Impact of Environmental Factors on Legionella Populations in Drinking Water
Abstract
:1. Introduction
2. Results
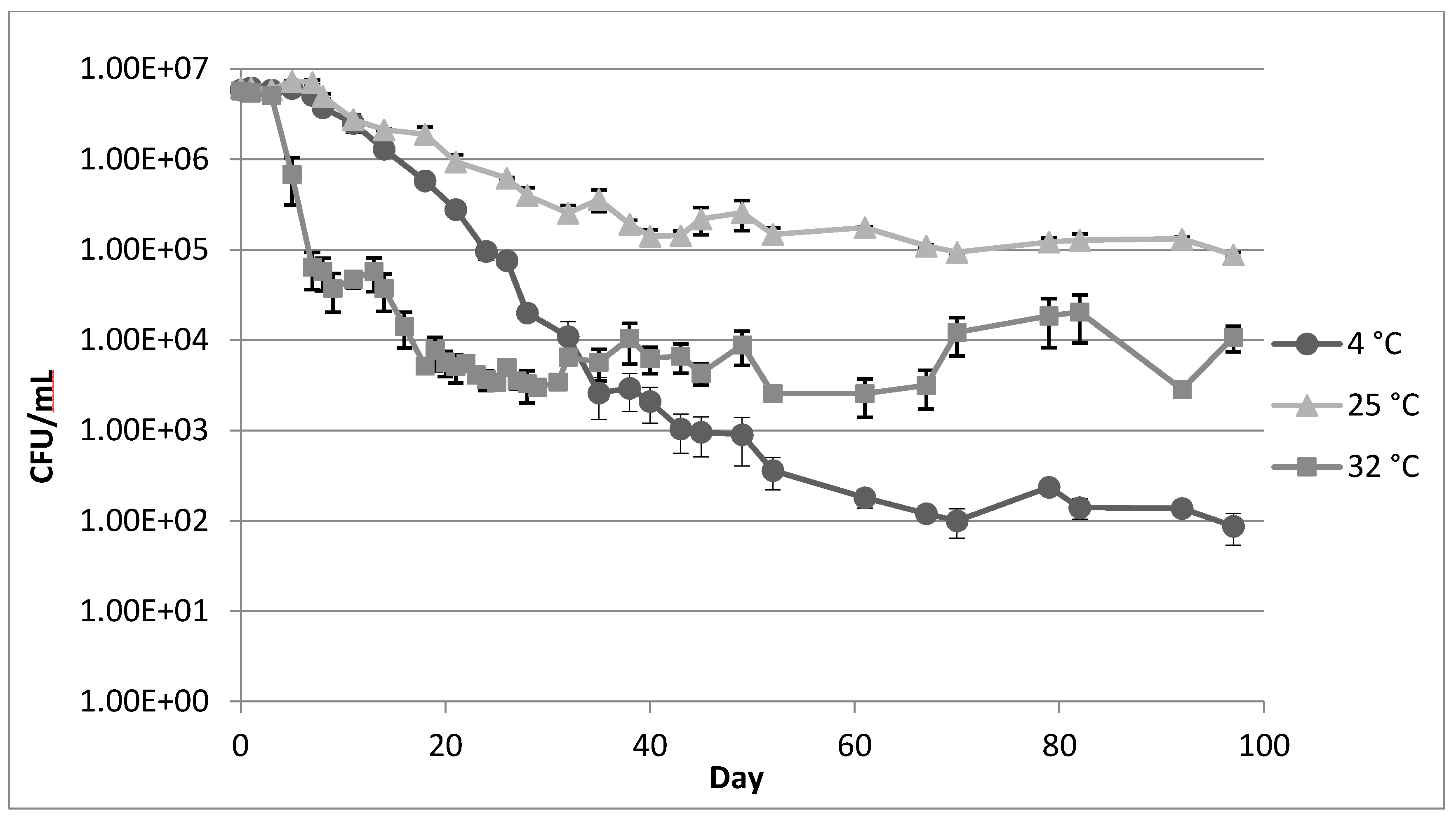
2.1. Survival of Legionella in Tap Water at 4 °C, 25 °C, and 32 °C
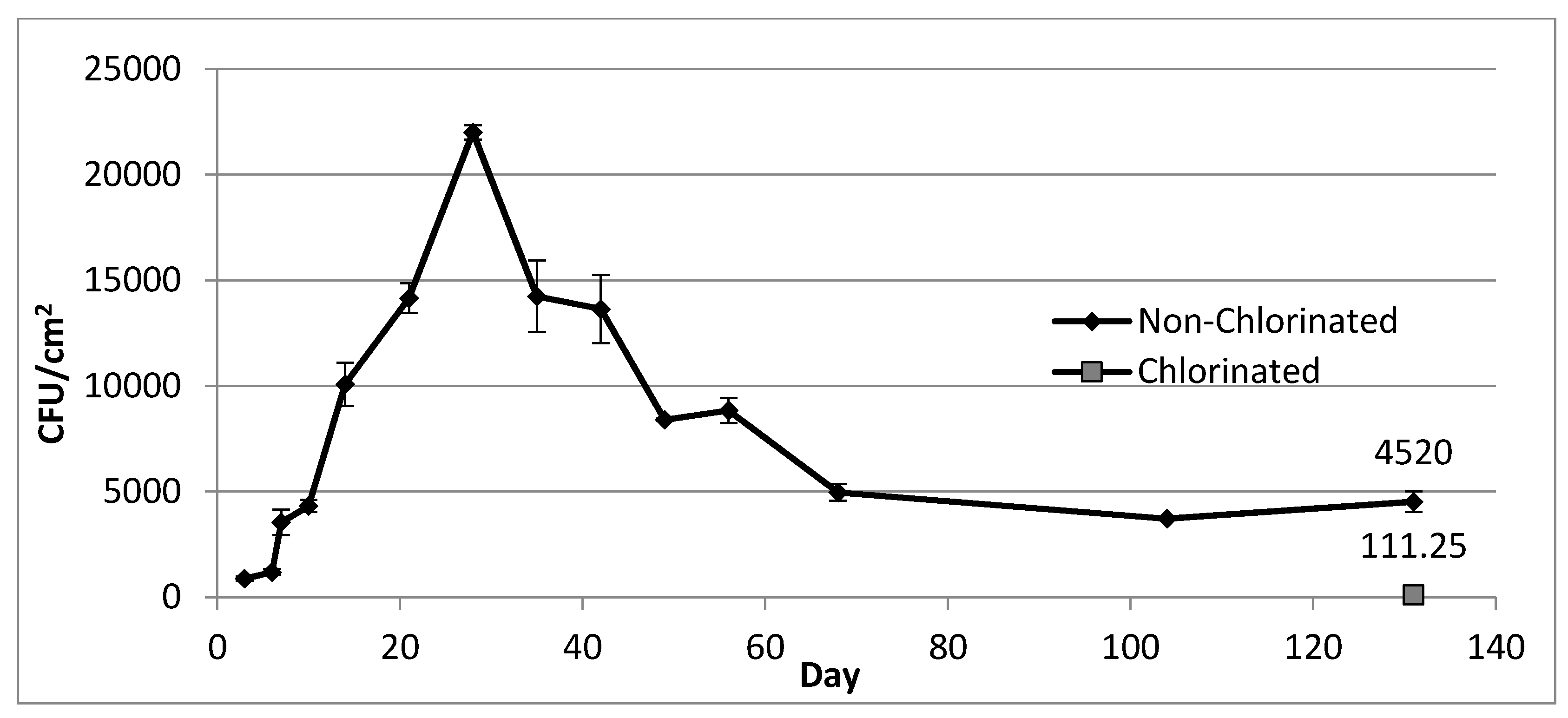
2.2. Association of Legionella within Biofilms on a Variety of Pipe Coupons


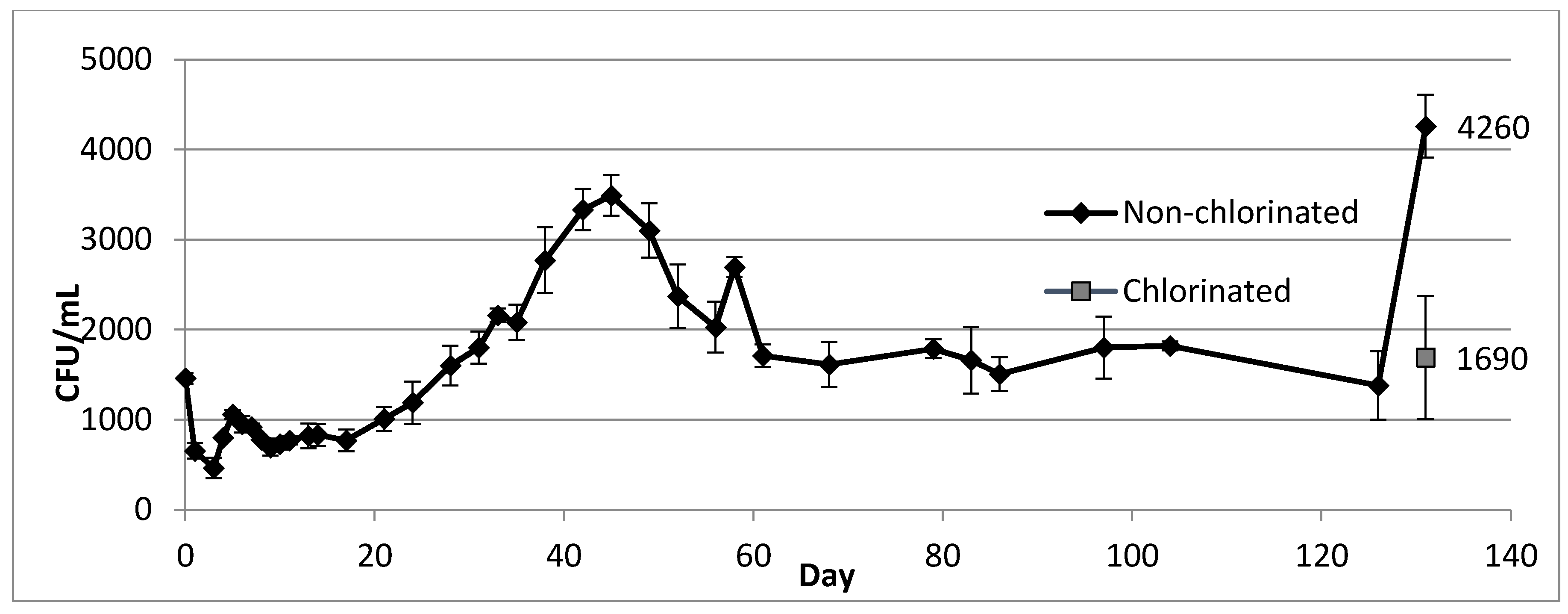
2.3. Growth and Survival of Legionella in a Model Drinking Water Distribution System
2.4. Presence of Legionella in Residential Water Meter Biofilms
| Sample Site | Legionella spp. Positive | L. pneumophila Positive |
|---|---|---|
| System A | 26% (9/35) | 14% (5/35) |
| System B | 0% (0/32) | 0% (0/32) |
3. Discussion
3.1. Survival of Legionella in Tap Water at 4 °C, 25 °C, and 32 °C
3.2. Association of Legionella within Biofilms on a Variety of Pipe Coupons
3.3. Growth and Survival of Legionella in a Model Drinking Water Distribution System
3.4. Presence of Legionella in Water Meter Biofilms
4. Materials and Methods
4.1. Media and Laboratory Strain of Legionella
4.2. Molecular Detection of Legionella
4.3. Survival of Legionella in Tap Water at 4 °C, 25 °C, and 32 °C
4.4. Association of Legionella within Biofilms on a Variety of Pipe Coupons
4.5. Growth and Survival of Legionella in a Model Drinking Water Distribution System
4.6. Presence of Legionella in Residential Water Meter Biofilms
4.7. Data Analysis
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Diederen, B.M.W. Legionella spp. and Legionnaires’ disease. J. Infect. 