Association between Body Mass Index and All-Cause Mortality in Hypertensive Adults: Results from the China Stroke Primary Prevention Trial (CSPPT)
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Sources
2.2. Participants and Treatment
2.3. Follow-Up and Outcomes
2.4. Statistical Analysis
3. Results
3.1. Patient Characteristics
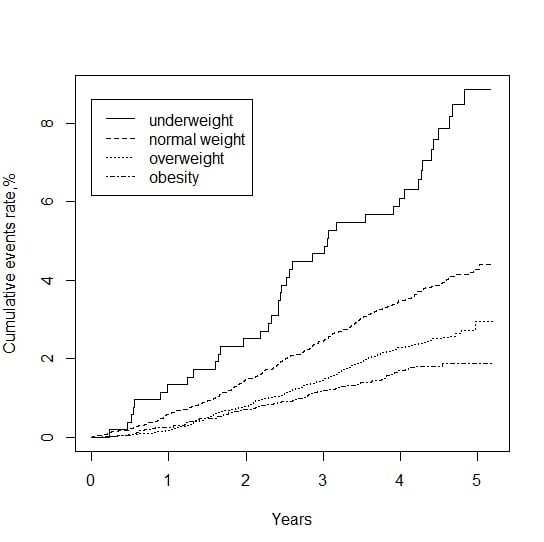
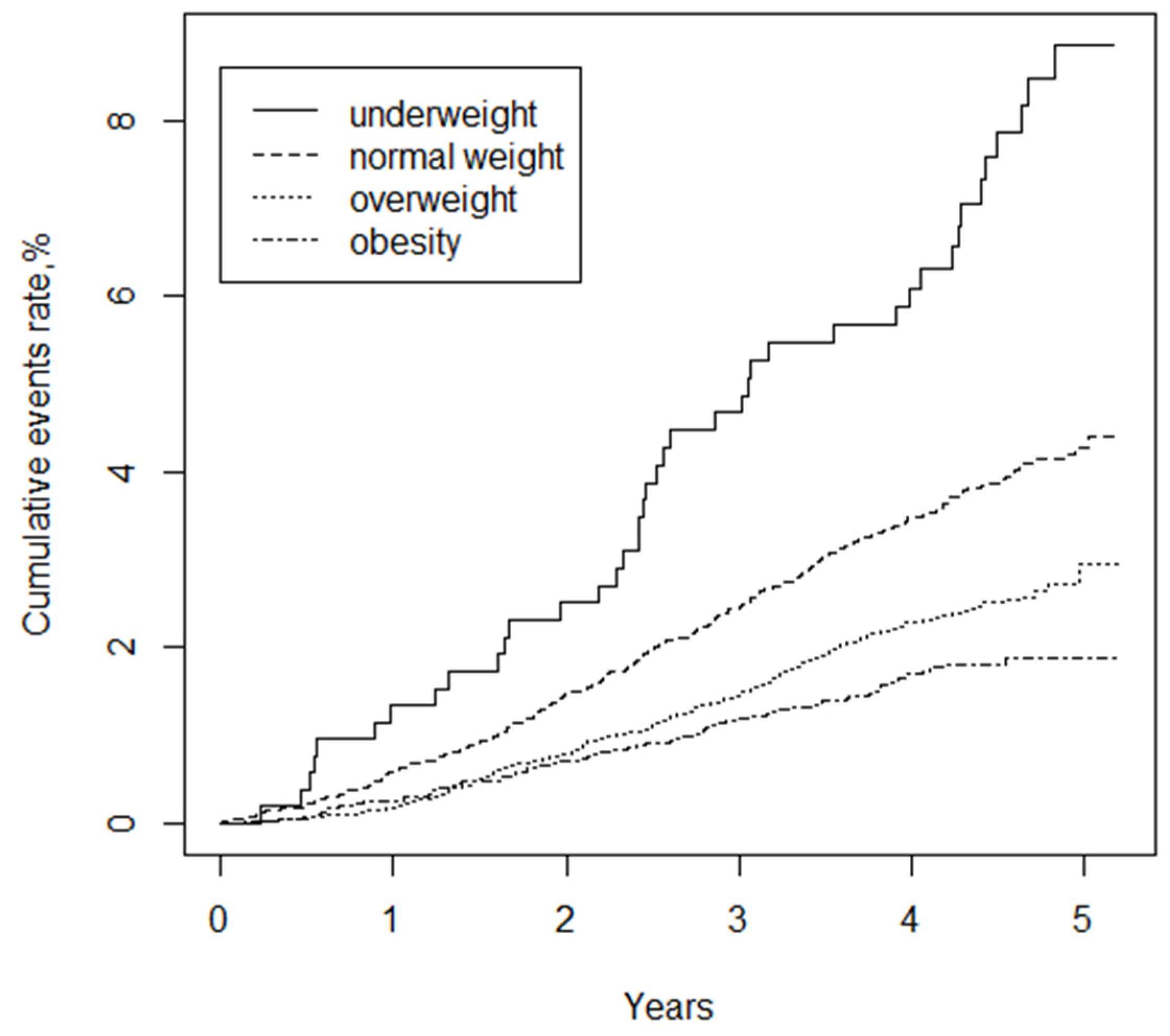
3.2. BMI and Mortality
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| BMI | body mass index |
| BP | blood pressure |
| CI | confidence interval |
| CSPPT | China Stroke Primary Prevention Trial |
| CV | major cardiovascular |
| DBP | diastolic blood pressure |
| FBG | fasting blood glucose |
| Hcy | homocysteine |
| HR | hazard ratio |
| MI | myocardial infarction |
| SBP | systolic blood pressure |
| SCr | serum creatinine |
| TC | total cholesterol |
| TG | triglycerides |
| WHO | The World Health Organization |
References
- Yang, Z.; Hall, A.G. The Financial Burden of Overweight and Obesity among Elderly Americans: The Dynamics of Weight, Longevity, and Health Care Cost. Health Serv. Res. 2008, 43, 849–868. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Global Infobase, 2014. Available online: http://www.who.int/gho/ncd/risk_factors/overweight_text/en/ (accessed on 22 December 2015).
- World Health Organization. Physical Status: The Use and Interpretation of Anthropometry; Report of a WHO Expert Committee; WHO Technical Report Series No. 854; World Health Organization: Geneva, Switzerland, 1995. [Google Scholar]
- Flegal, K.M.; Graubard, B.I.; Williamson, D.F.; Gail, M.H. Excess deaths associated with underweight, overweight, and obesity. JAMA 2005, 293, 1861–1867. [Google Scholar] [CrossRef] [PubMed]
