1. Introduction
Deoxynivalenol (DON) is a trichothecene mycotoxin produced by
Fusarium species, mainly
F. graminearum and
F. culmorum, and the most frequently-detected mycotoxin contaminant of maize, wheat and barley in temperate regions of the world [
1,
2]. Consumption of DON-contaminated feed has been associated with a number of adverse effects in animals, including feed refusal, vomiting, diarrhea, dizziness and fever, and chronic exposure to DON can lead to growth faltering, immunological and neurological dysfunction [
3,
4]. The acute effects of DON (or “vomitoxin”) in humans are similar to those seen in animals, and chronic dietary exposure of animals to DON causes altered nutritional efficiency [
2,
5], whilst long-term effects in humans have not been established so far. The primary toxic effect of DON is inhibition of protein synthesis, and it activates a signaling pathway known as ribotoxic stress response in cells and induces apoptosis [
4,
6]. Moreover, the effects include altered neuroendocrine signaling, impaired gut integrity and immune function [
7,
8].
DON is thus a concern for human health, and exposure early in life is of special interest in light of the following: DON transfer via the placenta to the fetus occurs in sows [
9], and maternal exposure has been linked to growth retardation [
10] and immunosuppression in the offspring [
11]. Since DON has been shown to cross also the human placenta, dietary exposure during pregnancy will lead to DON exposure of the fetus, whose detoxification mechanisms are not yet well developed [
12].
Along with conventional mycotoxin analysis in food, biomonitoring has greatly advanced an assessment of human DON exposure. As reviewed by Turner
et al. (2012) [
13], sensitive analytical methods for the analysis of DON and its metabolites in urine have been developed and validated as biomarkers of exposure: unmetabolized or “free” DON together with DON-glucuronides in urine reflect rather strong dietary mycotoxin exposure, and the mean estimated amount of biomarkers excreted within a day are rather high, with about 68% [
14] and 72% of the DON intake [
15]. As DON is largely present as a glucuronide conjugate in human urine [
14,
15], enzymatic hydrolysis of samples (deconjugation) is used in most single- or multi-analyte methods for biomarker determination to increase the detectability of total DON [
16]. Analysis should also include DOM-1, the detoxification product of DON formed by gut microbiota in animals and humans: a recent study found relatively high levels of DOM-1, indicating that a substantial proportion of DON can be detoxified in humans [
17], whilst the DOM-1 metabolite has been rarely detected or at only very low levels in urines from other cohorts [
15,
18,
19,
20].
DON biomarker occurrence has been analyzed in the urines of pregnant women from the U.K., Egypt and Croatia [
21,
22,
23]. More studies have been conducted in the general population of some Asian [
19,
24], European [
15,
18,
20,
25,
26,
27,
28,
29,
30] and African countries [
31,
32]. Overall, the results from these biomonitoring studies (in terms of frequency of detection and urinary analyte levels) indicate quite variable human exposure to DON, a finding in accord with reported differences in DON contamination of food commodities in various regions of the world [
1,
6].
When food contaminant data are scarce, as often is the case in developing countries, analysis of biomarkers in human body fluids provides useful insights, since biomonitoring covers mycotoxin intake from all dietary sources and exposure by various routes [
14,
33]. In Bangladesh, a small survey detected the presence of DON in 10 maize samples (17% positive) with the highest level of 337 µg/kg in maize from the northern part of the country [
34]. The reported DON levels did not exceed the U.S. or EU regulatory limits, but this survey focused on maize alone and did not include analysis of other possibly contaminated food commodities. In short, these data are insufficient to assess human DON exposure in Bangladesh.
Therefore, to gain more insight into maternal DON exposure during pregnancy, urine samples were collected from inhabitants of a rural and a suburban area of the Savar region in the Dhaka district of Bangladesh. The present study is the first biomarker-based DON exposure assessment for pregnant women in Bangladesh.
