Dairy Intake Enhances Body Weight and Composition Changes during Energy Restriction in 18–50-Year-Old Adults—A Meta-Analysis of Randomized Controlled Trials
Abstract
:1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Literature Search
2.3. Study Selection
2.4. Data Extraction and Quality Assessment
2.5. Rating of the Quality of the Body of Evidence
2.6. Statistical Analysis
3. Results
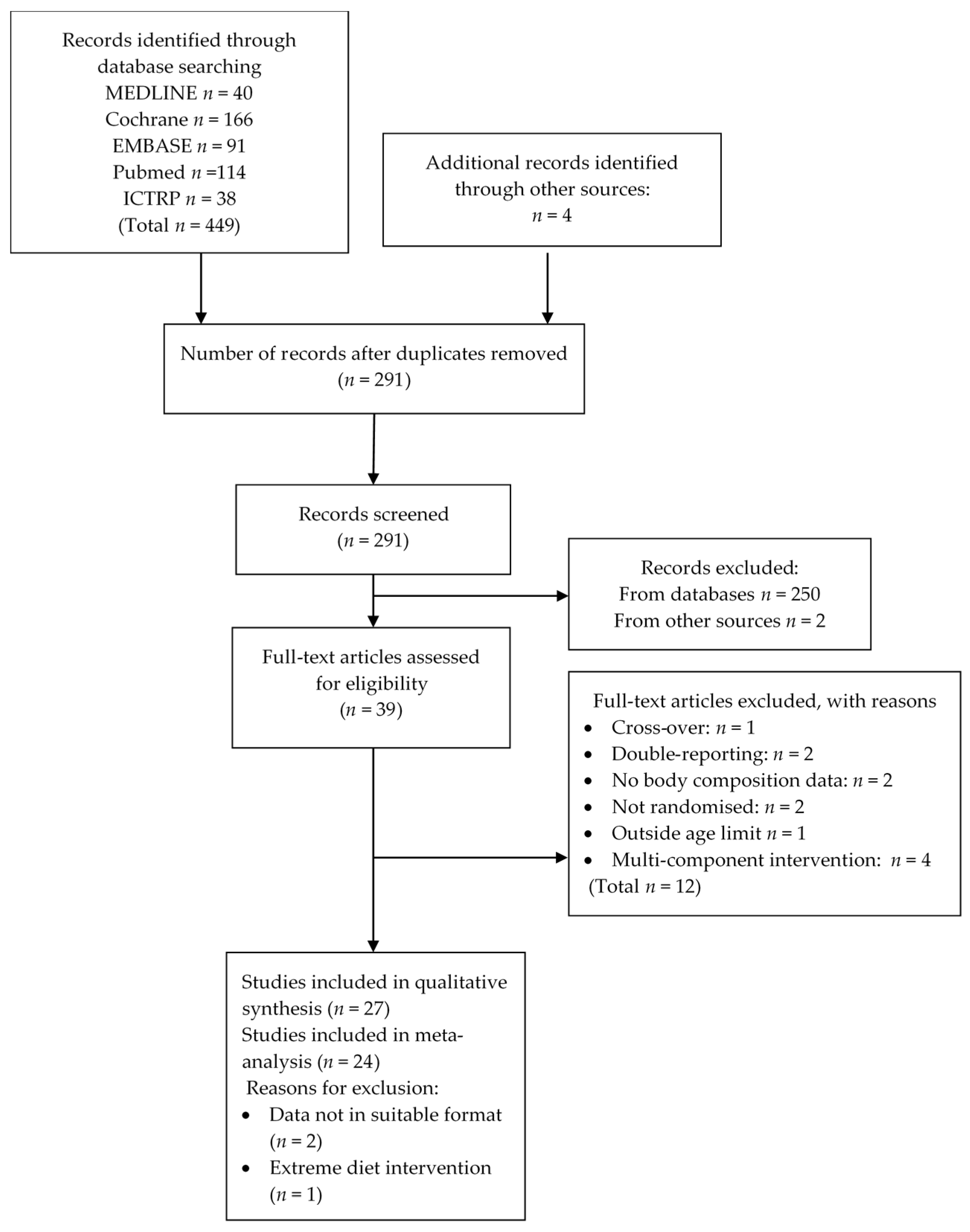
3.1. Literature Search Results
3.2. Characteristics of Included Studies
3.2.1. Geographical Location
3.2.2. Study Design
3.2.3. Study Populations
3.2.4. Interventions
3.2.5. Dietary Intakes
3.2.6. Exercise Regimes
3.2.7. Outcome Measures
3.3. Quality Assessment of Individual Studies
3.4. Effects of Dairy Intake on Body Weight and Fat Mass during Energy Restriction
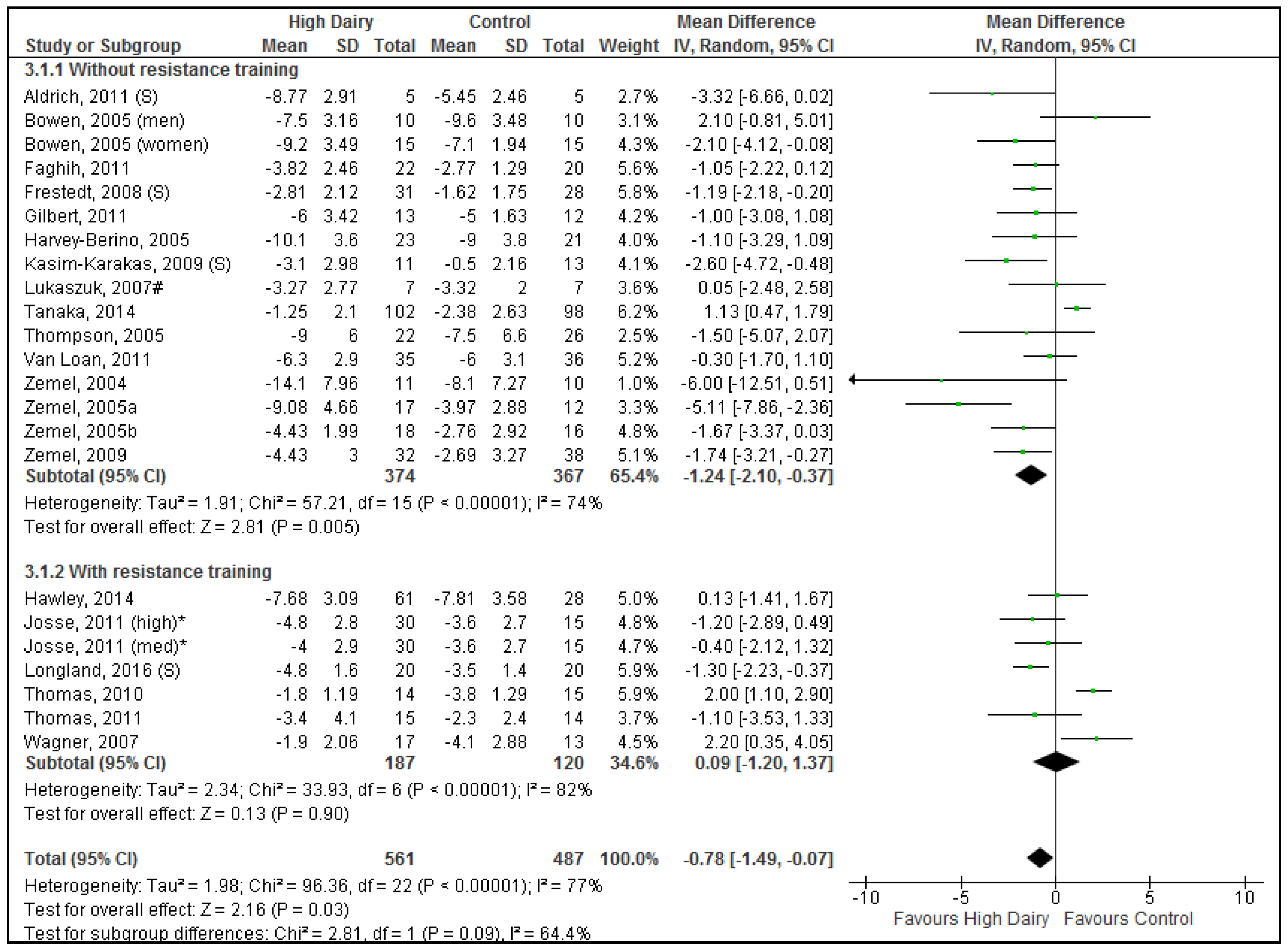
3.4.1. Energy Restriction without Resistance Training
3.4.2. Energy Restriction with Resistance Training
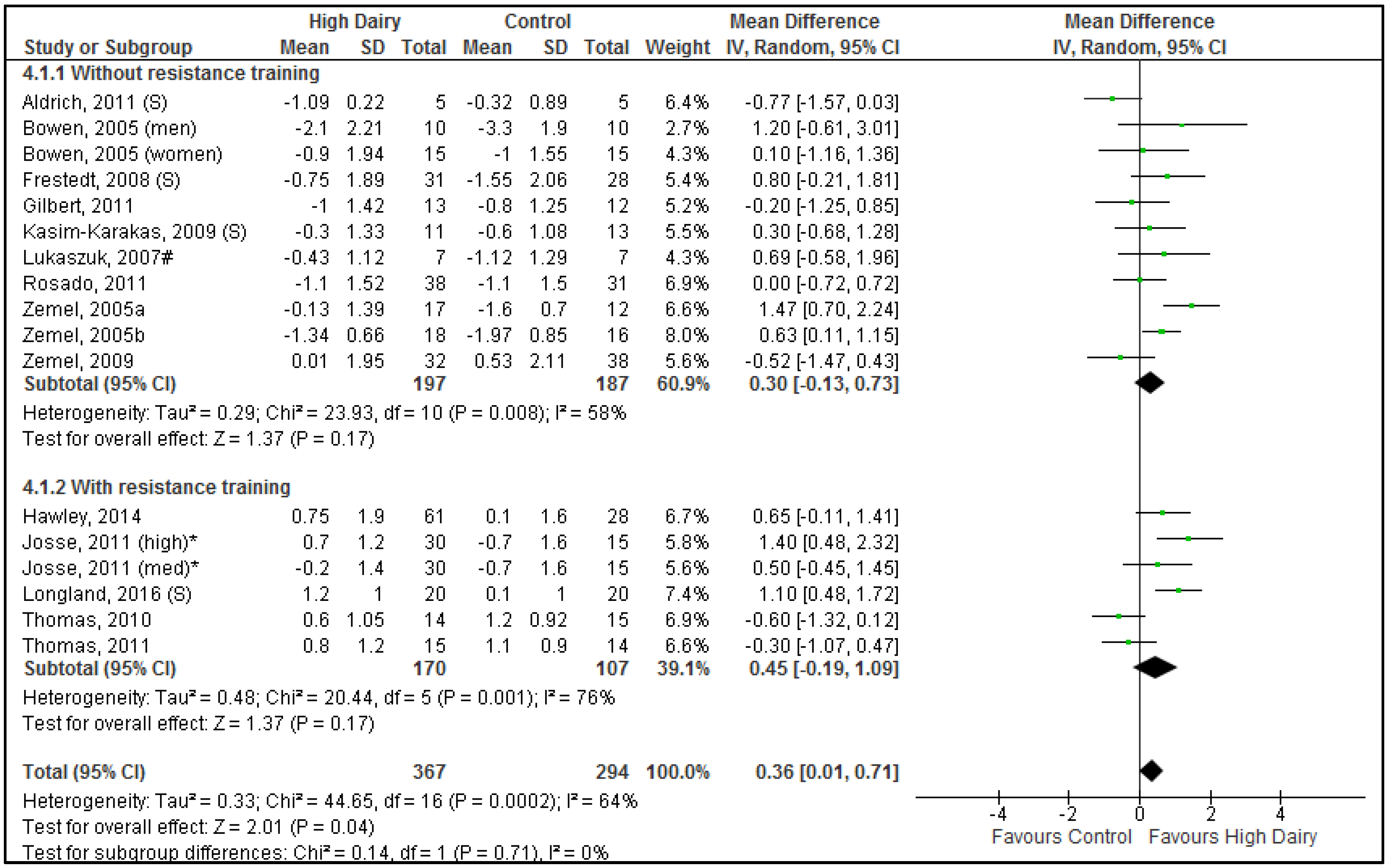
3.5. Effects of Dairy Intake on Body Lean Mass during Energy Restriction
3.6. Effects of Dairy Dose on Body Composition Outcomes
3.7. Publication Bias
3.8. Quality of the Total Body of Evidence
4. Discussion
4.1. Energy Restriction without Resistance Training on Body Weight and Fat Mass Loss
4.2. Energy Restriction with Resistance Training on Body Weight and Fat Mass Loss
4.3. Attenuation of Loss in Lean Mass
4.4. Dose
4.5. Strengths and Limitations
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| ADP | Air displacement plethysmography |
| AT | Aerobic training |
| BIA | Bioelectrical impedance analysis |
| BMI | Body mass index |
| Ca | Calcium |
| CHO | Carbohydrate |
| CI | Confidence interval |
| CLA | Conjugated linoleic acid |
| CT | Computed tomography |
| DEXA | Dual energy X-ray absorptiometry |
| % E | Percentage of total energy intake |
| ICTRP | International Clinical Trials Registry Platform Portal |
| ITT | Intention-to-treat |
| MCT | Medium-chain triacylglycerols |
| MeSH | Medical subject heading |
| MR | Meal replacement |
| MRI | Magnetic resonance imaging |
| NR | Not reported |
| PCOS | Polycystic ovary syndrome |
| RCT | Randomized controlled trial |
| RT | Resistance training |
References
- World Health Organisation. Obesity and Overweight: Fact Sheet No. 311; World Health Organisation: Geneva, Switzerland, 2015. [Google Scholar]
