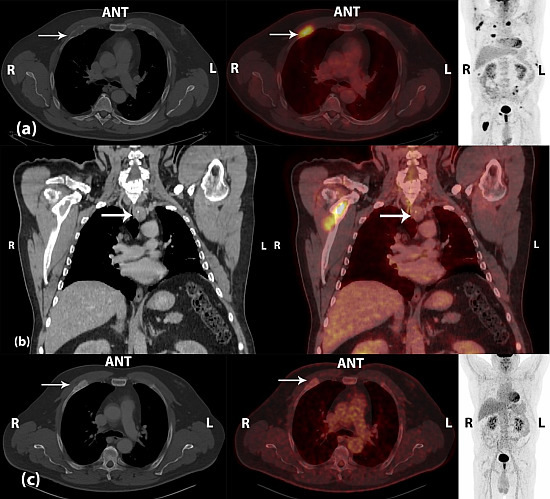
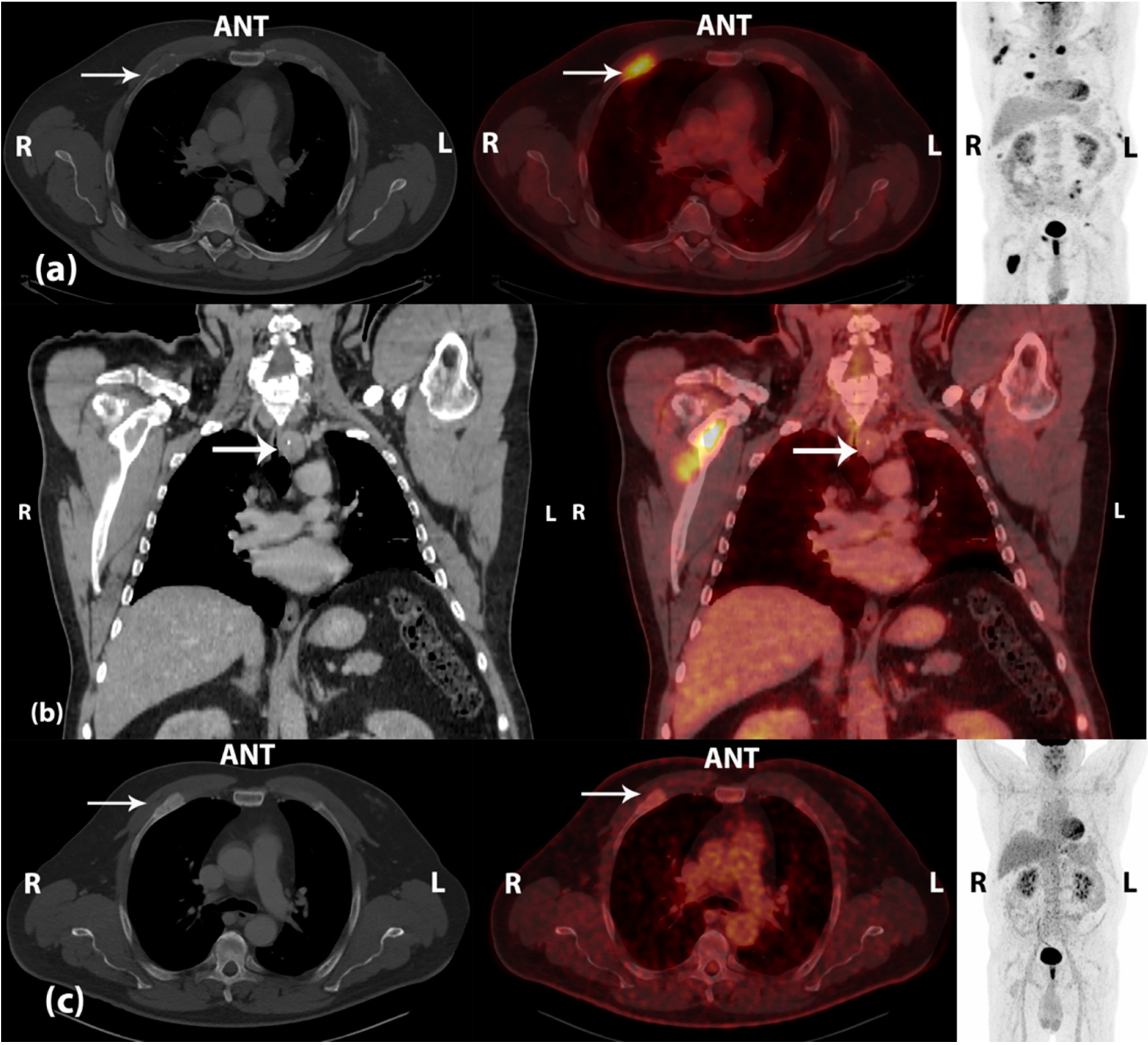
Brown Tumors Due to Primary Hyperparathyroidism in a Patient with Parathyroid Carcinoma Mimicking Skeletal Metastases on 18F-FDG PET/CT
Abstract
:
Conflicts of Interest
References
- Villar-del-Moral, J.; Jimenez-Garcia, A.; Salvador-Egea, P.; Martos-Martinez, J.M.; Nuno-Vazquez-Garza, J.M.; Serradilla-Martin, M.; Gomez-Palacios, A.; Moreno-Llorente, P.; Ortega-Serrano, J.; de la Quintana-Basarrate, A. Prognostic factors and staging systems in parathyroid cancer: A multicenter cohort study. Surgery 2014, 156, 1132–1144. [Google Scholar] [CrossRef] [PubMed]
- Evangelista, L.; Sorgato, N.; Torresan, F.; Boschin, I.M.; Pennelli, G.; Saladini, G.; Piotto, A.; Rubello, D.; Pelizzo, M.R. FDG-PET/CT and parathyroid carcinoma: Review of literature and illustrative case series. World J. Clin. Oncol. 2011, 2, 348–354. [Google Scholar] [CrossRef] [PubMed]
- Hindie, E.; Zanotti-Fregonara, P.; Tabarin, A.; Rubello, D.; Morelec, I.; Wagner, T.; Henry, J.F.; Taieb, D. The role of radionuclide imaging in the surgical management of primary hyperparathyroidism. J. Nucl. Med. 2015, 56, 737–744. [Google Scholar] [CrossRef] [PubMed]
- Gamelli, R.L.; Liu, H.; He, L.K.; Hofmann, C.A. Augmentations of glucose uptake and glucose transporter-1 in macrophages following thermal injury and sepsis in mice. J. Leukoc. Biol. 1996, 59, 639–647. [Google Scholar] [PubMed]