3. Discussion
As briefly outlined in the Introduction, DON is known to cause a range of adverse effects in animals and can also cross the placenta. Thus, exposure of pregnant women to DON is of particular concern, yet only few biomonitoring studies have been conducted so far in this group of the population.
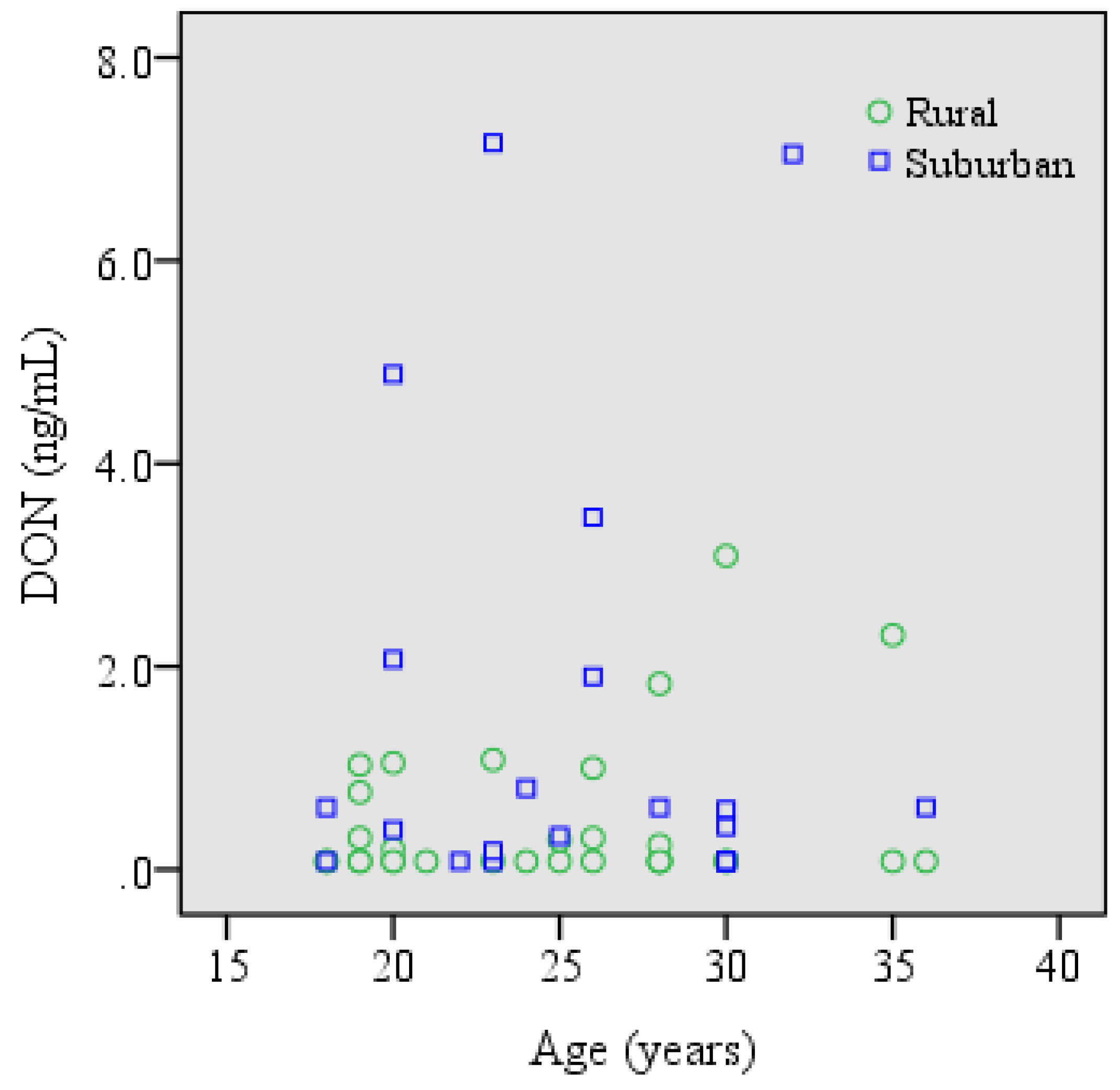
The present study is the first biomarker survey for DON exposure of pregnant women in Bangladesh: frequent detection of DON (52%) at a mean concentration of 0.86 ± 1.57 ng/mL or 2.14 ± 4.74 ng/mg creatinine (
Table 4) indicates DON exposure in pregnant women living in a rural and a suburban area of Bangladesh, albeit at comparatively moderate levels. The urinary DON concentrations determined in this study are similar to levels found in the urines of pregnant women from Egypt (geometric mean 1.11 ng/mg creatinine, range 0.5–59.9 ng/mg creatinine [
22]). On the other hand, values in our cohort (mean 2.1 ng/mg creatinine, range 0.6–24.3 ng/mg creatinine) are clearly lower than those reported for pregnant women (
n = 85) from Bradford, the U.K. (geometric mean 10.3 ng/mg creatinine, range 0.5–116.7 ng/mg creatinine [
21]) and for pregnant women (
n = 40) from Croatia (DON equivalents: mean 111.8 ng/mL, range 4.8–1238 ng/mg [
23]). The authors noted that maximum concentration in the rural sub-cohort of Croatian pregnant women indicated a nine-times higher exposure to DON than in U.K. pregnant women. Moreover, biomarker-based calculation of DON intake revealed mycotoxin exposures that clearly exceeded the tolerable daily intake (TDI) for DON of 1 µg/kg b.w., both in the U.K. and the Croatian cohort [
21,
23]. In the Bangladeshi cohort of pregnant women, even the highest calculated provisional daily DON intake of 461 ng/kg b.w. (
Table 5) did not exceed the TDI.
In our survey, DOM-1 metabolite was not detected in any of the 54 Bangladeshi urines. This is of interest, since human data on the occurrence of this detoxication product are limited. DOM-1 was found at modest levels in urines from Egyptian pregnant women (2/69; [
