Fluorescence-Guided Surgery for Hepatoblastoma with Indocyanine Green
Abstract
1. Introduction
2. The Principles of ICG Imaging for HB
3. Modalities
3.1. Hamamatsu Photonics: PDE System®
3.2. Olympus: VISERA ELITE System®
3.3. Stryker: PINPOINT System®
3.4. Karl Stolz: D-Light P System®
4. Clinical Application of ICG-Guided Surgery for Liver Tumors
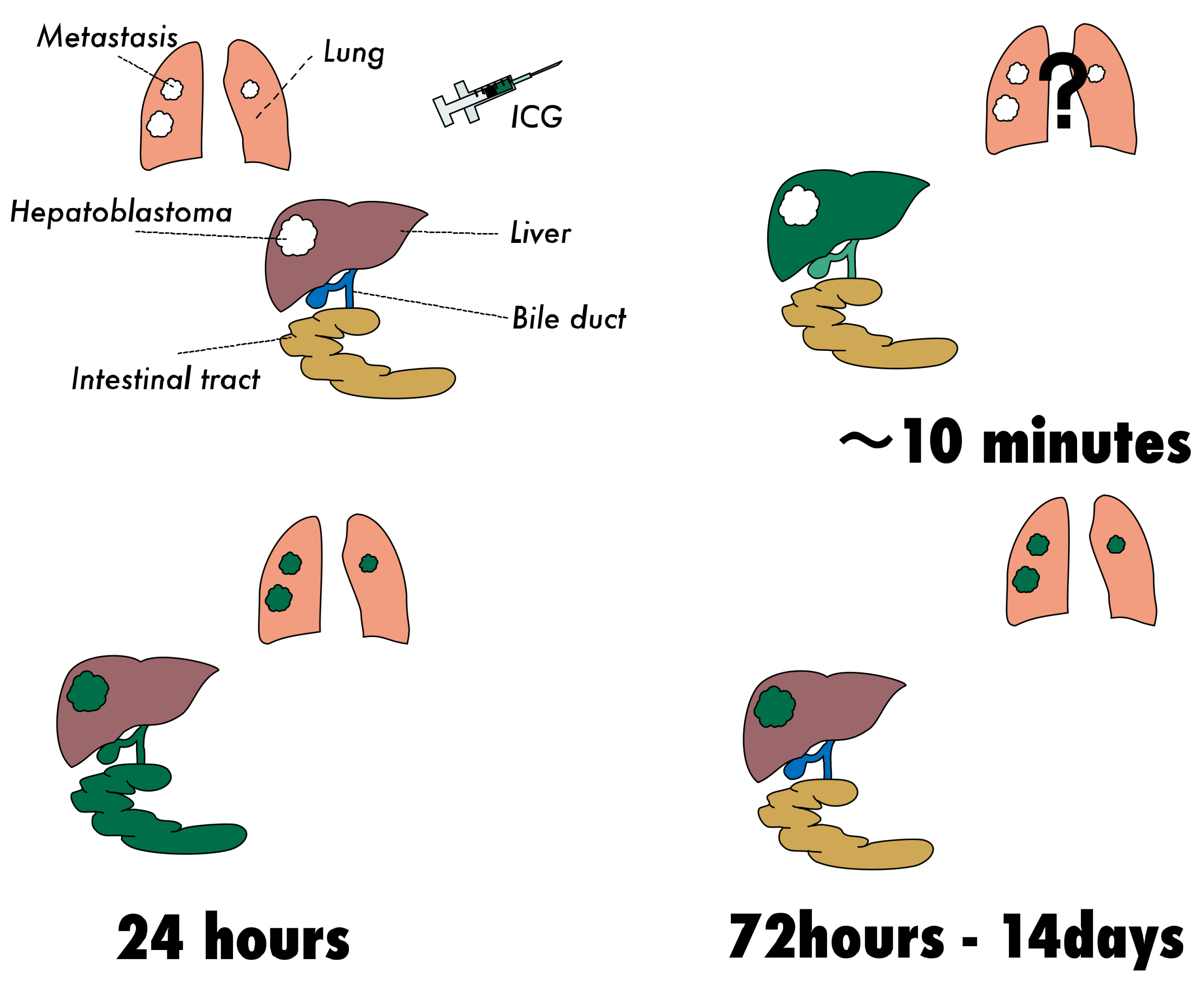
4.1. Pharmacokinetics of Intravenously Administered ICG
4.2. Protocol of ICG-Guided Surgery for HCC and Metastatic Liver Tumors in Adult Patients
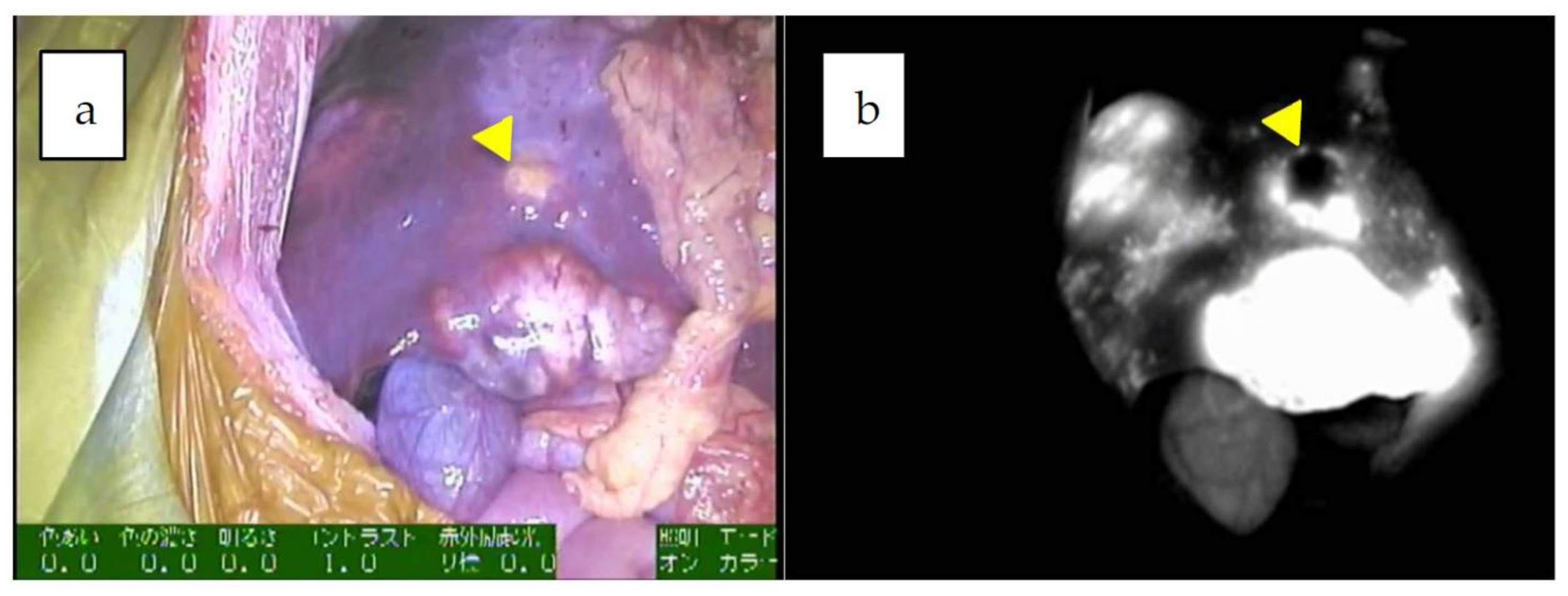
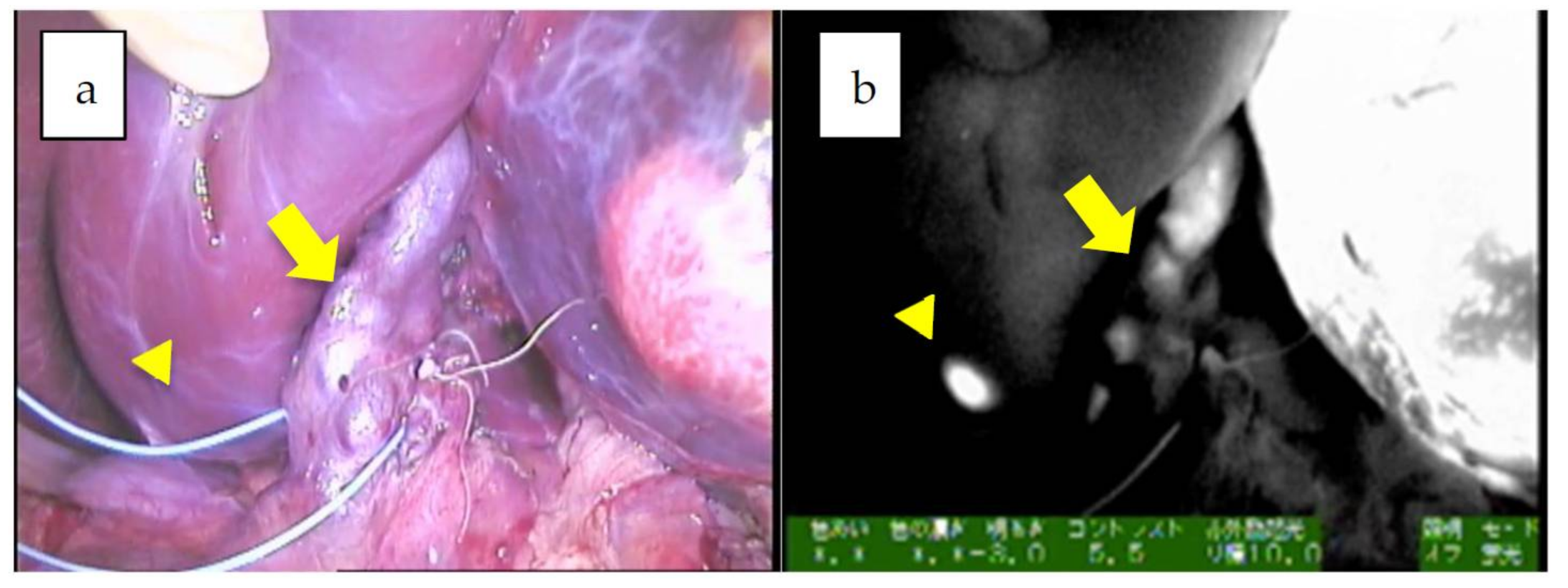
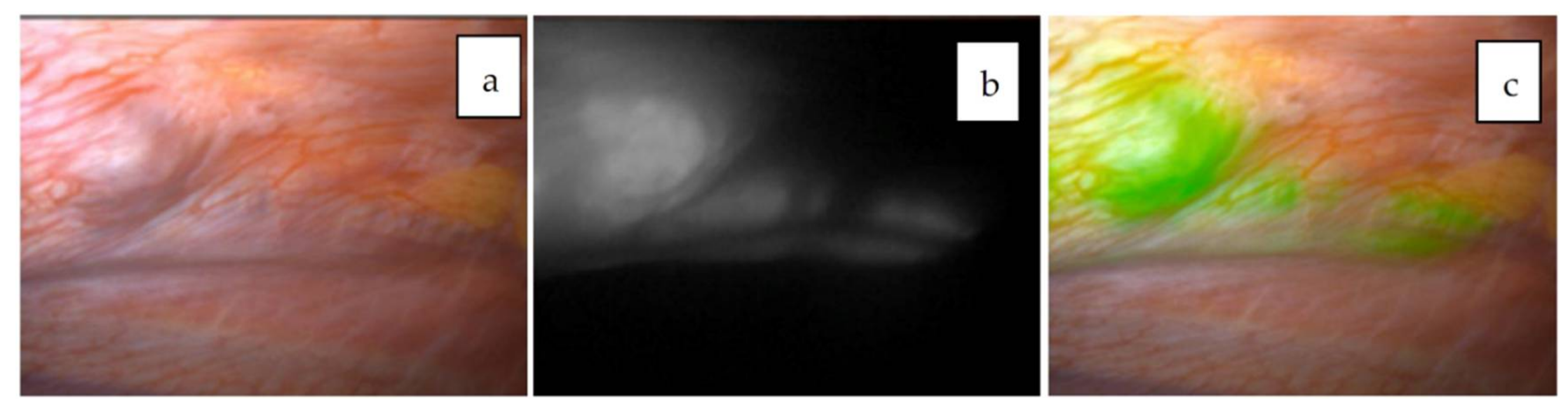
4.3. Institutional Experience
4.4. Proposed Protocol of ICG-Guided Surgery for Primary HB Lesions
4.5. Proposed Protocol for Metastatic Lesions
4.5.1. Pulmonary Metastases
4.5.2. Other Forms of Metastasis
5. Limitations
5.1. False Positives
5.2. Depth
6. Conclusions and Future Prospects
Funding
Conflicts of Interest
References
- Landsman, M.L.; Kwant, G.; Mook, G.A.; Zijlstra, W.G. Light-absorbing properties, stability, and spectral stabilization of indocyanine green. J. Appl. Physiol. 1976, 40, 575–583. [Google Scholar] [CrossRef] [PubMed]
- Guyer, D.R.; Puliafito, C.A.; Mones, J.M.; Friedman, E.; Chang, W.; Verdooner, S.R. Digital indocyanine-green angiography in chorioretinal disorders. Ophthalmology 1992, 99, 287–291. [Google Scholar] [CrossRef]
- Unno, N.; Inuzuka, K.; Suzuki, M.; Yamamoto, N.; Sagara, D.; Nishiyama, M.; Konno, H. Preliminary experience with a novel fluorescence lymphography using indocyanine green in patients with secondary lymphedema. J. Vasc. Surg. 2007, 45, 1016–1021. [Google Scholar] [CrossRef] [PubMed]
- Kitai, T.; Inomoto, T.; Miwa, M.; Shikayama, T. Fluorescence navigation with indocyanine green for detecting sentinel lymph nodes in breast cancer. Breast Cancer 2005, 12, 211–215. [Google Scholar] [CrossRef] [PubMed]
- Rubens, F.D.; Ruel, M.; Fremes, S.E. A new and simplified method for coronary and graft imaging during CABG. Heart Surg. Forum 2002, 5, 141–144. [Google Scholar] [PubMed]
- Raabe, A.; Beck, J.; Seifert, V. Technique and image quality of intraoperative indocyanine green angiography during aneurysm surgery using surgical microscope integrated near-infrared video technology. Zent. Neurosurg. 2005, 66, 1–6; discussion 7–8. [Google Scholar] [CrossRef] [PubMed]
