Performance of a RT-PCR Assay in Comparison to FISH and Immunohistochemistry for the Detection of ALK in Non-Small Cell Lung Cancer
Abstract
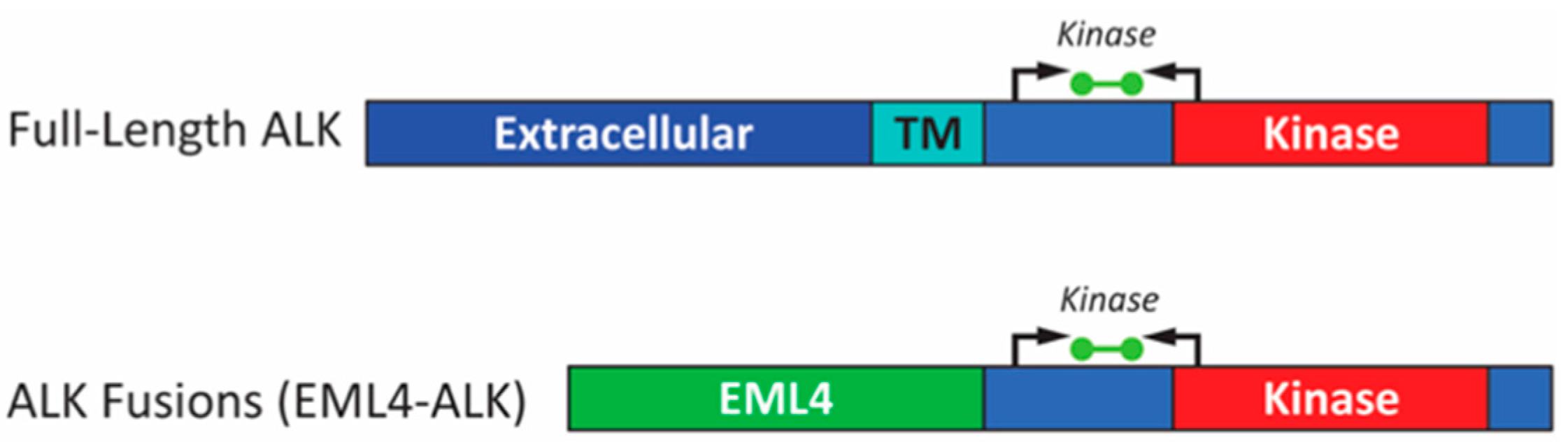
:1. Introduction
2. Results
2.1. Clinicopathological Characteristics
2.2. Sensitivity and Specificity of RT-PCR Compared to FISH
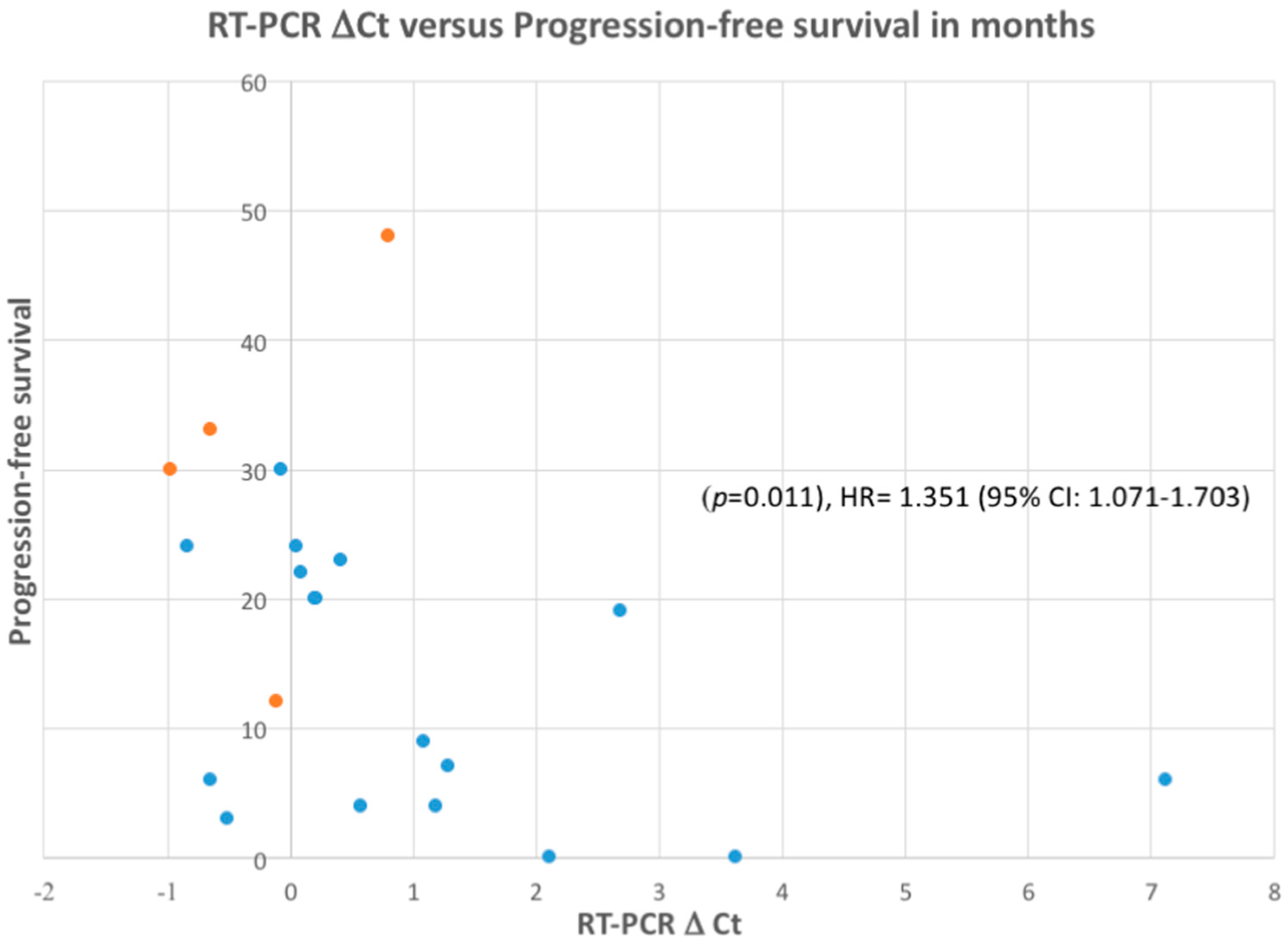
2.3. Correlation of RT-PCR, FISH and IHC with Response to ALK Inhibitor Therapy
2.4. Samples with Insufficient Tumor Content for IHC and FISH
3. Discussion
4. Materials and Methods
4.1. Patients and Tumor Samples
4.2. Immunohistochemistry
4.3. Fluorescence in Situ Hybridization
4.4. ALK RT-PCR
4.5. Sanger Sequencing
4.6. Next-Generation Sequencing
4.7. Statistical Analysis
5. Conclusions
Acknowledgments
Authors Contributions
Conflicts of Interest
References
- Morris, S.W.; Kirstein, M.N.; Valentine, M.B.; Dittmer, M.G.; Shapiro, D.N.; Saltman, D.L.; Look, A.T. Fusion of a kinase gene, ALK, to a nucleolar protein gene, NPM, in non-Hodgkin’s lymphoma. Science 1994, 263, 1281–1284. [Google Scholar] [CrossRef] [PubMed]
- Soda, M.; Choi, Y.L.; Enomoto, M.; Takada, S.; Yamashita, Y.; Ishikawa, S.; Fujiwara, S.; Watanabe, H.; Kurashina, K.; Hatanaka, H.; et al. Identification of the transforming EML4-ALK fusion gene in non-small cell lung cancer. Nature 2007, 448, 561–566. [Google Scholar] [CrossRef] [PubMed]
- Malik, S.M.; Maher, V.E.; Bijwaard, K.E.; Becker, R.L.; Zhang, L.; Tang, S.W.; Song, P.; Liu, Q.; Marathe, A.; Gehrke, B.; et al. U.S. Food and Drug Administration approval: Crizotinib for treatment of advanced or metastatic non-small cell lung cancer that is anaplastic lymphoma kinase positive. Clin. Cancer Res. 2014, 20, 2029–2034. [Google Scholar] [CrossRef] [PubMed]
- Shaw, A.T.; Kim, D.W.; Nakagawa, K.; Takashi, S.; Crino, L.; Ahn, M.-J.; De Pas, T.; Besse, B.; Solomon, B.J.; Blackhall, F.; et al. Crizotinib versus chemotherapy in advanced ALK-positive lung cancer. N. Engl. J. Med. 2013, 368, 2385–2394. [Google Scholar] [CrossRef] [PubMed]
- Shaw, A.T.; Kim, D.W.; Mehra, R.; Tan, D.S.W.; Felip, E.; Chow, L.Q.M.; Camidge, D.R.; Vansteenkiste, J.; Sharma, S.; De Pas, T.; et al. Ceritinib in ALK-rearranged non-small-cell lung cancer. N. Engl. J. Med. 2014, 370, 1189–1197. [Google Scholar] [CrossRef] [PubMed]
