Comparison of Diagnosis-Specific Survival Scores for Patients with Small-Cell Lung Cancer Irradiated for Brain Metastases
Abstract
:1. Introduction
2. Results
2.1. Development of the WBRT-30-SCLC
2.2. Comparison of Four Disease-Specific Survival Scores for Patients with Brain Metastasis from SCLC
3. Discussion
4. Materials and Methods
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Tsao, M.N.; Rades, D.; Wirth, A.; Lo, S.S.; Danielson, B.L.; Gaspar, L.E.; Sperduto, P.W.; Vogelbaum, M.A.; Radawski, J.D.; Wang, J.Z.; et al. Radiotherapeutic and surgical management for newly diagnosed brain metastasis(es): An American Society for Radiation Oncology evidence-based guideline. Pract. Radiat. Oncol. 2012, 2, 210–225. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yamamoto, M.; Serizawa, T.; Shuto, T.; Akabane, A.; Higuchi, Y.; Kawagishi, J.; Yamanaka, K.; Sato, Y.; Jokura, H.; Yomo, S.; et al. Stereotactic radiosurgery for patients with multiple brain metastases (JLGK0901): A multi-institutional prospective observational study. Lancet Oncol. 2014, 15, 387–395. [Google Scholar] [CrossRef]
- Schild, S.E.; Sio, T.T.; Daniels, T.B.; Chun, S.G.; Rades, D. Prophylactic cranial irradiation for extensive small-cell lung cancer. J. Oncol. Pract. 2017, 13, 732–738. [Google Scholar] [CrossRef] [PubMed]
- Rades, D.; Kieckebusch, S.; Lohynska, R.; Veninga, T.; Stalpers, L.J.; Dunst, J.; Schild, S.E. Reduction of overall treatment time in patients irradiated for more than three brain metastases. Int J. Radiat. Oncol. Biol. Phys. 2007, 69, 1509–1513. [Google Scholar] [CrossRef] [PubMed]
- DeAngelis, L.M.; Delattre, J.Y.; Posner, J.B. Radiation-induced dementia in patients cured of brain metastases. Neurology 1989, 39, 789–796. [Google Scholar] [CrossRef] [PubMed]
- Brown, P.D.; Ahluwalia, S.; Khan, O.H.; Asher, A.L.; Wefel, J.S.; Gondi, V. Whole-brain radiotherapy for brain metastases: Evolution or revolution? J. Clin. Oncol. 2018, 36, 483–491. [Google Scholar] [CrossRef] [PubMed]