22]) and from French farmers (26/76; [
18]), but it was not detected in studies of U.K. adults [
20] or U.K. pregnant women [
21]. However, in a recent small pilot study with 15 volunteers who provided spot urines in two years, DOM-1 was detected in 37% and 40% of the samples: The prevalence and the proportion of DOM-1 (up to 17.8% of urinary DON in some individuals) indicated that a substantial fraction of DON can be detoxified in humans harboring gut microbiota capable of DON detoxication [
17]. Other recent studies from Europe detected DOM-1 less frequently and also at very low levels compared to DON and DON glucuronide [
28,
35,
36]. DON toxicity in humans may be also related to their ability to produce DON-glucuronide [
37]. Yet, in light of the limited availability of urines, we did not determine the ratio of free DON (aglycone) to DON-glucuronides in our cohort.
Regarding possible sources of DON intake in Bangladesh: analysis of correlations between urinary biomarker levels and food consumption pattern based on FFQ data did not show significant associations with typical food items (
Table 6), and this may be due to the overall rather low DON exposure among the participants. Interestingly, pregnant women from the suburban area had a significantly higher mean level of urinary DON and also provisional daily DON intake than our rural cohort (
Table 4 and
Table 5). The higher DON exposure in the suburban participants may be related to higher consumption of wheat bread by the suburban residents than the rural residents. However, maize cannot be excluded, since our FFQ did not assess wheat and maize consumption separately, and wheat and maize flours are sometimes mixed together for making homemade bread and also in the bakery industry in Bangladesh. A small survey reported DON contamination at a low level in maize samples collected from the northern part of Bangladesh [
34], but food analysis data for DON are not available for other staple food, such as rice or wheat.