- Teixidó, C.; Karachaliou, N.; Peg, V.; Gimenez-Capitan, A.; Rosell, R. Concordance of IHC, FISH and RT-PCR for EML4-ALK rearrangements. Transl. Lung Cancer Res. 2014, 3, 70–74. [Google Scholar]
- Doshi, S.; Ray, D.; Stein, K.; Zhang, J.; Koduru, P.; Fogt, F.; Wellman, A.; Wat, R.; Mathews, C. Economic analysis of alternative strategies for detection of ALK rearrangements in non small cell lung cancer. Diagnostics 2016, 6, 4. [Google Scholar] [CrossRef] [PubMed]
- Ying, J.; Guo, L.; Qiu, T.; Shan, L.; Ling, Y.; Liu, X.; Lu, N. Diagnostic value of a novel fully automated immunochemistry assay for detection of ALK rearrangement in primary lung adenocarcinoma. Ann. Oncol. 2013, 24, 2589–2593. [Google Scholar] [CrossRef] [PubMed]
- Mattsson, J.S.; Brunnström, H.; Jabs, V.; Edlund, K.; Jirström, K.; Mindus, S.; la Fleur, L.; Pontén, F.; Karlsson, M.G.; Karlsson, C.; et al. Inconsistent results in the analysis of ALK rearrangements in non-small cell lung cancer. BMC Cancer 2016, 16, 603. [Google Scholar] [CrossRef] [PubMed]
- Cutz, J.C.; Craddock, K.J.; Torlakovic, E.; Brandao, G.; Carter, R.F.; Bigras, G.; Deschenes, J.; Izevbaye, I.; Xu, Z.; Greer, W.; et al. Canadian anaplastic lymphoma kinase study: A model for multicenter standardization and optimization of ALK testing in lung cancer. J. Thorac. Oncol. 2014, 9, 1255–1263. [Google Scholar] [CrossRef] [PubMed]
- Conde, E.; Hernandez, S.; Prieto, M.; Martinez, R.; Lopez-Rios, F. Profile of Ventana ALK (D5F3) companion diagnostic assay for non-small-cell lung carcinomas. Expert Rev. Mol. Diagn. 2016, 6, 707–713. [Google Scholar] [CrossRef] [PubMed]
- Savic, S.; Diebold, J.; Zimmermann, A.K.; Jochum, W.; Baschiera, B.; Grieshaber, S.; Tornillo, L.; Bisig, B.; Kerr, K.; Bubendorf, L. Screening for ALK in non-small cell lung carcinomas: 5A4 and D5F3 antibodies perform equally well, but combined use with FISH is recommended. Lung Cancer 2015, 89, 104–109. [Google Scholar] [CrossRef] [PubMed]
- Marchetti, A.; Di Lorito, A.; Pace, MV.; Iezzi, M.; Felicioni, L.; D’Antuono, T.; Filice, G.; Guetti, L.; Mucilli, F.; Buttitta, F. ALK protein analysis by IHC staining after recent regulatory changes: A comparison of two widely used approaches, revision of the literature, and a new testing algorithm. J. Thorac. Oncol. 2016, 11, 487–495. [Google Scholar] [CrossRef] [PubMed]