- Christensen, R.; Lorenzen, J.K.; Svith, C.R.; Bartels, E.M.; Melanson, E.L.; Saris, W.H.; Tremblay, A.; Astrup, A. Effect of calcium from dairy and dietary supplements on faecal fat excretion: A meta-analysis of randomized controlled trials. Obes. Rev. 2009, 10, 475–486. [Google Scholar] [CrossRef] [PubMed]
- Tang, J.E.; Moore, D.R.; Kujbida, G.W.; Tarnopolsky, M.A.; Phillips, S.M. Ingestion of whey hydrolysate, casein, or soy protein isolate: Effects on mixed muscle protein synthesis at rest and following resistance exercise in young men. J. Appl. Physiol. 2009, 107, 987–992. [Google Scholar] [CrossRef] [PubMed]
- Dougkas, A.; Reynolds, C.K.; Givens, I.D.; Elwood, P.C.; Minihane, A.M. Associations between dairy consumption and body weight: A review of the evidence and underlying mechanisms. Nutr. Res. Rev. 2011, 24, 72–95. [Google Scholar] [CrossRef] [PubMed]
- Feltrin, K.L.; Little, T.J.; Meyer, J.H.; Horowitz, M.; Smout, A.J.; Wishart, J.; Pilichiewicz, A.N.; Rades, T.; Chapman, I.M.; Feinle-Bisset, C. Effects of intraduodenal fatty acids on appetite, antropyloroduodenal motility, and plasma CCK and GLP-1 in humans vary with their chain length. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2004, 287, R524–R533. [Google Scholar] [CrossRef] [PubMed]
- Louie, J.C.; Flood, V.M.; Hector, D.J.; Rangan, A.M.; Gill, T.P. Dairy consumption and overweight and obesity: A systematic review of prospective cohort studies. Obes. Rev. 2011, 12, e582–e592. [Google Scholar] [CrossRef] [PubMed]
- Krieger, J.W.; Sitren, H.S.; Daniels, M.J.; Langkamp-Henken, B. Effects of variation in protein and carbohydrate intake on body mass and composition during energy restriction: A meta-regression. Am. J. Clin. Nutr. 2006, 83, 260–274. [Google Scholar] [PubMed]
- Wycherley, T.P.; Moran, L.J.; Clifton, P.M.; Noakes, M.; Brinkworth, G.D. Effects of energy-restricted high-protein, low-fat compared with standard-protein, low-fat diets: A meta-analysis of randomized controlled trials. Am. J. Clin. Nutr. 2012, 96, 1281–1298. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.; Pan, A.; Malik, V.S.; Hu, F.B. Effects of dairy intake on body weight and fat: A meta-analysis of randomized controlled trials. Am. J. Clin. Nutr. 2012, 96, 735–747. [Google Scholar] [CrossRef] [PubMed]
