuncture—What Is It and How Does It Work? In Essentials of Western Veterinary Acupuncture; Blackwell Publishing: Ames, IA, USA, 2006; pp. 33–44. [Google Scholar]
- Zhang, Z.-J.; Wang, X.-M.; McAlonan, G.M. Neural acupuncture unit: A new concept for interpreting effects and mechanisms of acupuncture. Pflugers Arch. 2011, 462, 645–653. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhang, R.X.; Zhang, M.; Shen, X.Y.; Li, A.; Xin, J.; Ren, K.; Berman, B.M.; Tan, M.; Lao, L. Electroacupuncture inhibition of hyperalgesia in an inflammatory pain rat model: Involvement of distinct spinal serotonin and norepinephrine receptors subtypes. Br. J. Anaesth. 2012, 109, 245–252. [Google Scholar] [CrossRef]
- Leung, A.Y.; Kim, S.J.; Schulteis, G.; Yaksh, T. The effect of acupuncture duration on analgesia and peripheral sensory thresholds. BMC Complement. Altern. Med. 2008, 8. [Google Scholar]
- Chae, Y.; Lee, H.; Kim, H. The neural substrates of verum acupuncture compared to non-penetrating placebo needle: An fMRI study. Neurosci. Lett. 2009, 450, 80–84. [Google Scholar] [CrossRef]
- Zeng, F.; Qin, W.; Ma, T.; Sun, J.; Tang, Y.; Yuan, K.; Li, Y.; Liu, J.; Liu, X.; Song, W.; et al. Influence of acupuncture treatment on cerebral activity in functional dyspepsia patients and its relationship with efficacy. Am. J. Gastroenterol. 2012. [Google Scholar]
- Li, J.; Li, J.; Chen, Z.; Liang, F.; Wu, S.; Wang, H. The influence of PC6 on cardiovascular disorders: A review of central neural mechanisms. Acupunct. Med. 2012, 30, 47–50. [Google Scholar] [CrossRef]
- Beissner, F.; Deichmann, R.; Henke, C.; Bär, K.J. Acupuncture—Deep pain with an autonomic dimension? Neuroimage 2012, 60, 653–660. [Google Scholar] [CrossRef]
- Schippers, R. Some Aspects of Horse Acupuncture in China in the Middle Ages. Argos 1994, 10, 326. [Google Scholar]
- Skarda, R.T.; Muir, W.W. Comparison of electroacupuncture and butorphanol on respiratory and cardiovascular effects and rectal pain threshold after controlled rectal distention in mares. Am. J. Vet. Res. 2003, 64, 137–144. [Google Scholar] [CrossRef]
- Xie, H.; Colahan, P.; Ott, E.A. Evaluation of electroacupuncture treatment of horses with signs of chronic thoracolumbar pain. J. Am. Vet. Med. Assoc. 2005, 227, 281–286. [Google Scholar] [CrossRef]
- Jaiswal, S.; Kumar, A. Clinico-Biochemical effects of electroacupuncture in goats. Indian J. Vet. Surg. 2005, 26, 25–27. [Google Scholar]
- Rungsri, P.; Trinarong, C.; Rojanasthien, S.; Xie, H.S.; Piransan, U. The effectiveness of electro-acupuncture on pain threshold in sport horses with back pain. AJTCVM 2009, 4, 22–26. [Google Scholar]
- Lee, S.E.; Seo, J.M.; Liu, J.Z.; Hong, M.-S.; Lee, Y.-W.; Lee, J.-Y.; Song, K.-H.; Kim, D.-H. The comparison on changes of the body heats in electroacupuncture analgesia and anesthesia by ketamine hydrochloride in dogs. Am. J. Chin. Med. 2006, 34, 69–76. [Google Scholar] [CrossRef]
- Kim, D.H.; Cho, S.H.; Song, K.H.; Lee, S.-E.; Lee, S.-H.; Kwon, G.-O.; Kim, I.-B.; Kim, Y.-C.; Cho, J.-H.; Kwon, Y.-Y.; et al. Electroacupuncture analgesia for surgery in cattle. Am. J. Chin. Med. 2004, 32, 131–140. [Google Scholar] [CrossRef]
- Xie, H.; Preast, V. Xie’s Veterinary Acupuncture; Blackwell Publishing: Ames, IA, USA, 2007; pp. 98–100. [Google Scholar]
- Travagli, R.A.; Hermann, G.E.; Browning, K.N.; Rogers, R.C. Brainstem circuits regulating gastric function. Annu. Rev. Physiol. 2006, 68, 279–305. [Google Scholar] [CrossRef]
- Xie, H.; Preast, V. Xie’s Veterinary Acupuncture; Blackwell Publishing: Ames, IA, USA, 2007; p. 34. [Google Scholar]
- Takayama, S.; Seki, T.; Nakazawa, T.; Aizawa, N.; Takahashi, S.; Watanabe, M.; Izumi, M.; Kaneko, S.; Kamiya, T.; Matsuda, A.; et al. Short-term effects of acupuncture on open-angle glaucoma in retrobulbar circulation: additional therapy to standard medication. Evid. Based Complement. Altern. Med. 2011. [Google Scholar]
- Frank, B.L.; Soliman, N. Shen Men: A critical assessment through advanced auricular therapy. Med. Acupunct. 1998. Available online: http://www.medicalacupuncture.org/aama_marf/journal/vol10_2/shenmen.html (accessed on 21 June 2012).