- Gruber, K.; Horn, H.; Kalla, J.; Fritz, P.; Rosenwald, A.; Kohlhaufl, M.; Friedel, G.; Schwab, M.; Ott, G.; Kalla, C. Detection of the rearrangements and transcriptional up-regulation of ALK in FFPE lung cancer specimens using a novel, sensitive, quantitative reverse transcription polymerase reaction assay. J. Thorac. Oncol. 2014, 9, 307–315. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Pepper, K.; Hendrickson, H.; Cagle, P.T.; Portier, B.P. Clinical validation of a novel commercial reverse transcription-quantitative polymerase chain reaction screening assay for detection of ALK translocations and amplifications in non-small cell lung carcinomas. Arch. Pathol. Lab. Med. 2016, 140, 690–693. [Google Scholar] [CrossRef] [PubMed]
- Marchetti, A.; Pace, M.A.; Di Lorito, A.; Canarecci, S.; Felicioni, L.; D’Antuono, T.; Liberatore, M.; Filice, G.; Guetti, L.; Mucilli, F.; et al. Validation of a new algorithm for a quick and easy RT-PCR-based ALK test in a large series of lung adenocarcinomas: Comparison with FISH, immunohistochemistry and next generation sequencing assays. Lung Cancer 2016, 99, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Weber, B.; Liu, M.; Sobkin, P.; Morris, S.W.; Hout, D.; Van der Westthuizen, N.; Tonseth, R.P.; Saltman, D. Successful treatment of hepatic oligometastases with stereotactic ablative body radiation and radiofrequency ablation in an anaplastic lymphoma kinase fusion-positive lung cancer patient. J. Med. Radiat. Sci. 2016, 63, 67–70. [Google Scholar] [CrossRef] [PubMed]
- Yi, E.S.; Boland, J.M.; Maleszewski, J.J; Roden, A.; Oliveria, A.M.; Aubry, M-C.; Erickson-Johnson, M.R.; Caron, B.L.; Li, Y.; Tang, H.; et al. Correlation of IHC and FISH for ALK gene rearrangement in non-small cell lung carcinoma: IHC Score Algorithm for FISH. J. Thoracic. Oncol. 2011, 6, 459–465. [Google Scholar] [CrossRef] [PubMed]
- Dacic, S.; Villaruz, L.C.; Abberbock, S.; Mahaffey, A.; Incharorn, P.; Nikifovova, M.N. ALK FISH patterns and the detection of ALK fusions by next generation sequencing in lung adenocarcinoma. Oncotarget 2016, 7, 82943–82952. [Google Scholar] [CrossRef] [PubMed]
