On The Role of Natural Killer Cells in Neurodegenerative Diseases
Abstract
:1. Introduction
1.1. Natural Killer (NK) Cells Express G Protein-Coupled Receptors
1.2. NK Cells Contain Different Subsets
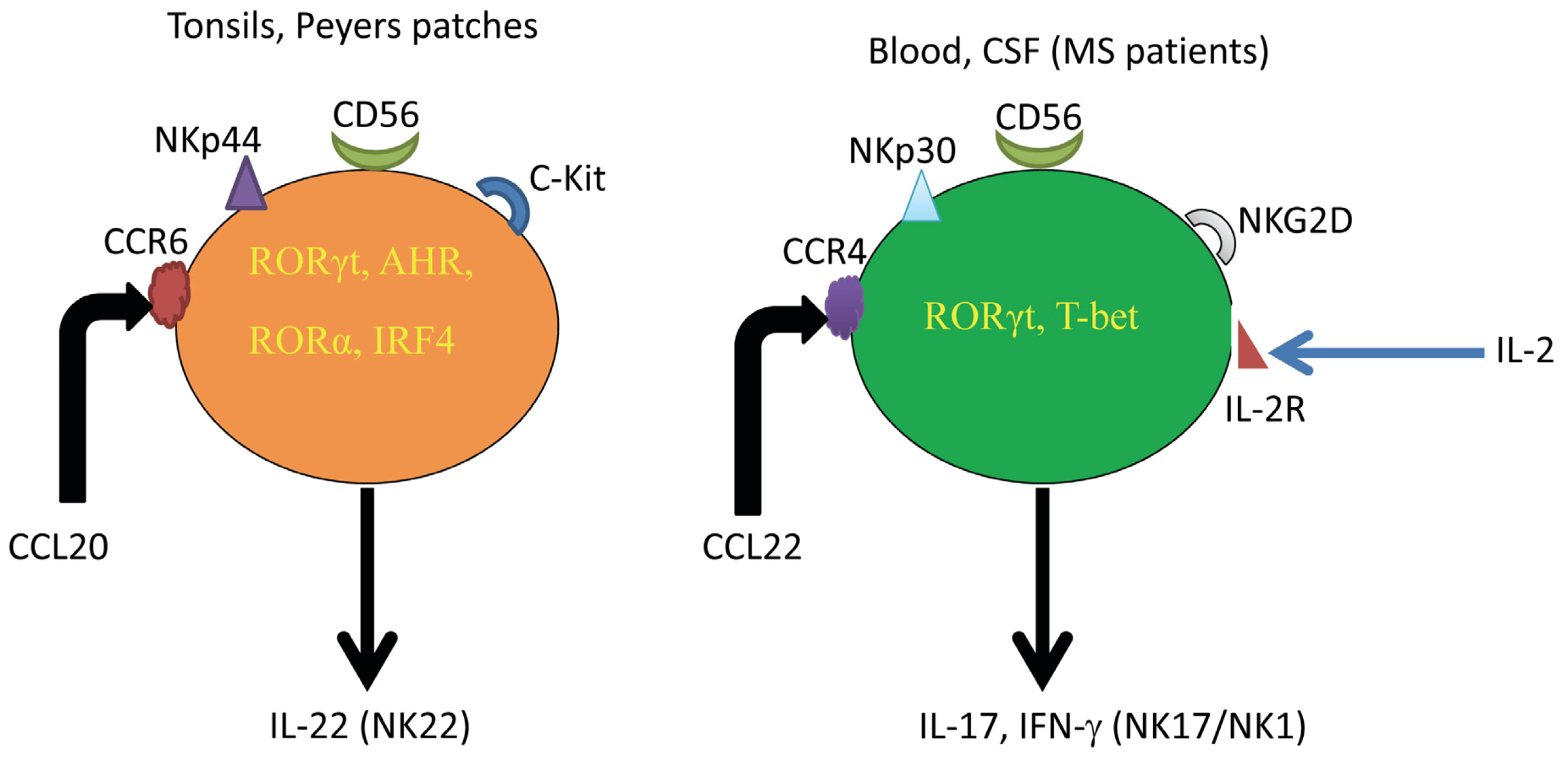
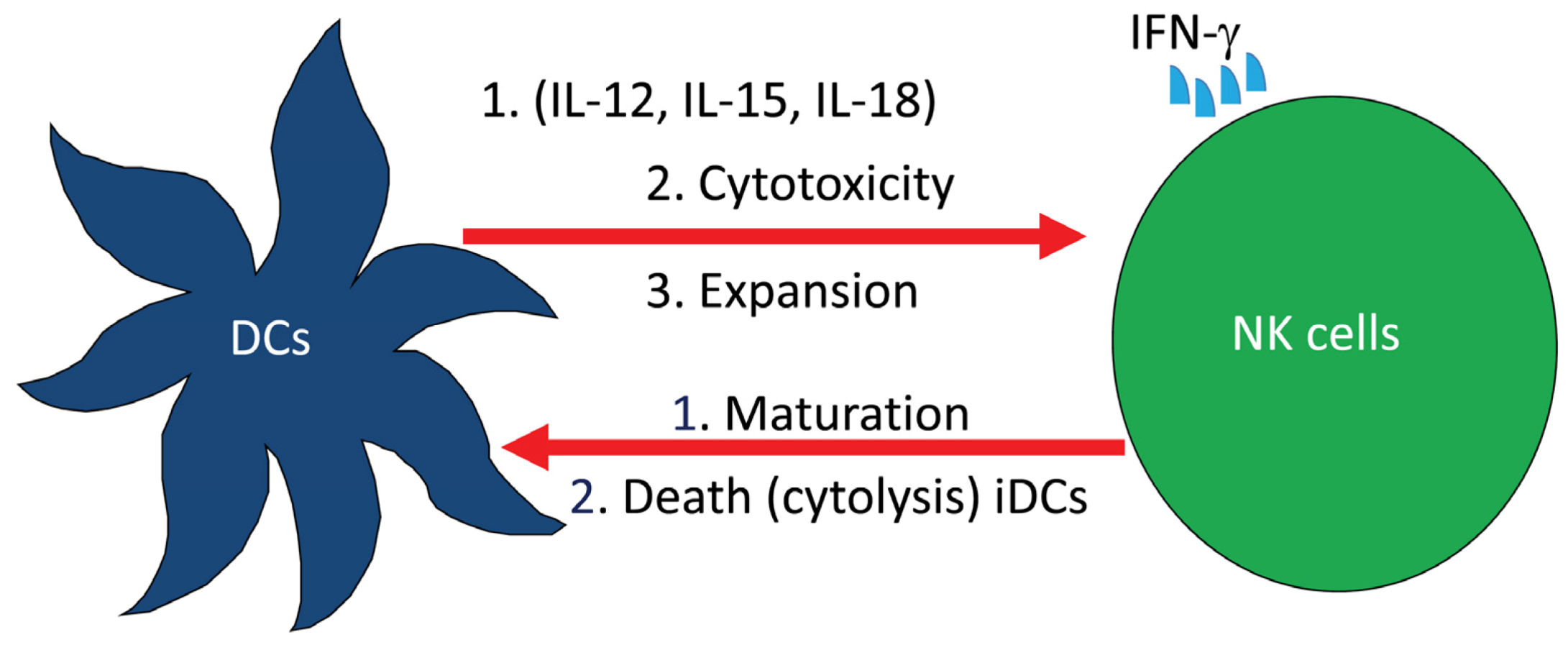
2. Role of NK Cells in Multiple Sclerosis (MS)
3. Role of NK Cells in Globoid Cell Leukodystrophy (GLD)

4. Conclusions
Acknowledgments
Conflict of Interests
References
- Cooper, M.A.; Yokoyama, W.M. Memory-like responses of natural killer cells. Immunol. Rev. 2010, 235, 297–305. [Google Scholar]
- Wood, S.M.; Ljunggren, H.G.; Bryceson, Y.T. Insights into NK cell biology from human genetics and disease associations. Cell. Mol. Life Sci. 2011, 68, 3479–3493. [Google Scholar] [CrossRef]
- Moretta, A.; Bottino, C.; Vitale, M.; Pende, D.; Cantoni, C.; Mingari, M.C.; Biassoni, R.; Moretta, L. Activating receptors and coreceptors involved in human natural killer cell-mediated cytolysis. Annu. Rev. Immunol. 2001, 19, 197–223. [Google Scholar] [CrossRef]
- Ljunggren, H.G.; Malmberg, K.J. Prospects for the use of NK cells in immunotherapy of human cancer. Nat. Rev. Immunol. 2007, 7, 329–339. [Google Scholar] [CrossRef]
- Yang, Q.; Goding, S.R.; Hokland, M.E.; Basse, P.H. Antitumor activity of NK cells. Immunol. Res. 2006, 36, 13–25. [Google Scholar] [CrossRef]
- Salazar-Mather, T.P.; Lewis, C.A.; Biron, C.A. Type I interferons regulate inflammatory cell trafficking and macrophage inflammatory protein 1α delivery to the liver. J. Clin. Invest. 2002, 110, 321–330. [Google Scholar]
- Maghazachi, A.A.; Al-Aoukaty, A. Chemokines activate natural killer cells through heterotrimeric G-proteins: Implications for the treatment of AIDS and cancer. FASEB J. 1998, 12, 913–924. [Google Scholar]
- Cooper, M.A.; Fehniger, T.A.; Caligiuri, M.A. The biology of human natural killer-cell subsets. Trends Immunol. 2001, 22, 633–640. [Google Scholar] [CrossRef]
- Rolstad, B.; Herberman, R.B.; Reynolds, C.W. Natural killer cell activity in the rat. V. The circulation patterns and tissue localization of peripheral blood large granular lymphocytes (LGL). J. Immunol. 1986, 136, 2800–2808. [Google Scholar]
- Sandel, M.H.; Speetjens, F.M.; Menon, A.G.; Albertsson, P.A.; Basse, P.H.; Hokland, M.; Nagelkerke, J.F.; Tollenaar, R.A.; van de Velde, C.J.; Kuppen, P.J. Natural killer cells infiltrating colorectal cancer and MHC class I expression. Mol. Immunol. 2005, 42, 541–546. [Google Scholar] [CrossRef]