- Abargouei, A.S.; Janghorbani, M.; Salehi-Marzijarani, M.; Esmaillzadeh, A. Effect of dairy consumption on weight and body composition in adults: A systematic review and meta-analysis of randomized controlled clinical trials. Int. J. Obes. 2012, 36, 1485–1493. [Google Scholar] [CrossRef] [PubMed]
- NHMRC. A Modelling System to Inform the Revision of the Australian Guide to Healthy Eating; Commonwealth of Australia: Canberra, Australia, 2011. [Google Scholar]
- Josse, A.R.; Atkinson, S.A.; Tarnopolsky, M.A.; Phillips, S.M. Increased consumption of dairy foods and protein during diet- and exercise-induced weight loss promotes fat mass loss and lean mass gain in overweight and obese premenopausal women. J. Nutr. 2011, 141, 1626–1634. [Google Scholar] [CrossRef] [PubMed]
- Health Canada. Guidance Document for Preparing a Submission for Food Health Claims; Bureau of Nutritional Sciences Food Directorate, Health Products and Food Branch Health Canada: Ottawa, ON, Canada, 2009. [Google Scholar]
- Balshem, H.; Helfand, M.; Schunemann, H.J.; Oxman, A.D.; Kunz, R.; Brozek, J.; Vist, G.E.; Falck-Ytter, Y.; Meerpohl, J.; Norris, S.; et al. GRADE guidelines: 3. Rating the quality of evidence. J. Clin. Epidemiol. 2011, 64, 401–406. [Google Scholar] [CrossRef] [PubMed]
- Guyatt, G.H.; Oxman, A.D.; Kunz, R.; Brozek, J.; Alonso-Coello, P.; Rind, D.; Devereaux, P.J.; Montori, V.M.; Freyschuss, B.; Vist, G.; et al. GRADE guidelines 6. Rating the quality of evidence—Imprecision. J. Clin. Epidemiol. 2011, 64, 1283–1293. [Google Scholar] [CrossRef] [PubMed]
- Guyatt, G.H.; Oxman, A.D.; Kunz, R.; Woodcock, J.; Brozek, J.; Helfand, M.; Alonso-Coello, P.; Falck-Ytter, Y.; Jaeschke, R.; Vist, G.; et al. GRADE guidelines: 8. Rating the quality of evidence—Indirectness. J. Clin. Epidemiol. 2011, 64, 1303–1310. [Google Scholar] [CrossRef] [PubMed]
- Guyatt, G.H.; Oxman, A.D.; Kunz, R.; Woodcock, J.; Brozek, J.; Helfand, M.; Alonso-Coello, P.; Glasziou, P.; Jaeschke, R.; Akl, E.A.; et al. GRADE guidelines: 7. Rating the quality of evidence—Inconsistency. J. Clin. Epidemiol. 2011, 64, 1294–1302. [Google Scholar] [CrossRef] [PubMed]
- Guyatt, G.H.; Oxman, A.D.; Vist, G.; Kunz, R.; Brozek, J.; Alonso-Coello, P.; Montori, V.; Akl, E.A.; Djulbegovic, B.; Falck-Ytter, Y.; et al. GRADE guidelines: 4. Rating the quality of evidence—Study limitations (risk of bias). J. Clin. Epidemiol. 2011, 64, 407–415. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions. Available online: http://training.cochrane.org/handbook (accessed on 1 June 2014).
