Measuring the Temperature Increase of an Ultrasonic Motor in a 3-Tesla Magnetic Resonance Imaging System
Abstract
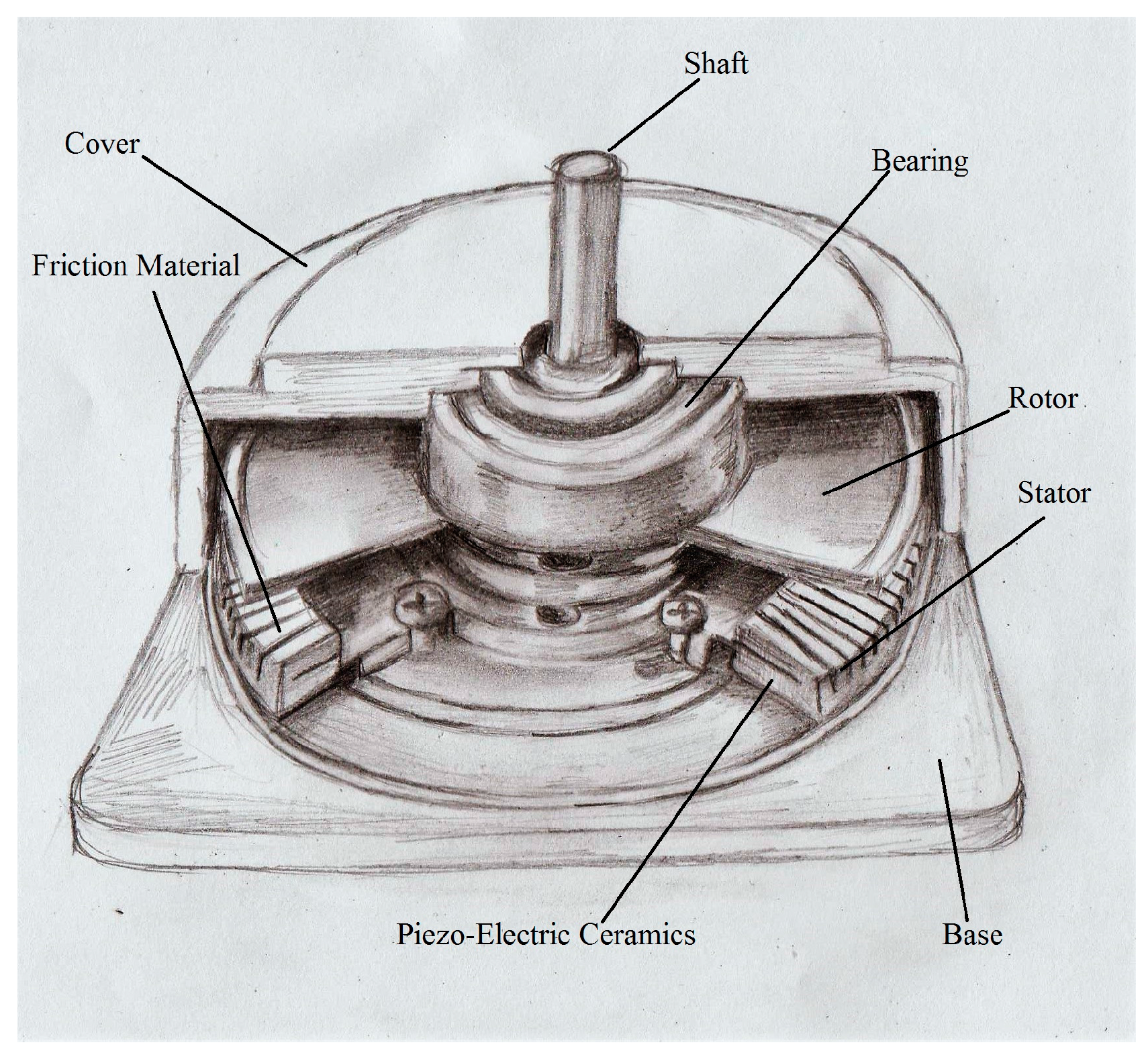