- Kuppen, P.J.; Gorter, A.; Hagenaars, M.; Jonges, L.E.; Giezeman-Smits, K.M.; Nagelkerke, J.F.; Fleuren, G.; van de Velde, C.J. Role of NK cells in adoptive immunotherapy of metastatic colorectal cancer in a syngeneic rat model. Immunol. Rev. 2001, 184, 236–243. [Google Scholar]
- Maghazachi, A.A. Compartmentalization of human natural killer cells. Mol. Immunol. 2005, 42, 523–529. [Google Scholar] [CrossRef]
- Maghazachi, A.A. Role of natural killer cells in multiple sclerosis. ISRN Immunol. 2012. [Google Scholar] [CrossRef]
- Schleinitz, N.; Vély, F.; Harlé, J.R.; Vivier, E. Natural killer cells in human autoimmune diseases. Immunology 2010, 131, 451–458. [Google Scholar] [CrossRef]
- Dalbeth, N.; Callan, M.F.C. A subset of natural killer cells is greatly expanded within inflamed joints. Arthritis Rheum. 2002, 46, 1763–1772. [Google Scholar] [CrossRef]
- Schurgers, E.; Billiau, A.; Matthys, P. Collagen-induced arthritis as an animal model for rheumatoid arthritis: Focus on interferon-γ. J. Interferon Cytokine Res. 2011, 31, 917–926. [Google Scholar] [CrossRef]
- Kveberg, L.; Bryceson, Y.; Inngjerdingen, M.; Rolstad, B.; Maghazachi, A.A. Sphingosine 1 phosphate induces the chemotaxis of human natural killer cells. Role for heterotrimeric G proteins and phosphoinositide 3 kinases. Eur. J. Immunol. 2002, 32, 1856–1864. [Google Scholar] [CrossRef]
- Jin, Y.; Knudsen, E.; Wang, L.; Maghazachi, A.A. Lysophosphatidic acid induces human natural killer cell chemotaxis and intracellular calcium mobilization. Eur. J. Immunol. 2003, 33, 2083–2089. [Google Scholar] [CrossRef]
- Rolin, J.; Maghazachi, A.A. Effects of lysophospholipids on tumor microenvironment. Cancer Microenviron. 2011, 4, 393–403. [Google Scholar] [CrossRef]
- Martins, L.C.; Rocha, N.P.; Torres, K.C.; dos Santos, R.R.; França, G.S.; de Moraes, E.N.; Mukhamedyarov, M.A.; Zefirov, A.L.; Rizvanov, A.A.; Kiyasov, A.P.; et al. Disease-specific expression of the serotonin-receptor 5-HT(2C) in natural killer cells in Alzheimer’s dementia. J. Neuroimmunol. 2012, 251, 73–79. [Google Scholar] [CrossRef]
- Masera, R.G.; Prolo, P.; Sartori, M.L.; Staurenghi, A.; Griot, G.; Ravizza, L.; Dovio, A.; Chiappelli, F.; Angeli, A. Mental deterioration correlates with response of natural killer (NK) cell activity to physiological modifiers in patients with short history of Alzheimer’s disease. Psychoneuroendocrinology 2002, 27, 447–461. [Google Scholar] [CrossRef]