- Gilbert, J.A.; Joanisse, D.R.; Chaput, J.P.; Miegueu, P.; Cianflone, K.; Almeras, N.; Tremblay, A. Milk supplementation facilitates appetite control in obese women during weight loss: A randomised, single-blind, placebo-controlled trial. Br. J. Nutr. 2011, 105, 133–143. [Google Scholar] [CrossRef] [PubMed]
- Piccolo, B.D.; Comerford, K.B.; Karakas, S.E.; Knotts, T.A.; Fiehn, O.; Adams, S.H. Whey protein supplementation does not alter plasma branched-chained amino acid profiles but results in unique metabolomics patterns in obese women enrolled in an 8-week weight loss trial. J. Nutr. 2015, 145, 691–700. [Google Scholar] [CrossRef] [PubMed]
- Thomas, D.T.; Wideman, L.; Lovelady, C.A. Effects of calcium and resistance exercise on body composition in overweight premenopausal women. J. Am. Coll. Nutr. 2010, 29, 604–611. [Google Scholar] [CrossRef] [PubMed]
- Anderson, J.W.; Fuller, J.; Patterson, K.; Blair, R.; Tabor, A. Soy compared to casein meal replacement shakes with energy-restricted diets for obese women: Randomized controlled trial. Metabolism 2007, 56, 280–288. [Google Scholar] [CrossRef] [PubMed]
- Anderson, J.W.; Hoie, L.H. Weight loss and lipid changes with low-energy diets: Comparator study of milk-based versus soy-based liquid meal replacement interventions. J. Am. Coll. Nutr. 2005, 24, 210–216. [Google Scholar] [CrossRef] [PubMed]
- Harbord, R.M.; Higgins, J.P.T. Meta-regression in Stata. Stata J. 2008, 8, 493–519. [Google Scholar]
- Buchowski, M.S.; Aslam, M.; Dossett, C.; Dorminy, C.; Choi, L.; Acra, S. Effect of dairy and non-dairy calcium on fecal fat excretion in lactose digester and maldigester obese adults. Int. J. Obes. (Lond.) 2010, 34, 127–135. [Google Scholar] [CrossRef] [PubMed]
- Bowen, J.; Noakes, M.; Clifton, P.M. A high dairy protein, high-calcium diet minimizes bone turnover in overweight adults during weight loss. J. Nutr. 2004, 134, 568–573. [Google Scholar] [PubMed]
- Smilowitz, J.T.; Wiest, M.M.; Teegarden, D.; Zemel, M.B.; German, J.B.; Loan, M.D. Dietary fat and not calcium supplementation or dairy product consumption is associated with changes in anthropometrics during a randomized, placebo-controlled energy-restriction trial. Nutr. Metab. 2014, 8, 67. [Google Scholar] [CrossRef] [PubMed]
- Buonopane, G.J.; Kilara, A.; Smith, J.S.; McCarthy, R.D. Effect of skim milk supplementation on blood cholesterol concentration, blood pressure, and triglycerides in a free-living human population. J. Am. Coll. Nutr. 1992, 11, 56–67. [Google Scholar] [CrossRef] [PubMed]
- Zheng, H.; Lorenzen, J.K.; Astrup, A.; Larsen, L.H.; Yde, C.C.; Clausen, M.R.; Bertram, H.C. Metabolic effects of a 24-week energy-restricted intervention combined with low or high dairy intake in overweightwomen: An NMR-based metabolomics investigation. Nutrients 2016, 8, 108. [Google Scholar] [CrossRef] [PubMed]
- Bosello, O.; Cominacini, L.; Zocca, I.; Garbin, U.; Compri, R.; Davoli, A.; Brunetti, L. Short- and long-term effects of hypocaloric diets containing proteins of different sources on plasma lipids and apoproteins of obese subjects. Ann. Nutr. Metab. 1988, 32, 206–214. [Google Scholar] [CrossRef] [PubMed]
- Rossi, F.; Alberto, B.; Jessica, C.; Simona, B. Diets containing dairy foods positively affects weight and fat loss and cytokines blood levels in premenopausal obese women. Mediterr. J. Nutr. Metab. 2015, 8, 165–174. [Google Scholar] [CrossRef]
- Ping-Delfos, W.C.S. Effects of Dairy Products and Resistacne Exercise on Energy Balance; Curtin University of Technology: Perth, Australia, 2009. [Google Scholar]
- Berg, A.; Frey, I.; Deibert, P.; Landmann, U.; Konig, D.; Schmidt-Trucksass, A.; Ruecker, G.; Kreiter, H.; Berg, A.; Dickhuth, H.-H.; et al. Weight reduction is feasible—Preliminary results of a controlled, randomised intervention study in overweight adults. Ernahrungs Umschau 2003, 50, 386–393. [Google Scholar]
- Demling, R.H.; DeSanti, L. Effect of a hypocaloric diet, increased protein intake and resistance training on lean mass gains and fat mass loss in overweight police officers. Ann. Nutr. Metab. 2000, 44, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Jones, K.W.; Eller, L.K.; Parnell, J.A.; Doyle-Baker, P.K.; Edwards, A.L.; Reimer, R.A. Effect of a dairy- and calcium-rich diet on weight loss and appetite during energy restriction in overweight and obese adults: A randomized trial. Eur. J. Clin. Nutr. 2013, 67, 371–376. [Google Scholar] [CrossRef] [PubMed]
- Zarrati, M.; Salehi, E.; Nourijelyani, K.; Mofid, V.; Zadeh, M.J.; Najafi, F.; Ghaflati, Z.; Bidad, K.; Chamari, M.; Karimi, M.; et al. Effects of probiotic yogurt on fat distribution and gene expression of proinflammatory factors in peripheral blood mononuclear cells in overweight and obese people with or without weight-loss diet. J. Am. Coll. Nutr. 2014, 33, 417–425. [Google Scholar] [CrossRef] [PubMed]
- Summerbell, C.D.; Watts, C.; Higgins, J.P.T.; Garrow, J.S. Randomised controlled trial of novel, simple, and well supervised weight reducing diets in outpatients. Br. Med. J. 1998, 317, 1487–1489. [Google Scholar] [CrossRef]
- Harvey-Berino, J.; Gold, B.C.; Lauber, R.; Starinski, A. The impact of calcium and dairy product consumption on weight loss. Obes. Res. 2005, 13, 1720–1726. [Google Scholar] [CrossRef] [PubMed]
