Optimal Elbow Angle for Extracting sEMG Signals During Fatiguing Dynamic Contraction
Abstract
:1. Introduction
2. Methods
2.1. Data Recording and Pre-Processing
2.2. Labelling the Signals
2.3. Genetic Algorithms
| Parameter | Value |
|---|---|
| Independent runs | 26 |
| Population size | 5000 |
| Maximum number of generations | 20 |
| Mutation probability | 10% |
| Crossover probability | 90% |
| Selection type | Tournament, size 5 |
| Termination criterion | Maximum number of generations |
2.4. Evolved Elbow Angle Selection

2.5. Classification
2.6. Feature Extraction Techniques
- Higher-order statistics (HOS) (HO2 and HO3 were used as they gave the best results.)
- Mean Frequency (MF)
- Median Frequency (MDF)
- Power Spectrum Density (PSD)
- Root Mean Square (RMS)
- Daubechies 4 (Db4)
- Mexican Hat (Mex H)
- Pseudo-wavelet (p-w)
3. Results
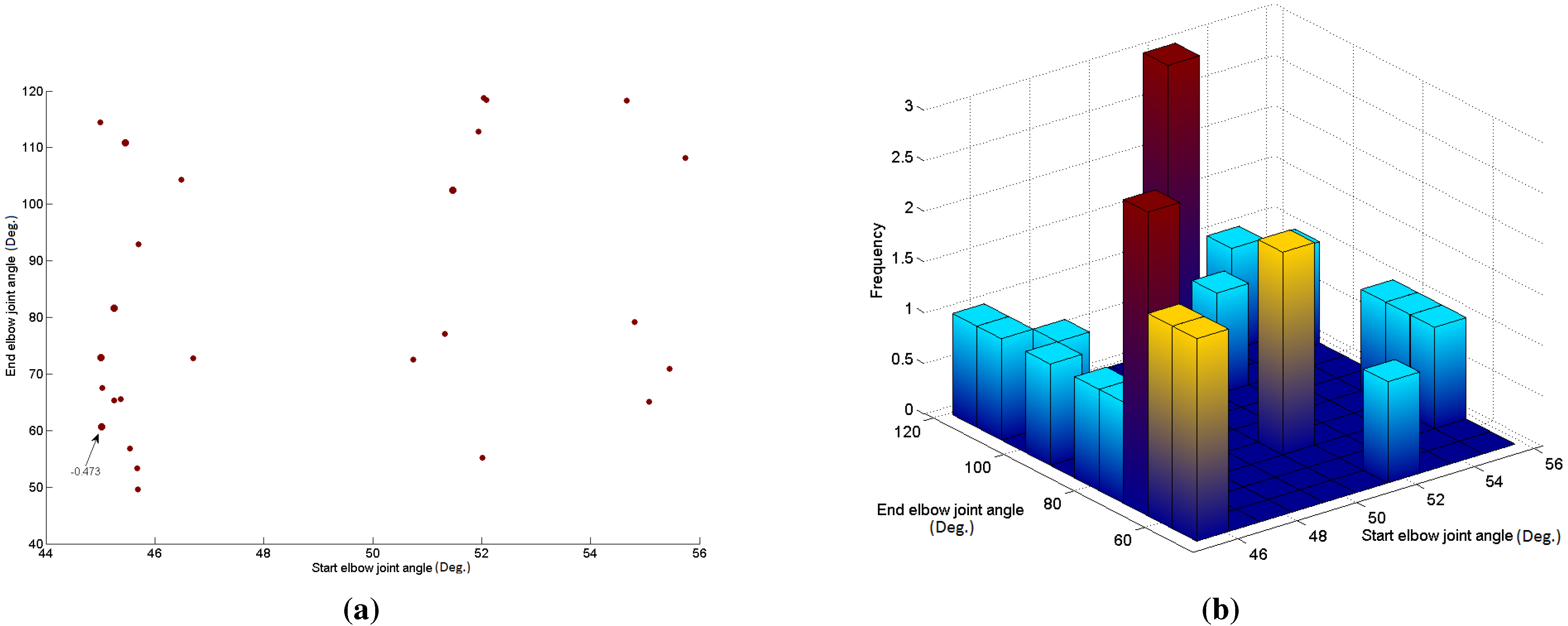
| GA Run | Elbow Joint 1 | Elbow Joint 2 | DBI |
|---|---|---|---|
| 1 | 54.66 | 118.27 | –0.491 |
| 2 | 54.81 | 79.13 | –0.483 |
| 3 | 55.74 | 108.17 | –0.486 |
| 4 | 55.08 | 65.12 | –0.487 |
| 5 | 55.46 | 70.93 | –0.491 |
| 6 | 50.75 | 72.56 | –0.494 |
| 7 | 46.71 | 72.78 | –0.483 |
| 8 | 51.33 | 77.10 | –0.482 |
| 9 | 45.55 | 56.87 | –0.492 |
| 10 | 45.01 | 72.87 | –0.475 |
| 11 | 52.08 | 118.39 | –0.503 |
| 12 | 45.25 | 81.60 | –0.474 |
| 13 | 45.45 | 110.82 | –0.478 |
| 14 | 52.04 | 118.76 | –0.503 |
| 15 | 51.94 | 112.88 | –0.491 |
| 16 | 45.69 | 49.57 | –0.498 |
| 17 | 45.68 | 53.35 | –0.481 |
| 18 | 51.47 | 102.53 | –0.478 |
| 19 | 45.02 | 60.63 | –0.473 |
| 20 | 46.49 | 104.29 | –0.505 |
| 21 | 45.70 | 92.98 | –0.490 |
| 22 | 45.37 | 65.55 | –0.498 |
| 23 | 45.26 | 65.36 | –0.494 |
| 24 | 52.01 | 55.24 | –0.491 |
| 25 | 45.00 | 114.42 | –0.500 |
| 26 | 45.03 | 67.56 | –0.506 |
| Average | 49.02 | 83.37 | –0.49 |
| St. Dev | 4.07 | 23.35 | 0.01 |
| Subjects | HO2 | HO3 | Mean Freq | Median Freq | PSd | RMS | Db4 | Mexican Hat | P-W |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 83.58 | 83.58 | 88.06 | 82.84 | 80.60 | 88.29 | 86.57 | 17.16 | 90.99 |
| 2 | 94.89 | 91.97 | 94.89 | 89.05 | 90.51 | 96.35 | 93.43 | 90.51 | 94.16 |
| 3 | 79.69 | 76.56 | 78.91 | 66.41 | 74.22 | 78.91 | 85.16 | 69.53 | 85.94 |
| 4 | 68.52 | 67.28 | 82.72 | 74.07 | 64.20 | 82.72 | 83.95 | 80.25 | 88.27 |