- Flegal, K.M.; Kit, B.K.; Orpana, H.; Graubard, B.I. Association of all-cause mortality with overweight and obesity using standard body mass index categories: A systematic review and meta-analysis. JAMA 2013, 309, 71–82. [Google Scholar] [CrossRef] [PubMed]
- Hu, F.B.; Willett, W.C.; Li, T.; Stampfer, M.J.; Colditz, G.A.; Manson, J.E. Adiposity as Compared with Physical Activity in Predicting Mortality among Women. N. Engl. J. Med. 2004, 351, 2694–2703. [Google Scholar] [CrossRef] [PubMed]
- Winter, J.E.; MacInnis, R.J.; Wattanapenpaiboon, N.; Nowson, C.A. BMI and all-cause mortality in older adults: A meta-analysis. Am. J. Clin. Nutr. 2014, 99, 875–890. [Google Scholar] [CrossRef] [PubMed]
- Zheng, W.; McLerran, D.F.; Rolland, B.; Zhang, X.; Inoue, M.; Matsuo, K.; He, J.; Gupta, P.C.; Ramadas, K.; Tsugane, S.; et al. Association between body-mass index and risk of death in more than 1 million Asians. N. Engl. J. Med. 2011, 364, 719–729. [Google Scholar] [CrossRef] [PubMed]
- Haslam, D.W.; James, W.P. Obesity. Lancet 2005, 366, 1197–1209. [Google Scholar] [CrossRef]
- WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004, 363, 157–163. [Google Scholar]
- Chen, C.; Lu, F.C. The guidelines for prevention and control of overweight and obesity in Chinese adults. Biomed. Environ. Sci. 2004, 17, 1–36. [Google Scholar] [PubMed]
- Liu, L.S. 2010 Chinese guidelines for the management of hypertension. Zhonghua Xin Xue Guan Bing Za Zhi 2011, 39, 579–615. [Google Scholar] [PubMed]
- Huo, Y.; Li, J.; Qin, X.; Huang, Y.; Wang, X.; Gottesman, R.F.; Tang, G.; Wang, B.; Chen, D.; He, M.; et al. Efficacy of Folic Acid Therapy in Primary Prevention of Stroke Among Adults With Hypertension in China. JAMA 2015, 313, 1325. [Google Scholar] [CrossRef] [PubMed]
- EmpowerStats. Available online: http://www.empowerstats.com (accessed on 25 March 2016).