- Thompson, W.G.; Rostad Holdman, N.; Janzow, D.J.; Slezak, J.M.; Morris, K.L.; Zemel, M.B. Effect of energy-reduced diets high in dairy products and fiber on weight loss in obese adults. Obes. Res. 2005, 13, 1344–1353. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, S.; Uenishi, K.; Ishida, H.; Takami, Y.; Hosoi, T.; Kadowaki, T.; Orimo, H.; Ohashi, Y. A randomized intervention trial of 24-week dairy consumption on waist circumference, blood pressure, and fasting blood sugar and lipids in Japanese men with metabolic syndrome. J. Nutr. Sci. Vitaminol. (Tokyo) 2014, 60, 305–312. [Google Scholar] [CrossRef] [PubMed]
- Longland, T.M.; Oikawa, S.Y.; Mitchell, C.J.; Devries, M.C.; Phillips, S.M. Higher compared with lower dietary protein during an energy deficit combined with intense exercise promotes greater lean mass gain and fat mass loss: A randomized trial. Am. J. Clin. Nutr. 2016, 103, 738–746. [Google Scholar] [CrossRef] [PubMed]
- Bowen, J.; Noakes, M.; Clifton, P.M. Effect of calcium and dairy foods in high protein, energy-restricted diets on weight loss and metabolic parameters in overweight adults. Int. J. Obes. (Lond.) 2005, 29, 957–965. [Google Scholar] [CrossRef] [PubMed]
- Thomas, D.T.; Wideman, L.; Lovelady, C.A. Effects of a dairy supplement and resistance training on lean mass and insulin-like growth factor in women. Int. J. Sport Nutr. Exerc. Metab. 2011, 21, 181–188. [Google Scholar] [PubMed]
- Lukaszuk, J.M.; Luebbers, P.; Gordon, B.A. Preliminary study: Soy milk as effective as skim milk in promoting weight loss. J. Am. Diet. Assoc. 2007, 107, 1811–1814. [Google Scholar] [CrossRef] [PubMed]
- Zemel, M.B.; Richards, J.; Mathis, S.; Milstead, A.; Gebhardt, L.; Silva, E. Dairy augmentation of total and central fat loss in obese subjects. Int. J. Obes. (Lond.) 2005, 29, 391–397. [Google Scholar] [CrossRef] [PubMed]
- Frestedt, J.L.; Zenk, J.L.; Kuskowski, M.A.; Ward, L.S.; Bastian, E.D. A whey-protein supplement increases fat loss and spares lean muscle in obese subjects: A randomized human clinical study. Nutr. Metab. 2008, 5, 8. [Google Scholar] [CrossRef] [PubMed]
- Aldrich, N.D.; Reicks, M.M.; Sibley, S.D.; Redmon, J.B.; Thomas, W.; Raatz, S.K. Varying protein source and quantity do not significantly improve weight loss, fat loss, or satiety in reduced energy diets among midlife adults. Nutr. Res. 2011, 31, 104–112. [Google Scholar] [CrossRef] [PubMed]
- Kasim-Karakas, S.E.; Almario, R.U.; Cunningham, W. Effects of protein versus simple sugar intake on weight loss in polycystic ovary syndrome (according to the National Institutes of Health criteria). Fertil. Steril. 2009, 92, 262–270. [Google Scholar] [CrossRef] [PubMed]
- Hawley, J.A. Effect of Dairy-Based High Protein, Variable-Carbohydrate Diets and Exercise on Muscle Maintenance and Movement; Dairy Health Nutrition Consortium: Werribee, Australia, 2014. [Google Scholar]
- Rosado, J.L.; Garcia, O.P.; Ronquillo, D.; Hervert-Hernandez, D.; Caamano, M.D.C.; Martinez, G.; Gutiérrez, J.; García, S. Intake of milk with added micronutrients increases the effectiveness of an energy-restricted diet to reduce body weight: A randomized controlled clinical trial in Mexican women. J. Am. Diet. Assoc. 2011, 111, 1507–1516. [Google Scholar] [CrossRef] [PubMed]
- Van Loan, M.D.; Keim, N.L.; Adams, S.H.; Souza, E.; Woodhouse, L.R.; Thomas, A.; Witbracht, M.; Gertz, E.R.; Piccolo, B.; Bremer, A.A.; et al. Dairy foods in a moderate energy restricted diet do not enhance central fat, weight, and intra-abdominal adipose tissue losses nor reduce adipocyte size or inflammatory markers in overweight and obese adults: A controlled feeding study. J. Obes. 2011, 2011, 989657. [Google Scholar] [CrossRef] [PubMed]
- Wagner, G.; Kindrick, S.; Hertzler, S.; DiSilvestro, R.A. Effects of various forms of calcium on body weight and bone turnover markers in women participating in a weight loss program. J. Am. Coll. Nutr. 2007, 26, 456–461. [Google Scholar] [CrossRef] [PubMed]
- Zemel, M.B.; Teegarden, D.; Loan, M.V.; Schoeller, D.A.; Matkovic, V.; Lyle, R.M.; Craig, B.A. Dairy-rich diets augment fat loss on an energy-restricted diet: A multicenter trial. Nutrients 2009, 1, 83–100. [Google Scholar] [CrossRef] [PubMed]
- Faghih, S.; Abadi, A.R.; Hedayati, M.; Kimiagar, S.M. Comparison of the effects of cows’ milk, fortified soy milk, and calcium supplement on weight and fat loss in premenopausal overweight and obese women. Nutr. Metab. Cardiovasc. Dis. 2011, 21, 499–503. [Google Scholar] [CrossRef] [PubMed]
- Zemel, M.B.; Richards, J.; Milstead, A.; Campbell, P. Effects of calcium and dairy on body composition and weight loss in African-American adults. Obes. Res. 2005, 13, 1218–1225. [Google Scholar] [CrossRef] [PubMed]
- Torres, M.R.; Francischetti, E.A.; Genelhu, V.; Sanjuliani, A.F. Effect of a high-calcium energy-reduced diet on abdominal obesity and cardiometabolic risk factors in obese Brazilian subjects. Int. J. Clin. Pract. 2010, 64, 1076–1083. [Google Scholar] [CrossRef] [PubMed]
- Zemel, M.B.; Thompson, W.; Milstead, A.; Morris, K.; Campbell, P. Calcium and dairy acceleration of weight and fat loss during energy restriction in obese adults. Obes. Res. 2004, 12, 582–590. [Google Scholar] [CrossRef] [PubMed]
- Berger, P.K.; Principe, J.L.; Laing, E.M.; Henley, E.C.; Pollock, N.K.; Taylor, R.G.; Blair, R.M.; Baile, C.A.; Hall, D.B.; Lewis, R.D. Weight gain in college females is not prevented by isoflavone-rich soy protein: A randomized controlled trial. Nutr. Res. 2014, 34, 66–73. [Google Scholar] [CrossRef] [PubMed]