- Pekar-Zlotin, M.; Hirsh, F.R.; Soussan-Gutman, L.; Ilouze, M.; Dvir, A.; Bolye, T.; Wynes, M.; Miller, V.A.; Lipson, D.; Palmer, G.A. Fluorescence in situ hybridization, immunohistochemistry, and next generation sequencing for the detection of EML4-ALK rearrangement in lung cancer. Oncologist 2015, 20, 316–322. [Google Scholar] [CrossRef] [PubMed]
- Ali, S.M.; Hensing, T.; Schrock, A.B.; Allen, J.; Sanford, E.; Gowen, K.; Kulani, A.; He, J.; Suh, J.H.; Lipson, D.; et al. Comprehensive genomic profiling identifies a subset of crizotinib responsive ALK-rearranged nonsmall cell lung cancer not detected by fluorescence in situ hybridization. Oncologist 2016, 6, 762–770. [Google Scholar] [CrossRef] [PubMed]
- Kokkat, T.J.; Patel, M.S.; McGarvey, D.; LiVolsi, V.A.; Baloch, Z.W. Archived formalin-fixed paraffin-embedded (FFPE) blocks: A valuable underexploited resource for extraction of DNA, RNA, and protein. Biopreserv. Biobank. 2013, 11, 101–106. [Google Scholar] [CrossRef] [PubMed]
- Ludya, N.; Günwauld, B.; Azimzadeh, O.; Englert, S.; Höfler, H.; Taio, S.; Aubele, M. Nucleic acids from long-term preserved FFPE tissues are suitable for downstream analyses. Virchows Arch. 2012, 460, 131–140. [Google Scholar] [CrossRef] [PubMed]
- Lung, J.; Lin, Y.C.; Hung, M.S.; Jiang, Y.Y.; Lee, K.D.; Lin, P.Y.; Tsai, Y.H. A sensitive and high throughput TaqMan-based reverse transcription quantitative polymerase chain reaction assay efficiently discriminates ALK rearrangement from overexpression for lung cancer FFPE specimens. Lung Cancer 2016, 94, 114–120. [Google Scholar] [CrossRef] [PubMed]
- Peretti, U.; Ferrara, R.; Pilotto, S.; Kinspergher, S.; Caccese, M.; Santo, A.; Brunelli, M.; Caliò, A.; Carbognin, L.; Sperduti, I.; et al. ALK gene copy number gains in non-small-cell lung cancer: prognostic impact and clinico-pathological correlations. Respir. Res. 2016, 17, 105. [Google Scholar] [CrossRef] [PubMed]
- George, R.E.; Sanda, T.; Hanna, M.; Fröhling, S.; Luther, W., II; Zhang, J.; Ahn, Y.; Zhou, W.; London, W.B.; McGrady, P.; et al. Activating mutations in ALK provide a therapeutic target in neuroblastoma. Nature 2008, 455, 975–978. [Google Scholar] [CrossRef] [PubMed]