- R Software, Verson 3.2.1. Available online: http://www.R-project.org/ (accessed on 25 March 2016).
- Janssen, I.; Mark, A.E. Elevated body mass index and mortality risk in the elderly. Obes. Rev. 2007, 8, 41–59. [Google Scholar] [CrossRef] [PubMed]
- Woo, J.; Ho, S.C.; Sham, A. Longitudinal changes in body mass index and body composition over 3 years and relationship to health outcomes in Hong Kong Chinese age 70 and older. J. Am. Geriatr. Soc. 2001, 49, 737–746. [Google Scholar] [CrossRef] [PubMed]
- Chung, W.; Ho, F.; Cheng, N.; Lee, M.; Yeh, C. BMI and all-cause mortality among middle-aged and older adults in Taiwan: A population-based cohort study. Public Health. Nutr. 2015, 18, 1839–1846. [Google Scholar] [CrossRef] [PubMed]
- Lin, W.; Albu, J.; Liu, C.; Huang, H.; Pi-Sunyer, F.X.; Li, C.; Li, T.; Lin, C.; Huang, K. Larger Body Mass Index and Waist Circumference Are Associated with Lower Mortality in Chinese Long-Term Care Facility Residents. J. Am. Geriatr. Soc. 2010, 58, 2092–2098. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.S.W.; Auyeung, T.; Chau, P.P.H.; Hui, E.; Chan, F.; Chi, I.; Woo, J. Obesity Can Benefit Survival—A 9-Year Prospective Study in 1614 Chinese Nursing Home Residents. J. Am. Med. Dir. Assoc. 2014, 15, 342–348. [Google Scholar] [CrossRef] [PubMed]
- Romero-Corral, A.; Montori, V.M.; Somers, V.K.; Korinek, J.; Thomas, R.J.; Allison, T.G.; Mookadam, F.; Lopez-Jimenez, F. Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: A systematic review of cohort studies. Lancet 2006, 368, 666–678. [Google Scholar] [CrossRef]
- Chang, V.W.; Asch, D.A.; Werner, R.M. Quality of care among obese patients. JAMA 2010, 303, 1274–1281. [Google Scholar] [CrossRef] [PubMed]
- Schooling, C.M.; Lam, T.H.; Li, Z.B.; Ho, S.Y.; Chan, W.M.; Ho, K.S.; Tham, M.K.; Cowling, B.J.; Leung, G.M. Obesity, physical activity, and mortality in a prospective Chinese elderly cohort. Arch. Intern. Med. 2006, 166, 1498–1504. [Google Scholar] [CrossRef] [PubMed]
- Yi, S.; Ohrr, H.; Shin, S.; Yi, J. Sex-age-specific association of body mass index with all-cause mortality among 12.8 million Korean adults: A prospective cohort study. Int. J. Epidemiol. 2015, 44, 1696–1705. [Google Scholar] [CrossRef] [PubMed]

| Variables | BMI Categories, kg/m2 | |||||
|---|---|---|---|---|---|---|
| All Subjects | <18.5 | 18.5–23.9 | 24.0–27.9 | ≥28.0 | p-Value | |
| Number (%) | 20,694 | 526(2.5) | 8083 (39.1) | 8043 (38.9) | 4042 (19.5) | |
| Age, mean (SD), years | 60.0 (7.5) | 64.6 (6.7) | 61.3 (7.4) | 59.3 (7.5) | 58.2 (7.4) | <0.001 |