2008, 56, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Donlan, R.M.; Forster, T.; Murga, R.; Brown, E.; Lucas, C.; Carpenter, J.; Fields, B. Legionella pneumophila associated with the protozoan Hartmanella vermiformis in a model multi-species biofilm has reduced susceptibility to disinfectants. Biofouling 2005, 21, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Valster, R.M.; Wullings, B.A.; van der Kooij, D. Detection of protozoan hosts for Legionella pneumophila in engineered water systems by using a biofilm batch test. Appl. Environ. Microbiol. 2010, 76, 7144–7153. [Google Scholar] [CrossRef] [PubMed]
- Wadowsky, R.M.; Wilson, T.M.; Kapp, N.J.; West, A.J.; Kuchta, J.M.; States, S.J.; Dowling, J.N.; Yee, R.B. Multiplication of Legionella spp. in tap water containing Hartmanella vermiformis. Appl. Environ. Microbiol. 1991, 57, 1950–1955. [Google Scholar] [PubMed]
- Declerck, P. Biofilms: The environmental playground of Legionella pneumophila. Environ. Microbiol. 2012, 12, 557–566. [Google Scholar] [CrossRef]
- Brenner, D.J.; Steigerwalt, A.G.; McDade, J.E. Classification of the Legionnaires’ disease bacterium: Legionella pneumophila, genus novum, species nova, of the family Legionellaceae, familia nova. Ann. Intern. Med. 1979, 90, 656–658. [Google Scholar] [CrossRef] [PubMed]
- Hicks, L.A.; Garrison, L.E.; Nelson, G.E.; Hampton, L.M. Legionellosis—United States, 2000–2009. Am. J. Transpl. 2012, 12, 250–253. [Google Scholar] [CrossRef]
- Stout, J.E.; Yu, V.L. Legionellosis. N. Engl. J. Med. 1997, 337, 682–687. [Google Scholar] [CrossRef] [PubMed]
- Brunkard, J.M.; Ailes, E.; Roberts, V.A.; Hill, V.; Hillborn, E.D.; Craun, G.F.; Rajasingham, A.; Kahler, A.; Garrison, L.; Hicks, L.; et al. Surveillance for Waterborne Disease Outbreaks Associated with Drinking Water—United States, 2007–2008. CDC MMWR Surveill. Summ. 2011, 60, 38–68. [Google Scholar]
- Farhat, M.; Moletta-Denat, M.; Frère, J.; Onillon, S.; Trouilhé, M.; Robine, E. Effects of disinfection on Legionella spp., eukarya, and biofilms in a hot water system. Environ. Microbiol. 2012, 78, 6850–6858. [Google Scholar] [CrossRef]
