2. Methods
The recommendations in this article are based on data collected from three sources: NIN monitoring data (e.g., sales and distribution indicators); a qualitative survey with health workers; and a quantitative coverage survey with caregivers.
Table 2 provides a summary of the project design, sampling size, and implementation time frame.
2.1. Coverage Survey Details, Sampling Method, and Sampling Size Calculation
The coverage survey consisted of structured interviews for the caregivers that were adapted from GAIN’s standard Fortification Assessment Coverage Tool (FACT) and composed of different validated modules.
A stratified multistage cluster sampling with probability proportional to size (PPS) was used to select caregivers. At the first stage, two districts were selected per province by simple random sampling (SRS). In the second stage, four communes per selected district were selected. Each commune was considered as one primary sampling unit. A total of 32 communes were selected. In the final stage, children from 6 to 60 months old were selected by SRS in each commune from the list of the children under 5 years old living in the 32 selected communes.
The primary survey respondents were caregivers of the selected children. To get a precision of 5.0% with an expected design effect of 2.0 and assuming the effective coverage would be around 8%, the minimum sample size was 230 children per province, i.e., 920 children in total and 29 children per commune. To allow a 15% drop-out or non-response rate (caregivers not coming to the CHC or refusing to respond), 35 children per commune were selected. For the health workers, all the health staff at the selected provinces, districts, and communes who were trained were recruited to participate in the in-depth health worker interviews.
2.2. Coverage Survey Instruments and Indicator Definition
The coverage terminology is defined as follows:
Message coverage: percentage of caregivers who have ever heard of or seen Bibomix.
Contact coverage: percentage of children under five years who have ever tried Bibomix.
Partial coverage: percentage of children under five years who consumed at least one sachet of Bibomix over the past week.
Effective coverage: percentage of children under five who consumed at least three sachets of Bibomix over the past week.
The three sachets per week consumption frequency was calculated assuming 60 sachets over six months as recommended by WHO (two months consuming the MNP daily and four months without MNP, [
13]). These guidelines, also recommended by the Home Fortification Technical Advisory Group Programmatic Brief were adapted to be more practical from a program implementation perspective by allowing more flexibility of purchase and use by consumers [
19]. The 60 sachets over six months represents an average consumption of 10 sachets per month, and 2.5 sachets per week, which was round up to three sachets per week for ease of communication by health workers, and to be sure that the recommended levels of consumption would lead to nutritional impact [
20].
Caregivers were asked to recall the MNP consumption over the past week. A one-week recall was chosen to avoid a recall for a longer period, which could result in significant recall bias and other related errors.
The MNP compliant use was assessed among the caregivers. Compliance was defined if all of the following conditions were met:
The caregiver gave one full sachet of MNP on the most recent day.
The MNP sachet was mixed into one meal.
The MNP sachet was added separately for the older infant or young child with mashed family food or was added with semi-solid food prepared for the infant/child.
The MNP sachet was added just before serving the child a meal.
In addition, data were collected on the household assets and amenities, to allow us to construct a wealth index. A principal component analysis (PCA) was run, and to construct the wealth index, the principal component (first factor) was taken to represent the household’s wealth. For further analysis, the sampling was weighed by household size, and the wealth index was divided into quintiles and ranked into five categories, from the poorest to poor, medium, wealthy, and the wealthiest. The wealth index quintile was applied to each survey respondent who was classified into one of the five categories.
2.3. Ethical Considerations for the Coverage Survey Implementation
The survey protocol was approved by the NIN scientific and ethical committee, and signed by Associate Professor Le Danh Tuyen, Director of the NIN, on 28 November 2014 (Ethical Clearance Approval number: 1615/QD-VDD). In addition, the provincial local authorities, as well as the directors of all selected commune health centers, granted permission for the survey. Signed informed consent was obtained from all participating caregivers and health workers. Within the survey database, the respondents were anonymized and identified through unique identifier numbers.
