Alterations in Circulating Amino Acid Metabolite Ratio Associated with Arginase Activity Are Potential Indicators of Metabolic Syndrome: The Korean Genome and Epidemiology Study
Abstract
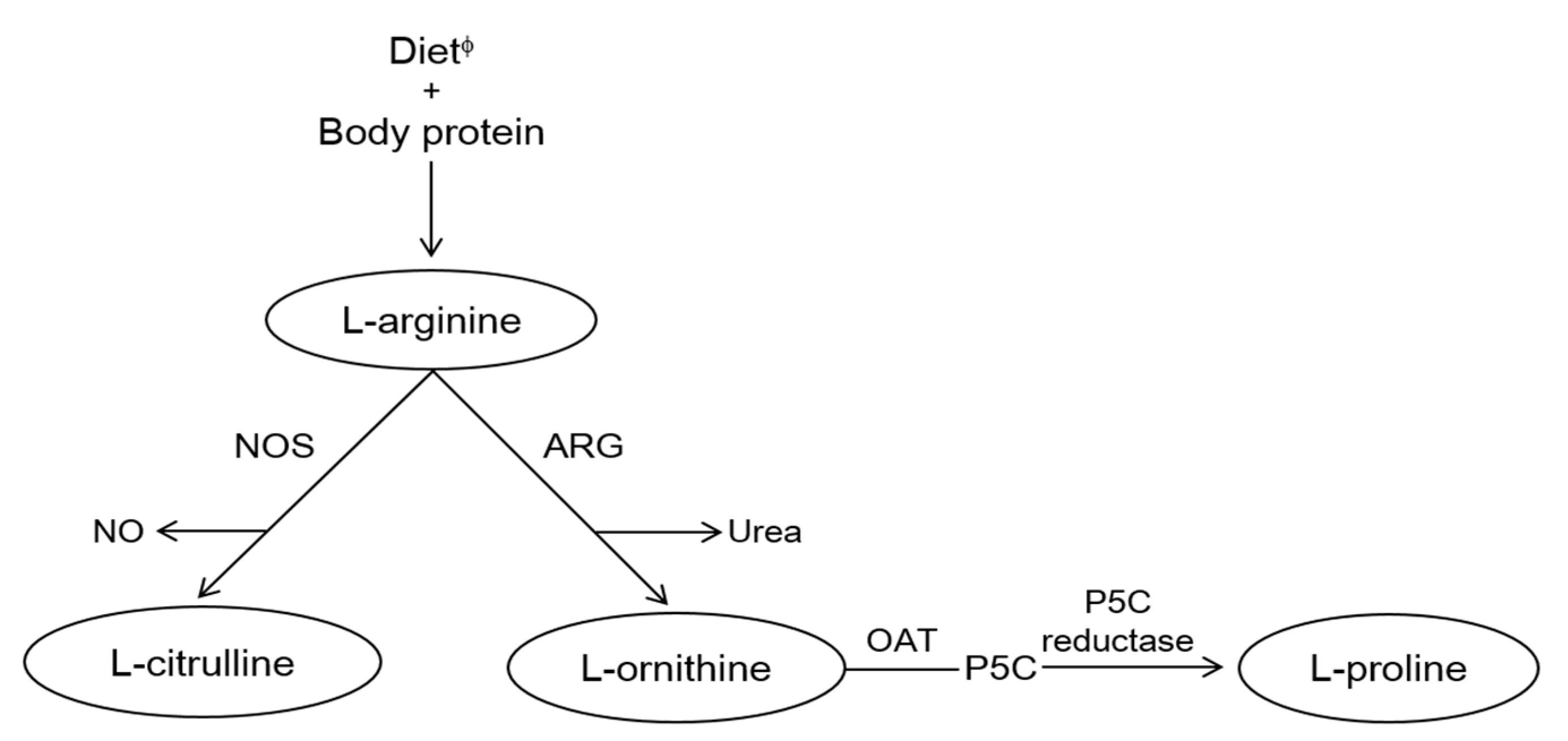
:1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. General Information, Anthropometric and Biochemical Measurements
2.3. Metabolite Measurement
2.4. Definition of Metabolic Syndrome
2.5. Statistical Analysis
3. Results
3.1. General Characteristics of Participants According to Metabolic Syndrome
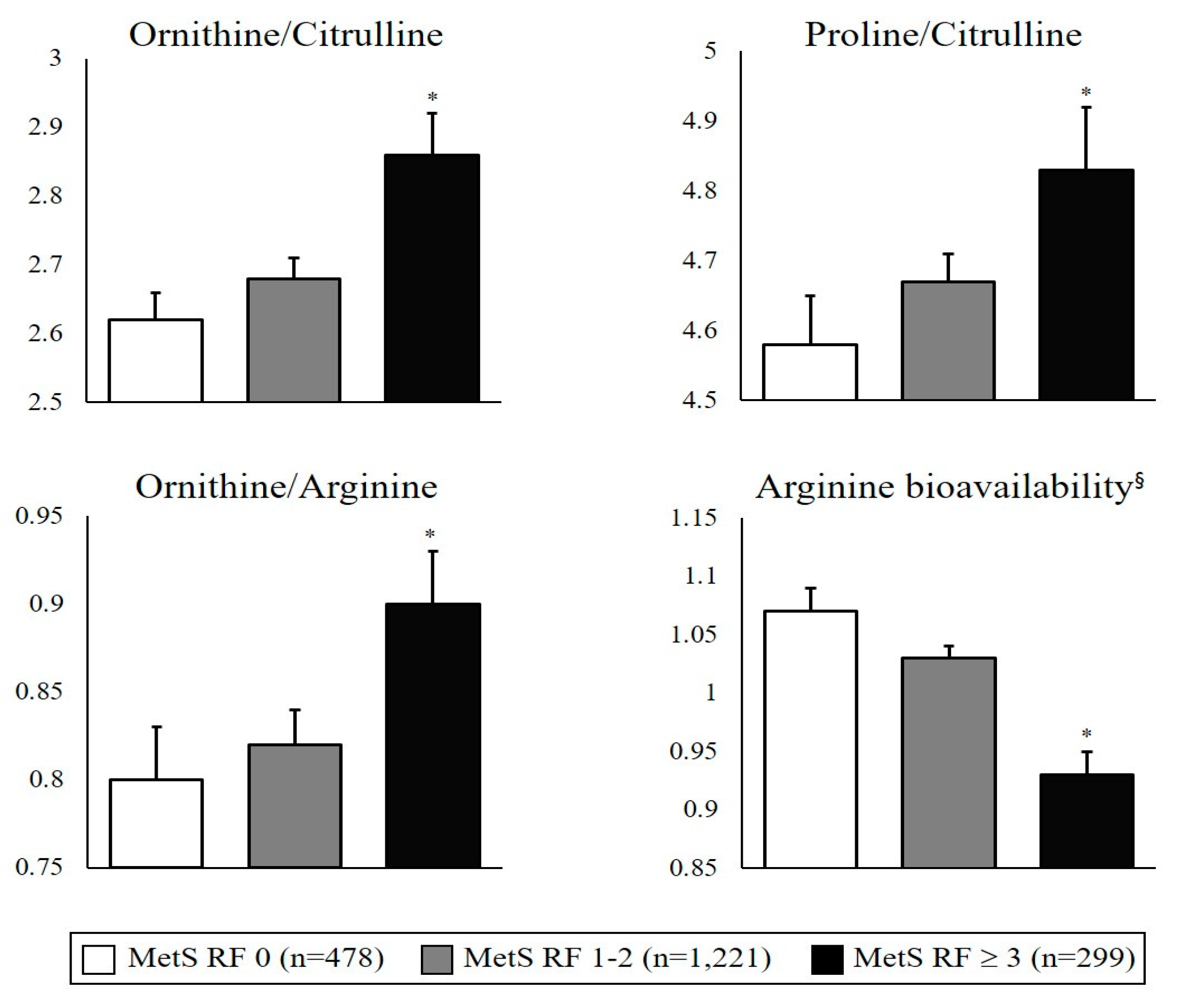
3.2. Circulating Amino Acid Metabolite Ratios Associated with Arginase and Nitric Oxide Synthase Activities According to Metabolic Syndrome Risk Status
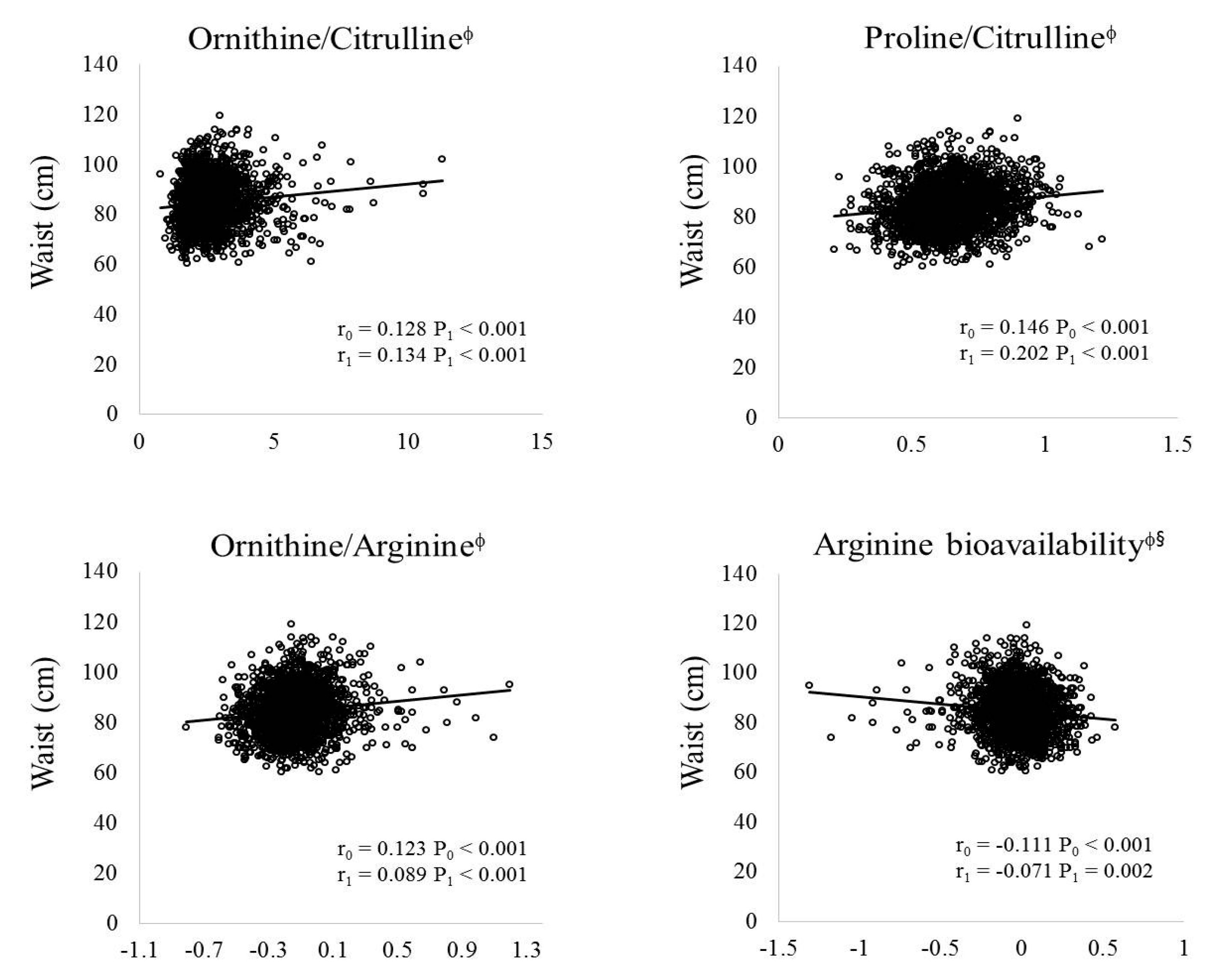
3.3. Correlations between Amino Acid Metabolites and Metabolic Syndrome Risk-Related Parameters
3.4. Association between Circulating Amino Acid Metabolite Ratios and Metabolic Syndrome Risk
4. Discussion
Acknowledgments
Author Contributions
Conflicts of Interest
References
- International Diabetes Federation (IDF). IDF Consensus Worldwide Definition of the Metabolic Syndrome; International Diabetes Federation (IDF): Brussels, Belgium, 2006. [Google Scholar]
- Hossain, P.; Kawar, B.; El Nahas, M. Obesity and diabetes in the developing world—A growing challenge. N. Engl. J. Med. 2007, 2007, 213–215. [Google Scholar] [CrossRef] [PubMed]
- Mello, M.M.; Studdert, D.M.; Brennan, T.A. Obesity—The new frontier of public health law. N. Engl. J. Med. 2006, 354, 2601–2610. [Google Scholar] [CrossRef] [PubMed]
- Kaur, J. A comprehensive review on metabolic syndrome. Cardiol. Res. Pract. 2014, 2014. [Google Scholar] [CrossRef] [PubMed]
- Lakka, H.M.; Laaksonen, D.E.; Lakka, T.A.; Niskanen, L.K.; Kumpusalo, E.; Tuomilehto, J.; Salonen, J.T. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA 2006, 288, 2709–2716. [Google Scholar] [CrossRef]
- Alberti, K.; Eckel, R.; Grundy, S.; Zimmet, P.; Cleeman, J.; Donato, K. Harmonizing the metabolic syndrome. A joint interim statement of the international diabetes federation task force on epidemiology and prevention; national heart, lung and blood institute; american heart association; world heart federation; international atherosclerosis society; and international atherosclerosis for the study of obesity. Circulation 2009, 120, 1640–1645. [Google Scholar] [PubMed]