- Fox, I.J.; Brooker, L.G.; Heseltine, D.W.; Essex, H.E.; Wood, E.H. A tricarbocyanine dye for continuous recording of dilution curves in whole blood independent of variations in blood oxygen saturation. Proc. Staff Meet. Mayo Clin. 1957, 32, 478–484. [Google Scholar] [PubMed]
- Speich, R.; Saesseli, B.; Hoffmann, U.; Neftel, K.A.; Reichen, J. Anaphylactoid reactions after indocyanine-green administration. Ann. Intern. Med. 1988, 109, 345–346. [Google Scholar] [CrossRef] [PubMed]
- Ishizawa, T.; Tamura, S.; Masuda, K.; Aoki, T.; Hasegawa, K.; Imamura, H.; Beck, Y.; Kokudo, N. Intraoperative fluorescent cholangiography using indocyanine green: A biliary road map for safe surgery. J. Am. Coll. Surg. 2009, 208, e1–e4. [Google Scholar] [CrossRef] [PubMed]
- Ishizawa, T.; Fukushima, N.; Shibahara, J.; Masuda, K.; Tamura, S.; Aoki, T.; Hasegawa, K.; Beck, Y.; Fukayama, M.; Kokudo, N. Real-time identification of liver cancers by using indocyanine green fluorescent imaging. Cancer 2009, 115, 2491–2504. [Google Scholar] [CrossRef] [PubMed]
- Nakaseko, Y.; Ishizawa, T.; Saiura, A. Fluorescence-guided surgery for liver tumors. J. Surg. Oncol. 2018, 118, 324–331. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, A. The emerging family of hepatoblastoma tumours: From ontogenesis to oncogenesis. Eur. J. Cancer 2005, 41, 1503–1514. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Terrada, D.; Zimmermann, A. Current issues and controversies in the classification of pediatric hepatocellular tumors. Pediatr. Blood Cancer 2012, 59, 780–784. [Google Scholar] [CrossRef] [PubMed]
- Haines, K.; Sarabia, S.F.; Alvarez, K.R.; Tomlinson, G.; Vasudevan, S.A.; Heczey, A.A.; Roy, A.; Finegold, M.J.; Parsons, D.W.; Plon, S.E.; et al. Characterization of pediatric hepatocellular carcinoma reveals genomic heterogeneity and diverse signaling pathway activation. Pediatr. Blood Cancer 2019, 66, e27745. [Google Scholar] [CrossRef] [PubMed]
- Prokurat, A.; Kluge, P.; Kosciesza, A.; Perek, D.; Kappeler, A.; Zimmermann, A. Transitional liver cell tumors (TLCT) in older children and adolescents: A novel group of aggressive hepatic tumors expressing beta-catenin. Med. Pediatr. Oncol. 2002, 39, 510–518. [Google Scholar] [CrossRef] [PubMed]