2.4. Coverage Survey Data Collection, Entry, and Analysis
Data collection forms and questionnaires were pretested and translated into Vietnamese. Surveyors were trained for one day on the data collection forms/questionnaires. For both caregivers and health workers, the surveyors administered the questionnaire only after having obtained signed informed consent from the respondent. The survey took place in four provinces (Thai Nguyen, Hai Phong, Quang Nam, and Ca Mau) in eight districts and 32 communes.
Data entry was done in Epidata v.3.1 (The EpiData Association, Odense, Denmark). To reduce entry errors, data entry screens were programmed to accept only predetermined codes or values within a given range for each variable. Data analyses were conducted with SPSS software (SPSS 19.0 for Windows, Chicago, IL, USA). Summary enrollment characteristics of the children and caregivers were calculated as means ± standard deviation (SD) for continuous measures. Differences in prevalence were tested with chi-square statistics and associations between variables were tested with Pearson correlation. A p-value of < 0.05 was considered significant.
3. Results
3.1. Routine Monitoring Results
MNPs were delivered for sale by health center staff for approximately six months to a total of 337 health centers, including four provincial health centers (one in each province), 20 district health centers, and 313 CHCs. In Hai Phong, 7 district health centers and 128 CHCs participated in the pilot; in Thai Nguyen, three district health centers and 37 CHCs participated; in Quang Nam, six district health centers and 94 CHCs participated; and in Ca Mau, four district health centers and 54 CHCs participated.
More than 1000 training manuals, 1000 booklets, and 340 counseling cards were developed and produced for the health workers to support their training and counseling. In addition, 340 product displays, 300 posters to drive awareness of MNP, 300 posters to educate on correct use of MNP, and 25,000 educational fans (on home fortification of complementary foods with MNPs) were produced and delivered to the selected commune health centers, together with the guidelines on how to use or distribute these materials.
MNP sales in the four provinces during the project timeline varied by province, with a total of 1,000,500 sachets sold through the pilot and an additional 497,940 sachets sold to other national nutrition programs during the pilot intervention. Thus, the target of 1.5 million sachets in the initial business plan was reached.
The main purchaser of the MNP was the primary caregiver, i.e., the mother (99.4%). Caregivers from the northern provinces, Hai Phong and Thai Nguyen, bought Bibomix in full 60-sachet boxes (52% and 71% of caregivers, respectively), while 74% of caregivers from the center province (Quang Nam) bought the product mainly in 10-sachet packets. In the southern province (Ca Mau), 49% of caregivers bought single sachets and 43% bought packets of 10 sachets.
3.2. Health Worker Survey (Monitoring and Coverage Survey) Results
A total of 991 health workers were trained on IYCF, WASH, and home fortification of complementary foods with MNPs (all health workers who were contacted attended the training). A large majority of the health workers (80.8%) who were trained reported having counseled caregivers at their last visit to the health center. The mean duration of one counseling session was 13.9 ± 7.4 min (no significant differences among the provinces).