| 5 | 74.12 | 71.93 | 80.70 | 73.25 | 71.49 | 79.39 | 83.77 | 79.39 | 81.58 |
| 6 | 86.79 | 88.68 | 91.51 | 83.96 | 86.79 | 89.62 | 90.57 | 84.91 | 93.40 |
| 7 | 75.17 | 73.15 | 83.89 | 79.19 | 71.14 | 83.22 | 77.18 | 83.89 | 82.55 |
| 8 | 73.33 | 74.81 | 71.11 | 65.19 | 75.56 | 73.33 | 79.26 | 71.11 | 87.41 |
| 9 | 91.18 | 89.71 | 88.24 | 85.29 | 91.18 | 92.65 | 94.12 | 89.71 | 92.65 |
| 10 | 71.19 | 68.64 | 83.05 | 74.58 | 69.49 | 81.36 | 85.59 | 77.97 | 86.44 |
| 11 | 59.46 | 63.06 | 63.96 | 66.67 | 62.16 | 67.57 | 81.98 | 67.57 | 93.69 |
| 12 | 53.44 | 53.05 | 62.60 | 53.82 | 56.49 | 64.50 | 64.12 | 53.05 | 83.59 |
| 13 | 69.14 | 69.14 | 82.72 | 79.01 | 66.67 | 83.95 | 82.10 | 83.33 | 82.10 |
| Average | 75.42 | 74.74 | 80.95 | 74.87 | 73.88 | 81.68 | 83.68 | 72.95 | 87.90 |
| St. Dev | 11.87 | 11.32 | 9.81 | 9.88 | 10.83 | 9.25 | 7.72 | 19.65 | 4.67 |

4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Garrett, W.E. Muscle strain injuries: Clinical and basic aspects. Med. Sci. Sports Exerc. 1990, 22, 436–443. [Google Scholar] [CrossRef] [PubMed]
- Edwards, R. Human muscle function and fatigue. Ciba Found. Symp. 1981, 82, 1–18. [Google Scholar] [PubMed]
- Lindstrom, L.; Kadefors, R.; Petersen, I. An electromyographic index for localized muscle fatigue. J. Appl. Physiol. 1977, 43, 750–754. [Google Scholar] [PubMed]
- Masuda, K.; Masuda, T.; Sadoyama, T.; Inaki, M.; Katsuta, S. Changes in surface EMG parameters during static and dynamic fatiguing contractions. J. Electromyogr. Kinesiol. 1999, 9, 39–46. [Google Scholar] [CrossRef]
- Ravier, P.; Buttelli, O.; Jennane, R.; Couratier, P. An EMG fractal indicator having different sensitivities to changes in force and muscle fatigue during voluntary static muscle contractions. J. Electromyogr. Kinesiol. 2005, 15, 210–221. [Google Scholar] [CrossRef] [PubMed]
- Onishi, H.; Yagi, R.; Oyama, M.; Akasaka, K.; Ihashi, K.; Handa, Y. EMG-angle relationship of the hamstring muscles during maximum knee flexion. J. Electromyogr. Kinesiol. 2002, 5, 399–406. [Google Scholar] [CrossRef]
- Okada, M. Effect of muscle length on surface EMG wave forms in isometric contractions. Eur. J. Appl. Physiol. Occup. Physiol. 1987, 56, 482–486. [Google Scholar] [CrossRef] [PubMed]