- Murugan, A.K.; Xing, M. Anaplastic thyroid cancers harbor novel oncogenic mutations of the ALK gene. Cancer Res. 2011, 71, 4403–4411. [Google Scholar] [CrossRef] [PubMed]
- Guan, J.; Wolfstetter, G.; Siaw, J.; Chand, D.; Hugosson, F.; Palmer, R.H.; Hallberg, B. Anaplastic lymphoma kinase L1198F and G1201E mutations identified in anaplastic thyroid cancer patients are not ligand-independent. Oncotarget 2017, 8, 11566–11578. [Google Scholar] [CrossRef] [PubMed]
- Preusser, M.; Berhoff, A.S.; IIhan-Mutlu, A.; Magerle, M.; Dinhof, C.; Widhalm, G.; Dieckmann, K.; Marosi, C.; Wöhrer, A.; Hackl, M.; et al. ALK gene translocations and amplifications in brain metastases of non-small cell lung cancer. Lung Cancer 2013, 80, 278–283. [Google Scholar] [CrossRef] [PubMed]
- Morris, S.W.; Naeve, C.; Matthew, P.; James, P.L.; Kirstein, M.N.; Cui, X.; Witte, D.P. ALK, the chromosome 2 gene locus altered by the t(2;5) in non-Hodgkin’s lymphoma, encodes novel neural receptor tyrosine kinase that is highly related to leukocyte tyrosine kinase (LTK). Oncogene 1997, 8, 2175–2188. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zhang, J.; Gao, G.; Li, X.; Zhao, C.; He, Y.; SU, C.; Zhang, Z.; Chen, X.; Zhang, J.; et al. EML4-ALK fusion detected by RT-PCR confers similar response to crizotinib as detected by FISH in patients with advanced non-small cell lung cancer. J. Thorac. Oncol. 2015, 10, 1546–1552. [Google Scholar] [CrossRef] [PubMed]
- Woo, C.G.; Seo, S.; Kim, S.W.; Jang, S.J.; Park, K.S.; Song, J.Y.; Lee, B.; Richards, M.W.; Bayliss, R.; Lee, D.H.; et al. Differential protein stability and clinical responses of EML4-ALK fusion variants to various ALK inhibitors in advanced ALK-rearranged non-small cell lung cancer. Ann. Oncol. 2017, 28, 791–797. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.C.; Chang, I.C.; Wang, C.L.; Chen, T.D.; Chen, Y.D.; Liu, H.P.; Chu, Y.; Chiu, Y.T.; Wu, T.H.; Chou, L.H.; et al. Comparison of IHC, FISH and RT-PCR methods for detection of ALK rearrangements in 312 non-small cell lung cancer patients in Taiwan. PLoS ONE 2013, 8, e70839. [Google Scholar] [CrossRef] [PubMed]
- ALK RGQRT-PCR Kit Handbook. Available online: https://www.qiagen.com/us/resourses/download.aspx?id=3016f056-577f-404a (accessed on 7 July 2017).