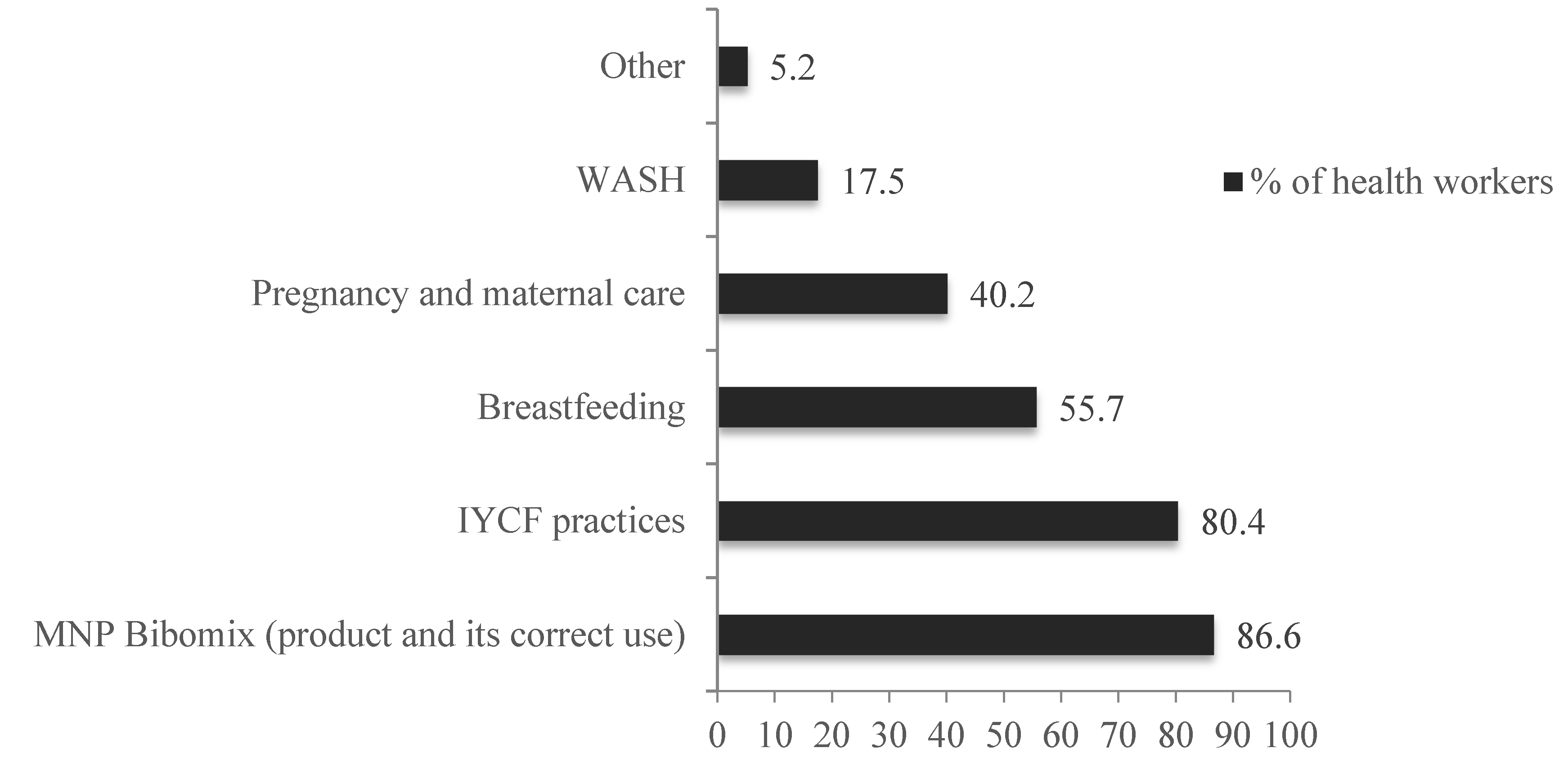
Health workers were questioned about the counseling topics they provided to the caregivers and had the possibility to give multiple responses. The main counselling topics provided to caregivers were on IYCF, MNP, and breastfeeding, as detailed in
Figure 2, demonstrating that Bibomix was well integrated with the promotion of optimal IYCF practices.
The majority of the health workers reported using BCI materials as a support for their counseling, with the majority of them using the training manual and the counseling cards. Specifically, 72.8% of the health staff reported using counseling cards, 69.9% used the training manual, 65.2% used the educational fan, and 56.5% used the educational poster; evidence that most materials were used in compliance with the guidelines.