| BMI, mean (SD), kg/m2 | 25.0 (3.7) | 17.5 (0.8) | 21.8 (1.4) | 25.8 (1.1) | 30.4 (2.2) | <0.001 |
| Male, No. (%) | 8491 (41.0) | 271 (51.5) | 3863 (47.8) | 3137 (39.0) | 1220 (30.2) | <0.001 |
| Center, No. (%) | <0.001 | |||||
| Anqing | 5211 (25.2) | 350 (66.5) | 3119 (38.6) | 1406 (17.5) | 336 ( 8.3) | |
| Lianyungang | 15,483 (74.8) | 176 (33.5) | 4964 (61.4) | 6637 (82.5) | 3706 (91.7) | |
| SBP, mean (SD), mmHg | ||||||
| baseline | 166.9 (20.4) | 164.3 (17.9) | 166.0 (20.0) | 167.1 (20.4) | 168.4 (21.4) | <0.001 |
| on-treatment | 139.4 (10.9) | 138.8 (10.8) | 138.9 (11.0) | 139.4 (10.8) | 140.4 (11.0) | <0.001 |
| DBP, mean (SD),mmHg | ||||||
| baseline | 94.1 (11.9) | 88.0 (11.4) | 91.8 (11.7) | 95.0 (11.6) | 97.7 (11.9) | <0.001 |
| on-treatment | 82.9 (7.5) | 78.9 (7.7) | 81.5 (7.4) | 83.5 (7.2) | 85.3 (7.2) | <0.001 |
| Pulse, mean (SD),bpm | 73.6 (10.1) | 74.0 (11.0) | 73.6 (10.2) | 73.5 (10.1) | 73.8 (9.9) | 0.53 |
| Smoking status (%) | <0.001 | |||||
| never | 14,252 (68.9) | 293 (55.7) | 5015 (62.1) | 5791 (72.0) | 3153 (78.0) | |
| former | 1567 (7.6) | 35 (6.7) | 604 (7.5) | 649 (8.1) | 279 (6.9) | |
| current | 4867 (23.5) | 198 (37.6) | 2459 (30.4) | 1601 (19.9) | 609 (15.1) | |
| Alcohol drinking (%) | <0.001 | |||||
| never | 14,265 (69.0) | 343 (65.2) | 5155 (63.8) | 5665 (70.5) | 3102 (76.8) | |
| former | 1458 (7.0) | 52 (9.9) | 609 (7.5) | 540 (6.7) | 257 (6.4) | |
| current | 4960 (24.0) | 131 (24.9) | 2313 (28.6) | 1836 (22.8) | 680 (16.8) | |
| Education (%) | <0.001 | |||||
| illiterate | 13,221 (63.9) | 365 (69.4) | 5261 (65.1) | 4999 (62.2) | 2596 (64.3) | |
| primary | 3446 (16.7) | 103 (19.6) | 1468 (18.2) | 1296 (16.1) | 579 (14.3) | |
| secondary or above | 4015 (19.4) | 58 (11.0) | 1347 (16.7) | 1745 (21.7) | 865 (21.4) | |
| Stress (%) | 0.035 | |||||
| mild | 12,578 (60.8) | 289 (54.90) | 4846 (60.0) | 4960 (61.7) | 2479 (61.4) | |
| moderate | 6921 (33.4) | 204 (38.8) | 2765 (34.2) | 2627 (32.7) | 1323 (32.8) | |
| severe | 1189 (5.7) | 33 (6.3) | 464 (5.7) | 454 (5.6) | 237 (5.9) | |
| FPG, mean (SD), mmol/L | 5.8 (1.7) | 5.3 (1.6) | 5.6 (1.6) | 5.9 (1.8) | 6.1 (1.7) | <0.001 |
| TC, mean (SD), mmol/L | 5.5 (1.2) | 5.0 (1.2) | 5.4 (1.2) | 5.6 (1.2) | 5.7 (1.2) | <0.001 |
| TG, mean (SD), mmol/L | 1.7 (1.2) | 1.2 (0.5) | 1.4 (0.8) | 1.8 (1.0) | 2.0 (1.8) | <0.001 |
| HDL-C, mean (SD), mmol/L | 1.3 (0.4) | 1.6 (0.4) | 1.5 (0.4) | 1.3 (0.3) | 1.2 (0.3) | <0.001 |
| SCr, mean (SD), umol/L | 66.0 (19.3) | 67.6 (16.7) | 67.3 (19.6) | 65.6 (20.5) | 64.0 (16.3) | <0.001 |