- EFSA Panel on Dietetic Products Nutrition and Allergies (NDA). Guidance on the scientific requirements for health claims related to appetite ratings, weight management, and blood glucose concentrations. EFSA J. 2012, 10, 2604. [Google Scholar]
- O’Sullivan, T.A.; Bremner, A.P.; Bremer, H.K.; Seares, M.E.; Beilin, L.J.; Mori, T.A.; Lyons-Wall, P.; Devine, A.; Oddy, W.H. Dairy product consumption, dietary nutrient and energy density and associations with obesity in Australian adolescents. J. Hum. Nutr. Diet. 2015, 28, 452–464. [Google Scholar] [CrossRef] [PubMed]
- Hamman, R.F.; Wing, R.R.; Edelstein, S.L.; Lachin, J.M.; Bray, G.A.; Delahanty, L.; Hoskin, M.; Kriska, A.M.; Mayer-Davis, E.J.; Pi-Sunyer, X.; et al. Effect of weight loss with lifestyle intervention on risk of diabetes. Diabetes Care 2006, 29, 2102–2107. [Google Scholar] [CrossRef] [PubMed]
- Onakpoya, I.J.; Perry, R.; Zhang, J.; Ernst, E. Efficacy of calcium supplementation for management of overweight and obesity: Systematic review of randomized clinical trials. Nutr. Rev. 2011, 69, 335–343. [Google Scholar] [CrossRef] [PubMed]
- Evans, E.M.; Mojtahedi, M.C.; Thorpe, M.P.; Valentine, R.J.; Kris-Etherton, P.M.; Layman, D.K. Effects of protein intake and gender on body composition changes: A randomized clinical weight loss trial. Nutr. Metab. (Lond.) 2012, 9, 55. [Google Scholar] [CrossRef] [PubMed]
- Fine, E.J.; Feinman, R.D. Thermodynamics of weight loss diets. Nutr. Metab. (Lond.) 2004, 1, 15. [Google Scholar] [CrossRef] [PubMed]
- Halton, T.L.; Hu, F.B. The effects of high protein diets on thermogenesis, satiety and weight loss: A critical review. J. Am. Coll. Nutr. 2004, 23, 373–385. [Google Scholar] [CrossRef] [PubMed]
- St-Onge, M.P.; Jones, P.J. Physiological effects of medium-chain triglycerides: Potential agents in the prevention of obesity. J. Nutr. 2002, 132, 329–332. [Google Scholar] [PubMed]
- Mumme, K.; Stonehouse, W. Effects of medium-chain triglycerides on weight loss and body composition: A meta-analysis of randomized controlled trials. J. Acad. Nutr. Diet. 2015, 115, 249–263. [Google Scholar] [CrossRef] [PubMed]
- Onakpoya, I.J.; Posadzki, P.P.; Watson, L.K.; Davies, L.A.; Ernst, E. The efficacy of long-term conjugated linoleic acid (CLA) supplementation on body composition in overweight and obese individuals: A systematic review and meta-analysis of randomized clinical trials. Eur. J. Nutr. 2012, 51, 127–134. [Google Scholar] [CrossRef] [PubMed]
- USDA. USDA National Nutrient Database for Standard Reference, Release 26. 2011. Available online: http://ndb.nal.usda.gov/ (accessed on 1 October 2014). [Google Scholar]
- Norton, L.E.; Layman, D.K. Leucine regulates translation initiation of protein synthesis in skeletal muscle after exercise. J. Nutr. 2006, 136, 533S–537S. [Google Scholar] [PubMed]
- Hector, A.J.; Marcotte, G.R.; Churchward-Venne, T.A.; Murphy, C.H.; Breen, L.; von Allmen, M.; Baker, S.K.; Phillips, S.M. Whey protein supplementation preserves postprandial myofibrillar protein synthesis during short-term energy restriction in overweight and obese adults. J. Nutr. 2015, 145, 246–252. [Google Scholar] [CrossRef] [PubMed]
- Tang, J.E.; Manolakos, J.J.; Kujbida, G.W.; Lysecki, P.J.; Moore, D.R.; Phillips, S.M. Minimal whey protein with carbohydrate stimulates muscle protein synthesis following resistance exercise in trained young men. Appl. Physiol. Nutr. Metab. 2007, 32, 1132–1138. [Google Scholar] [CrossRef] [PubMed]

| Reference 2 (Country) | Quality Score 3 | Population | Intervention | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N 4 | Age (Year) | Description (BMI) 5 | Female (%) | Dairy | Control | Estimated Dose Difference 6,7 | Calorie Restriction | Iso-Caloric 8 | Exercise 9 | Duration (Weeks) | Outcomes Assessed | ||
| Dairy Food Studies | |||||||||||||
| Anderson, 2005 [24] (USA) | 11 | 90 (52) | 18–65 | Overweight/obese BMI = 27–40 | 88 | 2× milk-based meal replacement (Slim-Fast®)/day | 5× soy-based meal replacements (Scan-Diet™)/day | 2 servings | Diets = 5020 kJ | Yes | No | 12 | BW 10 |
| Bowen, 2005 [43] (Australia) | 8 | (50) | 20–65 | Overweight/obese BMI = 27–40 | 60 | 4.5 serves dairy/day (skim milk, reduced fat cheese, yoghurt, skim milk powder) | 0.5 serves dairy/day | 4 servings | Caloric restriction (12 weeks): Diet = 5500–7000 kJ Eucaloric (4 weeks) | Yes | No | 16 | BW, FM, LM |
| Faghih, 2011 [55] (Iran) | 7 | 50 (42) | 20–50 | Healthy pre-menopausal overweight/obese women BMI = 25–40 | 100 | 3× 220 mL low-fat milk/day | Control diet providing 500 mg/day dietary Ca | 2.64 servings | −2092 kJ | Yes | No | 8 | BW, FM |
| Gilbert, 2011 [20] (USA) | 10 | 41 (25) | 25–50 | Healthy overweight/obese low Ca consumers (<800 mg/day) BMI = 27–42 | 100 | 1 serving (568 mL providing 1000 mg Ca) milk supplement/day (Lactancia Addition Nature 35% plus de Ca (1% fat); Parmalat Canada, Toronto, ON, Canada) | 1 serving (463 mL) Placebo (Rice Dream; Hain Celestial Canada, Toronto, ON, Canada) | 2.3 servings | −2508 kJ | Yes | No | 24 | BW, FM, FFM |
| Harvey-Berino, 2005 [39] (USA) | 9 | 55 (44) | 18–60 | Overweight/obese adults with low dairy (<1 serve/day) and Ca (<500 mg/day) intake. Baseline dairy intake ~1.4 servings/day BMI = 25–34.9 | 91 | 3–4 (3.2 ± 1.1) servings dairy/day (milk, yogurt, cheese) providing 1200–1400 mg Ca/day | 1 (0.85 ± 0.4) serving dairy/day providing 400–500 mg Ca/day. | 2.7 servings | −2092 kJ | Yes | No | 52 | BW, FM |
