Prescribing under the Influence: The Business of Breastmilk Substitutes
Abstract
:1. Introduction
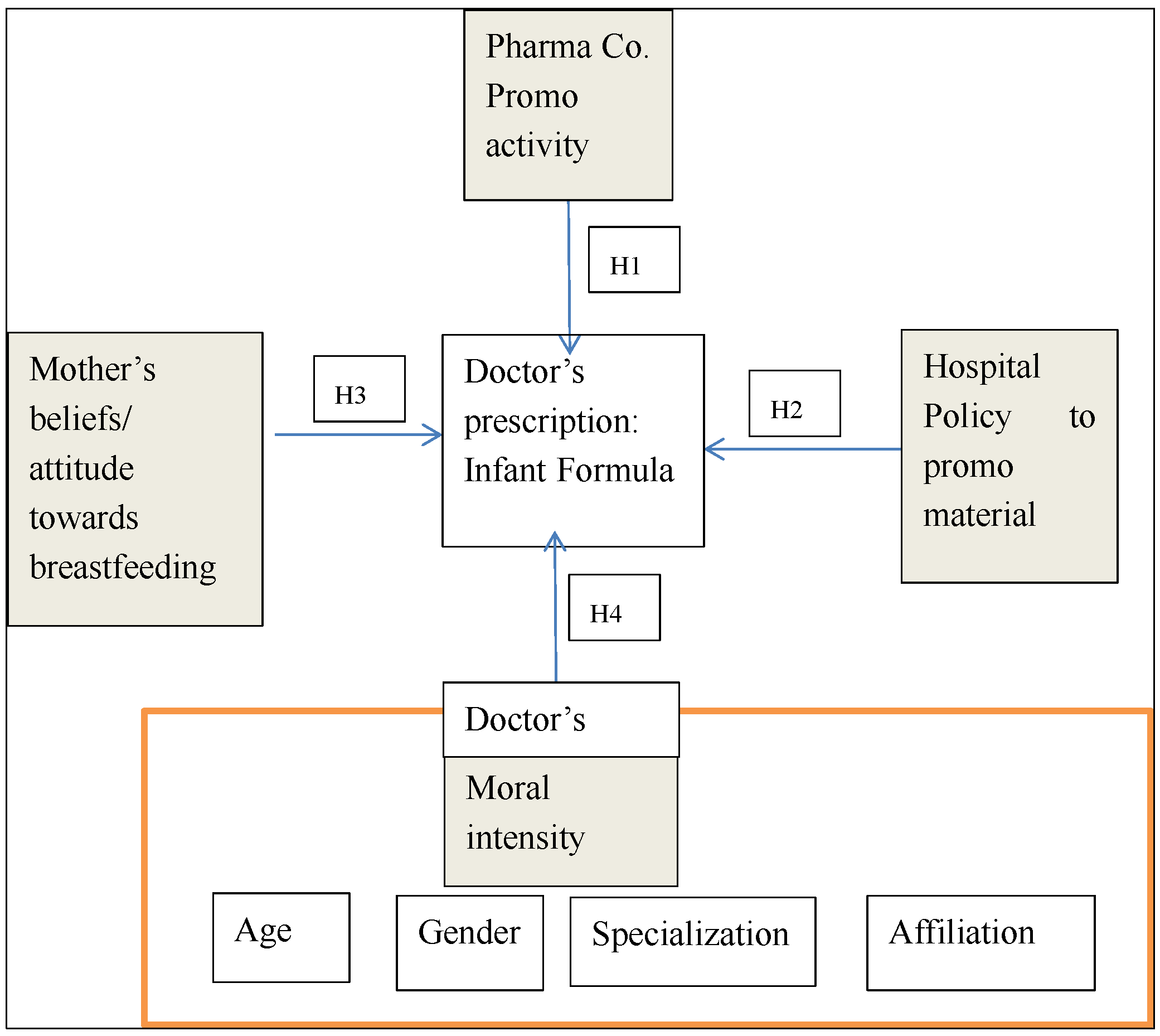
Theoretical Framework
2. Materials and Methods
2.1. Design
2.2. Setting
2.3. Sample
2.4. Measures
- Scenario 1:
- A healthcare provider (doctor) is told by a mother that she is planning to bottle-feed her baby. However, because of his intention to prescribe an infant formula, the healthcare provider does not inform her about the benefits of breastfeeding and prescribed an infant formula instead.