- Williams, T. Metabolic syndrome: Nonalcoholic fatty liver disease. FP Essent. 2015, 435, 24–29. [Google Scholar] [PubMed]
- Marchesini, G.; Brizi, M.; Morselli-Labate, A.M.; Bianchi, G.; Bugianesi, E.; McCullough, A.J.; Forlani, G.; Melchionda, N. Association of nonalcoholic fatty liver disease with insulin resistance. Am. J. Med. 1999, 107, 450–455. [Google Scholar] [CrossRef]
- Marchesini, G.; Brizi, M.; Bianchi, G.; Tomassetti, S.; Bugianesi, E.; Lenzi, M.; McCullough, A.J.; Natale, S.; Forlani, G.; Melchionda, N. Nonalcoholic fatty liver disease. Diabetes 2001, 50, 1844–1850. [Google Scholar] [CrossRef] [PubMed]
- Shemyakin, A.; Kövamees, O.; Rafnsson, A.; Böhm, F.; Svenarud, P.; Settergren, M.; Jung, C.; Pernow, J. Arginase inhibition improves endothelial function in patients with coronary artery disease and type 2 diabetes mellitusclinical perspective. Circulation 2012, 126, 2943–2950. [Google Scholar] [CrossRef] [PubMed]
- Moon, J.; Do, H.J.; Cho, Y.; Shin, M.-J. Arginase inhibition ameliorates hepatic metabolic abnormalities in obese mice. PLoS ONE 2014, 9, e103048. [Google Scholar] [CrossRef] [PubMed]
- Chung, J.H.; Moon, J.; Lee, Y.S.; Chung, H.-K.; Lee, S.-M.; Shin, M.-J. Arginase inhibition restores endothelial function in diet-induced obesity. Biochem. Biophys. Res. Commun. 2014, 451, 179–183. [Google Scholar] [CrossRef] [PubMed]
- McKnight, J.R.; Satterfield, M.C.; Jobgen, W.S.; Smith, S.B.; Spencer, T.E.; Meininger, C.J.; McNeal, C.J.; Wu, G. Beneficial effects of l-arginine on reducing obesity: Potential mechanisms and important implications for human health. Amino Acids 2010, 39, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Jobgen, W.; Fu, W.J.; Gao, H.; Li, P.; Meininger, C.J.; Smith, S.B.; Spencer, T.E.; Wu, G. High fat feeding and dietary l-arginine supplementation differentially regulate gene expression in rat white adipose tissue. Amino Acids 2009, 37, 187–198. [Google Scholar] [CrossRef] [PubMed]