- Gondi, V.; Pugh, S.L.; Tome, W.A.; Caine, C.; Corn, B.; Kanner, A.; Rowley, H.; Kundapur, V.; DeNittis, A.; Greenspoon, J.N.; et al. Preservation of memory with conformal avoidance of the hippocampal neural stem-cell compartment during whole-brain radiotherapy for brain metastases (RTOG 0933): A phase II multi-institutional trial. J. Clin. Oncol. 2014, 32, 3810–3816. [Google Scholar] [CrossRef]
- Kundapur, V.; Ellchuk, T.; Ahmed, S.; Gondi, V. Risk of hippocampal metastases in small cell lung cancer patients at presentation and after cranial irradiation: A safety profile study for hippocampal sparing during prophylactic or therapeutic cranial irradiation. Int. J. Radiat. Oncol. Biol. Phys. 2015, 91, 781–786. [Google Scholar] [CrossRef]
- Brown, P.D.; Pugh, S.; Laack, N.N.; Wefel, J.S.; Khuntia, D.; Meyers, C.; Choucair, A.; Fox, S.; Suh, J.H.; Roberge, D.; et al. Radiation Therapy Oncology Group (RTOG): Memantine for the prevention of cognitive dysfunction in patients receiving whole-brain radiotherapy: A randomized, double-blind, placebo-controlled trial. Neuro Oncol. 2013, 15, 1429–1437. [Google Scholar] [CrossRef]
- Rades, D.; Panzner, A.; Dziggel, L.; Haatanen, T.; Lohynska, R.; Schild, S.E. Dose-escalation of whole-brain radiotherapy for brain metastasis in patients with a favorable survival prognosis. Cancer 2012, 118, 3852–3859. [Google Scholar] [CrossRef]
- Gaspar, L.; Scott, C.; Rotman, M.; Asbell, S.; Phillips, T.; Wasserman, T.; McKenna, W.G.; Byhardt, R. Recursive partitioning analysis (RPA) of prognostic factors in three Radiation Therapy Oncology Group (RTOG) brain metastases trials. Int. J. Radiat. Oncol. Biol. Phys. 1997, 37, 745–751. [Google Scholar] [CrossRef]
- Sperduto, P.W.; Berkey, B.; Gaspar, L.E.; Mehta, M.; Curran, W. A new prognostic index and comparison to three other indices for patients with brain metastases: An analysis of 1960 patients in the RTOG database. Int. J. Radiat. Oncol. Biol. Phys. 2008, 70, 510–514. [Google Scholar] [CrossRef] [PubMed]