- Scenario 2:
- An infant formula company sponsors a hospital’s advertisement campaign, and in return, the hospital allows the company to distribute and promote its branded ready to feed milk formula and branded maternity goody bags to mothers.
2.5. Analysis Plan
3. Results
4. Discussion
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Howard L. Sobel, Alessandro Iellamo, René R. Raya, Alexander A. Padilla, Jean-Marc Olivé, and Soe Nyunt-U. “Is unimpeded marketing for breast milk substitutes responsible for the decline in breastfeeding in the Philippines? An exploratory survey and focus group analysis.” Social Science & Medicine 73 (2011): 1445–48. [Google Scholar] [CrossRef] [PubMed]
- WHO/UNICEF. Acceptable Medical Reasons for Use of Breast-Milk Substitutes. Geneva: World Health Organization, 2009. [Google Scholar]
- Mari Jeeva Sankar, Bireshwar Sinha, Ranadip Chowdhury, Nita Bhandari, Sunita Taneja, Jose Martines, and Rajiv Bahl. “Optimal breastfeeding practices and infant and child mortality: A systematic review and meta-analysis.” Acta Paediatrica 104 (2015): 3–13. [Google Scholar] [CrossRef] [PubMed]
- Cathal McCrory, and Richard Layte. “The effect of breastfeeding on children’s educational test scores at nine years of age: Results of an Irish cohort study.” Social Science & Medicine 72 (2011): 1515–21. [Google Scholar] [CrossRef] [PubMed]
- Stacy J. Carling, Margaret M. Demment, Chris L. Kjolhede, and Christine M. Olson. “Breastfeeding duration and weight gain trajectory in infancy.” Pediatrics 135 (2015): 111–19. [Google Scholar] [CrossRef] [PubMed]
- Colin W. Binns, Mi Kyung Lee, Li Tang, Chuan Yu, Tomiko Hokama, and Andy Lee. “Ethical issues in infant feeding after disasters.” Asia-Pacific Journal of Public Health 24 (2012): 672–80. [Google Scholar] [CrossRef] [PubMed]
- Flavia Bustreo. “Understanding the past—Planning the future: Celebrating 10 years of WHO/UNICEF’s Global Strategy for Infant and Young Child Feeding. Maternal, newborn, child and adolescent health.” 2012. Available online: http://www.who.int/maternal_child_adolescent/news_events/news/2012/30_07_2012/en/# (accessed on 5 July 2015).
- WHO. “European Region has lowest global breastfeeding rates.” 5 August 2015. Available online: http://www.euro.who.int/en/health-topics/Life-stages/maternal-and-newborn-health/news/news/2015/08/who-european-region-has-lowest-global-breastfeeding-rates (accessed on 1 December 2015).
- Cesar G. Victora, Rajiv Bahl, Aluísio J. D. Barros, Giovanny V. A. França, Susan Horton, Julia Krasevec, Simon Murch, Mari Sankar, Neff Walker, and Nigel Rollins. “Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect.” The Lancet 387 (2016): 475–90. [Google Scholar] [CrossRef]
- Ranadip Chowdhury, Bireshwar Sinha, Mari Jeeva Sankar, Sunita Taneja, Nita Bhandari, Nigel Rollins, Rajiv Bahl, and Jose Martines. “Breastfeeding and maternal health outcomes: A systematic review and meta-analysis.” Acta Paediatrica 104 (2015): 96–113. [Google Scholar] [CrossRef] [PubMed]
- The Lancet. “Breastfeedindg: Achieving the new normal.” 30 January 2016. Available online: http://thelancet.com/journals/lancet/article/PIIS0140-6736%2816%2900210-5/fulltext (accessed on 29 May 2016).