- Clemmensen, C.; Madsen, A.N.; Smajilovic, S.; Holst, B.; Bräuner-Osborne, H. l-Arginine improves multiple physiological parameters in mice exposed to diet-induced metabolic disturbances. Amino Acids 2012, 43, 1265–1275. [Google Scholar] [CrossRef] [PubMed]
- Jobgen, W.; Meininger, C.J.; Jobgen, S.C.; Li, P.; Lee, M.-J.; Smith, S.B.; Spencer, T.E.; Fried, S.K.; Wu, G. Dietary l-arginine supplementation reduces white fat gain and enhances skeletal muscle and brown fat masses in diet-induced obese rats. J. Nutr. 2008, 139, 230–237. [Google Scholar] [CrossRef] [PubMed]
- Fu, W.J.; Haynes, T.E.; Kohli, R.; Hu, J.; Shi, W.; Spencer, T.E.; Carroll, R.J.; Meininger, C.J.; Wu, G. Dietary l-arginine supplementation reduces fat mass in zucker diabetic fatty rats. J. Nutr. 2005, 135, 714–721. [Google Scholar] [PubMed]
- Caldwell, R.B.; Toque, H.A.; Narayanan, S.P.; Caldwell, R.W. Arginase: An old enzyme with new tricks. Trends Pharmacol. Sci. 2015, 36, 395–405. [Google Scholar] [CrossRef] [PubMed]
- Vanhoutte, P.M. Arginine and arginase. Circ. Res. 2008, 102, 923–932. [Google Scholar] [CrossRef] [PubMed]
- Pernow, J.; Jung, C. Arginase as a potential target in the treatment of cardiovascular disease: Reversal of arginine steal? Cardiovasc. Res. 2013, 98, 334–343. [Google Scholar] [CrossRef] [PubMed]
- Cho, Y.S.; Go, M.J.; Kim, Y.J.; Heo, J.Y.; Oh, J.H.; Ban, H.J.; Yoon, D.; Lee, M.H.; Kim, D.J.; Park, M.; et al. A large-scale genome-wide association study of asian populations uncovers genetic factors influencing eight quantitative traits. Nat. Genet. 2009, 41, 527–534. [Google Scholar] [CrossRef] [PubMed]
- Ainsworth, B.E.; Haskell, W.L.; Whitt, M.C.; Irwin, M.L.; Swartz, A.M.; Strath, S.J.; O’Brien, W.L.; Bassett, D.R., Jr.; Schmitz, K.H.; Emplaincourt, P.O.; et al. Compendium of physical activities: An update of activity codes and met intensities. Med. Sci. Sports Exerc. 2000, 32, S498–S504. [Google Scholar] [CrossRef] [PubMed]
- Friedewald, W.T.; Levy, R.I.; Fredrickson, D.S. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin. Chem. 1972, 18, 499–502. [Google Scholar] [PubMed]
- Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel iii). JAMA 2001, 285, 2486–2497. [Google Scholar]
- Kim, J.A.; Choi, C.J.; Yum, K.S. Cut-off values of visceral fat area and waist circumference: Diagnostic criteria for abdominal obesity in a korean population. J. Korean Med. Sci. 2006, 21, 1048–1053. [Google Scholar] [CrossRef] [PubMed]
- Zieba, R. Obesity: A review of currently used antiobesity drugs and new compounds in clinical development. Postep. Hig. Med. Doswiadczalnej 2006, 61, 612–626. [Google Scholar]
- Halford, J. Obesity drugs in clinical development. Curr. Opin. Investig. Drugs 2006, 7, 312–318. [Google Scholar] [PubMed]
- Kim, O.Y.; Lee, S.-M.; Chung, J.H.; Do, H.J.; Moon, J.; Shin, M.-J. Arginase I and the very low-density lipoprotein receptor are associated with phenotypic biomarkers for obesity. Nutrition 2012, 28, 635–639. [Google Scholar] [CrossRef] [PubMed]
- Katusic, Z.S. Mechanisms of endothelial dysfunction induced by aging. Circ. Res. 2007, 101, 640–641. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z.; Ming, X.-F. Endothelial arginase: A new target in atherosclerosis. Curr. Hypertens. Rep. 2006, 8, 54–59. [Google Scholar] [CrossRef] [PubMed]
- Bagnost, T.; Ma, L.; Da Silva, R.F.; Rezakhaniha, R.; Houdayer, C.; Stergiopulos, N.; André, C.; Guillaume, Y.; Berthelot, A.; Demougeot, C. Cardiovascular effects of arginase inhibition in spontaneously hypertensive rats with fully developed hypertension. Cardiovasc. Res. 2010, 87, 569–577. [Google Scholar] [CrossRef] [PubMed]
- Bagnost, T.; Berthelot, A.; Bouhaddi, M.; Laurant, P.; André, C.; Guillaume, Y.; Demougeot, C. Treatment with the arginase inhibitor Nω-hydroxy-nor-l-arginine improves vascular function and lowers blood pressure in adult spontaneously hypertensive rat. J. Hypertens. 2008, 26, 1110–1118. [Google Scholar] [CrossRef] [PubMed]
- Prati, C.; Berthelot, A.; Wendling, D.; Demougeot, C. Endothelial dysfunction in rat adjuvant-induced arthritis: Up-regulation of the vascular arginase pathway. Arthritis Rheum. 2011, 63, 2309–2317. [Google Scholar] [CrossRef] [PubMed]
