Residents of Central Queensland, Australia Are Aware of Healthy Eating Practices but Consume Unhealthy Diets
Abstract
:1. Introduction
2. Materials and Methods
2.1. Pilot Testing
2.2. Survey Methods
2.3. Survey Respondents
2.4. Survey Structure
2.5. Statistical Analyses
2.6. Nutritional Knowledge
2.7. Nutritional Behaviors
3. Results
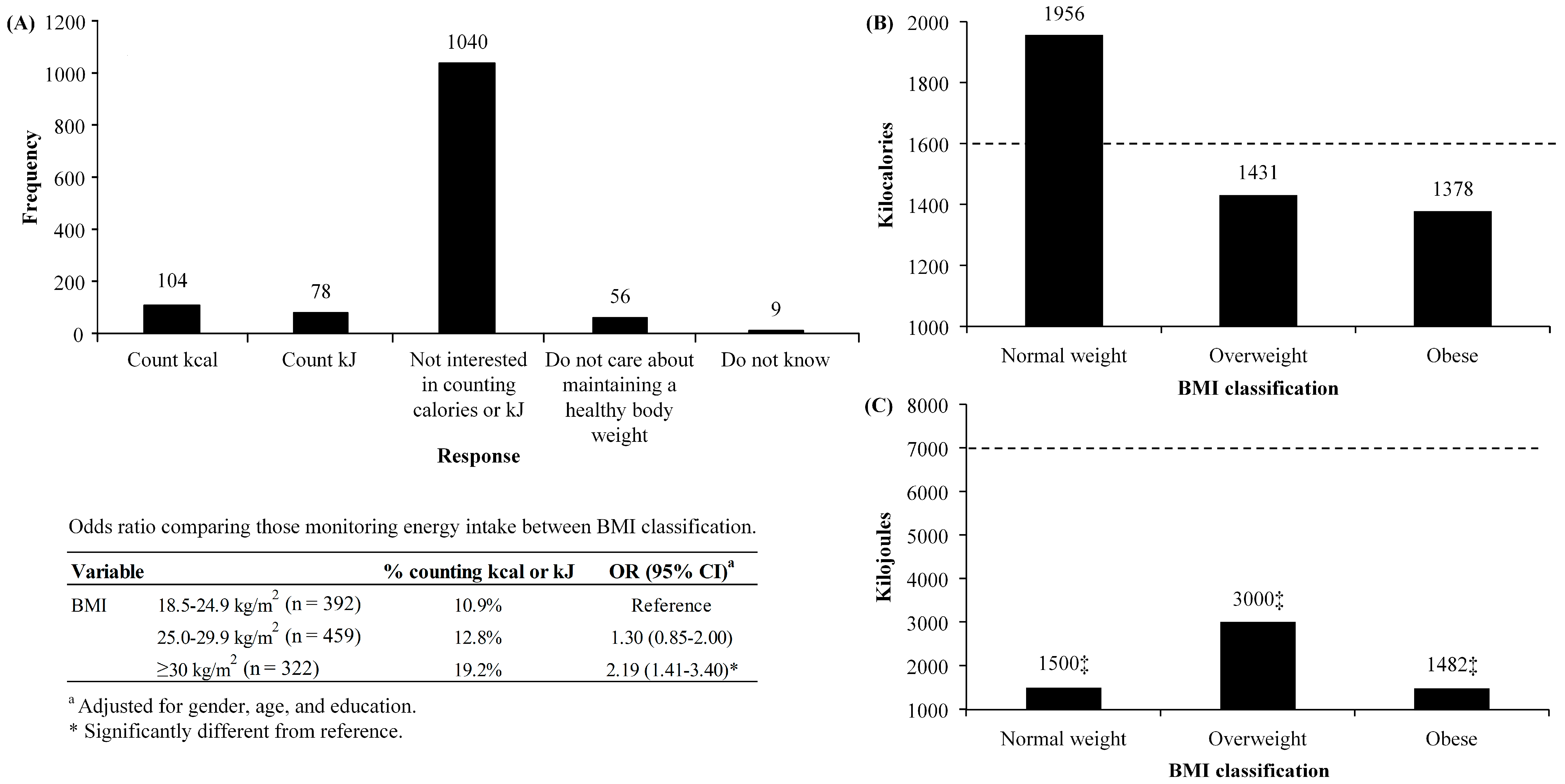
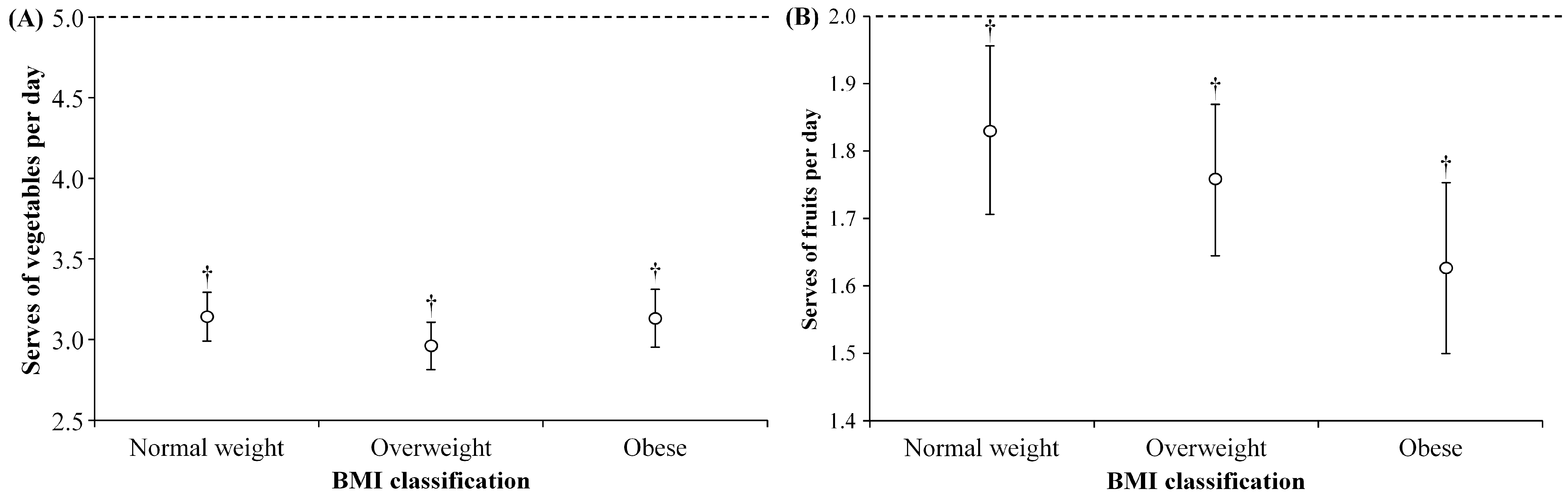
3.1. Nutritional Knowledge
3.2. Nutritional Behaviors
4. Discussion
5. Limitations
6. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Swinburn, B.; Caterson, I.; Seidell, J.; James, W. Diet, nutrition and the prevention of excess weight gain and obesity. Public Health Nutr. 2004, 7, 123–146. [Google Scholar] [PubMed]
- Australian Bureau of Statistics. 4364.0.55.003-Australian Health Survey: Updated Results, 2011–2012. Available online: http://www.abs.gov.au/ausstats/[email protected]/Lookup/33C64022ABB5ECD5CA257B8200179437?opendocument (accessed on 1 August 2017).
- Organisation for Economic Cooperation and Development (OECD). Health at A Glance 2011: OECD Indicators. Available online: http://dx.doi.org/10.1787/health_glance-2011-en (accessed on 1 August 2017).
- Access Economics. The Growing Cost of Obesity in 2008: Three Years On. Available online: https://www.diabetesaustralia.com.au/PageFiles/7830/FULLREPORTGrowingCostOfObesity2008.pdf (accessed on 5 August 2017).
- Begg, S.; Vos, T.; Barker, B.; Stevenson, C.; Stanley, L.; Lopez, A. Burden of Disease and Injury in Australia, 2003; Australian Institute of Health and Welfare: Canberra, Australia, 2007.
- National Heart, Lungs, and Blood Institute. Signs, Symptoms, and Complications. Available online: https://www.nhlbi.nih.gov/health/health-topics/topics/obe/signs (accessed on 8 November 2017).