- Peritt, D.; Robertson, S.; Gri, G.; Showe, L.; Aste-Amezaga, M.; Trinchieri, G. Differentiation of human NK cells into NK1 and NK2 subsets. J. Immunol. 1998, 161, 5821–5824. [Google Scholar]
- Berahovich, R.D.; Lai, N.L.; Wei, Z.; Lanier, L.L.; Schall, T.J. Evidence for NK cell subsets based on chemokine receptor expression. J. Immunol. 2006, 177, 7833–7840. [Google Scholar]
- Cella, M.; Fuchs, A.; Vermi, W.; Facchetti, F.; Otero, K.; Lennerz, J.K.; Doherty, J.M.; Mills, J.C.; Colonna, M. A human natural killer cell subset provides an innate source of IL-22 for mucosal immunity. Nature 2009, 457, 722–725. [Google Scholar] [CrossRef]
- Sanos, S.L.; Bui, V.L.; Mortha, A.; Oberle, K.; Heners, C.; Johner, C.; Diefenbach, A. RORγt and commensal microflora are required for the differentiation of mucosal interleukin 22-producing NKp46+ cells. Nat. Immunol. 2009, 10, 83–91. [Google Scholar]
- Hughes, T.; Becknell, B.; McClory, S.; Briercheck, E.; Freud, A.G.; Zhang, X.; Mao, H.; Nuovo, G.; Yu, J.; Caligiuri, M.A. Stage 3 immature human natural killer cells found in secondary lymphoid tissue constitutively and selectively express the TH17 cytokine interleukin-22. Blood 2009, 113, 4008–4010. [Google Scholar] [CrossRef]
- Pandya, A.D.; Al-Jaderi, Z.; Høglund, R.A.; Holmøy, T.; Harbo, H.F.; Norgauer, J.; Maghazachi, A.A. Identification of human NK17/NK1 cells. PLoS One 2011, 6, e26780. [Google Scholar]
- Hwang, S.Y.; Kim, J.Y.; Kim, K.W.; Park, M.K.; Moon, Y.; Kim, W.U.; Kim, H.Y. IL-17 induces production of IL-6 and IL-8 in rheumatoid arthritis synovial fibroblasts via NF-κB- and PI3-kinase/Akt-dependent pathways. Arthritis. Res. Ther. 2004, 6, R120–R128. [Google Scholar] [CrossRef] [Green Version]
- Sylvester, J.; Liacini, A.; Li, W.Q.; Zafarullah, M. Interleukin-17 signal transduction pathways implicated in inducing matrix metalloproteinase-3, -13 and aggrecanase-1 genes in articular chondrocytes. Cell. Signal. 2004, 16, 469–476. [Google Scholar] [CrossRef]
- Honorati, M.C.; Neri, S.; Cattini, L.; Facchini, A. Interleukin-17, a regulator of angiogenic factor release by synovial fibroblasts. Osteoarthr. Cartil. 2006, 14, 345–352. [Google Scholar]
- O’Connor, W., Jr.; Kamanaka, M.; Booth, C.J.; Town, T.; Nakae, S.; Iwakura, Y.; Kolls, J.K.; Flavell, R.A. A protective function for interleukin 17A in T cell-mediated intestinal inflammation. Nat. Immunol. 2009, 10, 603–609. [Google Scholar] [CrossRef]