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2016. [Google Scholar]
| ALK RT-PCR | ALK RT-PCR, IHC and FISH | ||
|---|---|---|---|
| Clinicopathological Characteristics | Positive | Negative | Positive |
| Total Number of Cases | 36 | 59 | 21 |
| Median age | 69 (36–81) | 69.5 (43–82) | 67 (36–81) |
| Gender | |||
| Male | 14 (39%) | 26 (44%) | 6 (29%) |
| Female | 22 | 33 | 15 |
| Sample site | |||
| Lung primary | 19 (52%) | 36 (61%) | 10 (48%) |
| Metastatic | 17 (47%) | 23 (39%) | 11 (52%) |
| Sample type | |||
| Resection | 9 (25%) | 14 (24%) | 3 (14%) |
| Lung | 4 | 11 | 2 |
| Brain | 4 | 3 | |
| Kidney | 1 | 1 | |
| Biopsy and cytology | 27 (75%) | 45 (76%) | 18 (86%) |
| Histology | |||
| Adenocarcinoma | 34 (95%) | 59 (100%) | 19 (90%) |
| Adenosquamous | 2 | 0 | 2 |
| Stage | |||
| I-IIIA | 0 | 0 | 0 |
| IIIB-IV | 36 | 59 | 21 |
| Smoking history | |||
| Never or light smoker | 18 (50%) | 1 (1.7%) | 16 (76%) |
| Smoker | 18 | 58 | 5 |
| EGFR mutations | |||
| Wild-type | 36 | 59 | 21 |
| Mutant | 0 | 0 | 0 |
| Case | Sample | Tumor Content (%) | IHC (0,1,2,3) | FISH (% Positive) | RT-PCR ΔCt | ALK Fusion by Sequencing | Response to First-Line ALK Inhibitor and PFS (Months) |
|---|---|---|---|---|---|---|---|
| 1 | B | 60 | 3 | +(66) | −65 | EML4-Var1 (2) | +(6) |
| 2 | B | 95 | 2 | +(78) | −0.07 | EML4-Var1 (1,2) | +(30) |
| 3 | B | 70 | 3 | +(59) | 0.09 | EML4-Var1 (1) | +(22) |
| 4 | R | 90 | 2 | +(21) | 0.22 | EML4-Var1 (2) | +(20) |
| 5 | B | 90 | 3 | +(96) | 0.58 | EML4-Var1 (1,2) | +(4) |
| 6 | C | 40 | 3 | +(31) | 0.06 | EML4-Var1 (2) | +(24) |
| 7 | R | 95 | 3 | +(66) | 0.41 | EML4-Var3a (2) | +(23) |
| 8 | B | >50 | 3 | +(53) | 1.09 | EML4-Var3a (2) | +(9) |
| 9 | B | 90 | 3 | +(52) | 2.11 | EML4-Var3a/5 (2) | No Response |
| 10 | B | 50 | 3 | +(16) | 1.29 | EML4-Var3b (2) | +(7) |
| 11 | R | 90 | 3 | +(65) | −0.83 | ND | +(24) |
| 12 | B | 80 | 3 | +(94) | 2.69 | ND | +(19) |
| 13 | C | >50 | 3 | +(34) | 1.19 | QNS | +(4) |
| 14 | B | 50 | 3 | failed twice | 0.21 | QNS | +(20) |
| 15 | B | 85 | 1 | +(38) | 7.12 | QNS | +(6) |
| 16 | R | 80 | 3 | +(84) | −0.97 | QNS | +(30) |
| 17 | C | 60 | 3 | +(73) | −0.64 | QNS | +(33) |
| 18 | B | 60 | 2 | +(58) | −0.51 | QNS | +(3) |
| 19 | B | 80 | 2 | +(56) | −0.11 | QNS | +(12) |
| 20 | B | 50 | 3 | +(40) | 3.62 | QNS | No Response |
| 21 | B | 70 | ND | +(25) | 0.80 | EML4-Var1 (1,2) | +(48) |
| 22 | R | 80 | 1 | −(0) | 5.63 | EML4-Var1 (2) | NT |
| 23 | B | 70 | 0 | −(6) | 3.45 | EML4-Var1 (1,2) | NT |
| 24 | B | 50 | 0 | −(2) | 4.35 | EML4-Var1 (1,2) | NT |
| 25 | B | 90 | 0 | −(0) | 5.22 | EML4-Var1 (1,2) | NT |
| 26 | B | 50 | 0 | −(0) | 5.22 | EML4-Var1 (1) | NT |