- Dalbo, V.; Czerepusko, J.; Tucker, P.; Kingsley, M.; Moon, J.; Young, K.; Scanlan, A. Not sending the message: A low prevalence of strength-based exercise participation in rural and regional central queensland. Aust. J. Rural Health 2015, 23, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Price Waterhous Coopers. Weighing the Cost of Obesity: A Case for Action; Price Waterhouse Coopers: Canberra, Australia, 2015. [Google Scholar]
- Worsley, A. Nutrition knowledge and food consumption: Can nutrition knowledge change food behaviour? Asia Pac. J. Clin. Nutr. 2002, 11, S579–S585. [Google Scholar] [CrossRef] [PubMed]
- Barbosa, L.; Vasconcelos, S.; Correia, L.; Ferreira, R. Nutrition knowledge assessment studies in adults: A systematic review. Ciência Saúde Coletiva 2016, 21, 449–462. [Google Scholar] [CrossRef] [PubMed]
- Axelson, M.; Brinberg, D. The measurement and conceptualization of nutrition knowledge. J. Nutr. Educ. 1992, 24, 239–246. [Google Scholar] [CrossRef]
- Spronk, I.; Kullen, C.; Burdon, C.; O’Connor, H. Relationship between nutrition knowledge and dietary intake. Br. J. Nutr. 2014, 111, 1713–1726. [Google Scholar] [CrossRef] [PubMed]
- Wardle, J.; Parmeter, K.; Waller, J. Nutrition knowledge and food intake. Appetite 2000, 34, 269–275. [Google Scholar] [CrossRef] [PubMed]
- O’Dea, J.; Wilson, R. Socio-cognitive and nutritional factors associated with body mass index in children and adolescents: Possibilities for childhood obesity prevention. Health Educ. Res. 2006, 21, 796–805. [Google Scholar] [CrossRef] [PubMed]
- Hendrie, G.; Coveney, J.; Cox, D. Exploring nutrition knowledge and the demographic variation in knowledge levels in an australian community sample. Public Health Nutr. 2008, 11, 1365–1371. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, G.; Davies, M. Nutrition knowledge and body mass index. Health Educ. Res. 2007, 22, 571–575. [Google Scholar] [CrossRef] [PubMed]
- Reinehr, T.; Kersting, M.; Chahda, C.; Andler, W. Nutritional knowledge of obese compared to non obese children. Nutr. Res. 2003, 23, 645–649. [Google Scholar] [CrossRef]
- Dalbo, V.; Teramoto, M.; Roberts, M.; Scanlan, A. Lack of reality: Positive self-perceptions of health in the presence of disease. Sports 2017, 5, 23. [Google Scholar] [CrossRef]
- Acheampong, I.; Haldeman, L. Are nutrition knowledge, attitudes, and beliefs associated with obesity among low-income hispanic and african american women caretakers? J. Obes. 2013, 2013, 123901. [Google Scholar] [CrossRef] [PubMed]
- Humphries, B.; Duncan, M.; Mummery, W. Prevalence and correlates of resistance training in a regional australian population. Br. J. Sports Med. 2010, 44, 653–656. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, T.; Bauman, A.; Davies, J. Physical Activity Patterns of Australian Adults: Results of the 1999 National Physical Activity Survey; Australian Institute of Health and Welfare: Canberra, Australia, 2000.
- Brown, W.; Trost, S.; Bauman, A.; Mummery, K.; Owen, N. Test-retest reliability of four physical activity measures used in population surveys. J. Sci. Med. Sport 2004, 7, 205–215. [Google Scholar] [CrossRef]
- Frankenfield, D.; Roth-Yousey, L.; Compher, C.; Evidence Analysis Working Group. Comparison of predictive equations for resting metabolic rate in healthy nonobese and obese adults: A systematic review. J. Am. Diet. Assoc. 2005, 105, 775–789. [Google Scholar] [CrossRef] [PubMed]
- Elliott, D.; Walker, D. Evaluation of the National Go for 2 & 5 Campaign. Available online: www.healthyactive.gov.au/internet/healthyactive/publishing.nsf/Content/025D9EB302CAEC0ECA2572DC0017DEC8/$File/2&5-eval-jan07.pdf (accessed on 2 August 2017).
- Brown, K.; Timotijevic, L.; Barnett, J.; Shepherd, R.; Lähteenmäki, L.; Raats, M. A review of consumer awareness, understanding and use of food-based dietary guidelines. Br. J. Nutr. 2011, 106, 15–26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Food Standards Australia and New Zealand. Australia New Zealand Food Standards Code-Standard 1.2.8-Nutrition Information Requirements; Food Standards Australia and New Zealand: Canberra, Australia, 2016.
- National Health and Medical Research Council. Australian Dietary Guidelines. Available online: https://www.eatforhealth.gov.au/ (accessed on 1 August 2017).
- Australian Bureau of Statistics. 4364.0.55.007-Australian Health Survey: Nutrition First Results-Foods and Nutrients, 2011–2012. Available online: http://www.abs.gov.au/ausstats/[email protected]/Lookup/4364.0.55.007main+features12011-012 (accessed on 4 August 2017).