| Hcy, mean (SD), umol/L | 14.5(8.4) | 14.3 (7.7) | 14.5 (8.1) | 14.5 (8.4) | 14.3 (8.9) | 0.534 |
| Albumin, mean (SD), g/L | 49.0 (5.9) | 47.57 (6.6) | 48.57 (6.0) | 49.34 (5.7) | 49.34 (5.6) | <0.001 |
| Treatment (%) | 0.832 | |||||
| Enalapril | 10,352 (50.0) | 271 (51.5) | 4053 (50.1) | 4025 (50.0) | 2003 (49.6) | |
| Enalapril-Folic Acid | 10,342 (50.0) | 255 (48.5) | 4030 (49.9) | 4018 (50.0) | 2039 (50.4) | |
| BMI kg/m2 | N | Event (%) | Curde Rate | All-Cause Mortality | |||
|---|---|---|---|---|---|---|---|
| Model 1 | p-Value | Model 2 | p-Value | ||||
| Continuous | 20,694 | 622 (3.0%) | 7.03 | 0.90 (0.88, 0.92) | <0.001 | 0.94 (0.91, 0.96) | <0.001 |
| <18.5 | 526 | 41 (7.8%) | 17.63 | 1.97 (1.42, 2.73) | <0.001 | 1.56 (1.11, 2.18) | 0.010 |
| 18.5–23.9 | 8083 | 312 (3.9%) | 8.93 | 1 | 1 | ||
| 24.0–27.9 | 8043 | 197 (2.4%) | 5.76 | 0.64 (0.54, 0.77) | <0.001 | 0.78 (0.64, 0.95) | 0.012 |
| ≥28 | 4042 | 72 (1.8%) | 4.24 | 0.47 (0.37, 0.61) | <0.001 | 0.64 (0.48, 0.85) | 0.002 |
| Variables | N | Death, n | % | BMI Categories( kg/m2) | Adjusted * p for Interaction | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| <18.5 | 18.5–23.9 | 24.0–27.9 | ≥28 | ||||||||
| HR 95%CI | p-Value | HR 95%CI | HR 95%CI | p-Value | HR 95%CI | p-Value | |||||
| All Participants | 20,694 | 622 | 3.0 | 1.56 (1.10, 2.14) | 0.012 | 1 | 0.80 (0.66, 0.97) | 0.026 | 0.66 (0.49, 0.87) | 0.003 | |
| Sex | 0.692 | ||||||||||
| Females | 12,203 | 258 | 2.1 | 1.24 (0.66, 2.33) | 0.505 | 1 | 0.78 (0.58, 1.05) | 0.097 | 0.60 (0.41, 0.89) | 0.010 | |
| Males | 8491 | 364 | 4.3 | 1.74 (1.16, 2.58) | 0.007 | 1 | 0.82 (0.63, 1.07) | 0.144 | 0.71 (0.46, 1.09) | 0.119 | |
| Center | 0.719 | ||||||||||
| Anqing | 5211 | 218 | 4.2 | 1.58 (1.04, 2.38) | 0.030 | 1 | 0.72 (0.49, 1.05) | 0.090 | 0.88 (0.45, 1.72) | 0.709 | |
| Lianyungang | 15,483 | 404 | 2.6 | 1.59 (0.88, 2.88) | 0.125 | 1 | 0.84 (0.67, 1.06) | 0.153 | 0.65 (0.47, 0.90) | 0.009 | |
| Age | 0.588 | ||||||||||
| <60 | 10,469 | 172 | 1.6 | 1.82 (0.78, 4.25) | 0.167 | 1 | 0.82 (0.56, 1.19) | 0.302 | 0.84 (0.52, 1.34) | 0.463 | |
| ≥60 | 10,225 | 450 | 4.4 | 1.62 (1.13, 2.34) | 0.009 | 1 | 0.75 (0.60, 0.95) | 0.016 | 0.53 (0.36, 0.76) | <0.001 | |
| Smoking Status | 0.298 | ||||||||||
| Never | 14,254 | 327 | 2.3 | 1.40 (0.83, 2.37) | 0.208 | 1 | 0.80 (0.61, 1.04) | 0.090 | 0.62 (0.43, 0.89) | 0.009 | |
| Former | 1570 | 75 | 4.8 | 3.76 (1.64, 8.67) | 0.002 | 1 | 1.37 (0.75, 2.49) | 0.305 | 1.28 (0.56, 2.90) | 0.558 | |
| Current | 4869 | 219 | 4.5 | 1.33 (0.79, 2.25) | 0.281 | 1 | 0.70 (0.50, 1.00) | 0.052 | 0.60 (0.33, 1.09) | 0.095 | |