| 27 | B | 95 | 0 | NT | 4.57 | EML4-Var2 (2) | NT |
| 28 | B | 80 | 0 | −(6) | 6.83 | EML4-Var3a (1) | NT |
| 29 | R (brain) | 90 | 0 | −(6) | 4.83 | KIF5B (2) | NT |
| 30 | B | 50 | 0 | −(13) | 5.81 | KIF5B (2) | NT |
| 31 | R | 60 | 0 | −(0) | 4.07 | KIF5B (2) | NT |
| 32 | C | 60 | 1 | −(8) | 4.79 | EML4-Var3a (1) | No Response |
| 33 | R (brain) | 90 | 0 | −(0) | 3.98 | Wild-Type (1,2) | NT |
| 34 | B (brain) | 90 | 0 | −(0) | 4.47 | Wild-Type (1,2) | +(28) |
| 35 | B | 90 | 0 | −(2) | 5.1 | Wild-Type (1) | NT |
| 36 | B (brain) | 95 | 0 | −(0) | 5.22 | Wild-Type (2) | NT |
| RT-PCR | FISH+ | FISH− | Total |
| ΔCt cut-off of ≤8 | |||
| Positive | 21 | 15 | 36 |
| Negative | 0 | 59 | 59 |
| Total | 21 | 74 | 95 |
| Sensitivity = 100% (95% CI: 84–100%) | |||
| Specificity = 80% (95% CI: 69–88%) | |||
| RT-PCR | FISH+ | FISH− | Total |
| ΔCt cut-off of ≤3.5 | |||
| Positive | 19 | 1 | 20 |
| Negative | 2 | 73 | 75 |
| Total | 21 | 74 | 95 |
| Sensitivity = 90% (95% CI: 70–99%) | |||
| Specificity = 99% (95% CI: 93–100%) | |||
| RT-PCR | FISH or Sequencing+ | FISH− or Sequencing− | Total |
| ΔCt cut-off of ≤8 | |||
| Positive | 32 | 4 | 36 |
| Negative | 0 | 59 | 59 |
| Total | 32 | 63 | 95 |
| Sensitivity = 100% (95% CI: 89–100%) | |||
| Specificity = 94% (95% CI: 85–98%) | |||
| RT-PCR | FISH+ or Sequencing+ | FISH− or Sequencing− | Total |
| ΔCt cut-off of ≤3.5 | |||
| Positive | 20 | 0 | 20 |
| Negative | 12 | 63 | 75 |
| Total | 32 | 63 | 95 |
| Sensitivity = 62% (95% CI: 44–79%) | |||
| Specificity = 100% (95% CI: 94–100%) | |||
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hout, D.R.; Schweitzer, B.L.; Lawrence, K.; Morris, S.W.; Tucker, T.; Mazzola, R.; Skelton, R.; McMahon, F.; Handshoe, J.; Lesperance, M.; et al. Performance of a RT-PCR Assay in Comparison to FISH and Immunohistochemistry for the Detection of ALK in Non-Small Cell Lung Cancer. Cancers 2017, 9, 99. https://doi.org/10.3390/cancers9080099
Hout DR, Schweitzer BL, Lawrence K, Morris SW, Tucker T, Mazzola R, Skelton R, McMahon F, Handshoe J, Lesperance M, et al. Performance of a RT-PCR Assay in Comparison to FISH and Immunohistochemistry for the Detection of ALK in Non-Small Cell Lung Cancer. Cancers. 2017; 9(8):99. https://doi.org/10.3390/cancers9080099
Chicago/Turabian StyleHout, David R., Brock L. Schweitzer, Kasey Lawrence, Stephan W. Morris, Tracy Tucker, Rosetta Mazzola, Rachel Skelton, Frank McMahon, John Handshoe, Mary Lesperance, and et al. 2017. "Performance of a RT-PCR Assay in Comparison to FISH and Immunohistochemistry for the Detection of ALK in Non-Small Cell Lung Cancer" Cancers 9, no. 8: 99. https://doi.org/10.3390/cancers9080099