- Story, M.; Kaphingst, K.; Robinson-O’Brien, R.; Glanz, K. Creating healthy food and eating environments: Policy and environmental approaches. Annu. Rev. Public Health 2008, 29, 253–272. [Google Scholar] [CrossRef] [PubMed]
- Stark, L. Can nutrition counselling be more behavioural? Lessons learned from dietary management of cystic fibrosis. Proc. Nutr. Soc. 2007, 62, 793–799. [Google Scholar] [CrossRef] [PubMed]
- Toulabi, T.; Khosh Niyat Nikoo, M.; Amini, F.; Nazari, H.; Mardani, M. The influence of a behavior modification interventional program on body mass index in obese adolescents. J. Formos. Med. Assoc. 2012, 111, 153–159. [Google Scholar] [CrossRef] [PubMed]
- Australian Institute of Health and Welfare. Frisk Factors to Health. Available online: https://www.aihw.gov.au/reports/biomedical-risk-factors/risk-factors-to-health/contents/overweight-and-obesity (accessed on 8 November 2017).
| Question | Answer Choice(s) |
|---|---|
| Nutritional Knowledge | |
| Which of these fats is a poor food choice? | Saturated fat, unsaturated fat, Omega-3 fatty acids, don’t know/unsure |
| Which is a good choice to build or maintain muscle? | Protein (steak, chicken, fish), carbohydrate (potato, apple, orange), fat (cookies, ice cream), don’t know/unsure |
| How many calories should you consume per day to maintain your current body weight? | Open answer |
| How many kilojoules should you consume per day to maintain your current body weight? | Open answer |
| Nutritional Behavior | |
| How many servings of vegetable do you eat on a usual day? | Open answer |
| How many servings of fruit do you eat on a usual day? | Open answer |
| In the last week did you consume fast food? | Yes or no |
| What do you do to maintain a healthy body weight? | Count kilocalories, count kilojoules, not interested in counting kilocalories or kilojoules, do not care about maintaining a healthy body weight |
| Variable | Categories | % |
|---|---|---|
| Gender | Male | 64.6 |
| Female | 35.4 | |
| Age | 18–34 years | 30.9 |
| 35–44 years | 19.6 | |
| 45–54 years | 18.2 | |
| 55+ years | 31.4 | |
| Body Mass Index | <18.5 kg/m2 | 1.7 |
| 18.5–24.9 kg/m2 | 30.2 | |
| 25.0–29.9 kg/m2 | 35.4 | |
| ≥30 kg/m2 | 24.9 | |
| No response | 7.8 | |
| Household Income | Up to $26,000 | 12.5 |
| $26,001–$52,000 | 11.5 | |
| $52,001–$100,000 | 17.9 | |
| >$100,000 | 25.9 | |
| Don’t know/No response | 32.2 | |
| Years of Education | 1–10 years | 28.6 |
| 11–12 years | 25.9 | |
| 13–14 years | 16.1 | |
| 15+ years | 28.9 | |
| No schooling | 0.1 | |
| Don’t know/No response | 0.4 |
| BMI Classification | % Correct | OR (95% CI) * | |
|---|---|---|---|
| Ability to Choose the Correct Answer Regarding Types of Dietary Fats | |||
| Normal | 18.5–24.9 kg/m2 (N = 392) | 73.5% | Reference |
| Overweight | 25.0–29.9 kg/m2 (N = 459) | 71.9% | 1.18 (0.83–1.69) |
| Obese | ≥30 kg/m2 (N = 322) | 77.0% | 0.90 (0.38–2.14) |
| Ability to Choose the Correct Answer Regarding Protein in the Diet | |||
| Normal | 18.5–24.9 kg/m2 (N = 392) | 80.4% | Reference |
| Overweight | 25.0–29.9 kg/m2 (N = 459) | 78.9% | 1.06 (0.75–1.50) |
| Obese | ≥30 kg/m2 (N = 322) | 78.9% | 1.08 (0.74–1.59) |
| BMI Classification | % Eating Fast Food | OR (95% CI) * | |
|---|---|---|---|
| Normal | 18.5–24.9 kg/m2 (N = 391) | 48.3% | Reference |
| Overweight | 25.0–29.9 kg/m2 (N = 460) | 53.7% | 1.52 (1.13–2.04) # |
| Obese | ≥30 kg/m2 (N = 322) | 50.9% | 1.43 (1.04–1.98) # |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dalbo, V.J.; Hiskens, M.I.; Teramoto, M.; Kingsley, M.I.; Young, K.C.; Scanlan, A.T. Residents of Central Queensland, Australia Are Aware of Healthy Eating Practices but Consume Unhealthy Diets. Sports 2017, 5, 94. https://doi.org/10.3390/sports5040094
Dalbo VJ, Hiskens MI, Teramoto M, Kingsley MI, Young KC, Scanlan AT. Residents of Central Queensland, Australia Are Aware of Healthy Eating Practices but Consume Unhealthy Diets. Sports. 2017; 5(4):94. https://doi.org/10.3390/sports5040094
Chicago/Turabian StyleDalbo, Vincent J., Matthew I. Hiskens, Masaru Teramoto, Michael I. Kingsley, Kaelin C. Young, and Aaron T. Scanlan. 2017. "Residents of Central Queensland, Australia Are Aware of Healthy Eating Practices but Consume Unhealthy Diets" Sports 5, no. 4: 94. https://doi.org/10.3390/sports5040094