Notably, only 24 health staff (20%) did not encounter any difficulties promoting the MNP to caregivers. For the remaining majority, a variety of barriers to sales, thereby impeding effective coverage, were reported: 11.7% of health workers reported that product usage, i.e., mixing Bibomix into semi-solid foods, was particularly difficult for feeding children over two years old, as these children were not eating semi-solid food anymore; 11.5% of health workers stated that the price of Bibomix was found to be too expensive for caregivers (no significant differences were found between provinces); the lack of rapid and visible benefit/impact on the child’s health after using Bibomix was also raised as a barrier to sales by five health staff. These health workers reported counseling caregivers that improvement in nutritional status with MNP consumption has been proven, but that it is a long-term process and that the product must be used for at least six months to be effective. Eight health workers reported that they encountered caregivers who stopped using Bibomix because of some side effects they attributed to the MNPs use, such as vomiting and diarrhea. The link between MNP consumption and side effects was not proven, and the health staff did their very best to address the problem, providing the required referrals and reassuring the caregivers. Finally, 8.3% of health staff reported that it was difficult to sell the MNPs to caregivers because Bibomix had a lot of competitors and there were many other similar products to Bibomix that were better known.
During field trips to the provinces, the health workers also mentioned that the current guideline on the MNP ordering cycle and supply was quite difficult for them to implement. Indeed, health staff did not forecast the MNP orders “optimally”, as for instance they ordered too much product during their 1st order to NIN which led to budget issues regarding paying for MNP supplies, as they did not sell all the boxes ordered the first month (while the policy was to pay for the MNP based on its order, not on its sales). Although it happened only rarely, according to some health staff, transportation challenges also lead to a shortage of Bibomix in three out of 337 health centers (one in Hai Phong, and two in Quang Nam provinces). None of the supply shortage at health centers was due to lack of production capacity at the plant, but rather to underestimations during forecasting and payment delays.
3.3. MNP Coverage and Compliance Use among Mothers of Children under Five Years
The coverage survey at the end of the pilot study included a random sample of 962 surveyed caregivers with children from 6 to 60 months meeting the inclusion criteria.
Table 3 presents the characteristics of the surveyed children and their caregivers.
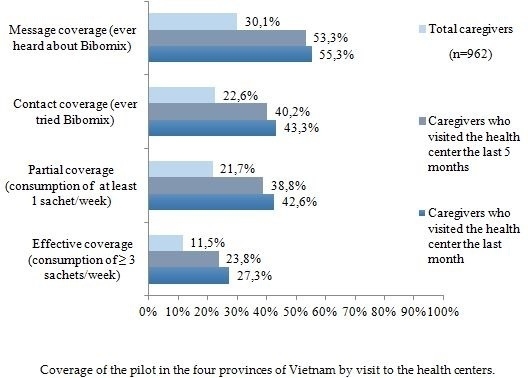
The MNP coverage survey during the pilot implementation showed that 30.1% of the surveyed caregivers had ever heard about Bibomix, 22.6% of them had ever given the product to their child, 21.7% of them had given some of it to their child (at least one sachet per week), and 11.5% used the product effectively (i.e., at least three sachets per week for the child).
MNP message coverage was found higher among the caregivers who had visited the health center the month prior to the coverage survey (
p = 0.003) as illustrated in the
Figure 3, which shows that the health center as a delivery channel for the intervention was a key success factor to guarantee effective MNP coverage.
The caregivers’ access to the health center differed greatly by province, with Ca Mau having the lowest rate of caregivers visiting the health center within the last five months while Hai Phong had the highest, 18.2% and 68.8%, respectively (p < 0.001).
MNP coverage differed significantly by province, with Hai Phong having the highest coverage rates and Ca Mau the lowest (p < 0.05). Message coverage reached 44.2% of caregivers in Hai Phong, 32.6% in Quang Nam, 27.5% in Thai Nguyen, and 17.4% in Ca Mau. The percentage of caregivers who ever gave the MNP to their child (i.e., contact coverage) was 28.6% in Hai Phong, 26.9% in Quang Nam, 20.8% in Thai Nguyen, and 14.6% in Ca Mau. In addition, 26.8% of caregivers in Hai Phong, 26.9% in Quang Nam, 19.1% in Thai Nguyen, and 14.6% in Ca Mau had given at least one sachet of MNP per week to their child. Finally, the effective use of the MNP (i.e., at least three sachets per week for the child) was found among 17.7% of caregivers in Hai Phong, 12.8% of caregivers in Quang Nam, 11% in Thai Nguyen and 5.1% in Ca Mau. In Ca Mau province, while fewer than 20% of the caregivers had heard about the MNP and the effective coverage was only 5.1%, the conversion rate from product awareness to product trial was the highest, with 84.0% of the caregivers who had heard about the MNP Bibomix trying it. For the remaining provinces, the conversion rate was 65.0% in Hai Phong, 72.0% in Thai Nguyen, and 82.0% in Quang Nam (p = 0.02).