- World Health Organization (WHO). International Code of Marketing of Breast-Milk Substitutes. Geneva: WHO, 1981, p. 24. [Google Scholar]
- The Lancet. “No ifs, no buts, no follow-on milk.” 21 May 2016. Available online: http://www.thelancet.com/journals/lancet/article/PIIS0140-6736%2816%2930599-2/fulltext?rss=yes (accessed on 27 July 2016).
- Clare Relton, Barbara Whelan, Mark Strong, Kate Thomas, Heather Whitford, Elaine Scott, and Patrice van Cleemput. “Are financial incentives for breastfeeding feasible in the UK? A mixed methods field study.” The Lancet 384 (2014): S5. [Google Scholar] [CrossRef]
- Dylan Walters, Jakub Kakietek, Julia Eberwein, Thomas Pullum, and Meera Shekar. “Breastfeeding in the 21st century.” 2016. Available online: http://www.thelancet.com/pdfs/journals/lancet/PIIS0140-6736%2816%2930546-3.pdf (accessed on 27 July 2016).
- Hilary Bishop, Wendy Cousins, Karen Casson, and Ann Moore. “Culture and caregivers: Factors influencing breastfeeding among mothers in west Belfast, Northern Ireland.” Child Care in Practice 14 (2008): 165–79. [Google Scholar] [CrossRef]
- Helen Skouteris, Cate Nagle, Michelle Fowler, Bridie Kent, Pinki Sahota, and Heather Morris. “Interventions designed to promote exclusive breastfeeding in high-income countries: A systematic review.” Breastfeeding Medicine 9 (2014): 113–27. [Google Scholar] [CrossRef] [PubMed]
- Ke Zhang, Li Tang, Hong Wang, Li-Qian Qiu, Colin W. Binns, and Andy H. Lee. “Why do mothers of young infants choose to formula feed in china? Perceptions of mothers and hospital staff.” International Journal of Environmental Research and Public Health 12 (2015): 4520–32. [Google Scholar] [CrossRef] [PubMed]
- Sara F. L. Kirk, Sarah Meaghan Sim, Erin Hemmens, and Sheri L. Price. “Lessons learned from the implementation of a provincial breastfeeding policy in Nova Scotia, Canada and the implications for childhood obesity prevention.” International Journal of Environmental Research and Public Health 9 (2012): 1308–18. [Google Scholar] [CrossRef] [PubMed]
- Jennifer M. Nelson, Ruowei Li, and Cria G. Perrine. “Trends of US hospitals distributing infant formula packs to breastfeeding mothers, 2007 to 2013.” Pediatrics 135 (2015): 1051–56. [Google Scholar] [CrossRef] [PubMed]
- Todd Wolynn. “Breastfeeding—So easy even a doctor can support it.” Breastfeeding Medicine 6 (2011): 345–47. [Google Scholar] [CrossRef] [PubMed]
- Huda. “Breastfeeding in Islam.” 11 March 2016. Available online: http://islam.about.com/od/parenting/a/breastfeeding.htm (accessed on 8 August 2016).
- Quinn Grundy, Lisa Bero, and Ruth Malone. “Interactions between non-physician clinicians and industry: A systematic review.” PLOS Medicine 10 (2013): e1001561. [Google Scholar] [CrossRef] [PubMed]
- Worst Pills, and Best Pills. “Misprescribing and overprescribing of drugs.” Available online: http://www.worstpills.org/public/page.cfm?op_id=3 (accessed on 1 December 2015).