- Kitagawa, N.; Shinkai, M.; Mochizuki, K.; Usui, H.; Miyagi, H.; Nakamura, K.; Tanaka, M.; Tanaka, Y.; Kusano, M.; Ohtsubo, S. Navigation using indocyanine green fluorescence imaging for hepatoblastoma pulmonary metastases surgery. Pediatr. Surg. Int. 2015, 31, 407–411. [Google Scholar] [CrossRef] [PubMed]
- Yamamichi, T.; Oue, T.; Yonekura, T.; Owari, M.; Nakahata, K.; Umeda, S.; Nara, K.; Ueno, T.; Uehara, S.; Usui, N. Clinical application of indocyanine green (ICG) fluorescent imaging of hepatoblastoma. J. Pediatr. Surg. 2015, 50, 833–836. [Google Scholar] [CrossRef] [PubMed]
- Hishiki, T.; Watanabe, K.; Ida, K.; Hoshino, K.; Iehara, T.; Aoki, Y.; Kazama, T.; Kihira, K.; Takama, Y.; Taguchi, T.; et al. The role of pulmonary metastasectomy for hepatoblastoma in children with metastasis at diagnosis: Results from the JPLT-2 study. J. Pediatr. Surg. 2017, 52, 2051–2055. [Google Scholar] [CrossRef] [PubMed]
- Meyers, R.L.; Maibach, R.; Hiyama, E.; Häberle, B.; Krailo, M.; Rangaswami, A.; Aronson, D.C.; Malogolowkin, M.H.; Perilongo, G.; von Schweinitz, D.; et al. Risk-stratified staging in paediatric hepatoblastoma: A unified analysis from the Children’s Hepatic tumors International Collaboration. Lancet Oncol. 2017, 18, 122–131. [Google Scholar] [CrossRef]
- Zsiros, J.; Brugieres, L.; Brock, P.; Roebuck, D.; Maibach, R.; Zimmermann, A.; Childs, M.; Pariente, D.; Laithier, V.; Otte, J.B.; et al. Dose-dense cisplatin-based chemotherapy and surgery for children with high-risk hepatoblastoma (SIOPEL-4): A prospective, single-arm, feasibility study. Lancet Oncol. 2013, 14, 834–842. [Google Scholar] [CrossRef]
- de Graaf, W.; Bennink, R.J.; Vetelainen, R.; van Gulik, T.M. Nuclear imaging techniques for the assessment of hepatic function in liver surgery and transplantation. J. Nucl. Med. 2010, 51, 742–752. [Google Scholar] [CrossRef] [PubMed]
- Paumgartner, G. The handling of indocyanine green by the liver. Schweiz. Med. Wochenschr. 1975, 105, 1–30. [Google Scholar] [PubMed]
- de Graaf, W.; Hausler, S.; Heger, M.; van Ginhoven, T.M.; van Cappellen, G.; Bennink, R.J.; Kullak-Ublick, G.A.; Hesselmann, R.; van Gulik, T.M.; Stieger, B. Transporters involved in the hepatic uptake of (99m)Tc-mebrofenin and indocyanine green. J. Hepatol. 2011, 54, 738–745. [Google Scholar] [CrossRef] [PubMed]