- Kerstens, M.N.; de Vries, R.; Plukker, J.T.; Slart, R.H.; Dullaart, R.P. Multiple skeletal lesions on FDG PET in severe primary hyperparathyroidism. Eur. J. Nucl. Med. Mol. Imaging 2014, 41, 182–183. [Google Scholar] [CrossRef] [PubMed]
- Kuwahara, K.; Izawa, S.; Murabe, H.; Murakami, N.; Yokota, T.; Wani, Y.; Notohara, K.; Tsukayama, C.; Ishimori, T.; Watanabe, Y. Increased 18F-fluorodeoxyglucose uptake in a brown tumor in a patient with primary hyperparathyroidism. J. Clin. Endocrinol. Metab. 2007, 92, 2408–2409. [Google Scholar] [CrossRef] [PubMed]
- Shim, H.K.; Kim, B.S. 18F-FDG PET findings of a parathyroid cancer with cortical skeletal demineralization. Clin. Nucl. Med. 2012, 37, 293–295. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Andersen, K.F.; Albrecht-Beste, E. Brown Tumors Due to Primary Hyperparathyroidism in a Patient with Parathyroid Carcinoma Mimicking Skeletal Metastases on 18F-FDG PET/CT. Diagnostics 2015, 5, 290-293. https://doi.org/10.3390/diagnostics5030290
Andersen KF, Albrecht-Beste E. Brown Tumors Due to Primary Hyperparathyroidism in a Patient with Parathyroid Carcinoma Mimicking Skeletal Metastases on 18F-FDG PET/CT. Diagnostics. 2015; 5(3):290-293. https://doi.org/10.3390/diagnostics5030290
Chicago/Turabian StyleAndersen, Kim Francis, and Elisabeth Albrecht-Beste. 2015. "Brown Tumors Due to Primary Hyperparathyroidism in a Patient with Parathyroid Carcinoma Mimicking Skeletal Metastases on 18F-FDG PET/CT" Diagnostics 5, no. 3: 290-293. https://doi.org/10.3390/diagnostics5030290