- Marc A. Rodwin. Medicine, Money, and Morals: Physicians’ Conflicts of Interest. New York: Oxford University Press, 1993. [Google Scholar]
- Charlotte M. Wright, and Tony Waterston. “Relationships between paediatricians and infant formula milk companies.” Archives of Disease in Childhood 91 (2006): 383–85. [Google Scholar] [CrossRef] [PubMed]
- Klaus Lieb, and Simone Brandtönies. “A survey of German physicians in private practice about contacts with pharmaceutical sales representatives.” Deutsches Ärzteblatt International 107 (2010): 392–98. [Google Scholar] [PubMed]
- Dana Katz, Arthur Caplan, and Jon Merz. “All gifts large and small. Toward an understanding of the ethics of pharmaceutical industry gift-giving.” The American Journal of Bioethics 3 (2003): 39–46. [Google Scholar] [CrossRef] [PubMed]
- IBFAN. Breaking the Rules, Stretching the Rules 2014. Edited by Annelies Allain. Penang: International Baby Food Action Network, 2014, p. 40. Available online: http://www.babymilkaction.org/wp-content/uploads/2014/05/BTR14inbrief.pdf (accessed on 25 July 2016).
- Kuwait-WBTi. “Kuwait WBTi Assessment report.” In The Worldbreastfeeding Trends Initiative (WBTi). Kuwait: Kuwait MOH, 2015. [Google Scholar]
- Rizwan Raheem Ahmed, and Ahmad Saeed. “Pharmaceutical drug promotion in Pakistan: Issues in ethical and non-ethical practices.” Interdisciplinary Journal of Contemporary Research in Business 4 (2012): 149–64. [Google Scholar]
- Barbara Mintzes. “Regulation of formula advertising in the Philippines and promotion and protection of breastfeeding: A commentary on Sobel, Iellamo, Raya, Padilla, Olivé and Nyunt-U.” Social Science & Medicine 73 (2011): 1449–51. [Google Scholar] [CrossRef] [PubMed]
- June P. Brady, and Leila Srour. “India, Laos and South Africa reject sponsorship and gifts from formula companies.” African Health Sciences 14 (2014): 211–15. [Google Scholar] [CrossRef] [PubMed]
- BBC News. “Danone in management shuffle amid China bribery claims.” 15 October 2013. Available online: http://www.bbc.com/news/business-24530034 (accessed on 5 July 2015).
- Bob D. Cutler, and Robert F. Wright. “The US infant formula industry: Is direct-to-consumer advertising unethical or inevitable? ” Health Marketing Quarterly 19 (2002): 39–55. [Google Scholar] [CrossRef] [PubMed]
- WHO. “Baby-friendly hospital initiative.” Available online: http://www.who.int/nutrition/topics/bfhi/en/ (accessed on 5 July 2015).
- Fairbank Lisa, Susan O’Meara, Mary Renfrew, Mike Woolridge, and Amanda Sowden. “A systematic review to evaluate the effectiveness of interventions to promote the initiation of breastfeeding.” Health Technology Assessment 4 (2000): 1–171. [Google Scholar]
- Angela Donnelly, Helen Snowden, Mary Renfrew, and Mike Woolridge. “Commercial hospital discharge packs for breastfeeding women.” In The Cochrane Library. Chichester: John Wiley & Sons, Ltd., 2004. [Google Scholar]
- Barbara L. Philipp, Anne Merewood, Lisa W. Miller, Neetu Chawla, Melissa M. Murphy-Smith, Jenifer S. Gomes, Sabrina Cimo, and John T. Cook. “Baby-friendly hospital initiative improves breastfeeding initiation rates in a US hospital setting.” Pediatrics 108 (2001): 677–81. [Google Scholar] [CrossRef] [PubMed]
- June Pauline Brady. “Marketing breast milk substitutes: Problems and perils throughout the world.” Archives of Disease in Childhood 97 (2012): 529–32. [Google Scholar] [CrossRef] [PubMed]
- Summer Sherburne Hawkins, Ariel Dora Stern, Christopher F. Baum, and Matthew W. Gillman. “Evaluating the impact of the Baby-Friendly Hospital Initiative on breast-feeding rates: A multi-state analysis.” Public Health Nutrition 18 (2015): 189–97. [Google Scholar] [CrossRef] [PubMed]
- Joy Heads. “The baby friendly hospital initiative: A case study from NSW.” New South Wales Public Health Bulletin 16 (2005): 63–66. [Google Scholar] [PubMed]
- Australian Health Ministers’ Conference. The Australian National Breastfeeding Strategy 2010–2015; Canberra: Australian Government Department of Health and Ageing, 2009.