- Doud, J.R.; Walsh, J.M. Muscle fatigue and muscle length interaction: Effect on the EMG frequency components. Electromyogr. Clin. Neurophysiol. 1995, 35, 331–339. [Google Scholar] [PubMed]
- Nosaka, K.; Sakamoto, K. Effect of elbow joint angle on the magnitude of muscle damage to the elbow flexors. Med. Sci. Sports Exerc. 2001, 33, 22–29. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, L.F.; Matta, T.T.; Alves, D.S.; Garcia, M.A.; Vieira, T.M. Effect of the shoulder position on the biceps brachii EMG in different dumbbell curls. J. Sports Sci. Med. 2009, 8, 24–29. [Google Scholar] [PubMed]
- Kumar, D.K.; Pah, N.D.; Bradley, A. Wavelet analysis of surface electromyography to determine muscle fatigue. IEEE Trans. Neural. Syst. Rehabil. Eng. 2003, 11, 400–406. [Google Scholar] [CrossRef] [PubMed]
- Bonato, P.; Roy, S.H.; Knaflitz, M.; de Luca, C.J. Time-frequency parameters of the surface myoelectric signal for assessing muscle fatigue during cyclic dynamic contractions. IEEE Trans. Neural. Syst. Rehabil. Eng. 2001, 48, 745–753. [Google Scholar] [CrossRef] [PubMed]
- Karlsson, S.; Yu, J.; Akay, M. Enhancement of spectral analysis of myoelectric signals during static contractions using wavelet methods. IEEE Trans.Biomed. Eng. 1999, 46, 670–684. [Google Scholar] [CrossRef] [PubMed]
- Sparto, P.J.; Parnianpour, M.; Barria, E.A.; Jagadeesh, J.M. Wavelet analysis of electromyography for back muscle fatigue detection during isokinetic constant-torque exertions. Spine 1999, 24, 1791–1798. [Google Scholar] [CrossRef] [PubMed]
- Khezri, M.; Jahed, M. Real-time intelligent pattern recognition algorithm for surface EMG signals. Biomed. Eng. Online 2007. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.; Yan, Z.; Hu, X.; Xie, H.; Wang, Z. Classification of surface EMG signals using harmonic wavelet packet transform. Physiol. Meas. 2007, 27, 1255–1267. [Google Scholar] [CrossRef] [PubMed]
- Venugopal, G.; Navaneethakrishna, M.; Ramakrishnan, S. Extraction and analysis of multiple time window features associated with muscle fatigue conditions using semg signals. Expert Syst. Appl. 2014, 41, 2652–2659. [Google Scholar] [CrossRef]
- Li, Z.; Hayashibe, M.; Fattal, C.; Guiraud, D. Muscle fatigue tracking with evoked EMG via recurrent neural network: Toward personalized neuroprosthetics. Comput. Intell. Mag. IEEE 2014, 9, 38–46. [Google Scholar] [CrossRef]