- Ishizawa, T.; Masuda, K.; Urano, Y.; Kawaguchi, Y.; Satou, S.; Kaneko, J.; Hasegawa, K.; Shibahara, J.; Fukayama, M.; Tsuji, S.; et al. Mechanistic background and clinical applications of indocyanine green fluorescence imaging of hepatocellular carcinoma. Ann. Surg. Oncol. 2014, 21, 440–448. [Google Scholar] [CrossRef] [PubMed]
- Kono, Y.; Ishizawa, T.; Tani, K.; Harada, N.; Kaneko, J.; Saiura, A.; Bandai, Y.; Kokudo, N. Techniques of Fluorescence Cholangiography During Laparoscopic Cholecystectomy for Better Delineation of the Bile Duct Anatomy. Medicine 2015, 94, e1005. [Google Scholar] [CrossRef] [PubMed]
- Yokoyama, N.; Otani, T.; Hashidate, H.; Maeda, C.; Katada, T.; Sudo, N.; Manabe, S.; Ikeno, Y.; Toyoda, A.; Katayanagi, N. Real-time detection of hepatic micrometastases from pancreatic cancer by intraoperative fluorescence imaging: Preliminary results of a prospective study. Cancer 2012, 118, 2813–2819. [Google Scholar] [CrossRef] [PubMed]
- Shoji, Y.; Kumagai, K.; Kamiya, S.; Ida, S.; Nunobe, S.; Ohashi, M.; Yoshimizu, S.; Horiuchi, Y.; Yoshio, T.; Ishiyama, A.; et al. Prospective feasibility study for single-tracer sentinel node mapping by ICG (indocyanine green) fluorescence and OSNA (one-step nucleic acid amplification) assay in laparoscopic gastric cancer surgery. Gastric Cancer 2019, 22, 873–880. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.W. Lymph node mapping and anastomosis evaluation by VISERA ELITE II((R)), a novel surgical endoscope system, with infrared fluorescence imaging during laparoscopic rectal cancer surgery—A video vignette. Colorectal Dis. 2019, 21, 375–376. [Google Scholar] [CrossRef]
- Jafari, M.D.; Wexner, S.D.; Martz, J.E.; McLemore, E.C.; Margolin, D.A.; Sherwinter, D.A.; Lee, S.W.; Senagore, A.J.; Phelan, M.J.; Stamos, M.J. Perfusion assessment in laparoscopic left-sided/anterior resection (PILLAR II): A multi-institutional study. J. Am. Coll. Surg. 2015, 220, 82–92.e1. [Google Scholar] [CrossRef]
- Sherwinter, D.A. Identification of anomolous biliary anatomy using near-infrared cholangiography. J. Gastrointest. Surg. 2012, 16, 1814–1815. [Google Scholar] [CrossRef]
- Zarrinpar, A.; Dutson, E.P.; Mobley, C.; Busuttil, R.W.; Lewis, C.E.; Tillou, A.; Cheaito, A.; Hines, O.J.; Agopian, V.G.; Hiyama, D.T. Intraoperative Laparoscopic Near-Infrared Fluorescence Cholangiography to Facilitate Anatomical Identification: When to Give Indocyanine Green and How Much. Surg. Innov. 2016, 23, 360–365. [Google Scholar] [CrossRef] [PubMed]