- Richard L. Kravitz, Robert A. Bell, Rahman Azari, Edward Krupat, Steven Kelly-Reif, and David Thom. “Request fulfillment in office practice: Antecedents and relationship to outcomes.” Medical Care 40 (2002): 38–51. [Google Scholar] [CrossRef] [PubMed]
- Richard L. Kravitz, Robert A. Bell, Carol E. Franz, Richard L. Kravitz, Marc N. Elliott, Ezra Amsterdam, Carrie Willis, and Lisa Silverio. “Characterising patient requests and physician responses in office practice.” Health Services Research 37 (2002): 217–38. [Google Scholar] [PubMed]
- Lori B. Feldman-Winter, Richard J. Schanler, Karen G. O’Connor, and Ruth A. Lawrence. “Pediatricians and the promotion and support of breastfeeding.” Archives of Pediatrics & Adolescent Medicine 162 (2008): 1142–49. [Google Scholar] [CrossRef] [PubMed]
- Patricia J. Lucas, Christie Cabral, Alastair D. Hay, and Jeremy Horwood. “A systematic review of parent and clinician views and perceptions that influence prescribing decisions in relation to acute childhood infections in primary care.” Scandinavian Journal of Primary Health Care 33 (2015): 11–20. [Google Scholar] [CrossRef] [PubMed]
- Thomas M. Jones. “Ethical decision making by individuals in organizations: An issue-contingent model.” Academy of Management Review 16 (1991): 366–95. [Google Scholar]
- Loy D. Watley, and Douglas R. May. “Enhancing moral intensity: The roles of personal and consequential information in ethical decision-making.” Journal of Business Ethics 50 (2004): 105–26. [Google Scholar] [CrossRef]
- Douglas R. May, and Kevin P. Pauli. “The role of moral intensity in ethical decision making a review and investigation of moral recognition, evaluation, and intention.” Business & Society 41 (2002): 84–117. [Google Scholar] [CrossRef]
- Mark A. Davis, Nancy Brown Johnson, and Douglas G. Ohmer. “Issue-contingent effects on ethical decision making: A cross-cultural comparison.” Journal of Business Ethics 17 (1998): 373–89. [Google Scholar] [CrossRef]
- Tim Barnett. “Dimensions of moral intensity and ethical decision making: An empirical study.” Journal of Applied Social Psychology 31 (2001): 1038–57. [Google Scholar] [CrossRef]
- Joan Marie McMahon, and Robert J. Harvey. “The effect of moral intensity on ethical judgment.” Journal of Business Ethics 72 (2007): 335–57. [Google Scholar] [CrossRef]
- Susan C. Borkowski, and Yusuf J. Ugras. “Business students and ethics: A meta-analysis.” Journal of Business Ethics 17 (1998): 1117–27. [Google Scholar] [CrossRef]
- Stephen Thomas, and James Rest. “Moral judgement, behavior, decision making, and attitudes.” In Moral Development: Advances in Research and Theory. Edited by James Rest. New York: Praeger, 1986, pp. 133–75. [Google Scholar]
- Carma L. Bylund, and Gregory Makoul. “Empathic communication and gender in the physician-patient encounter.” Patient Education and Counseling 48 (2002): 207–16. [Google Scholar] [CrossRef]
- Letizia Orzella, Francesco Chini, Patrizzio Pezzotti, and Marco Nardelli. “Antibiotic prescriptions in the paediatric population in the Lazio Region of Italy: Association with children’s and physician’s characteristics.” Annali di Igiene: Medicina Preventiva e di Comunita 26 (2013): 507–17. [Google Scholar]