Finally, the present biomonitoring study revealed only moderate exposure of pregnant women in Bangladesh. Nonetheless, further studies are indicated: urine samples were collected in wintertime (2014), but the country has a subtropical monsoon climate, characterized by clear seasonal variations in rainfall, temperature and humidity (
http://en.wikipedia.org/wiki/Geography_of_Bangladesh). Since the growth and distribution of
Fusarium fungi depends on climatic factors, such as moisture and temperature, quite variable DON contamination of crops cannot be excluded [
17,
38].
4. Experimental Section
4.1. Standards and Reagents
Standards for deoxynivalenol (DON), de-epoxy DON (DOM-1) and isotope-labeled internal standard ([13C15] DON) were obtained from Romer Labs Diagnostics GmbH (Tulln, Austria). The enzyme β-glucuronidase/arylsulfatase (β-Gluc/ArylS) from Helix pomatia (with specific activity 5.5 U/mL β-glucuronidase, 2.6 U/mL arylsulfatase at 37 °C) was from Roche Diagnostics (Mannheim, Germany) and used with 10-fold hydrolysis buffer (13.6 g sodium acetate hydrate, 1.0 g ascorbic acid, 0.1 g EDTA in 100 mL deionized water, adjusted to pH 5.0 with acetic acid 98%) for enzymatic treatment of urine samples. Immunoaffinity DONTest™ columns (Vicam®, purchased from Ruttmann, Hamburg, Germany) were used for clean-up and enrichment of analytes. Methanol (LC-MS grade) was purchased from Merck (Darmstadt, Germany).
4.2. Participants and Sample Collection
During February–March 2014, fifty-four pregnant women (
n = 47 in the third,
n = 6 in the second and
n = 1 in the first trimester) were recruited from a rural (Dhamrai, Dhamsona, Nolam, Paichail) and a suburban area (Baipail, Dhamrai, Kashimpur, Modhupur, Namabazar) of the Savar region in the Dhaka district of Bangladesh. All participants were apparently healthy according to external clinical examination by professional nurses. Written consent was obtained from the women before inclusion in this study. Volunteers were asked to fill out a short questionnaire for anthropometric information (age, height and weight), occupation and food habits, using the same food frequency questionnaire (FFQ) as in our previous studies in Bangladesh [
39]. The spot urine samples were collected in the morning (between 8:00 and 11:00 am) into non-sterile disposable containers and then stored at −20 °C. All urine samples were shipped on dry ice to IfADo (Dortmund, Germany) in March 2014, and biomarker analysis was conducted in January 2015. This study was approved by the Institute of Biological Sciences of Rajshahi University, Rajshahi-6205, Bangladesh (Memo no. 40/320/IAMEBBC/IDSC), and by the Institutional Internal Review Board of IfADo.
4.3. Enzymatic Hydrolysis
To cleave DON (and DOM-1) conjugates, 250 µL hydrolysis buffer (pH 5.0) and 40 µL of β-Gluc/ArylS enzyme were added to 3 mL urine aliquots and incubated at 37 °C overnight before sample extraction.
4.4. Sample Preparation
Urine sample clean-up and enrichment of analytes was performed by immunoaffinity column (IAC) extraction with DONTest™ following the protocol provided by the manufacturer (VICAM). Briefly, after rinsing the column with 1 mL of water, the entire hydrolyzed urine sample was loaded on a DONTest™ column at a flow rate of 1 drop/s. The column was washed with 5 mL distilled water, then DON was eluted (flow rate 1 drop/s) from the column using 2 mL of methanol. The elute was evaporated to dryness under a stream of nitrogen at 45 °C; the residue was dissolved in 500 µL water/methanol (90:10), vortexed and filtered through a 0.45-µm pore size Teflon syringe filter prior to LC-MS/MS analysis. Thus, the enrichment factor was 6.