- Prati, C.; Berthelot, A.; Kantelip, B.; Wendling, D.; Demougeot, C. Treatment with the arginase inhibitor Nw-hydroxy-nor-l-arginine restores endothelial function in rat adjuvant-induced arthritis. Arthritis Res. Ther. 2012, 14, R130. [Google Scholar] [PubMed]
- Toya, T.; Hakuno, D.; Shiraishi, Y.; Kujiraoka, T.; Adachi, T. Arginase inhibition augments nitric oxide production and facilitates left ventricular systolic function in doxorubicin-induced cardiomyopathy in mice. Physiol. Rep. 2014, 2, e12130. [Google Scholar] [CrossRef] [PubMed]
- Kovamees, O.; Shemyakin, A.; Eriksson, M.; Angelin, B.; Pernow, J. Arginase inhibition improves endothelial function in patients with familial hypercholesterolaemia irrespective of their cholesterol levels. J. Intern. Med. 2016, 279, 477–484. [Google Scholar] [CrossRef] [PubMed]
- Grönros, J.; Jung, C.; Lundberg, J.O.; Cerrato, R.; Östenson, C.-G.; Pernow, J. Arginase inhibition restores in vivo coronary microvascular function in type 2 diabetic rats. Am. J. Physiol. Heart Circ. Physiol. 2011, 300, H1174–H1181. [Google Scholar] [CrossRef] [PubMed]
- Morris, C.R.; Poljakovic, M.; Lavrisha, L.; Machado, L.; Kuypers, F.A.; Morris, S.M., Jr. Decreased arginine bioavailability and increased serum arginase activity in asthma. Am. J. Respir. Crit. Care Med. 2004, 170, 148–153. [Google Scholar] [CrossRef] [PubMed]
- El-Bassossy, H.M.; El-Fawal, R.; Fahmy, A.; Watson, M.L. Arginase inhibition alleviates hypertension in the metabolic syndrome. Br. J. Pharmacol. 2013, 169, 693–703. [Google Scholar] [CrossRef] [PubMed]
- Buga, G.M.; Singh, R.; Pervin, S.; Rogers, N.E.; Schmitz, D.A.; Jenkinson, C.P.; Cederbaum, S.D.; Ignarro, L.J. Arginase activity in endothelial cells: Inhibition by NG-hydroxy-l-arginine during high-output NO production. Am. J. Physiol. Heart Circ. Physiol. 1996, 271, H1988–H1998. [Google Scholar]
- Ryoo, S.; Lemmon, C.A.; Soucy, K.G.; Gupta, G.; White, A.R.; Nyhan, D.; Shoukas, A.; Romer, L.H.; Berkowitz, D.E. Oxidized low-density lipoprotein–dependent endothelial arginase II activation contributes to impaired nitric oxide signaling. Circ. Res. 2006, 99, 951–960. [Google Scholar] [CrossRef] [PubMed]