- Lawrence Kohlberg. “Moral Stages and Moralization: The Cognitive-Developmental.” In Moral Development and Behavior: Theory, Research, and Social Issues. Edited by Thomas Lickona. New York: Rinehart and Winston, 1976. [Google Scholar]
- American Academy of Pediatrics (AAP). “The promotion of breast-feeding.” Pediatrics 69 (1981): 654–61. [Google Scholar]
- Kyung-Hyun Choi, Sang-Min Park, Ju-Hyun Lee, and Soonman Kwon. “Factors affecting the prescribing patterns of antibiotics and injections.” Journal of Korean Medical Science 27 (2012): 120–27. [Google Scholar] [CrossRef] [PubMed]
- Sophonneary Prak, Miriam Iuell Dahl, Sam Oeurn, Joel Conkle, Aaron Wise, and Arnaud Laillou. “Breastfeeding Trends in Cambodia, and the Increased Use of Breast-Milk Substitute—Why Is It a Danger? ” Nutrients 6 (2014): 2920–30. [Google Scholar] [CrossRef] [PubMed]
- “salesforce.com.” Available online: https://www.salesforce.com/ (accessed on 25 September 2015).
- R. Eric Reidenbach, Donald P. Robin, and Lyndon Dawson. “An application and extension of a multidimensional ethics scale to selected marketing practices and marketing groups.” Journal of the Academy of Marketing Science 19 (1991): 83–92. [Google Scholar] [CrossRef]
- Anusorn Singhapakdi, Scott J. Vitell, and Kenneth L. Kraft. “Moral intensity and ethical decision-making of marketing professionals.” Journal of Business Research 36 (1996): 245–55. [Google Scholar] [CrossRef]
- David Glen Mick. “Are studies of dark side variables confounded by socially desirable responding? The case of materialism.” Journal of Consumer Research 23 (1996): 106–19. [Google Scholar] [CrossRef]
- Delroy Paulhus. “Two-Component Models of Socially Desirable Responding.” Journal of Personality and Social Psychology 46 (1984): 598–609. [Google Scholar] [CrossRef]
- David Streiner, Geoffrey Norman, and John Cairney. Health Measurement Scales: A Practical Guide to Their Development and Use, 5th ed. New York: Oxford University Press, 2014. [Google Scholar]
- Joseph F. Hair, Marko Sarstedt, Torsten M. Pieper, and Christian M. Ringle. “The use of partial least squares structural equation modeling in strategic management research: A review of past practices and recommendations for future applications.” Long Range Planning 45 (2012): 320–40. [Google Scholar] [CrossRef]
- Joan M. McMahon, and Robert J. Harvey. “An analysis of the factor structure of Jones’ moral intensity construct.” Journal of Business Ethics 64 (2006): 381–404. [Google Scholar] [CrossRef]
- Hussain Al-Qatari. “Milking Health for All Its Worth.” Kuwait Times, 22 July 2011. [Google Scholar]
- Jennifer Kish-Gephart, David Harrison, and Linda Trevino. “Bad apples, bad cases, and bad barrels: Meta-analytic evidence about sources of unethical decision work.” Journal of Applied Psychology 95 (2010): 1–31. [Google Scholar] [CrossRef] [PubMed]
- Alan Berkowitz. “The social norms approach: Theory, research, and annotated bibliography.” 2004. Available online: alanberkowitz.com/articles/social_norms.pdf (accessed on 24 August 2015).