- Kool, J.L.; Bergmire-Sweat, D.; Butler, J.C.; Brown, E.W.; Peabody, D.J.; Massi, D.S.; Carpenter, J.C.; Pruckler, J.M.; Benson, R.F.; Fields, B.S. Hospital characteristics associated with colonization of water systems by Legionella and risk of nosocomial legionnaires’ disease: A cohort study of 15 hospitals. Infect. Control Hosp. Epidemiol. 1999, 20, 798–805. [Google Scholar] [CrossRef] [PubMed]
- Donohue, M.J.; O’Connell, K.; Vesper, S.J.; Mistry, J.H.; King, D.; Kostich, M.; Pfaller, S. Widespread molecular detection of Legionella pneumophila Serogroup 1 in cold water taps across the United States. Environ. Sci. Technol. 2014, 48, 3145–3152. [Google Scholar] [CrossRef] [PubMed]
- Schulze-Röbbecke, R.; Rödder, M.; Exner, M. Multiplication and killing temperatures of naturally occurring legionellas. Zbl. Bakt. Mikrobiol. Hyg. 1987, 184, 495–500. [Google Scholar]
- Al-Bana, B.H.; Haddad, M.T.; Garduño, R.A. Stationary phase and mature infectious forms of Legionella pneumophila produce distinct viable but non-culturable cells. Environ. Microbiol. 2013, 16, 382–395. [Google Scholar] [CrossRef] [PubMed]
- Piao, Z.; Sze, C.C.; Barysheva, O.; Iida, K.; Yoshida, S. Temperature-regulated formation of mycelial mat-like biofilms by Legionella pneumophila. Appl. Environ. Microbiol. 2006, 72, 1613–1622. [Google Scholar] [CrossRef] [PubMed]
- Pongratz, A.; Schwarzkopf, A.; Hahn, H.; Heesemann, J.; Karch, H.; Döll, W. The effect of the pipe material of the drinking water system on the frequency of Legionella in a hospital. Zbl. Hyg. Umweltmed. 1994, 195, 483–488. [Google Scholar]