4.5. LC-MS/MS Analysis
DON and its metabolite DOM-1 were measured in urine extracts by liquid chromatography with tandem mass spectrometry. Analysis was performed with a Varian 1200-L Quadrupole MS/MS equipped with an electrospray ionization (ESI) source, a Prostar® Varian HPLC system and a Varian MS Workstation version 6.9.1 data system (Agilent Technologies, Germany). The following settings were used: nitrogen as the drying gas (21 psi), gas temperature 250 °C, and argon used as the collision gas (2.0 mTorr). Chromatographic separation was carried out at 25 °C on a Nucleosil® 100-5 C18 125 × 3 mm column (Macherey-Nagel, Dŭren, Germany) with water (Mobile Phase A) and methanol (Mobile Phase B) as eluents in the following gradient: 0–1.1 min 45% B, 1.1–5.3 min 60% B, 5.3–7.3 min 95% B (column wash), 8–18 min 45% B (re-equilibration). The flow rate was 0.2 mL/min, and the injection volume was 20 µL. The retention time for DON and its metabolite DOM-1 was 4.5 and 5.6 min and for the internal standard (IS) 4.5 min. ESI-MS/MS was executed by multiple reaction monitoring (MRM) in negative ion mode. The specific transitions of precursor ion and product ion were as follows: 295.1 → 265.1 m/z and 295.1 → 138.1 for DON. The optimized collision energy (CE) was −10 and −15.5 eV, respectively. For DOM-1, the transitions of precursor and product ions were 279.1 → 248.9 and 279.1 → 231.1 m/z with an optimized CE of −9 and −13 eV, and for the internal standard (IS), the transition of precursor and product ions was 310.0 → 279.2 m/z with an optimized CE of −9 in that order.
4.6. Creatinine Analysis
Urinary creatinine was measured by a modified Jaffe method on a 96-well plate reader (Tecan Genios) [
40] to account for variability in urine dilution between individual samples. Urinary DON levels determined in ng/mL were adjusted for creatinine in the urine sample and their concentrations expressed as ng/mg creatinine to allow also comparison with other biomarker data.
4.7. Exposure Assessment
The estimation of DON intake among the participants was performed based on the results of urinary DON analysis. The following equation was used to assess the provisional daily intake (PDI) of DON among the participants:
with
C = biomarker concentration (µg/L),
V = daily urine excretion (L),
W = body weight (kg) and
E = excretion rate (%). In the calculation, urinary output during pregnancy was considered as 2 L per day [
41]. Individual body weight was used during the calculation of PDI and a daily urinary DON excretion rate of 68% [
14], a value close to estimates in other studies [
15,
42].
4.8. Food Consumption Data
All participants were asked to fill in a questionnaire with a focus on the last two days of food consumption prior to urine sampling and in addition to record their regular food habits. The food frequency questionnaire (FFQ) asked for the intake of typical food items consumed by Bangladeshi people: staple foods, mainly cereals, such as rice, wheat, maize and lentils, as the major pulses. Consumption frequency was graded 1–4 (see
Table 4). Chicken meat, eggs, groundnuts, milk and milk-based products were also included. Among these items, only rice is regularly consumed one to three times in a day and, to a lesser extent, also roti (whole wheat flatbread) for breakfast by the majority of participants.
4.9. Statistical Analysis
Descriptive statistics are presented as means (±SD), medians and interquartile ranges. Those samples containing DON below the limit of detection (LOD) were assigned a value of one-half the detection limit for the calculation of mean and median values, since this is considered a better approach to estimate average concentrations for left censored data, rather than assigning a value of zero to measurements below the detection limit [
43]. Differences in urinary DON levels between the rural and the suburban cohort were analyzed by an independent sample
t-test. The Spearman correlation coefficient (two-tailed) was used to assess the correlation between urinary DON concentration with food consumption, age and body mass index (BMI) of the participants. All analyses were carried out using IBM SPSS Statistics Version 22. A level of alpha 0.05 was assigned for statistical significance.