The results of the caregivers visit and counseling at the health centers, as well as the MNP coverage, are summarized in the
Figure 4.
In terms of compliant use, caregivers of children under five years of age using the MNP reported adding it just before the meal was served (86%), adding it to semi-solid food (85% total, and 82% among caregivers with children above two years old), mixing the MNP into one single meal (80%), and giving one full sachet per day (84%). When combining all optimal use behaviors, results show that the majority of the caregivers surveyed (59.0%) were compliant with all the recommended product use behaviors.
Among the 290 caregivers who had heard of MNPs, 74.8% of them had tried it for their child. The most frequently mentioned reasons why the 73 caregivers who had heard of Bibomix did not try it were: (1) “Don’t see the need for Bibomix” (25%); (2) No specific reason given (18%); (3) “I am using another product” (12%); and (4) “I haven’t seen Bibomix at the health center” (11%). In addition, among the 209 caregivers partially covered (i.e., who use the MNP for their child at least once per week), only 16 caregivers reported that they stopped buying the MNP, mainly due to child refusal (56.2%), lack of perceived need (25%), price (6.2%), “do not see impact on child’s health” (6.2%), and side effects (6.2%).
Households’ assets and amenities were analyzed in order to apply a wealth index quintile for each survey respondent, from the poorest, to poor, medium, wealthy, and wealthiest quintile. In northern provinces (Hai Phong and Thai Nguyen), the majority of the caregivers were from the medium to the wealthiest quintiles, while in the center and the southern provinces (Quang Nam and Ca Mau), they were mainly from the poorest to the medium quintiles (
p < 0.001). The MNP purchase trends by caregivers and by the wealth index quintiles are represented in
Figure 5.
There was a positive correlation between the number of MNP sachets purchased and the wealth index (r = 0.434, p < 0.001).
4. Discussion
The results illustrate that the pilot project model of the locally manufactured MNP Bibomix, via the public health system, was successful in attaining the project goals. It was indeed the first time in the country that a MNP produced by the NIN was distributed for sale through the local health centers, and the MNP coverage results and financial sustainability are very promising.
The overall effective coverage of the project was 11.5% among all surveyed caregivers (and 27.3% among the ones who had visited the health center in the 30 days prior to the survey), which was higher than the initial projection of 8% effective coverage. In addition, 75.0% of the caregivers who had heard of Bibomix purchased it and gave it to their child, demonstrating a high conversion rate from product awareness to product trial. The MNP coverage in the province in the south (Ca Mau) did not reach the 8% target, with an effective coverage of only 5.1%. This was due mainly to the fact that fewer than 20% of caregivers in Ca Mau had ever heard about Bibomix, and the main reason was that they had difficulties accessing a health center. Indeed, only 18.2% of the caregivers surveyed had visited the health center within the last five months, and this could be explained because, unlike the other provinces, Ca Mau has an extensive network of canals from the Mekong Delta, which isolates the health centers from the village/commune and makes it more difficult to access for caregivers.
Therefore, while the health system was a reliable and trusted channel for the caregivers, one of the weaknesses and limitations of this pilot model was adapting for differentiated access to health centers. The MNP distribution intervention did not reach caregivers who did not have access to the local public health centers. For these specific groups (especially the ethnic minorities) who are “left behind” in the current public health system, a complementary delivery model to reach them is required.