:1. Introduction
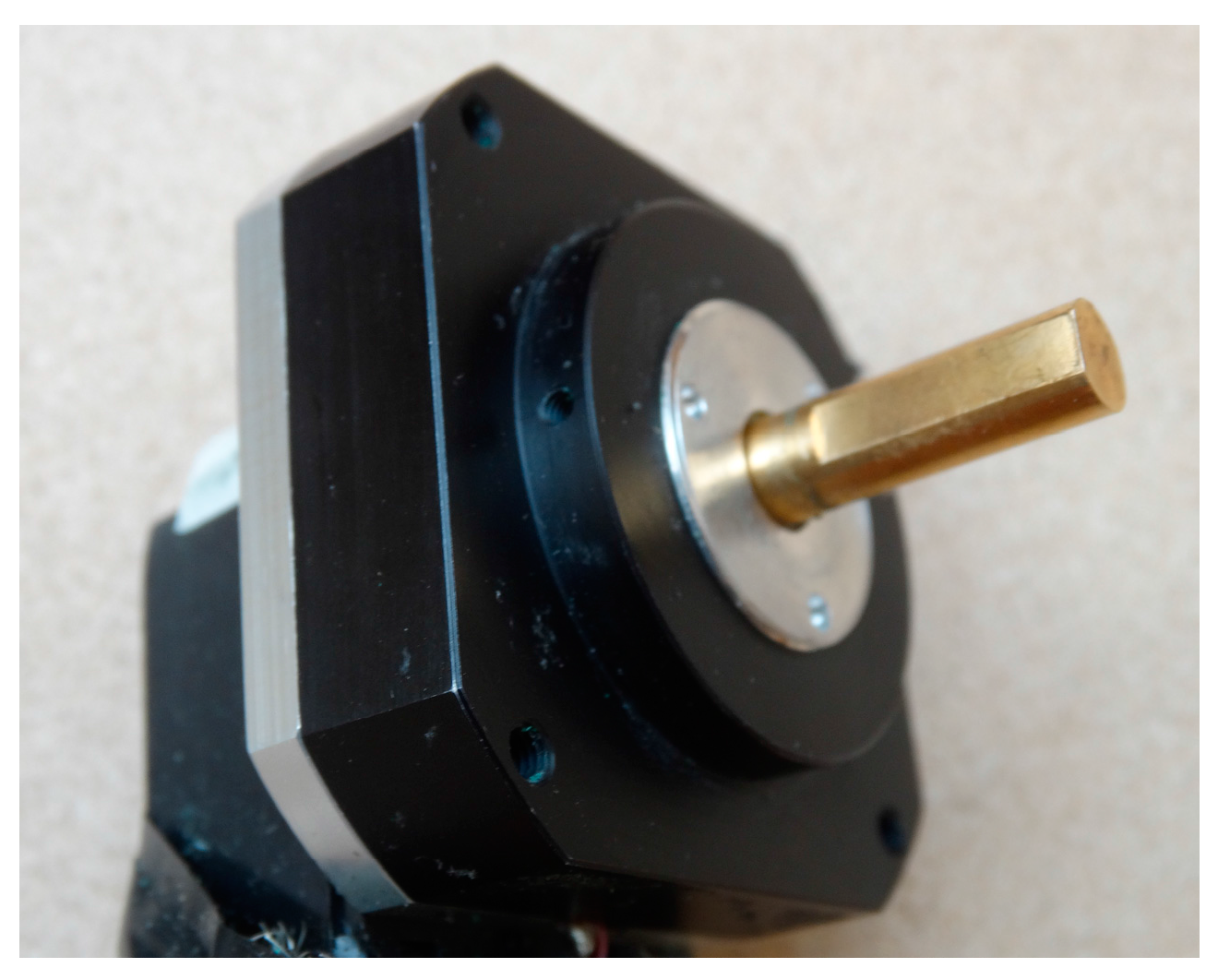
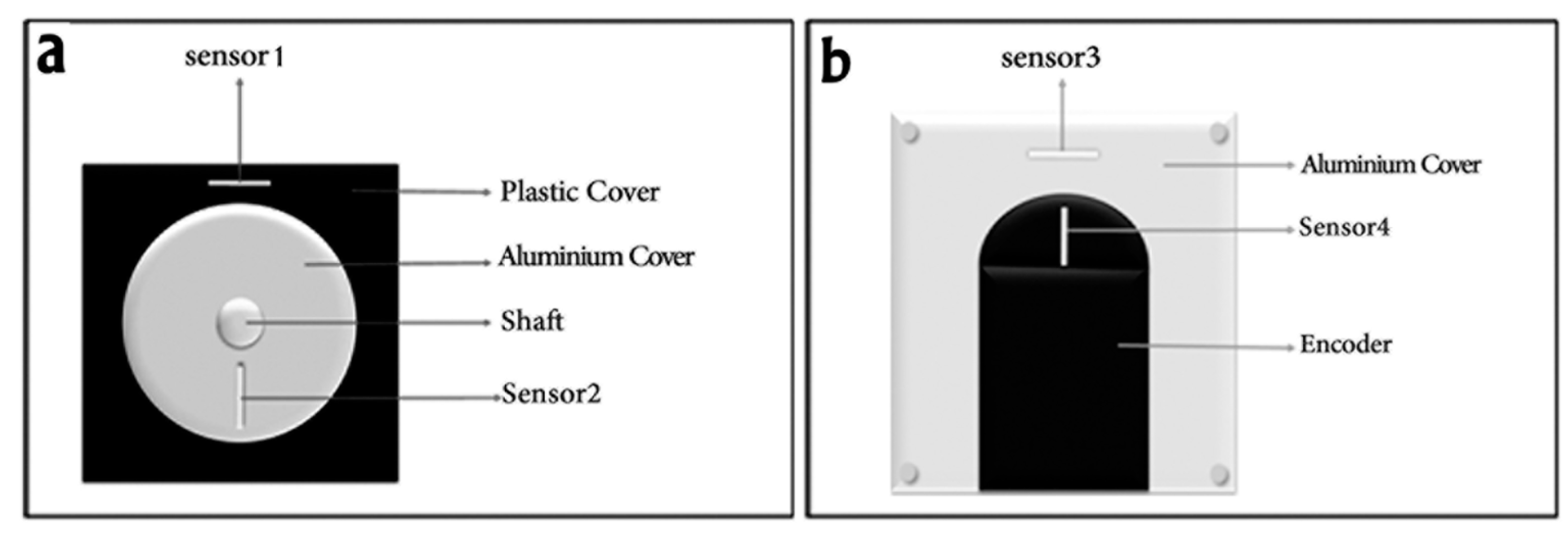
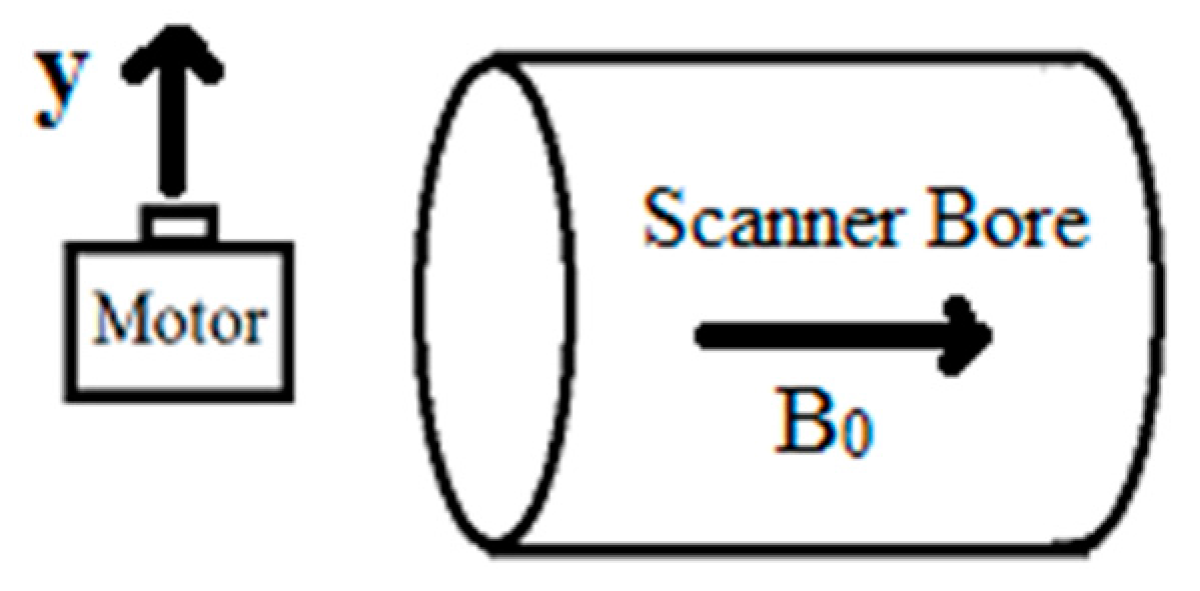
2. Materials and Methods
- T1W: TE = 10 ms, TR = 0.60 s, FOV = 160 160 150 mm3, in-plane voxel size = 1 mm, slice thickness = 5 mm, and flip angle = 70°.