- Zhu, W.; Chandrasekharan, U.M.; Bandyopadhyay, S.; Morris, S.M.; DiCorleto, P.E.; Kashyap, V.S. Thrombin induces endothelial arginase through AP-1 activation. Am. J. Physiol. Cell Physiol. 2010, 298, C952–C960. [Google Scholar] [CrossRef] [PubMed]
- Hu, H.; Moon, J.; Chung, J.H.; Kim, O.Y.; Yu, R.; Shin, M.-J. Arginase inhibition ameliorates adipose tissue inflammation in mice with diet-induced obesity. Biochem. Biophys. Res. Commun. 2015, 464, 840–847. [Google Scholar] [CrossRef] [PubMed]
- Bivalacqua, T.J.; Hellstrom, W.J.; Kadowitz, P.J.; Champion, H.C. Increased expression of arginase II in human diabetic corpus cavernosum: In diabetic-associated erectile dysfunction. Biochem. Biophys. Res. Commun. 2001, 283, 923–927. [Google Scholar] [CrossRef] [PubMed]
- Romero, M.J.; Platt, D.H.; Tawfik, H.E.; Labazi, M.; El-Remessy, A.B.; Bartoli, M.; Caldwell, R.B.; Caldwell, R.W. Diabetes-induced coronary vascular dysfunction involves increased arginase activity. Circ. Res. 2008, 102, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Olivon, V.C.; Fraga-Silva, R.A.; Segers, D.; Demougeot, C.; de Oliveira, A.M.; Savergnini, S.S.; Berthelot, A.; de Crom, R.; Krams, R.; Stergiopulos, N. Arginase inhibition prevents the low shear stress-induced development of vulnerable atherosclerotic plaques in ApoE−/− mice. Atherosclerosis 2013, 227, 236–243. [Google Scholar] [CrossRef] [PubMed]
- Sansbury, B.E.; Hill, B.G. Regulation of obesity and insulin resistance by nitric oxide. Free Radic. Biol. Med. 2014, 73, 383–399. [Google Scholar] [CrossRef] [PubMed]
- Kim, F.; Pham, M.; Maloney, E.; Rizzo, N.O.; Morton, G.J.; Wisse, B.E.; Kirk, E.A.; Chait, A.; Schwartz, M.W. Vascular inflammation, insulin resistance, and reduced nitric oxide production precede the onset of peripheral insulin resistance. Arterioscler. Thromb. Vasc. Biol. 2008, 28, 1982–1988. [Google Scholar] [CrossRef] [PubMed]
- Bender, S.; Herrick, E.; Lott, N.; Klabunde, R. Diet-induced obesity and diabetes reduce coronary responses to nitric oxide due to reduced bioavailability in isolated mouse hearts. Diabetes Obes. Metab. 2007, 9, 688–696. [Google Scholar] [CrossRef] [PubMed]