The purchase trends also showed that caregivers in Northern provinces preferred buying a full box of Bibomix, while in the center and southern provinces they purchased mainly the intermediate packet and primarily single sachets respectively. Wealth index varies significantly by provinces, as the majority of caregivers were from the medium to the wealthiest quintiles in the northern provinces, while in the center and southern there were mainly from the poorest to the medium quintiles. The number of sachets bought by the caregivers was positively correlated with the wealth index, demonstrating that the innovation in the packaging size, i.e., offering single sachets, packets of 10 sachets or boxes of 60 sachets, proved to be well suited to adapt to different purchasing powers. The different price points helped increase the product affordability and can be considered an important factor in driving trial of the MNP. As the coverage survey was conducted only five months after the start of the MNP sales at the health centers, repurchase trends by caregivers could not be assessed.
A majority of the health workers reported encountering difficulties when selling Bibomix to caregivers. These barriers were related mainly to the product Bibomix itself, where health workers reported caregiver concerns about the product usage/dosage, the lack of visible impact in the short term, and attributing side effects. Addressing these barriers would require further investment in awareness building and messaging (such as related long-term use of Bibomix to see health benefits) through continued counseling by the health workers. In addition, the distribution channel through commune health centers, while promising, was not yet “optimal” during the pilot, as there were reports of difficulties related to supply/logistics, such as budgeting for payment for supplies based on order rather than sales and transportation issues, which would require review and further training to better optimize the MNP supply and cash flow, and especially on forecasting and monitoring.
The strategy used in the pilot to strengthen the health system by increasing the capacity of health workers to counsel on IYCF and home fortification practices effectively was successful, and embed the distribution of MNPs in existing platforms. The BCI implementation showed that, through investment in training with supportive communication and education materials, IYCF and home fortification with MNPs messaging was effectively transferred to caregivers by interpersonal communication activities, such as counseling by the health workers. Indeed, the high compliance rate in the product use among the caregivers (59.0%) indicates that recommended behaviors were well communicated by the health staff, who was the primary source of credible information, to the caregivers. The MNP was correctly used in mashed/semi-solid foods even for children over two years old in most cases. This interesting result demonstrates that, while some caregivers complained about the MNP application not being adapted for children over two years old (as they no longer eat mashed or semi-solid food at that age), proper health staff training on product use demonstration was reflected in counseling to the caregivers that overcame established practices.
A limitation of the coverage survey was that, while the questionnaire was developed to have harmonized questions for countries implementing MNP programs globally, some relevant indicators that would have helped better understand caregivers’ behaviors/purchase trends/use of Bibomix in Vietnam were missing. For instance, data on ethnicity of the caregivers were missing, which would have allowed segmenting by ethnic minority groups. In addition, information about the frequency of visits to the health centers was not collected. Another limitation was that all the data were collected through face-to-face interviews with caregivers at the health centers, and not at the home. Caregivers of the selected children were invited to come at the CHC, which could have biased the responses given because they may have wanted to please the surveyors. Caregivers were asked to report consumption within one week, which is commonly used in dietary assessment, however may not be representative of habitual practice. The use of one-week recall methodology was chosen to avoid recall bias. In addition, as this survey was conducted in a programmatic setting, budget, and logistics constraints did not allow measurement and tracking of consumption per child, per week. Finally, for health worker routine monitoring, the main limitation was that the health staff did not always use the recording templates that were designed for the project, as they preferred using the recording form that they were already accustomed to. As a result, they could not have recorded the identity of the primary caregivers buying Bibomix, which would have been useful for following up the purchase and repurchase trends.
The findings of this pilot were very promising and subsequent to the pilot, Bibomix MNP was endorsed by the MOH (Decision 4994/QD-BYT on 27 November 2014) in its strategy for micronutrient deficiencies prevention. This policy change is the first key milestone to scaling up MNP distribution in the country using the model piloted through this project. It is also noteworthy that while the pilot ended at the end of December 2014, the counseling services, as well as MNP sales, are still running in the provinces, truly demonstrating political will and ultimately the sustainability of the model.