- Aoki, T.; Murakami, M.; Koizumi, T.; Matsuda, K.; Fujimori, A.; Kusano, T.; Enami, Y.; Goto, S.; Watanabe, M.; Otsuka, K. Determination of the surgical margin in laparoscopic liver resections using infrared indocyanine green fluorescence. Langenbecks Arch. Surg. 2018, 403, 671–680. [Google Scholar] [CrossRef] [PubMed]
- Yamada, Y.; Hoshino, K.; Mori, T.; Kawaida, M.; Abe, K.; Takahashi, N.; Fujimura, T.; Kameyama, K.; Kuroda, T. Metastasectomy of Hepatoblastoma Utilizing a Novel Overlay Fluorescence Imaging System. J. Laparoendosc. Adv. Surg. Tech. A 2018, 28, 1152–1155. [Google Scholar] [CrossRef] [PubMed]
- Boogerd, L.S.; Handgraaf, H.J.; Lam, H.D.; Huurman, V.A.; Farina-Sarasqueta, A.; Frangioni, J.V.; van de Velde, C.J.; Braat, A.E.; Vahrmeijer, A.L. Laparoscopic detection and resection of occult liver tumors of multiple cancer types using real-time near-infrared fluorescence guidance. Surg. Endosc. 2017, 31, 952–961. [Google Scholar] [CrossRef] [PubMed]
- Tummers, Q.R.; Verbeek, F.P.; Prevoo, H.A.; Braat, A.E.; Baeten, C.I.; Frangioni, J.V.; van de Velde, C.J.; Vahrmeijer, A.L. First experience on laparoscopic near-infrared fluorescence imaging of hepatic uveal melanoma metastases using indocyanine green. Surg. Innov. 2015, 22, 20–25. [Google Scholar] [CrossRef] [PubMed]
- Souzaki, R.; Kawakubo, N.; Matsuura, T.; Yoshimaru, K.; Koga, Y.; Takemoto, J.; Shibui, Y.; Kohashi, K.; Hayashida, M.; Oda, Y.; et al. Navigation surgery using indocyanine green fluorescent imaging for hepatoblastoma patients. Pediatr. Surg. Int. 2019, 35, 551–557. [Google Scholar] [CrossRef] [PubMed]
- Verbeek, F.P.; Schaafsma, B.E.; Tummers, Q.R.; van der Vorst, J.R.; van der Made, W.J.; Baeten, C.I.; Bonsing, B.A.; Frangioni, J.V.; van de Velde, C.J.; Vahrmeijer, A.L.; et al. Optimization of near-infrared fluorescence cholangiography for open and laparoscopic surgery. Surg. Endosc. 2014, 28, 1076–1082. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, E.; Choi, H.S.; Humblet, V.; Ohnishi, S.; Laurence, R.G.; Frangioni, J.V. Real-time intraoperative assessment of the extrahepatic bile ducts in rats and pigs using invisible near-infrared fluorescent light. Surgery 2008, 144, 39–48. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.M.; Shi, R.; Hou, J.C.; Liu, Z.R.; Cui, Z.L.; Li, Y.; Wu, D.; Shi, Y.; Shen, Z.Y. Liver tumor boundaries identified intraoperatively using real-time indocyanine green fluorescence imaging. J. Cancer Res. Clin. Oncol. 2017, 143, 51–58. [Google Scholar] [CrossRef]