- Troitskaya, M.; Baysa, A.; Vaage, J.; Sand, K.L.; Maghazachi, A.A.; Valen, G. Interleukin-17 (IL-17) Expression is reduced during acute myocardial infarction: Role on chemokine receptor expression in monocytes and their in vitro chemotaxis towards chemokines. Toxins 2012, 4, 1427–1439. [Google Scholar] [CrossRef]
- Gold, R.; Linington, C.; Lassmann, H. Understanding pathogenesis and therapy of multiple sclerosis via animal models: 70 years of merits and culprits in experimental autoimmune encephalomyelitis. Brain 2006, 129, 1953–1971. [Google Scholar] [CrossRef]
- Friese, M.A.; Montalban, X.; Wilcox, N.; Bell, J.I.; Martin, R.; Fugger, L. The value of animal models for drug development in multiple sclerosis. Brain 2006, 129, 1940–1952. [Google Scholar] [CrossRef]
- Hestvick, A.L.K. The Double-edged sword of autoimmunity: Lessons from multiple sclerosis. Toxins 2010, 2, 856–877. [Google Scholar] [CrossRef]
- Shi, F.-D.; Zhou, Q. Natural killer cells as indispensable players and therapeutic targets in autoimmunity. Autoimmunity 2011, 44, 3–10. [Google Scholar] [CrossRef]
- Maghazachi, A.A. Role of chemokines in the biology of natural killer cells. Curr. Top. Microbiol. Immunol. 2010, 341, 37–58. [Google Scholar] [CrossRef]
- Segal, B.M. The role of natural killer cells in curbing neuroinflammation. J. Neuroimmunol. 2007, 191, 2–7. [Google Scholar] [CrossRef]
- Takahashi, K.; Aranami, T.; Endoh, M.; Miyake, S.; Yamamura, T. The regulatory role of natural killer cells in multiple sclerosis. Brain 2004, 127, 1917–1927. [Google Scholar] [CrossRef]
- Huang, D.; Shi, F.D.; Jung, S.; Pien, G.C.; Wang, J.; Salazar-Mather, T.P.; He, T.T.; Weaver, J.T.; Ljunggren, H.G.; Biron, C.A.; et al. The neuronal chemokine CX3CL1/fractalkine selectively recruits NK cells that modify experimental autoimmune encephalomyelitis within the central nervous system. FASEB J. 2006, 20, 896–905. [Google Scholar] [CrossRef]
- Hao, J.; Liu, R.; Piao, W.; Zhou, Q.; Vollmer, T.L.; Campagnolo, D.I.; Xiang, R.; la Cava, A.; Van Kaer, L.; Shi, F.D. Central nervous system (CNS)-resident natural killer cells suppress Th17 responses and CNS autoimmune pathology. J. Exp. Med. 2010, 207, 1907–1921. [Google Scholar] [CrossRef]
- Kastrukoff, L.F.; Morgan, N.G.; Zecchini, D.; White, R.; Petkau, A.J.; Satoh, J.; Paty, D.W. A role for natural killer cells in the immunopathogenesis of multiple sclerosis. J. Neuroimmunol. 1998, 86, 123–133. [Google Scholar] [CrossRef]