- Moshou, D.; Hostens, I.; Papaioannou, G.; Ramon, H. Dynamic muscle fatigue detection using self-organizing maps. Appl. Soft Comput. 2005, 5, 391–398. [Google Scholar] [CrossRef]
- Kattan, A.; Al-Mulla, M.R.; Sepulveda, F.; Poli, R. Detecting localised muscle fatigue during isometric contraction using genetic programming. In Proceedings of the IJCCI, Madeira, Portugal, 5–7 October 2009; pp. 292–297.
- Al-Mulla, M.R.; Sepulveda, F.; Colley, M.; Kattan, A. Classification of localized muscle fatigue with genetic programming on sEMG during isometric contraction. In Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society EMBC, Minneapolis, MN, USA, 3–6 September 2009; pp. 2633–2638.
- Al-Mulla, M. Evolutionary computation extracts a super sEMG feature to classify localized muscle fatigue during dynamic contractions. In Proceedings of the Computer Science and Electronic Engineering Conference (CEEC), Essex, UK, 12–13 September 2012; pp. 220–224.
- Al-Mulla, M.R.; Sepulveda, F.; Colley, M. Evolved pseudo-wavelet function to optimally decompose sEMG for automated classification of localized muscle fatigue. Med. Eng. Phys. 2011, 33, 411–417. [Google Scholar] [CrossRef] [PubMed]
- Al-Mulla, M.R.; Sepulveda, F.; Colley, M.; Al-Mulla, F. Statistical class separation using sEMG features towards automated muscle fatigue detection and prediction. In Proceedings of the International Congress on Image and Signal Processing, Tianjin, China, 17–19 October 2009; pp. 1–5.
- Al-Mulla, M.R.; Sepulveda, F. A Novel Feature Assisting in the Prediction of sEMG Muscle Fatigue Towards a Wearable Autonomous System. In Proceedings of the 16th IEEE International Mixed-Signals, Sensors and Systems Test Workshop (IMS3TW’10), La Grande Motte, France, 7–9 June 2010.
- Al-Mulla, M.R.; Sepulveda, F. Novel feature modelling the prediction and detection of sEMG muscle fatigue towards an automated wearable system. Sensors 2010, 10, 4838–4854. [Google Scholar] [CrossRef] [PubMed]
- Al-Mulla, M.R.; Sepulveda, F. Predicting the time to localized muscle fatigue using ANN and evolved sEMG feature. In Proceedings of the IEEE International Conference on Autonomous and Intelligent Systems, (AIS 2010), Povoa de Varzim, Portugal, 21–23 July 2010; pp. 1–6.