- T2W: TE = 80 ms, TR = 3 s, FOV = 160 160 150 mm3, in-plane voxel size = 1 mm, slice thickness = 5 mm, flip angle = 90°, and turbo factor = 5.
- TSE: TE = 72 ms, TR = 4 s, FOV = 160 160 150 mm3, in-plane voxel size = 1 mm, slice thickness = 5 mm, flip angle = 90°, and turbo factor = 16.
- FFE: TE = 2.8 ms, TR = 12.1 ms, FOV = 160160150 mm3, in-plane voxel size = 1 mm, slice thickness = 5 mm, and flip angle = 30°.
3. Results
3.1. Theoretical Evaluation
3.2. Scanner Off
3.3. Scanner on Common Clinical Imaging Sequences
3.4. Scanner on Echo Planar Imaging Sequence
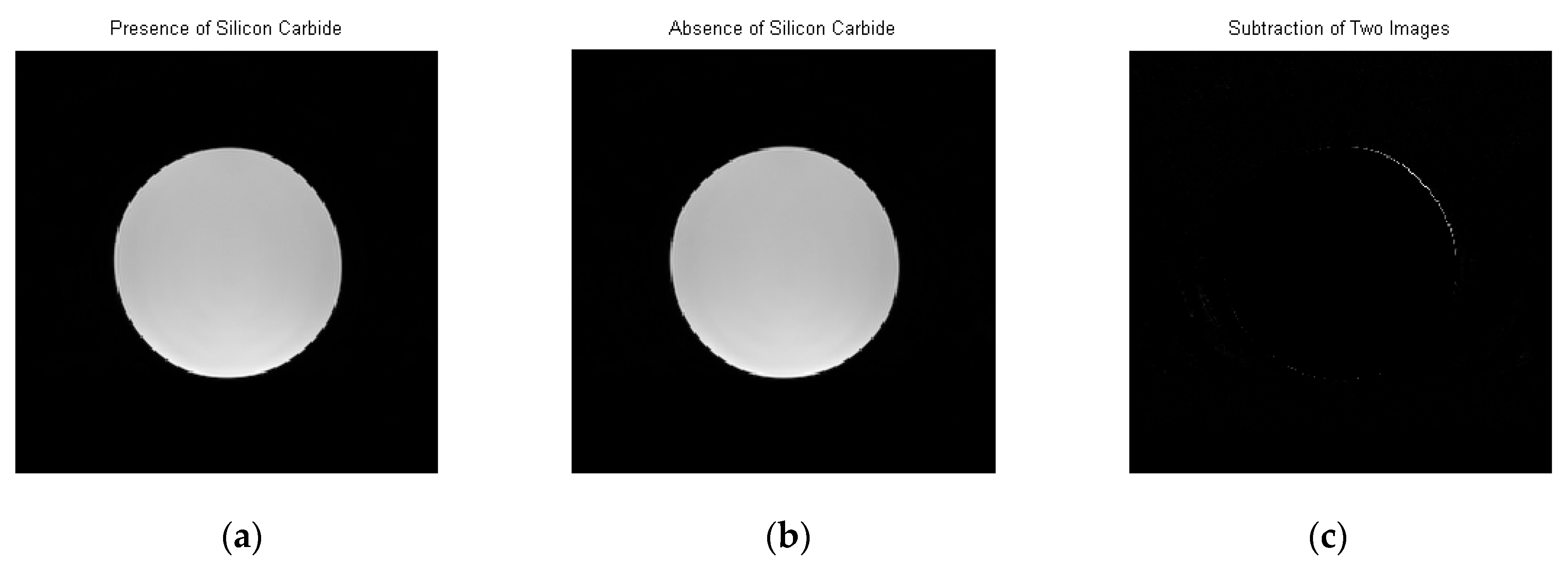
3.5. MR Image of Silicon Carbide
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Shellock, F.G.; Shellock, V.J. Cardiovascular catheters and accessories: Ex vivo testing of ferromagnetism, heating, and artifacts associated with MRI. J. Magn. Reson. Imaging 1998, 8, 1338–1342. [Google Scholar] [CrossRef] [PubMed]
- The Joint Commission. Preventing accidents and injuries in the MRI suite. J. Radiol. Nurs. 2008, 27, 74–77. [Google Scholar]
- Stoianovici, D.; Song, D.; Petrisor, D.; Ursu, D.; Mazilu, D.; Muntener, M.; Schar, M.; Patriciu, A. “MRI Stealth” robot for prostate interventions. Minim. Invasive Ther. Allied. Technol. 2007, 16, 241–248. [Google Scholar] [CrossRef] [PubMed]
- Chinzei, K.; Hata, N.; Jolesz, F.A.; Kikinis, R. Surgical assist robot for the active navigation in the intraoperative MRI: Hardware design issues. In Proceedings of the 2000 IEEE/RSJ International Conference on Intelligent Robots and Systems, Takamatsu, Japan, 30 October–5 November 2000. [Google Scholar] [CrossRef]
- Koseki, Y.; Washio, T.; Chinzei, K.; Iseki, H. Endoscope manipulator for trans-nasal neurosurgery, optimized for and compatible to vertical field open MRI. Med. Image Comput. Comput. Assist. Interv. 2002, 2488, 114–121. [Google Scholar]
- Tsekos, N.V.; Khanicheh, A.; Christoforou, E.; Mavroidis, C. Magnetic resonance-compatible robotic and mechatronics systems for image-guided interventions and rehabilitation: A review study. Annu. Rev. Biomed. Eng. 2007, 9, 351–387. [Google Scholar] [CrossRef] [PubMed]
- Elhawary, H.; Tse, Z.T.H.; Hamed, A.; Rea, M.; Davies, B.L.; Lamperth, M.U. The case for MR-compatible robotics: A review of the state of the art. Int. J. Med. Robot. Comput. Assist. Surg. 2008, 4, 105–113. [Google Scholar] [CrossRef] [PubMed]
- Wong, T.Z.; Schwartz, R.B.; Pergolizzi, R.S., Jr.; Black, P.M.; Kacher, D.F.; Morrison, P.R.; Jolesz, F.A. Interactive MR image guidance for neurosurgical and minimally invasive procedures. Proc. SPIE 1999, 3594, 170–177. [Google Scholar]