- Gruber, H.; Mayer, C.; Mangge, H.; Fauler, G.; Grandits, N.; Wilders-Truschnig, M. Obesity reduces the bioavailability of nitric oxide in juveniles. Int. J. Obes. 2008, 32, 826–831. [Google Scholar] [CrossRef] [PubMed]
- Sansbury, B.E.; Cummins, T.D.; Tang, Y.; Hellmann, J.; Holden, C.R.; Harbeson, M.A.; Chen, Y.; Patel, R.P.; Spite, M.; Bhatnagar, A. Overexpression of endothelial nitric oxide synthase prevents diet-induced obesity and regulates adipocyte phenotypenovelty and significance. Circ. Res. 2012, 111, 1176–1189. [Google Scholar] [CrossRef] [PubMed]
- Jobgen, W.S.; Fried, S.K.; Fu, W.J.; Meininger, C.J.; Wu, G. Regulatory role for the arginine-nitric oxide pathway in metabolism of energy substrates. J. Nutr. Biochem. 2006, 17, 571–588. [Google Scholar] [CrossRef] [PubMed]
| Total (n = 1998) | Non-MetS (n = 1699) | MetS (n = 299) | P0 | P1 | P2 |
|---|---|---|---|---|---|
| Age (years) | 56.02 ± 0.22 | 59.92 ± 0.50 | <0.001 | - | - |
| Male (%) | 48.73 | 28.43 | <0.001 | - | - |
| Body weight (kg) φ | 61.23 ± 0.25 | 65.88 ± 0.59 | <0.001 | - | - |
| BMI (kg/m2) φ | 23.89 ± 0.07 | 26.82 ± 0.17 | <0.001 | - | - |
| Physical activity (%) | |||||
| Low | 14.83 | 11.41 | 0.292 | 0.296 | 0.454 |
| Moderate | 36.35 | 37.25 | |||
| High | 48.82 | 51.34 | |||
| Drinking status (%) | |||||
| Never | 47.00 | 55.85 | 0.018 | <0.001 | - |
| Former | 4.71 | 3.68 | |||
| Current | 48.29 | 40.47 | |||
| Smoking status (%) | |||||
| Never | 61.13 | 74.92 | <0.001 | <0.001 | - |
| Former | 18.14 | 8.70 | |||
| Current | 20.73 | 16.39 | |||
| MetS risk factors | |||||
| WC (cm) | 83.13 ± 0.21 | 93.44 ± 0.45 | <0.001 | - | <0.001 |
| TG (mg/dL) φ | 121.63 ± 1.90 | 233.57 ± 11.31 | <0.001 | <0.001 | <0.001 |
| HDLC (mg/dL) φ | 45.55 ± 0.25 | 37.85 ± 0.40 | <0.001 | <0.001 | <0.001 |
| FBG (mg/dL) φ | 89.85 ± 0.25 | 95.97 ± 0.68 | <0.001 | <0.001 | <0.001 |
| SBP (mmHg) | 114.20 ± 0.37 | 129.14 ± 0.90 | <0.001 | <0.001 | <0.001 |
| DBP (mmHg) | 74.98 ± 0.23 | 84.19 ± 0.57 | <0.001 | <0.001 | <0.001 |
| Biochemical parameters | |||||
| TC (mg/dL) | 191.08 ± 0.85 | 202.56 ± 2.24 | <0.001 | <0.001 | <0.001 |
| LDLC (mg/dL) | 121.43 ± 0.74 | 125.34 ± 2.08 | 0.054 | <0.001 | <0.001 |