- Al-Mulla, M.R.; Sepulveda, F.; Colley, M. An autonomous wearable system for predicting and detecting localised muscle fatigue. Sensors 2011, 11, 1542–1557. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Al-Mulla, M.R.; Sepulveda, F. Novel pseudo-wavelet function for MMG signal extraction during dynamic fatiguing contractions. Sensors 2014, 14, 9489–9504. [Google Scholar] [CrossRef] [PubMed]
- Al-Mulla, M.R.; Sepulveda, F. Super wavelet for sEMG signal extraction during dynamic fatiguing contractions. J. Med. Syst. 2015, 39, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Al-Mulla, M.R.; Sepulveda, F.; Souod, M. Optimal Elbow Angle for MMG Signal Classification of Biceps Brachii during Dynamic Fatiguing Contraction. In Proceedings of the IWBBIO, International Work-Conference on Bioinformatics and Biomedical Engineering, Granada, Spain, 15–17 April 2015.
- Konrad, P. The ABC of EMG: A Practical Introduction to Kinesiological Electromyography; Noraxon, Inc.: Scottsdale, AZ, USA, 2005. [Google Scholar]
- Michalewicz, Z. Genetic Algorithms + Data Structures = Evolution Programs; Springer-Verlag: New York, NY, USA, 1996. [Google Scholar]
- Sepulveda, F.; Meckes, M.; Conway, B. Cluster separation index suggests usefulness of non-motor EEG channels in detecting wrist movement direction intention. In Proceedings of the IEEE Conference on Cybernetics and Intelligent Systems, Singapore, 1–3 December 2004; pp. 943–947.
- Merletti, R.; Farina, D.; Gazzoni, M. The linear electrode array: A useful tool with many applications. J. Electromyogr. Kinesiol. 2003, 13, 37–47. [Google Scholar] [CrossRef]
- De Luca, C.J. The use of surface electromyography in biomechanics. J. Appl. Biomech. 1997, 13, 135–163. [Google Scholar]
- Ortengren, R.; Andersson, G.; Broman, H.; Magnusson, R.; Petersen, I. Vocational electromyography: Studies of localized muscle fatigue at the assembly line. Ergonomics 1975, 18, 157–174. [Google Scholar] [CrossRef] [PubMed]
- Hagberg, M. Work load and fatigue in repetitive arm elevations. Ergonomics 1981, 24, 543–555. [Google Scholar] [CrossRef] [PubMed]
- Raez, M.B.; Hussain, M.S.; Mohd-Yasin, F. Techniques of EMG signal analysis: Detection, processing, classification and applications. Biol. Proc. Online 2006, 8, 11–35. [Google Scholar] [CrossRef] [PubMed]
- Walker, J.S. A Primer on Wavelets and Their Scientific Applications; Chapman and Hall/CRC: Boca Raton Fla, FL, USA, 2000. [Google Scholar]
- Mamghani, N.K.; Shimomura, Y.; Iwanaga, K.; Katsuur, T. Mechanomyogram and Electromyogram Responses of Upper Limb during Sustained Isometric Fatigue with Varying Shoulder and Elbow Postures. J. Physiol. Anthropol. 2002, 21, 29–43. [Google Scholar] [CrossRef]
- Al-Mulla, M.R.; Sepulveda, F.; Al-Bader, B. Optimal Elbow Angle for Extraction of sEMG and MMG Signals During Dynamic Fatiguing Contractions, Mobihealth. In Proceedings of the 5th EAI International Conference on Wireless Mobile Communication and Healthcare—Transforming Healthcare Through Innovations in Mobile And Wireless Technologies, London, UK, 14–16 October 2015. in press.
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Mulla, M.R.; Sepulveda, F.; Al-Bader, B. Optimal Elbow Angle for Extracting sEMG Signals During Fatiguing Dynamic Contraction. Computers 2015, 4, 251-264. https://doi.org/10.3390/computers4030251
Al-Mulla MR, Sepulveda F, Al-Bader B. Optimal Elbow Angle for Extracting sEMG Signals During Fatiguing Dynamic Contraction. Computers. 2015; 4(3):251-264. https://doi.org/10.3390/computers4030251
Chicago/Turabian StyleAl-Mulla, Mohamed R., Francisco Sepulveda, and Bader Al-Bader. 2015. "Optimal Elbow Angle for Extracting sEMG Signals During Fatiguing Dynamic Contraction" Computers 4, no. 3: 251-264. https://doi.org/10.3390/computers4030251