| Hawley, 2014 [50] (Australia) | 9 | 111 (89) | 35–59 | Health overweight/obese sedentary low dairy consumers (1.3 serves/day) BMI = 27–40 | 71 | 4 + (3.8 ± 0.7) serves dairy/day | 1–2 (1.0 ± 0.3) serves dairy/day | 2.8 servings | −1046 kJ | Yes | RT: 3×/week AT: 4×/week | 16 | BW, FM, LM |
| Josse, 2011 [12] (Canada) | 13 | 90 (78) | 19-45 | Pre-menopausal overweight/obese low dairy consumers BMI = 27–40 | 100 | High dairy: 6–7 servings dairy/day (milk, cheese, yoghurt) | Low diary: 0–1 servings dairy/day | 6 servings | −2092 kJ | Yes | RT: 2×/week + AT: 7×/week | 16 | BW, FM, LM |
| Medium dairy: 3–4 servings dairy/day (milk, cheese, yoghurt) | 3 servings | ||||||||||||
| Lukaszuk, 2007 [45] (USA) | 10 | 18 (14) | 18–45 | Healthy pre-menopausal overweight/obese low Ca consumers (<600 mg/day) BMI = ~36 | 100 | 3 cups/day (720 mL) skim milk | 3 cups/day (720 mL) light soy milk + added soy protein to equate protein of milk | 3 servings | −2092 kJ | Yes | No | 8 | BW, FM, FFM |
| Rosado, 2011 [51] (Mexico) | 11 | 93 (69) | 25–45 | Obese low dairy consumers (<3 servings/day) BMI ≥ 30 | 100 | 3 servings milk/day. No other dairy. | 0 servings of dairy/day. | 3 servings | −2092 kJ | Yes | No | 16 | BW, FM 10, LM |
| Summerbell, 1998 [38] (UK) | 13 | 28 (20) | >17 | Healthy overweight/obese BMI ≥ 27 | 79 | Milk (full-cream/skim) to provide 3.4 MJ (nil other food) | Conventional balanced diet providing 3.4 MJ/day | 7.3 servings | Diet = 3.4 MJ | Yes | No | 16 | BW |
| Tanaka, 2014 [41] (Japan) | 12 | 213 (200) | 20–60 | ≥2 components of metabolic syndrome BMI = average ~27 | 0 | 400 g dairy/day (milk, yoghurt) | Low dairy: <0.5 servings dairy/day | 1.3 servings | −1255 kJ | Yes | No | 24 | BW, FM |
| Thomas, 2010 [22] (USA) | 12 | 35 (29) | 29–45 | Overweight/obese low dairy consumers (≤1 serving/day) BMI = 25–30 | 100 | ≥3 servings dairy/day providing 1200 mg Ca/day | ≤1 serving dairy/day providing 500 mg Ca/day | 3 servings | −1046 kJ | Yes | RT: 3×/week | 16 | BW, FM, FFM |
| Thomas, 2011 [44] (USA) | 10 | 35 (29) | 29–45 | Overweight, non-RT BMI = 25–30 | 100 | 2× 170 g fat free yoghurt 3×/week—20 min before exercise and immediately after exercise | 2× sucrose beverage 3×/week—20 min before exercise and immediately after exercise | 0.75 servings | −1046 kJ | Yes | RT: 3×/week | 16 | BW, FM, LM |
| Thompson, 2005 [40] (USA) | 13 | 59 (48) (adherers: 36) | 25–70 | Obese adults BMI = 30–40 | 86 | 4 servings (3.13 achieved) dairy/day (2 as fluid milk) | 2 servings (1.38 achieved) dairy/day | 1.8 servings | −2092 kJ | Yes | AT: 30 min 4×/week | 48 | BW, FM |
| Torres, 2010 [57] (Brazil) | 11 | 50 (39) | 22–55 | Obese low Ca consumers (<500 mg/day) of multi-ethnic origin BMI = 30–34.9 | 90 | 60 g/day (2 servings) of non-fat powdered milk (1200–1300 mg Ca/day) | Low-Ca diet (<500 mg Ca/day) | 2 servings | −3347 kJ | Yes | No | 16 | BW |
| Van Loan, 2011 [52] (USA) | 7 | 78 (71) | 19–50 | Overweight/obese low dairy consumers (≤1 serving dairy/day) BMI = 28–37 | 77 | 3–4 servings dairy/day (milk, yogurt, cheese) providing 1339 mg Ca/day | ≤1 serving dairy/day providing 460 mg Ca/day | 3 servings | −2092 kJ | Yes | No | 15 | BW, FM, LM 10 |
| Wagner, 2007 [53] (USA) | 9 | ~42 (30) | 19–53 | Pre-menopausal overweight BMI = 26–40 | 100 | Low-fat milk providing 800 mg calcium/day | Placebo capsules (cellulose) | 2.7 servings | −2092 kJ | Yes | RT + AT: 3×/week | 12 | BW, FM |
| Zemel, 2004 [58] (USA) | 8 | 28 (21) | 18–60 | Healthy overweight/obese BMI = 30–39.9 | 81 | 3 serves of dairy providing 1200–1300 mg Ca/day + placebo | <1 serve of dairy providing 400–500 mg of Ca/day + placebo (content NR) | 2.5 servings | −2092 kJ | Yes | No | 24 | BW, FM |
| Zemel, 2005a [56] (USA) | 9 | 36 (29) | 26–55 | Healthy obese, low dairy consumers BMI = 30–40 | 86 | 3 serves low-fat dairy/day providing 1200 mg/day Ca, one as fluid milk. | Habitual diet 0–1 serves diary/day providing 500 mg/day Ca. | ~2.5 servings | −2092 kJ | Yes | No | 24 | BW, FM, LM |
| Zemel, 2005b [46] (USA) | 9 | 38 (34) | 18–50 | Healthy obese BMI = 30–39.9 | 79 | 3 serves (3× 170 g) fat free yoghurt (Yoplait Light) | 0–1 serves dairy/day + 3 serves of sugar-free, Ca-free, gelatin dessert (42 kJ/serve) | ~2.0 servings | −2092 kJ | Yes | No | 12 | BW, FM, LM |
| Zemel, 2009 [54] (USA) | 9 | 70 (64) | 18–35 | Healthy overweight/mildly obese, low Ca intake (<600 mg/day) BMI = 25–34.9 | 77 | 3 serves dairy/day (full/low-fat milk, cheese, yogurt) providing 1400 mg Ca/day | 0–1 serve dairy/day providing 500 mg Ca/day | 3.0 servings | −2092 kJ | Yes | No | 12 | BW, FM, LM |
| Dairy Supplement Studies | |||||||||||||
| Aldrich, 2011 [48] (USA) | 8 | 12 (10) | 40–60 | Overweight/obese BMI = 27–32 | 80 | 3× 28 g/day serves of Designer Whey (whey protein isolate) + 1.68 serves of milk/day | Assigned control diet including 1.2 serves of dairy/day + Ca tablets to balance Ca intake | 84 g | Tailored to promote 0.75 kg weight loss/week. 8 weeks feeding followed by 12 weeks ad libitum | Yes, for 8 weeks weight loss phase | No | 8 | BW, FM, LM |
| Anderson, 2007 [23] (USA) | 10 | 43 (35) | 20–65 | Healthy obese BMI = 30–40 | 100 | 3× Casein shakes/day (67.5 g protein) (Revival Soy, Physicians Pharmaceuticals Kernersville, NC) | 3× Soy shakes/day (61.8 g protein) | 67.5 | Diets = 4200–5000 kJ | Yes | Physical activity levels of 8400 kJ/week | 16 | BW 10, FM 10, LM 10 |