- Kaiser, M.; Krug, J.; Rose, G. Interventional MRI: Minimal-invasive surgery under MR guidance. In Proceedings of the 2011 IEEE MTT-S International Microwave Symposium Digest (MTT), Baltimore, MD, USA, 5–10 June 2011. [Google Scholar] [CrossRef]
- Masamune, K.; Kobayashi, E.; Masutani, Y.; Suzuki, M.; Dohi, T.; Iseki, H.; Takakura, K. Development of an MRI-compatible needle insertion manipulator for stereotactic neurosurgery. J. Image Guid. Surg. 1995, 1, 242–248. [Google Scholar] [CrossRef]
- Goldenberg, A.A.; Trachtenberg, J.; Yi, Y.; Weersink, R.; Sussman, M.S.; Haider, M.; Ma, L.; Kucharczyk, W. Robot-assisted MRI-guided prostatic interventions. Robotica 2010, 28, 215–234. [Google Scholar] [CrossRef]
- Krieger, A.; Iordachita, I.; Song, S.E.; Cho, N.B.; Guion, P.; Fichtinger, G.; Whitcomb, L.L. Development and preliminary evaluation of an actuated MRI-compatible robotic device for MRI-guided prostate intervention. In Proceedings of the 2010 IEEE International Conference on Robotics and Automation (ICRA), Anchorage, AK, USA, 3–7 May 2010; pp. 1066–1073. [Google Scholar]
- Larson, B.T.; Erdman, A.G.; Tsekos, N.V.; Yacoub, E.; Tsekos, P.V.; Koutlas, I.G. Design of an MRI-compatible robotic stereotactic device for minimally invasive interventions in the breast. J. Biomech. Eng. 2004, 126, 458–465. [Google Scholar] [CrossRef] [PubMed]
- Hashizume, M.; Yasunaga, T.; Tanoue, K.; Ieiri, S.; Konishi, K.; Kishi, K.; Nakamoto, H.; Ikeda, D.; Sakuma, I.; Fujie, M.; et al. New real-time MR image-guided surgical robotic system for minimally invasive precision surgery. Int. J. Comput. Assist. Radiol. Surg. 2008, 2, 317–325. [Google Scholar] [CrossRef]
- Sutherland, G.R.; McBeth, P.B.; Louw, D.F. NeuroArm: An MR compatible robot for microsurgery. Int. Congr. Ser. 2003, 1256, 504–508. [Google Scholar] [CrossRef]
- Hempel, E.; Fischer, H.; Gumb, L.; Höhn, T.; Krause, H.; Voges, U.; Breitwieser, H.; Gutmann, B.; Durke, J.; Bock, M.; et al. An MRI-compatible surgical robot for precise radiological interventions. Comput. Aided Surg. 2003, 8, 180–191. [Google Scholar] [CrossRef] [PubMed]
- Cole, G.A.; Harrington, K.; Su, H.; Camilo, A.; Pilitsis, J.G.; Fischer, G.S. Closed-Loop Actuated Surgical System Utilizing Real-Time In-Situ MRI Guidance. In Experimental Robotics; Springer: Berlin/Heidelberg, Germany, 2014; pp. 785–798. [Google Scholar]
- Shinsei Corporation. 2007. Available online: http://www.shinsei-motor.com/English/techno/ultrasonic_motor.html (accessed on 10 May 2017).