- He, W.; Rong, P.-J.; Li, L.; Ben, H; Zhu, B; Litscher, G. Auricular acupuncture may suppress epileptic seizures via activating the parasympathetic nervous system: A hypothesis based on innovative methods. Evid. Based Complement. Altern. Med. 2012. [Google Scholar]
- Lee, S.-E.; Song, K.-H.; Liu, J.; Kwon, H.J.; Youn, S.B.; Lee, Y.W.; Cho, S.H.; Kim, D.H. The effectiveness of auriculoacupoint treatment for artificially induced acute hepatic injury in dogs. Am. J. Chin. Med. 2004, 32, 445–451. [Google Scholar] [CrossRef]
- Still, J. A clinical study of auriculotherapy in canine thoracolumbar disc disease. J. S. Afr. Vet. Assoc. 1990, 61, 102–105. [Google Scholar]
- Panzer, R.B.; Chrisman, C.L. An auricular acupuncture treatment for idiopathic canine epilepsy: A preliminary report. Am. J. Chin. Med. 1994, 22, 11–17. [Google Scholar] [CrossRef]
- Xie, H.; Preast, V. Xie’s Veterinary Acupuncture; Blackwell Publishing: Ames, IA, USA, 2007; p. 80. [Google Scholar]
- Thoresen, A.S. Outcome of horses with sarcoids treated with acupuncture at a single Ting point: 18 cases (1995–2009). AJTCVM 2011, 6, 29–35. [Google Scholar]
- Kim, D.H.; Liu, J.Z.; Lee, J.Y.; MacManus, P.; Jennings, P.; Darcy, K.; Burke, F.; Rogers, P.A.M. Acupuncture treatment of torticollis in a foal. Korean J. Vet. Res. 2006, 46, 43–46. [Google Scholar]
- Janssens, L.A.A. Trigger points in 48 dogs with myofascial pain syndromes. 1991, 20, 274–278. [Google Scholar]
- Simons, D.G.; Travell, J.G.; Simons, L.S. Travell & Simons’ Myofascial Pain and Dysfunction: The Trigger Point Manual, Volume 1 Upper Half of Body, 2nd ed.; Williams & Wilkins: Baltimore, MD, USA, 1999. [Google Scholar]
- Meagher, J. Beating Muscle Injuries for Horses; Hamilton Horse Associates: Hamilton, MA, USA, 1985. [Google Scholar]
- Macgregor, J.; von Schweinitz, D.G. Needle electromyographic activity of myofascial trigger points and control sites in equine cleidobrachialis muscle—An observational study. Acupunct. Med. 2006, 24, 61–70. [Google Scholar] [CrossRef]
- Rungsri, P.; Trinarong, C.; Rojanasthien, S.; Xie, H.; Pirunsan, U. The effectiveness of electro-acupuncture on pain threshold in sport horses with back pain. Am. J. Trad. Chin. Vet. Med. 2009, 4, 22–26. [Google Scholar]
- Frank, E.M. Myofascial Trigger Points and Acupuncture. In Proceedings of the 32nd World Small Animal Veterinary Association Congress, Darling Harbour, Australia, 19–23 August 2007.
- Melzack, R.; Stillwell, D.M.; Fox, E.J. Trigger points and acupuncture points for pain: Correlations and implications. Pain 1977, 3, 3–23. [Google Scholar] [CrossRef]
- Janssens, L.A.A. Trigger Point Therapy. In Veterinary Acupuncture: Ancient Art to Modern Medicine, 2nd ed.; Schoen, A.M., Ed.; Mosby, Inc.: St. Louis, MI, USA, 2001; pp. 199–203. [Google Scholar]
- Mackley, R.J. The role of trigger points in the management of head, neck, and face pain. Funct. Orthod. 1990, 7, 4–14. [Google Scholar]
© 2012 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Robinson, N.G. One Medicine, One Acupuncture. Animals 2012, 2, 395-414. https://doi.org/10.3390/ani2030395
Robinson NG. One Medicine, One Acupuncture. Animals. 2012; 2(3):395-414. https://doi.org/10.3390/ani2030395
Chicago/Turabian StyleRobinson, Narda G. 2012. "One Medicine, One Acupuncture" Animals 2, no. 3: 395-414. https://doi.org/10.3390/ani2030395