- Scott J. Vitell, Anusorn Singhapakdi, and James Thomas. “Consumer ethics: An application and empirical testing of the Hunt-Vitell theory of ethics.” Journal of Consumer Marketing 18 (2001): 153–78. [Google Scholar] [CrossRef]
- Donelson R. Forsyth. “Judging the morality of business practices: The influence of personal moral philosophies.” Journal of Business Ethics 11 (1992): 461–70. [Google Scholar] [CrossRef]
- Albert Bandura, Claudio Barbaranelli, Gian Caprara, and Concetta Pastorelli. “Mechanisms of moral disengagement in the exercise of moral agency.” Journal of Personality and Social Psychology 71 (1996): 364–74. [Google Scholar] [CrossRef]
- Amit Bhattacharjee, Jonathan Berman, and Americus Reed II. “Moral decoupling enables consumers to admire and admonish.” Journal of Consumer Research 39 (2013): 1167–84. [Google Scholar] [CrossRef]
- Albert Bandura. “Social cognitive theory: An agentic perspective.” Asian Journal of Social Psychology 2 (1999): 21–41. [Google Scholar] [CrossRef]
- Robert M. Groves. “Nonresponse rates and nonresponse bias in household surveys.” Public Opinion Quarterly 70 (2006): 646–75. [Google Scholar] [CrossRef]
- 1The aim of this Code is “to contribute to the provision of safe and adequate nutrition for infants, by the protection and promotion of breast-feeding, and by ensuring the proper use of breast-milk substitutes, when these are necessary, on the basis of adequate information and through appropriate marketing and distribution.” [12]. It also aims to promote breast-feeding, to take legislative and social action to facilitate breast-feeding by working mothers, and to regulate inappropriate sales promotion of infant foods that can be used to replace breast milk.
- 2A doctor prescription is needed only for special formula that pharmacies dispense under the request of a doctor (personal communication with Dr. Mona Alsumaie, Kuwait Breastfeeding Promotion & Baby Friendly Hospital Initiative (BFHI) Implementation Program Coordinator).
| Scenario 1 | Scenario 2 | |||
|---|---|---|---|---|
| Mean | Standard Deviation | Mean | Standard Deviation | |
| Magnitude of consequences | 5.4 | 1.6 | 5.4 | 1.9 |
| Social consensus | 5.7 | 1.2 | 4.3 | 2.2 |
| Probability of effects | 5.4 | 1.5 | 5.4 | 1.7 |
| Temporal immediacy | 4.7 | 1.9 | 5.0 | 1.8 |
| Proximity | 4.0 | 2.2 | 3.6 | 2.1 |
| Concentration of effect | 5.3 | 1.5 | 5.5 | 1.5 |
| Predictor | Average Variance Extracted | Composite Reliability | Beta | Standard Error | Two-tailed p-values |
|---|---|---|---|---|---|
| Company Promotion ➔ infant formula prescription (H1) | 0.90 | 0.96 | 0.45 | 0.06 | 0.000 |
| Hospital policy ➔ infant formula prescription (H2) | 0.75 | 0.90 | 0.35 | 0.05 | 0.000 |
| Mother’s attitude ➔ infant formula prescription (H3) | 0.76 | 0.90 | -0.12 | 0.04 | 0.000 |
| Moral Intensity (d1) ➔ infant formula prescription (H4) | 0.82 | 0.90 | -0.14 | 0.05 | 0.003 |
| Moral Intensity (d2) ➔ infant formula prescription (H4) | 0.66 | 0.79 | 0.05 | 0.05 | 0.35 |
| Infant formula prescription (Dependent Variable) | 0.66 | 0.79 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rios, R.; Riquelme, H.; El Beshlawy, S. Prescribing under the Influence: The Business of Breastmilk Substitutes. Soc. Sci. 2016, 5, 53. https://doi.org/10.3390/socsci5040053
Rios R, Riquelme H, El Beshlawy S. Prescribing under the Influence: The Business of Breastmilk Substitutes. Social Sciences. 2016; 5(4):53. https://doi.org/10.3390/socsci5040053
Chicago/Turabian StyleRios, Rosa, Hernan Riquelme, and Sharif El Beshlawy. 2016. "Prescribing under the Influence: The Business of Breastmilk Substitutes" Social Sciences 5, no. 4: 53. https://doi.org/10.3390/socsci5040053