- Hirata, H.; Ueha, S. Characteristics estimation of a traveling wave type ultrasonic motor. IEEE Trans. Ultrason. Ferroelectr. Freq. Control. 2002, 40, 402–406. [Google Scholar] [CrossRef] [PubMed]
- Tsekos, N.V.; Shudy, J.; Yacoub, E.; Tsekos, P.V.; Koutlas, I.G. Development of a robotic device for MRI-guided interventions in the breast. In Proceedings of the IEEE 2nd International Symposium on Bioinformatics and Bioengineering, Bethesda, MD, USA, 4–6 November 2001; pp. 201–208. [Google Scholar]
- Bolborici, V. Modeling of the Stator of Piezoelectric Traveling Wave Rotary Ultrasonic Motors. Ph.D. Thesis, University of Toronto, Toronto, ON, Canada, 2009. [Google Scholar]
- Uchino, K. Piezoelectric ultrasonic motors: Overview. Smart Mater. Struct. 1998, 7, 273–285. [Google Scholar] [CrossRef]
- Senjyu, T.; Miyazato, H.; Yokoda, S.; Uezato, K. Speed control of ultrasonic motors using neural network. IEEE Trans. Power Electron. 1998, 13, 381–387. [Google Scholar] [CrossRef]
- Zhao, C. Ultrasonic Motors: Technologies and Applications; Springer Science & Business Media: New York, NY, USA, 2011. [Google Scholar]
- Dedini, R.D.; Karacozoff, A.M.; Shellock, F.G.; Xu, D.; McClellan, R.T.; Pekmezci, M. MRI issues for ballistic objects: Information obtained at 1.5-, 3- and 7-Tesla. Spine J. 2013, 13, 815–822. [Google Scholar] [CrossRef] [PubMed]
- Slack, G.A. Thermal conductivity of pure and impure silicon, silicon carbide, and diamond. J. Appl. Phys. 1964, 35, 3460–3466. [Google Scholar] [CrossRef]
- Bassen, H.; Kainz, W.; Mendoza, G.; Kellom, T. MRI-induced heating of selected thin wire metallic implants—Laboratory and computational studies—Findings and new questions raised. Minim. Invasive Ther. Allied Technol. 2006, 15, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Jeschke, M.G.; Kamolz, L.P.; Sjöberg, F.; Wolf, S.E. Handbook of Burns; Springer: Vienna, Austria; New York, NY, USA, 2012; p. 42. [Google Scholar]



© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shokrollahi, P.; Drake, J.M.; Goldenberg, A.A. Measuring the Temperature Increase of an Ultrasonic Motor in a 3-Tesla Magnetic Resonance Imaging System. Actuators 2017, 6, 20. https://doi.org/10.3390/act6020020
Shokrollahi P, Drake JM, Goldenberg AA. Measuring the Temperature Increase of an Ultrasonic Motor in a 3-Tesla Magnetic Resonance Imaging System. Actuators. 2017; 6(2):20. https://doi.org/10.3390/act6020020
Chicago/Turabian StyleShokrollahi, Peyman, James M. Drake, and Andrew A. Goldenberg. 2017. "Measuring the Temperature Increase of an Ultrasonic Motor in a 3-Tesla Magnetic Resonance Imaging System" Actuators 6, no. 2: 20. https://doi.org/10.3390/act6020020