| Alcohol | |||||||||||
| Never | 14,265 | 355 | 2.5 | 1.54 (0.98, 2.43) | 0.064 | 1 | 0.75 (0.58, 0.97) | 0.026 | 0.63 (0.44, 0.89) | 0.009 | 0.906 |
| Former | 1458 | 80 | 5.5 | 2.51 (1.17, 5.42) | 0.019 | 1 | 0.85 (0.48, 1.48) | 0.559 | 0.50 (0.20, 1.28) | 0.148 | |
| Current | 4960 | 186 | 3.8 | 1.27 (0.65, 2.47) | 0.482 | 1 | 0.93 (0.65, 1.34) | 0.695 | 0.84 (0.46, 1.55) | 0.581 | |
| Education | 0.599 | ||||||||||
| Illiterate | 13,221 | 411 | 3.1 | 1.43 (0.95, 2.15) | 0.087 | 1 | 0.75 (0.59, 0.96) | 0.021 | 0.67 (0.48, 0.94) | 0.022 | |
| Primary | 3446 | 116 | 3.3 | 1.52 (0.70, 3.31) | 0.290 | 1 | 0.98 (0.63, 1.53) | 0.935 | 0.49 (0.22, 1.09) | 0.080 | |
| Secondary or above | 4015 | 94 | 2.3 | 2.18 (0.88, 5.40) | 0.093 | 1 | 0.78 (0.47, 1.29) | 0.330 | 0.68 (0.33, 1.39) | 0.290 | |
| Stress | 0.506 | ||||||||||
| Mild | 12,574 | 391 | 3.1 | 1.26 (0.79, 2.00) | 0.333 | 1 | 0.73 (0.57, 0.94) | 0.013 | 0.66 (0.47, 0.94) | 0.019 | |
| Moderate | 6919 | 202 | 2.9 | 1.89 (1.13, 3.17) | 0.016 | 1 | 0.91 (0.64, 1.29) | 0.602 | 0.58 (0.33, 1.01) | 0.054 | |
| Severe | 1188 | 28 | 2.4 | 2.97 (0.59, 14.93) | 0.187 | 1 | 1.29 (0.49, 3.42) | 0.604 | 0.90 (0.24, 3.32) | 0.869 | |
| Albumin, g/L | 0.527 | ||||||||||
| <49 | 11,813 | 412 | 3.5 | 1.48 (1.00, 2.18) | 0.051 | 1 | 0.73 (0.57, 0.93) | 0.012 | 0.68 (0.48, 0.97) | 0.033 | |
| ≥49 | 8876 | 210 | 2.4 | 1.87 (0.98, 3.56) | 0.058 | 1 | 0.87 (0.63, 1.20) | 0.394 | 0.56 (0.34, 0.90) | 0.016 | |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, W.; Li, J.-P.; Zhang, Y.; Fan, F.-F.; Xu, X.-P.; Wang, B.-Y.; Xu, X.; Qin, X.-H.; Xing, H.-X.; Tang, G.-F.; et al. Association between Body Mass Index and All-Cause Mortality in Hypertensive Adults: Results from the China Stroke Primary Prevention Trial (CSPPT). Nutrients 2016, 8, 384. https://doi.org/10.3390/nu8060384
Yang W, Li J-P, Zhang Y, Fan F-F, Xu X-P, Wang B-Y, Xu X, Qin X-H, Xing H-X, Tang G-F, et al. Association between Body Mass Index and All-Cause Mortality in Hypertensive Adults: Results from the China Stroke Primary Prevention Trial (CSPPT). Nutrients. 2016; 8(6):384. https://doi.org/10.3390/nu8060384
Chicago/Turabian StyleYang, Wei, Jian-Ping Li, Yan Zhang, Fang-Fang Fan, Xi-Ping Xu, Bin-Yan Wang, Xin Xu, Xian-Hui Qin, Hou-Xun Xing, Gen-Fu Tang, and et al. 2016. "Association between Body Mass Index and All-Cause Mortality in Hypertensive Adults: Results from the China Stroke Primary Prevention Trial (CSPPT)" Nutrients 8, no. 6: 384. https://doi.org/10.3390/nu8060384