- Lieto, E.; Galizia, G.; Cardella, F.; Mabilia, A.; Basile, N.; Castellano, P.; Orditura, M.; Auricchio, A. Indocyanine Green Fluorescence Imaging-Guided Surgery in Primary and Metastatic Liver Tumors. Surg. Innov. 2018, 25, 62–68. [Google Scholar] [CrossRef]
- 72nd General meeting of the Japanese Society of Gastroenterological Surgery 2017. Available online: http://www.jsgs.or.jp/72/modules/en/index.php?content_id=3 (accessed on 10 August 2019).
- Morita, Y.; Sakaguchi, T.; Unno, N.; Shibasaki, Y.; Suzuki, A.; Fukumoto, K.; Inaba, K.; Baba, S.; Takehara, Y.; Suzuki, S.; et al. Detection of hepatocellular carcinomas with near-infrared fluorescence imaging using indocyanine green: Its usefulness and limitation. Int. J. Clin. Oncol. 2013, 18, 232–241. [Google Scholar] [CrossRef] [PubMed]
- Chen-Yoshioka, T.F.; Hatano, E.; Toshizawa, A.; Date, H. Clinical application of projection mapping technology for surgical resection of lung metastasis. Interact. Cardiovasc. Thorac. Surg. 2017, 25, 1010–1011. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, N.; Yamada, Y.; Hoshino, K.; Kawaida, M.; Mori, T.; Abe, K.; Fujimura, T.; Matsubara, K.; Hibi, T.; Shinoda, M.; et al. Living Donor Liver Re-Transplantation for Recurrent Hepatoblastoma in the Liver Graft following Complete Eradication of Peritoneal Metastases under Indocyanine Green Fluorescence Imaging. Cancers 2019, 11, 730. [Google Scholar] [CrossRef] [PubMed]
- Ohno, M. (National Center for Child Health and Development, Tokyo, Japan). Personal communication, 2019.
- Liberale, G.; Bourgeois, P.; Larsimont, D.; Moreau, M.; Donckier, V.; Ishizawa, T. Indocyanine green fluorescence-guided surgery after IV injection in metastatic colorectal cancer: A systematic review. Eur. J. Surg. Oncol. 2017, 43, 1656–1667. [Google Scholar] [CrossRef] [PubMed]
- Satou, S.; Ishizawa, T.; Masuda, K.; Kaneko, J.; Aoki, T.; Sakamoto, Y.; Hasegawa, K.; Sugawara, Y.; Kokudo, N. Indocyanine green fluorescent imaging for detecting extrahepatic metastasis of hepatocellular carcinoma. J. Gastroenterol. 2013, 48, 1136–1143. [Google Scholar] [CrossRef] [PubMed]
- Tetron TAPE. Available online: https://www.konoseisakusho.jp/pdf/catalog18.pdf (accessed on 10 August 2019).