| AST (IU/L) φ | 25.21 ± 0.27 | 27.74 ± 2.20 | 0.271 | <0.001 | <0.001 |
| ALT (IU/L) φ | 22.49 ± 0.41 | 24.97 ± 1.06 | 0.003 | <0.001 | <0.001 |
| Total (n = 1998) | ORN/CIT | PRO/CIT | ORN/ARG | Arginine Bioavailability § |
|---|---|---|---|---|
| TG (mg/dL) φ | 0.062 * | 0.149 | 0.027 * | −0.026 |
| HDLC (mg/dL) φ | −0.051 * | −0.056 | −0.088 * | 0.110 * |
| FBG (mg/dL) φ | 0.051 * | 0.134 | −0.002 * | 0.021 |
| SBP (mmHg) | 0.020 | 0.038 | 0.021 | −0.029 |
| DBP (mmHg) | 0.041 | 0.035 * | 0.054 | −0.051 * |
| TC (mg/dL) | 0.010 | 0.028 * | −0.048 | 0.074 * |
| LDLC (mg/dL) | −0.017 | −0.022 | −0.043 | 0.044 |
| AST (IU/L) φ | 0.114 * | −0.005 * | 0.170 | −0.107 * |
| ALT (IU/L) φ | 0.097 * | 0.079 * | 0.054 * | −0.025 |
| Total (n = 1998) | OR0 (95% CI) p-Value | OR1 (95% CI) p-Value | OR2 (95% CI) p-Value |
|---|---|---|---|
| ORN/CIT φ | 1.98 (1.39, 2.82) <0.001 | 1.75 (1.18, 2.59) 0.005 | 1.71 (1.15, 2.54) 0.008 |
| PRO/CIT φ | 1.29 (0.91, 1.85) 0.154 | 1.33 (0.88, 2.01) 0.174 | 1.30 (0.86, 1.97) 0.215 |
| ORN/ARG φ | 2.89 (1.98, 4.22) <0.001 | 2.58 (1.70, 3.90) <0.001 | 2.57 (1.69, 3.90) <0.001 |
| Arginine bioavailability φ,§ | 0.38 (0.26, 0.55) <0.001 | 0.40 (0.26, 0.60) <0.001 | 0.40 (0.26, 0.61) <0.001 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moon, J.; Kim, O.Y.; Jo, G.; Shin, M.-J. Alterations in Circulating Amino Acid Metabolite Ratio Associated with Arginase Activity Are Potential Indicators of Metabolic Syndrome: The Korean Genome and Epidemiology Study. Nutrients 2017, 9, 740. https://doi.org/10.3390/nu9070740
Moon J, Kim OY, Jo G, Shin M-J. Alterations in Circulating Amino Acid Metabolite Ratio Associated with Arginase Activity Are Potential Indicators of Metabolic Syndrome: The Korean Genome and Epidemiology Study. Nutrients. 2017; 9(7):740. https://doi.org/10.3390/nu9070740
Chicago/Turabian StyleMoon, Jiyoung, Oh Yoen Kim, Garam Jo, and Min-Jeong Shin. 2017. "Alterations in Circulating Amino Acid Metabolite Ratio Associated with Arginase Activity Are Potential Indicators of Metabolic Syndrome: The Korean Genome and Epidemiology Study" Nutrients 9, no. 7: 740. https://doi.org/10.3390/nu9070740