- Rades, D.; Dunst, J.; Schild, S.E. A new scoring system to predicting the survival of patients treated with whole-brain radiotherapy for brain metastases. Strahlenther. Onkol. 2008, 184, 251–255. [Google Scholar] [CrossRef] [PubMed]
- Rades, D.; Dziggel, L.; Nagy, V.; Segedin, B.; Lohynska, R.; Veninga, T.; Khoa, M.T.; Trang, N.T.; Schild, S.E. A new survival score for patients with brain metastases who received whole-brain radiotherapy (WBRT) alone. Radiother. Oncol. 2013, 108, 123–127. [Google Scholar] [CrossRef] [PubMed]
- Bernhardt, D.; Adeberg, S.; Bozorgmehr, F.; Opfermann, N.; Hoerner-Rieber, J.; König, L.; Kappes, J.; Thomas, M.; Herth, F.; Heußel, C.P.; et al. Outcome and prognostic factors in patients with brain metastases from small-cell lung cancer treated with whole brain radiotherapy. J. Neurooncol. 2017, 134, 205–212. [Google Scholar] [CrossRef] [PubMed]
- Sperduto, P.W.; Chao, S.T.; Sneed, P.K.; Luo, X.; Suh, J.; Roberge, D.; Bhatt, A.; Jensen, A.W.; Brown, P.D.; Shih, H.; et al. Diagnosis-specific prognostic factors, indexes, and treatment outcomes for patients with newly diagnosed brain metastases: A multi-institutional analysis of 4,259 patients. Int. J. Radiat. Oncol. Biol. Phys. 2010, 77, 655–661. [Google Scholar] [CrossRef]
- Sperduto, P.W.; Kased, N.; Roberge, D.; Xu, Z.; Shanley, R.; Luo, X.; Sneed, P.K.; Chao, S.T.; Weil, R.J.; Suh, J.; et al. Summary report on the graded prognostic assessment: An accurate and facile diagnosis-specific tool to estimate survival for patients with brain metastases. J. Clin. Oncol. 2012, 30, 419–425. [Google Scholar] [CrossRef]
- Rades, D.; Dziggel, L.; Segedin, B.; Oblak, I.; Nagy, V.; Marita, A.; Schild, S.E. The first survival score for patients with brain metastases from small cell lung cancer (SCLC). Clin. Neurol. Neurosurg. 2013, 115, 2029–2032. [Google Scholar] [CrossRef]
- Wong, J.; Hird, A.; Zhang, L.; Tsao, M.; Sinclair, E.; Barnes, E.; Danjoux, C.; Chow, E. Symptoms and quality of life in cancer patients with brain metastases following palliative radiotherapy. Int. J. Radiat. Oncol. Biol. Phys. 2009, 75, 1125–1131. [Google Scholar] [CrossRef]