- Ishizawa, T.; Bandai, Y.; Kokudo, N. Fluorescent cholangiography using indocyanine green for laparoscopic cholecystectomy: An initial experience. Arch. Surg. 2009, 144, 381–382. [Google Scholar] [CrossRef] [PubMed]
- Miyata, A.; Ishizawa, T.; Kamiya, M.; Shimizu, A.; Kaneko, J.; Ijichi, H.; Shibahara, J.; Fukayama, M.; Midorikawa, Y.; Urano, Y.; et al. Photoacoustic tomography of human hepatic malignancies using intraoperative indocyanine green fluorescence imaging. PLoS ONE 2014, 9, e112667. [Google Scholar] [CrossRef]






| Case No | Patient | Age/Sex | Device | Procedure | Primary Pathology | Fluorescence Pattern | Tumor Size | Preoperative AFP 3 (ng/dL) | Usefulness and Disease Free Survival (Months) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 1 | 1y/F | PDE 1 neo system | left lobectomy | mixed epithelial and mesenchymal type with teratoid features, post-chemotherapy | uneven | 125 × 75 × 70 mm | 87.8 | identification, surgical margin, 20 m |
| 2 | 2 | 2y/M | PDE neo system | LDLT 2 | combined fetal and embryonal subtype, post-chemotherapy | uneven | 40 mm, 70 mm | 5514.4 | identification, surgical margin, 29 m |
| 3 | 3 | 8m/M | PDE neo system | right lobectomy | fetal, post-chemotherapy | uneven | 65 mm | 41,311 | identification, surgical margin, 18 m |
| 4 | 4 | 1y/F | PDE neo system | right trisegmentectomy | combined fetal and embryonal subtype, post-chemotherapy | uneven | 65 mm | 936.3 | identification, surgical margin, 17 m |
| 5 | 5 | 4y/M | PDE neo system | LDLT 2 | combined fetal and embryonal subtype, post-chemotherapy | uneven | 90 mm | 42591 | identification, surgical margin, newly detected tumors, 19 m |
| 6 | 6 | 2y/M | PDE neo system | LDLT 2 | embryonal, post-chemotherapy | uneven | 25 mm, 10 mm | 6.6 | identification, surgical margin, not disease free |
| 7 | 7 | 9m/M | PDE neo system | left lobectomy | mixed fetal and embryonal subtype, post-chemotherapy | uneven | 51 × 66 × 52 mm | 46.1 | identification, surgical margin, 3 m |
| 8 | 8 | 14y/M | PDE neo system | partial resection (recurrences in the transplanted liver) | wholly epithelial type and fetal subtype | diffuse | 8 mm | 69 | identification, surgical margin, newly detected tumors |
| 9 | 8 | 14y/M | PDE neo system | LDLT 2 | wholly epithelial type and fetal subtype | diffuse | 8 mm | 394 | identification, surgical margin, 34 m |
| 10 | 9 | 8m/F | PDE neo system | right lobectomy | mixed epithelial and mesenchymal, post-chemotherapy | uneven | 22 × 17 mm | 1340 | identification, surgical margin, 26 m |
| 11 | 10 | 1y/M | PDE neo system | right lobectomy | fetal, post-chemotherapy | uneven | 128 × 88 × 70 mm | 807 | identification, surgical margin, 7 m |
| 12 | 11 | 1y/M | PDE neo system | left lateral segmentectomy | fetal | uneven | 32 × 25 × 20 mm | 361.5 | identification, surgical margin, 1 m |
| 13 | 12 | 4y/M | PDE neo system | LDLT 2 | mixed epithelial and mesenchymal, post-chemotherapy | uneven | 130 × 115 × 90 mm | 545323 | identification, surgical margin, false positive, 8 m |
| Case No | Patient | Age/Sex | Device | Procedure | Primary Pathology | Fluorescence Pattern | Tumor Size | Preoperative AFP (ng/dL) | Usefulness and Disease Free Survival (Months) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 13 | 3y/M | PDE neo system | right wedge resection | NA 1 | diffuse | 6 mm | 168.8 | identification, false positive |
| 2 | 13 | 3y/M | PDE neo system | left wedge resection | NA 1 | diffuse | 7 mm | 653.1 | identification |
| 3 | 13 | 4y/M | PDE neo system | right wedge resection | NA 1 | diffuse | 7 mm | 101.7 | identification, 44 m |
| 4 | 14 | 6m/M | PDE neo, D-light | right and left wedge resection | mixed epithelial and mesenchymal type, simple subtype | diffuse | left 1.5 mm, right 1 mm | 11623.9 | identification, newly detected tumors, false positive |
| 5 | 14 | 10 m/M | PDE neo system | right and left wedge resection | mixed epithelial and mesenchymal type, simple subtype | diffuse | 6.7 mm | 963.1 | identification, newly detected tumors, false positive, 34 m |
| 6 | 15 | 7y/M | PDE neo system | right wedge resection | mixed fetal + embryonal | diffuse | 3.5 mm, 2.8 mm, 1 mm, 3 mm, 3 mm | 3428.3 | identification, newly detected tumors, false positive, 34 m |
| 7 | 16 | 11y/M | PDE neo system | right wedge resection | mixed epithelial and mesenchymal type | diffuse | 5 mm | 146324 | identification, false positive |
| 8 | 16 | 11y/M | PDE neo system | right and left wedge resection | mixed epithelial and mesenchymal type | diffuse | left 4 mm, right 1mm | 123.1 | identification |
| 9 | 16 | 13y/M | PDE neo system | right wedge resection | mixed epithelial and mesenchymal type | diffuse | 5 mm | 354.2 | identification, newly detected tumors, 11 m |
| 10 | 17 | 12y/f | PDE neo system | left wedge resection | NA 1 | diffuse | 13 mm | 16.2 | identification, 28 m |