- Pagenstecher, A.; Lassmann, S.; Carson, M.J.; Kincaid, C.L.; Stalder, A.K.; Campbell, I.L. Astrocyte-targeted expression of IL-12 induces active cellular immune responses in the central nervous system and modulates experimental allergic encephalomyelitis. J. Immunol. 2000, 164, 4481–4492. [Google Scholar]
- Shi, F.D.; Takeda, K.; Akira, S.; Sarvetnick, N.; Ljunggren, H.G. IL-18 directs autoreactive T cells and promotes autodestruction in the central nervous system via induction of IFN-γ by NK cells. J. Immunol. 2000, 165, 3099–3104. [Google Scholar]
- Winkler-Pickett, R.; Young, H.A.; Cherry, J.M.; Diehl, J.; Wine, J.; Back, T.; Bere, W.E.; Mason, A.T.; Ortaldo, J.R. In vivo regulation of experimental autoimmune encephalomyelitis by NK cells: Alteration of primary adaptive responses. J. Immunol. 2008, 180, 4495–4506. [Google Scholar]
- Kala, M.; Miravalle, A.; Vollmer, T. Recent insights into the mechanism of action of glatiramer acetate. J. Neuroimmunol. 2011, 235, 9–17. [Google Scholar] [CrossRef]
- Johnson, K.P.; Brooks, B.R.; Ford, C.C.; Goodman, A.D.; Lisak, R.P.; Myers, L.W.; Pruitt, A.A.; Rizzo, M.A.; Rose, J.W.; Weiner, L.P.; Wolinsky, J.S. Glatiramer acetate (Copaxone): Comparison of continuous versus delayed therapy in a six-year organized multiple sclerosis trial. Multiple Sclerosis 2003, 9, 585–591. [Google Scholar] [CrossRef]
- Arnon, R.; Aharoni, R. Mechanism of action of glatiramer acetate in multiple sclerosis and its potential for the development of new applications. Proc. Natl. Acad. Sci. USA 2004, 101, 14593–14598. [Google Scholar] [CrossRef]
- Høglund, R.A.; Holmøy, T.; Harbo, H.F.; Maghazachi, A.A. A one year follow-up study of natural killer and dendritic cells activities in multiple sclerosis patients receiving glatiramer acetate (GA). PLoS One 2013, in press. [Google Scholar]
- Moretta, A. Natural killer cells and dendritic cells: Rendezvous in abused tissues. Nat. Rev. Immunol. 2002, 2, 957–964. [Google Scholar] [CrossRef]
- Sand, K.L.; Knudsen, E.; Rolin, J.; Al-Falahi, Y.; Maghazachi, A.A. Modulation of natural killer cell cytotoxicity and cytokine release by the drug glatiramer acetate. Cell. Mol. Life Sci. 2009, 66, 1446–1456. [Google Scholar] [CrossRef]
- Al-Falahi, Y.; Sand, K.L.; Knudsen, E.; Damaj, B.B.; Rolin, J.; Maghazachi, A.A. Splenic natural killer cell activity in two models of experimental neurodegenerative diseases. J. Cell. Mol. Med. 2009, 13, 2693–2703. [Google Scholar] [CrossRef]