- van Oorschot, B.; Beckmann, G.; Schulze, W.; Rades, D.; Feyer, P. Radiotherapeutic options for symptom control in breast cancer. Breast Care (Basel) 2011, 6, 14–19. [Google Scholar] [CrossRef]
- Mulvenna, P.; Nankivell, M.; Barton, R.; Faivre-Finn, C.; Wilson, P.; McColl, E.; Moore, B.; Brisbane, I.; Ardron, D.; Holt, T.; et al. Dexamethasone and supportive care with or without whole brain radiotherapy in treating patients with non-small cell lung cancer with brain metastases unsuitable for resection or stereotactic radiotherapy (QUARTZ): Results from a phase 3, non-inferiority, randomised trial. Lancet 2016, 388, 2004–2014. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, J.P.; Chakraborty, S.; Laskar, S.G.; Mummudi, N.; Patil, V.M.; Upasani, M.; Prabhash, K.; Noronha, V.; Joshi, A.; Purandare, N.; et al. Applying the QUARTZ Trial Results in Clinical Practice: Development of a Prognostic Model Predicting Poor Outcomes for Non-small Cell Lung Cancers with Brain Metastases. Clin. Oncol. (R. Coll. Radiol.) 2018, 30, 382–390. [Google Scholar] [CrossRef] [PubMed]
- Thapa, B.; Lauko, A.; Desai, K.; Venur, V.A.; Ahluwalia, M.S. Novel systemic treatments for brain metastases from lung cancer. Curr. Treat. Opt. Neurol. 2018, 20, 48. [Google Scholar] [CrossRef] [PubMed]
- Kim, R.; Keam, B.; Kim, S.; Kim, M.; Kim, S.H.; Kim, J.W.; Kim, Y.J.; Kim, T.M.; Jeon, Y.K.; Kim, D.W.; et al. Differences in tumor microenvironments between primary lung tumors and brain metastases in lung cancer patients: Therapeutic implications for immune checkpoint inhibitors. BMC Cancer 2019, 19, 19. [Google Scholar] [CrossRef] [PubMed]
- Melosky, B.; Cheema, P.; Agulnik, J.; Albadine, R.; Bebb, D.G.; Blais, N.; Burkes, R.; Butts, C.; Card, P.B.; Chan, A.M.Y.; et al. Canadian perspectives: Update on inhibition of ALK-positive tumours in advanced non-small-cell lung cancer. Curr. Oncol. 2018, 25, 317–328. [Google Scholar] [CrossRef] [PubMed]
- Kamath, S.D.; Kumthekar, P.U. Immune checkpoint inhibitors for the treatment of central nervous system (CNS) metastatic disease. Front. Oncol. 2018, 8, 414. [Google Scholar] [CrossRef] [PubMed]