| Frestedt, 2008 [47] (USA) | 8 | 106 (59) | 25–50 | Obese BMI = 30–42 | NR | 2×/day whey fraction high in leucine (Prolibra ™) 20 min before breakfast and dinner <1 serving of dairy/day | 2×/day maltodextrin <1 serving of dairy/day | 20 g | −2092 kJ | Yes | No | 12 | BW, FM, LM |
| Kasim-Karakas, 2009 [49] (USA) | 11 | 33 (24) | 18–45 | PCOS BMI = 25–40 | 100 | Whey protein isolate (96% pure) (Glanbia Foods, Twin Falls, ID) | Glucose + maltose + tricalcium phosphate | 60 g | −1883 kJ | Yes | No | 8 | BW, FM, LM |
| Longland, 2016 [42] (Canada) | 12 | 40 (40) | 18–30 | Overweight BMI > 25 | 0 | Whey protein isolate (Agropur IsoChill 9010) added to 680 ± 120 mL/day skimmed milk. Total whey consumed: 85 ± 20 g/day. 3–4 beverage/day; one consumed immediately after training. | Maltodextrin added to 530 ± 116 mL/day whole milk. Total whey consumed: 12 ± 9 g/day. 3–4 beverage/day; one consumed immediately after training. | ~73 g | 40% lower energy than estimated require-ments | Yes | RT + AT: 6×/week | 4 | BW, FM, LM |
| Piccolo, 2015 [21] (USA) | 9 | NR (29) | 18–56 | Obese with metabolic syndrome BMI = 27–42 | 100 | 2×/day 10 g whey-based supplement (Glanbia, Inc.) | 2×/day 10 g gelatin-based protein supplement (Glanbia, Inc.) | 20 g | Tailored to achieve 5%–10% reduction in body weight (−2740 ± 584 kJ) | Yes | No | 8 | BW |
| Quality Assessment of Body of Evidence | Number of Participants | Effect Estimate | Quality (Degree of Certainty) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Number Studies 1 | Design | Risk of Bias | Inconsistency | Indirectness | Imprecision | Publication Bias | Dairy | Control | Mean Difference (95% CI) (kg) | |
| 1. Increased intake of dairy products under conditions of energy-restriction without resistance training enhances body weight loss in 18–50-year-old overweight/obese participants. | ||||||||||
| 18 (19) | RCT | Moderate 2 | Low 3 | Moderate 4 | Low | Moderate | 443 | 421 | −0.92 [−1.63, −0.20] | ⊕⊕⊕ Moderate 5 |
| 2. Increased intake of dairy products under conditions of energy-restriction without resistance training enhances body weight loss in 18–50-year-old overweight/obese women. | ||||||||||
| 17 (17) 6 | RCT | Moderate 2 | Low 7 | Low | Low | Moderate | 331 | 313 | −1.16 [−1.66, −0.66] | ⊕⊕⊕⊕ High |
| 3. Increased intake of dairy products under conditions of energy-restriction without resistance training enhances body fat mass loss in 18–50-year-old overweight/obese participants. | ||||||||||
| 15 (16) | RCT | Moderate 2 | Low 8 | Moderate 4 | Low | Moderate | 374 | 367 | −1.24 [−2.10, −0.37] | ⊕⊕⊕ Moderate 5 |
| 4. Increased intake of dairy products under conditions of energy-restriction without resistance training enhances body fat mass loss in 18–50-year-old overweight/obese women. | ||||||||||
| 14 (14) 6 | RCT | Moderate 2 | Low 9 | Low | Low | Moderate | 262 | 259 | −1.49 [−2.06, −0.92] | ⊕⊕⊕⊕ High |
| 5. Increased intake of dairy products under conditions of energy-restriction in conjunction with resistance training enhances body weight loss in 18–50-year-old overweight/obese participants. | ||||||||||
| 6 (7) | RCT | Moderate 10 | Low 11 | Moderate 4 | Moderate 12 | Moderate | 187 | 120 | 0.36 [−0.34, 1.07] | ⊕⊕⊕ Moderate |
| 6. Increased intake of dairy products under conditions of energy-restriction in conjunction with resistance training enhances body fat mass loss in 18–50-year-old overweight/obese participants. | ||||||||||
| 6 (7) | RCT | Moderate 10 | Substantial 13 | Moderate 4 | High 12 | Moderate | 187 | 120 | 0.09 [−1.20, 1.37] | ⊕⊕ Low 14 |
| 7. Increased intake of dairy products under conditions of energy-restriction reduces the loss in lean mass associated with energy restriction in 18–50-year-old overweight/obese participants. | ||||||||||
| 15 (17) | RCT | Moderate 15 | Substantial 16 | Moderate 4 | Low | Moderate | 367 | 294 | 0.36 [0.01, 0.71] | ⊕⊕⊕ Moderate 17 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stonehouse, W.; Wycherley, T.; Luscombe-Marsh, N.; Taylor, P.; Brinkworth, G.; Riley, M. Dairy Intake Enhances Body Weight and Composition Changes during Energy Restriction in 18–50-Year-Old Adults—A Meta-Analysis of Randomized Controlled Trials. Nutrients 2016, 8, 394. https://doi.org/10.3390/nu8070394
Stonehouse W, Wycherley T, Luscombe-Marsh N, Taylor P, Brinkworth G, Riley M. Dairy Intake Enhances Body Weight and Composition Changes during Energy Restriction in 18–50-Year-Old Adults—A Meta-Analysis of Randomized Controlled Trials. Nutrients. 2016; 8(7):394. https://doi.org/10.3390/nu8070394
Chicago/Turabian StyleStonehouse, Welma, Thomas Wycherley, Natalie Luscombe-Marsh, Pennie Taylor, Grant Brinkworth, and Malcolm Riley. 2016. "Dairy Intake Enhances Body Weight and Composition Changes during Energy Restriction in 18–50-Year-Old Adults—A Meta-Analysis of Randomized Controlled Trials" Nutrients 8, no. 7: 394. https://doi.org/10.3390/nu8070394
APA StyleStonehouse, W., Wycherley, T., Luscombe-Marsh, N., Taylor, P., Brinkworth, G., & Riley, M. (2016). Dairy Intake Enhances Body Weight and Composition Changes during Energy Restriction in 18–50-Year-Old Adults—A Meta-Analysis of Randomized Controlled Trials. Nutrients, 8(7), 394. https://doi.org/10.3390/nu8070394