- Hidalgo, E.; Essex, S.J.; Yeo, L.; Curnow, S.J.; Filer, A.; Cooper, M.S.; Thomas, A.M.; McGettrick, H.M.; Salmon, M.; Buckley, C.D.; et al. The response of T cells to interleukin-6 is differentially regulated by the microenvironment of the rheumatoid synovial fluid and tissue. Arthritis Rheum. 2011, 63, 3284–3293. [Google Scholar]
- Krabbe, K. A new familial, infantile form of diffuse brain sclerosis. Brain 1916, 30, 74–114. [Google Scholar] [CrossRef]
- Svennerholm, L.; Vanier, M.-T.; Månsson, J.E. Krabbe disease: A galactosylsphingosine (psychosine) lipidosis. J. Lipid Res. 1980, 21, 53–64. [Google Scholar]
- Vanier, M.-T.; Svennerholm, L. Chemical pathology of Krabbe’s disease. III. Ceramide hexosides and gangliosides of brain. Acta Paediatr. Scand. 1975, 64, 641–648. [Google Scholar] [CrossRef]
- Baskin, G.B.; Ratterree, M.; Davison, B.B.; Falkenstein, K.P.; Clarke, M.R.; England, J.D.; Vanier, M.T; Luzi, P.; Rafi, M.A.; Wenger, D.A. Genetic galactocerebrosidase deficiency (globoid cell leukodystrophy, Krabbe disease) in rhesus monkeys (Macaca mulatta). Lab. Anim. Sci. 1998, 48, 476–482. [Google Scholar]
- Wenger, D.A. Murine, canine and non-human primate models of Krabbe disease. Mol. Med. Today 2000, 6, 449–451. [Google Scholar] [CrossRef]
- Wenger, D.A.; Victoria, T.; Rafi, M.A.; Luzi, P.; Vanier, M.T.; Vite, C.; Patterson, D.F.; Haskins, M.H. Globoid cell leukodystrophy in cairn and West Highland white terriers. J. Hered. 1990, 90, 138–142. [Google Scholar]
- Sigurdson, C.J.; Basaraba, R.J.; Mazzaferro, E.M.; Gould, D.H. Globoid cell-like leukodystrophy in a domestic longhaired cat. Vet. Pathol. 2002, 39, 494–496. [Google Scholar] [CrossRef]
- Whitfield, P.D.; Sharp, P.C.; Taylor, R.; Meikle, P. Quantification of galactosylsphingosine in the twitcher mouse using electrospray ionization-tandem mass spectrometry. J. Lipid Res. 2001, 42, 2092–2095. [Google Scholar]
- White, A.B.; Givogri, M.I.; Lopez-Rosas, A.; Cao, H.; van Breemen, R.; Thinakaran, G.; Bongarzone, E.R. Psychosine accumulates in membrane microdomains in the brain of krabbe patients, disrupting the raft architecture. J. Neurosci. 2009, 29, 6068–6077. [Google Scholar]
- Duchen, L.W.; Eicher, E.M.; Jacobs, J.M.; Scaravilli, F.; Teixeira, F. Hereditary leucodystrophy in the mouse: The new mutant twitcher. Brain 1980, 103, 695–710. [Google Scholar] [CrossRef]