- Gadgeel, S.M.; Pennell, N.A.; Fidler, M.J.; Halmos, B.; Bonomi, P.; Stevenson, J.; Schneider, B.; Sukari, A.; Ventimiglia, J.; Chen, W.; et al. Phase II Study of Maintenance Pembrolizumab in Patients with Extensive-Stage Small Cell Lung Cancer (SCLC). J. Thorac. Oncol. 2018, 13, 1393–1399. [Google Scholar] [CrossRef]
| Factor | At 3 Months (%) | At 6 Months (%) | At 9 Months (%) | At 12 Months (%) | p-Value |
|---|---|---|---|---|---|
| Age | |||||
| ≤ 64 years | 60 | 38 | 33 | 22 | |
| > 64 years | 38 | 18 | 12 | 12 | 0.002 |
| Karnofsky Performance Score | |||||
| < 70 | 20 | 0 | 0 | 0 | |
| = 70 | 52 | 34 | 28 | 28 | |
| > 70 | 76 | 52 | 42 | 28 | <0.001 |
| Systemic treatment prior to WBRT | |||||
| No | 38 | 22 | 20 | 17 | |
| Yes | 55 | 32 | 24 | 17 | 0.07 |
| Controlled primary tumor | |||||
| No | 43 | 28 | 21 | 14 | |
| Yes | 55 | 29 | 25 | 21 | 0.09 |
| Number of brain metastases | |||||
| 1–3 | 67 | 54 | 50 | 40 | |
| ≥ 4 | 42 | 18 | 11 | 7 | <0.001 |
| Extra-cerebral metastasis | |||||
| No | 58 | 50 | 41 | 39 | |
| Yes | 47 | 22 | 17 | 10 | 0.004 |
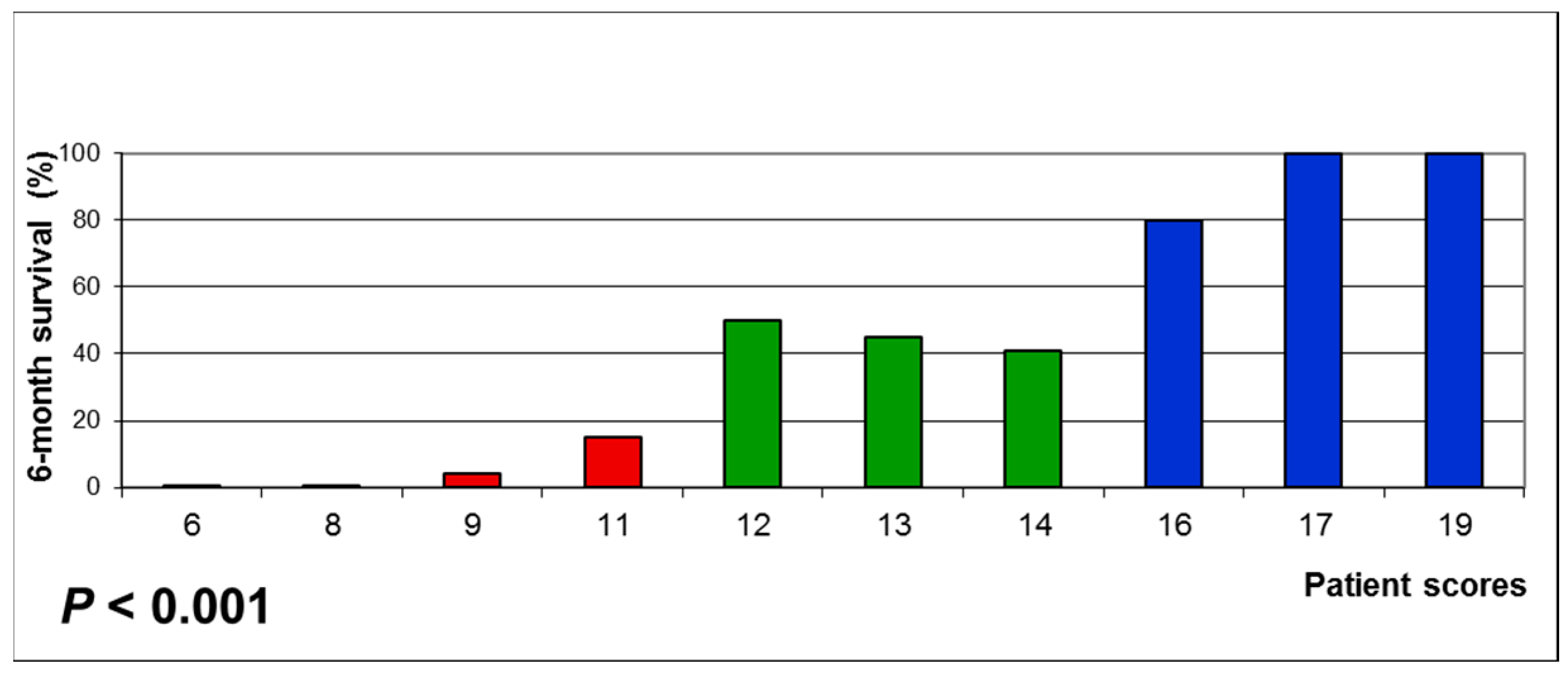
| Factor | 6-Month Survival Rate (%) | Factor Score |
|---|---|---|
| Age | ||
| ≤ 64 years | 38 | 4 |
| > 64 years | 18 | 2 |
| Karnofsky Performance Score | ||
| < 70 | 0 | 0 |
| = 70 | 34 | 3 |
| > 70 | 52 | 5 |
| Number of brain metastases | ||
| 1–3 | 54 | 5 |
| ≥ 4 | 18 | 2 |
| Extra-cerebral metastasis | ||
| No | 50 | 5 |
| Yes | 22 | 2 |
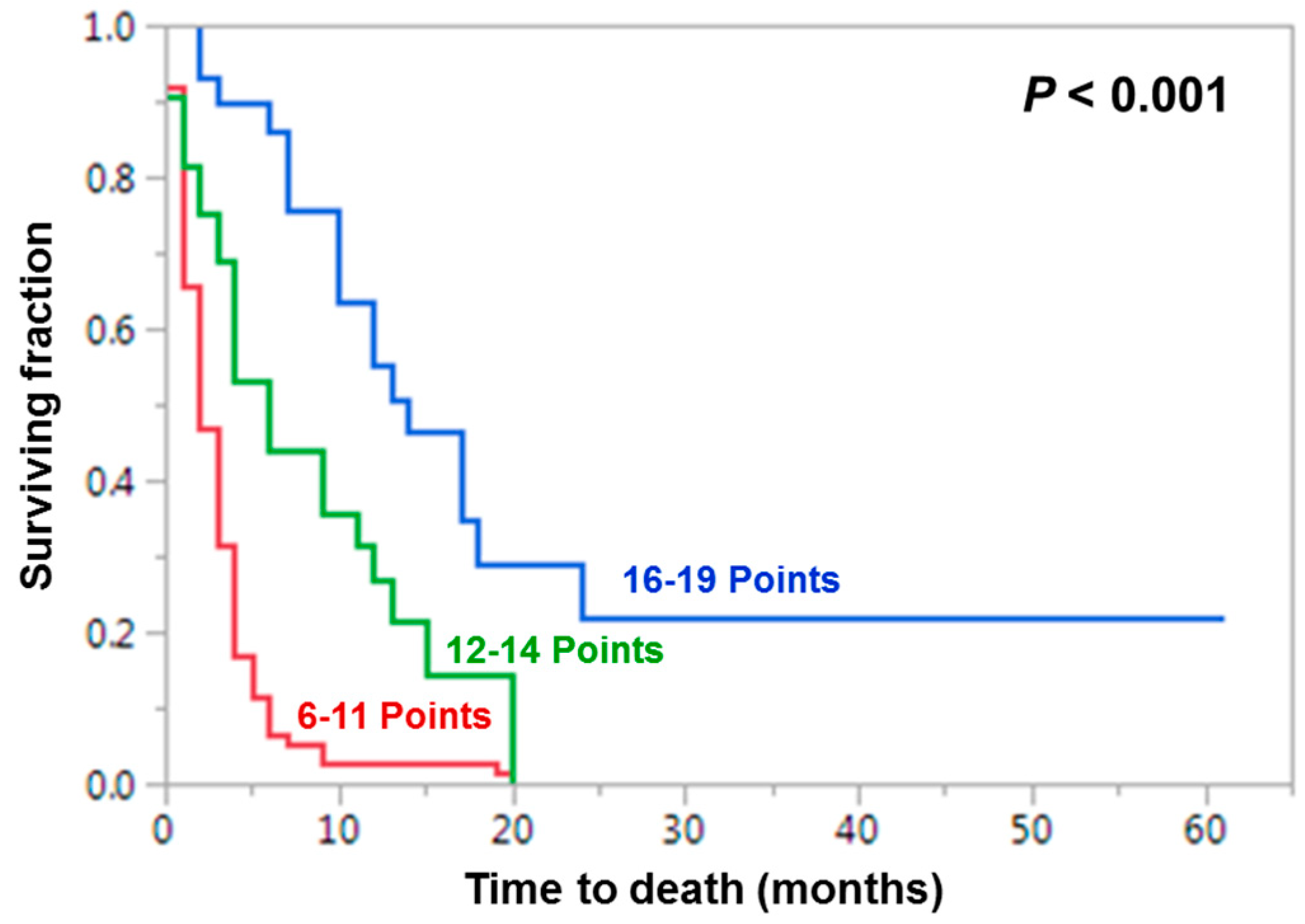
| ColuPrognostic Group | WBRT-30-SCLC | Rades-SCLC | Original DS-GPA | Updated DS-GPA | ||||
|---|---|---|---|---|---|---|---|---|
| Scoring points | 6-month Survival | Scoring points | 6-month survival | Scoring points | 6-month survival | Scoring points | 6-month survival | |
| Poor prognosis | 6–11 | 6% (6/96) | 5–8 | 0% (0/59) | 0.0–1.0 | 12% (12/103) | 0.0–1.0 | 12% (12/103) |
| Intermediate prognosis | 12–14 | 44% (14/32) | 9–12 | 40% (35/88) | 1.5–2.5 | 59% (27/46) | 1.5–2.0 | 54% (20/37) |