- Serrano-Suárez, A.; Dellundé, J.; Salvadó, H.; Cervero-Aragó, S.; Méndez, J.; Canals, O.; Blanco, S.; Arcas, A.; Araujo, R. Microbial and physiochemical parameters associated with Legionella contamination in hot water recirculation systems. Environ. Sci. Pollut. Res. Int. 2013, 20, 5534–5544. [Google Scholar] [CrossRef] [PubMed]
- Cooper, I.R.; Hanlon, G.W. Resistance of Legionella pneumophila serotype 1 biofilms to chlorine-based disinfection. J. Hosp. Infect. 2010, 74, 152–159. [Google Scholar] [CrossRef] [PubMed]
- Marchesi, I.; Marchegiano, P.; Bargellini, A.; Cencetti, S.; Frezza, G.; Miselli, M.; Borella, P. Effectiveness of different methods to control legionella in the water supply: Ten-year experience in an Italian university hospital. J. Hosp. Infect. 2011, 77, 47–51. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Health and Human Services. Procedures for the Recovery of Legionella from the Environment; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2005.
- Wullings, B.A.; Bakker, G.; van der Kooij, D. Concentration and diversity of uncultured Legionella spp. in two unchlorinated drinking water supplies with different concentrations of natural organic matter. Appl. Environ. Microbiol. 2011, 77, 634–641. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schwake, D.O.; Alum, A.; Abbaszadegan, M. Impact of Environmental Factors on Legionella Populations in Drinking Water. Pathogens 2015, 4, 269-282. https://doi.org/10.3390/pathogens4020269
Schwake DO, Alum A, Abbaszadegan M. Impact of Environmental Factors on Legionella Populations in Drinking Water. Pathogens. 2015; 4(2):269-282. https://doi.org/10.3390/pathogens4020269
Chicago/Turabian StyleSchwake, David Otto, Absar Alum, and Morteza Abbaszadegan. 2015. "Impact of Environmental Factors on Legionella Populations in Drinking Water" Pathogens 4, no. 2: 269-282. https://doi.org/10.3390/pathogens4020269