- Tanaka, K.; Nagara, H.; Kobayashi, T.; Goto, I. The twitcher mouse: Accumulation of galactosylsphingosine and pathology of sciatic nerve. Brain Res. 1988, 454, 340–346. [Google Scholar] [CrossRef]
- Jatana, M.; Giri, S.; Singh, A.K. Apoptotic positive cells in Krabbe brain and induction of apoptosis in rat C6 glial cells by psychosine. Neurosci. Lett. 2002, 330, 183–187. [Google Scholar] [CrossRef]
- Haq, E.; Giri, S.; Singh, I.; Singh, A.K. Molecular mechanism of psychosine-induced cell death in human oligodendrocyte cell line. J. Neurochem. 2003, 86, 1428–1440. [Google Scholar] [CrossRef]
- Huang, J.Q.; Trasler, J.M.; Igdoura, S.; Michaud, J.; Hanal, N.; Gravel, R.A. Apoptotic cell death in mouse models of GM2 gangliosidosis and observations on human Tay-Sachs and Sandhoff diseases. Hum. Mol. Genet. 1997, 6, 1879–1885. [Google Scholar] [CrossRef]
- Choi, J.W.; Lee, S.Y.; Choi, Y. Identification of a putative G protein-coupled receptor induced during activation-induced apoptosis of T cells. Cell. Immunol. 1996, 168, 78–84. [Google Scholar] [CrossRef]
- Kyaw, H.; Zeng, Z.; Su, K.; Fan, P.; Shell, B.K.; Carter, K.C.; Li, Y. loning, characterization, and mapping of human homolog of mouse T-cell death-associated gene. DNA Cell Biol. 1998, 17, 493–500. [Google Scholar] [CrossRef]
- Maghazachi, A.A.; Knudsen, E.; Jin, Y.; Jenstad, M.; Chaudhry, F.A. D-galactosyl-β1–1’ sphingosine and D-glucosyl-β1–1’ sphingosine induce human natural killer cell apoptosis. Biochem. Biophys. Res. Commun. 2004, 320, 810–815. [Google Scholar] [CrossRef]
- Sabatelli, M.; Quaranta, L.; Madia, F.; Lippi, G.; Conte, A.; lo Monaco, M.; di Trapani, G.; Rafi, M.A.; Wenger, D.A.; Vaccaro, A.M.; Tonali, P. Peripheral neuropathy with hypomyelinating features in adult-onset Krabbe’s disease. Neuromuscular Disord. 2002, 12, 386–391. [Google Scholar] [CrossRef]
- Wenger, D.A.; Coppola, S.; Liu, S.-L. Insights into the diagnosis and treatment of lysosomal storage diseases. Arch. Neurol. 2003, 60, 322–328. [Google Scholar] [CrossRef]
- Kondo, Y.; Adams, J.M.; Vanier, M.T.; Duncan, I.D. Macrophages counteract demyelination in a mouse model of globoid cell leukodystrophy. J. Neurosci. 2011, 31, 3610–3624. [Google Scholar]
- Ichioka, T.; Kishimoto, Y.; Brennan, S.; Santos, G.W.; Yeager, A.M. Hematopoietic cell transplantation in murine globoid cell leukodystrophy (the twitcher mouse): Effects on levels of galactosylceramidase, psychosine, and galactocerebrosides. Proc. Natl. Acad. Sci. USA 1987, 84, 4259–4263. [Google Scholar] [CrossRef]