| Favorable prognosis | 16–19 | 86% (25/29) | 15 | 100% (10/10) | ≥ 3.0 | 75% (6/8) | ≥ 2.5 | 76% (13/17) |
| Factor | N Patients (%) |
|---|---|
| Age | |
| ≤ 64 years | 81 (52) |
| > 64 years | 76 (48) |
| Gender | |
| Female | 60 (38) |
| Male | 97 (62) |
| Karnofsky Performance Score | |
| < 70 | 61 (39) |
| = 70 | 29 (18) |
| > 70 | 67 (43) |
| Interval from diagnosis of | |
| SCLC to WBRT | |
| ≤ 2 months | 80 (51) |
| > 2 months | 77 (49) |
| Systemic treatment prior to WBRT | |
| No | 50 (32) |
| Yes | 107 (68) |
| Controlled primary tumor | |
| No | 74 (47) |
| Yes | 83 (53) |
| Number of brain metastases | |
| 1–3 | 46 (29) |
| ≥ 4 | 111 (71) |
| Extra-cerebral metastasis | |
| No | 38 (24) |
| Yes | 119 (76) |
| Colu Factor | GPA Scoring Criteria | ||
|---|---|---|---|
| 0 | 0.5 | 1.0 | |
| Age (years) | >60 | 50–60 | <50 |
| Karnofsky Performance Score | <70 | 70-80 | 90–100 |
| Extra-cerebral metastasis | present | ---- | absent |
| Number of brain metastases | >3 | 2–3 | 1 |
| Factor | 6-Month Survival Rate (%) | Factor Score |
|---|---|---|
| Karnofsky Performance Score | ||
| < 70 | 5 | 1 |
| ≥ 70 | 51 | 5 |
| Number of brain metastases | ||
| 1–3 | 54 | 5 |
| ≥ 4 | 18 | 2 |
| Extra-cerebral metastasis | ||
| No | 50 | 5 |
| Yes | 22 | 2 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rades, D.; Hansen, H.C.; Janssen, S.; Schild, S.E. Comparison of Diagnosis-Specific Survival Scores for Patients with Small-Cell Lung Cancer Irradiated for Brain Metastases. Cancers 2019, 11, 233. https://doi.org/10.3390/cancers11020233
Rades D, Hansen HC, Janssen S, Schild SE. Comparison of Diagnosis-Specific Survival Scores for Patients with Small-Cell Lung Cancer Irradiated for Brain Metastases. Cancers. 2019; 11(2):233. https://doi.org/10.3390/cancers11020233
Chicago/Turabian StyleRades, Dirk, Heinke C. Hansen, Stefan Janssen, and Steven E. Schild. 2019. "Comparison of Diagnosis-Specific Survival Scores for Patients with Small-Cell Lung Cancer Irradiated for Brain Metastases" Cancers 11, no. 2: 233. https://doi.org/10.3390/cancers11020233