| 11 | 18 | 3y/M | PDE neo system | right wedge resection | embryonal | diffuse | 2 mm | 1154 | identification, newly detected tumors, false positive, 45 m |
| 12 | 2 | 2y/M | PDE neo system | right and left wedge resection | combined fetal and embryonal subtype | diffuse | left 8, 6, 3, 7, 4 mm, right 2, 3, 1 mm | 11492.6 | identification, newly detected tumors |
| 13 | 2 | 4y/M | PDE neo system | right wedge resection | combined fetal and embryonal subtype | false negative | 2 mm | 31.5 | false negative |
| 14 | 2 | 4y/M | PDE neo system | right and left wedge resection | combined fetal and embryonal subtype | diffuse | left 3 mm, right 2–3 mm | 66.1 | identification, newly detected tumors |
| 15 | 2 | 5y/M | PDE neo system | right wedge resection | combined fetal and embryonal subtype | diffuse | 10 mm, 3.5 mm | 95.8 | identification, newly detected tumors, 1m |
| 16 | 19 | 20y/F | PDE neo system | right wedge resections | transitional liver cell tumor | diffuse | 9 mm | 3525 | identification, newly detected tumors |
| 17 | 19 | 21y/F | PDE neo system | right upper +middle lobectomy | transitional liver cell tumor | diffuse | 12 mm | 411 | identification, 23 m |
| Case No | Patient | Age/Sex | Device | Procedure | Primary Pathology | Fluorescence Pattern | Tumor Size | Preoperative AFP (ng/dL) | Usefulness and Disease Free Survival (Months) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 16 | 13y/M | PDE neo system | Lymphadenectomy at tracheal bifurcation | mixed epithelial and mesenchymal type | diffuse | 18 × 10 × 31 mm | 354.2 | identification, 11 m |
| 2 | 1 | 2y/F | PDE neo system | Distal pancreatectomy + lymphadenectomy | HB with teratoid features | negative | 16 × 16 mm | 5.8 | NA, 6 m |
| 3 | 1 | 1y/F | PDE neo system | Bone biopsy | HB with teratoid features | negative | NA | 643.7 | identification |
| 4 | 8 | 14y/M | PDE neo system | Resection for peritoneal nodules | wholly epithelial type and fetal subtype | diffuse | undetected | 69 | identification, 34 m |
| 5 | 15 | 7y/M | PDE neo system | Resection for peritoneal nodules | NA | diffuse | 21 × 14 × 18 mm | 525.6 | identification, tumor margin, not disease free |
| 6 | 20 | 19y/F | Pinpoint + PDE neo | Pleural and diaphragm resection | wholly epithelial type and fetal subtype | diffuse | 47 × 38 × 21 mm | 2885 | tumor margin, identification, 28 m |
| References | Number of Patients | Location | Surgical Approach/Device | ICG administration Route/Dose/Timing Prior to Operation | Cancer Detectability |
|---|---|---|---|---|---|
| Kitagawa N, 2015 [16] | 10 | Lungs | Open/PDE (Hamamatsu Photonics) | IV, 0.5 mg/kg, 24 h | 250 pulmonary metastases were identified and extirpated. PPV = 88.4% |
| Yamamichi T, 2015 [17] | 3 | Primary | Open/HyperEye Medical System MNIRC-1000 (MIZUHO Medical Co. Ltd) | IV, 0.5 mg/kg, 72–96 h | Tumor identification, tumor margin |
| Toyofumi F, 2017 [43] | 1 | Lungs | Open/Medical Imaging Projection System, (Panasonic AVC Networks) | IV, 0.5 mg/kg, 24 h | Tumor identification |
| Yamada Y, 2018 [33] | 1 | Pleura and diaphragm | Endoscope/Pinpoint System (Stryker) | IV, 0.5 mg/kg, 72 h | Tumor identification, tumor margin |
| Souzaki R, 2019 [36] | 5 | Primary and lung | Endoscope/D-Light P (Karl Storz) | IV, 0.5 mg/kg, 18-27 h (lungs), 60–138 h (primary) | Tumor identification, tumor margin, PPV = 91.6% |
| Takahashi N, 2019 [44] | 1 | Peritoneum | Open/PDE (Hamamatsu Photonics) | IV, 0.5 mg/kg, 72 h | Tumor identification, tumor margin |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yamada, Y.; Ohno, M.; Fujino, A.; Kanamori, Y.; Irie, R.; Yoshioka, T.; Miyazaki, O.; Uchida, H.; Fukuda, A.; Sakamoto, S.; et al. Fluorescence-Guided Surgery for Hepatoblastoma with Indocyanine Green. Cancers 2019, 11, 1215. https://doi.org/10.3390/cancers11081215
Yamada Y, Ohno M, Fujino A, Kanamori Y, Irie R, Yoshioka T, Miyazaki O, Uchida H, Fukuda A, Sakamoto S, et al. Fluorescence-Guided Surgery for Hepatoblastoma with Indocyanine Green. Cancers. 2019; 11(8):1215. https://doi.org/10.3390/cancers11081215
Chicago/Turabian StyleYamada, Yohei, Michinobu Ohno, Akihiro Fujino, Yutaka Kanamori, Rie Irie, Takako Yoshioka, Osamu Miyazaki, Hajime Uchida, Akinari Fukuda, Seisuke Sakamoto, and et al. 2019. "Fluorescence-Guided Surgery for Hepatoblastoma with Indocyanine Green" Cancers 11, no. 8: 1215. https://doi.org/10.3390/cancers11081215
APA StyleYamada, Y., Ohno, M., Fujino, A., Kanamori, Y., Irie, R., Yoshioka, T., Miyazaki, O., Uchida, H., Fukuda, A., Sakamoto, S., Kasahara, M., Matsumoto, K., Fuchimoto, Y., Hoshino, K., Kuroda, T., & Hishiki, T. (2019). Fluorescence-Guided Surgery for Hepatoblastoma with Indocyanine Green. Cancers, 11(8), 1215. https://doi.org/10.3390/cancers11081215