- Yeager, A.M.; Brennan, S.; Tiffany, C.; Moser, H.W.; Santos, G.W. Prolonged survival and remyelination after hematopoietic cell transplantation in the twitcher mouse. Science 1984, 225, 1052–1054. [Google Scholar]
- Scruggs, B.A.; Bowles, A.C.; Zhang, X.; Semon, J.A.; Kyzar, E.J.; Myers, L.; Kalueff, A.V.; Bunnell, B.A. High-throughput screening of stem cell therapy for globoid cell leukodystrophy using automated neurophenotyping of twitcher mice. Behav. Brain Res. 2013, 236, 35–47. [Google Scholar] [CrossRef]
- Krivit, W.; Shapiro, E.G.; Peters, C.; Wagner, J.E.; Cornu, G.; Kurtzberg, J.; Wenger, D.A.; Kolodny, E.H.; Vanier, M.T.; Loes, D.J.; et al. Hematopoietic stem-cell transplantation in globoid-cell leukodystrophy. N. Engl. J. Med. 1998, 338, 1119–1126. [Google Scholar] [CrossRef]
- Rafi, M.A.; Rao, H.Z.; Luzi, P.; Curtis, M.T.; Wenger, D.A. Extended normal life after AAVrh10-mediated gene therapy in the mouse model of krabbe disease. Mol. Ther. 2012, 20, 2031–2042. [Google Scholar] [CrossRef]
- Qin, E.Y.; Hawkins-Salsbury, J.A.; Jiang, X.; Reddy, A.S.; Farber, N.B.; Ory, D.S.; Sands, M.S. Bone marrow transplantation increases efficacy of central nervous system-directed enzyme replacement therapy in the murine model of globoid cell leukodystrophy. Mol. Genet. Metab. 2012, 107, 186–196. [Google Scholar] [CrossRef]
- Reddy, A.S.; Kim, J.H.; Hawkins-Salsbury, J.A.; Macauley, S.L.; Tracy, E.T.; Vogler, C.A.; Han, X.; Song, S.K.; Wozniak, D.F.; Fowler, S.C.; Klein, R.S.; Sands, M.S. Bone marrow transplantation augments the effect of brain- and spinal cord-directed adeno-associated virus 2/5 gene therapy by altering inflammation in the murine model of globoid-cell leukodystrophy. J. Neurosci. 2011, 31, 9945–9957. [Google Scholar]
© 2013 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Maghazachi, A.A. On The Role of Natural Killer Cells in Neurodegenerative Diseases. Toxins 2013, 5, 363-375. https://doi.org/10.3390/toxins5020363
Maghazachi AA. On The Role of Natural Killer Cells in Neurodegenerative Diseases. Toxins. 2013; 5(2):363-375. https://doi.org/10.3390/toxins5020363
Chicago/Turabian StyleMaghazachi, Azzam A. 2013. "On The Role of Natural Killer Cells in Neurodegenerative Diseases" Toxins 5, no. 2: 363-375. https://doi.org/10.3390/toxins5020363



